Chapter 2
Making Glucose Control Your Goal
Many scientific studies show that the most effective way to decrease or eliminate the complications associated with diabetes is to keep blood glucose at or near normal levels. Most health problems that are associated with diabetes arise without many symptoms. Not knowing this simple fact can be a major roadblock to living a healthy life. If you don’t know that a threat to your life exists, then how can you attempt to prevent it? Say you have 45,000 miles on your car and you want to drive your car 20 miles down a steep canyon. Tucked away in the glove box is the manual that states that the braking system should be serviced at 40,000 miles to prevent its potential failure. And say that you did not happen to read every page of your car’s manual and did not know this particular fact. You would likely drive down the canyon completely unaware of the potential danger that lies ahead. Likewise, if glucose control is not your goal, potential dangers lie ahead. In this chapter we discuss the complications of poorly controlled diabetes.
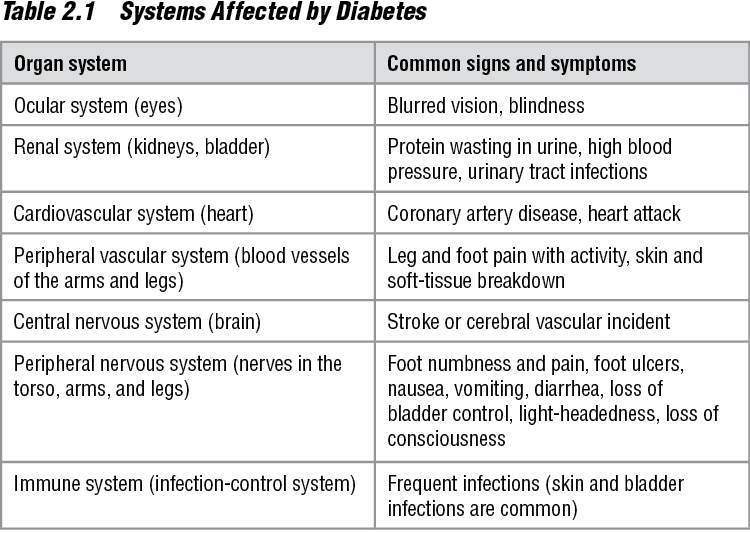
The visual system (eyes), renal system (kidneys), cardiovascular system (heart), peripheral vascular system (blood vessels in the extremities), nervous system (nerves), gastrointestinal system (stomach and intestines), and immune system (infection control) are the bodily systems affected by poor diabetes control. Given that many of these systems interrelate, I discuss diabetes as it relates to vision, the kidneys, the heart and blood vessels, and the nervous system. The effects on gastrointestinal and immune system are discussed as well. These complications are summarized in table 2.1.
Diabetes and Your Vision
Diabetes is a leading cause of blindness in the United States, and the best means of early detection of vision problems is to have an ophthalmologist examine your eyes by dilating them and observing the retina. It is recommended that all people with type 1 diabetes have annual eye exams starting five years after the onset of their condition. Those with type 2 diabetes should have an examination soon after their diagnosis is made. Any visual changes that occur should be taken seriously; such changes warrant a complete eye exam by an ophthalmologist.
Diabetes affects the eyes by damaging the retina, which is referred to as diabetic retinopathy. The retina is the part of the eye that is responsible for sensing light. Retinal damage can occur in two ways. First, the blood vessels that supply nutrients to the cells of the retina can become damaged as a consequence of high glucose levels in the blood that in turn cause bleeding and the formation of blood clots in them. The blood from these vessels that leaks into the eye can obscure light from reaching the retina, causing blindness. And if the retina cannot receive nutrients and oxygen because of a lack of blood flow in the vessels, the cells will die, causing permanent loss of vision.
Sometimes when small blood vessels in the retina are damaged in this way the body will produce new vessels in this area to try to deliver oxygen to the retinal cells. This can lead to far too many new blood vessels being formed in the retina, which in turn block out light and cause blindness. This condition is called proliferative diabetic retinopathy. The current treatment of this condition involves the use of a special laser to slow or stop new vessel overgrowth.
Blurring of vision can also occur when the blood glucose is high. These symptoms can sometimes be resolved when the blood glucose is brought under control. However, it is also known that high glucose levels can lead to nerve damage that can affect the way your eye moves. This is often a permanent condition. If the nerves to your eye muscles do not work properly, blurring of vision will occur.
Diabetes and Your Kidneys
According to the American Diabetes Association, 10 to 21 percent of people with diabetes have kidney disease, referred to as diabetic nephropathy. The kidneys are organs that filter out unnecessary products from your bloodstream and retain the necessary elements, such as proteins and electrolytes (sodium and potassium). However, high glucose levels can lead to an abnormality that allows necessary elements in your blood, such as proteins, to be wasted into the urine. This is referred to as proteiuria, which is a common sign of early kidney failure. Good glucose control through proper diet, exercise, and medication if needed can prevent diabetic nephropathy (Hostetter 2003).
Damage to your kidneys can also lead to the development of high blood pressure, also called hypertension. If you develop high blood pressure, it is important that you control your blood pressure. But if you develop high blood pressure and you have diabetes, it is even more important for you to control your blood pressure. The diseases that are directly related to high blood pressure, such as heart, eye, and kidney disease, may progress more rapidly in someone with diabetes and high blood pressure. Some classes of blood pressure–lowering medications may be more beneficial than others for diabetics with kidney problems. Your physician will need to take into account your medical condition to determine what medications are best for you.
Further damage to the kidneys can occur from untreated or undertreated urinary tract infections. Infections of the bladder are often controlled easily with the implementation of antibiotics. People with diabetes are more susceptible to these types of infections and at a greater risk of kidney damage if the infection spreads from the bladder to the kidneys causing them to become infected, too. This type of infection is commonly referred to as pyelonephritis.
Controlling glucose through exercise is one key to preventing other health problems that can result from diabetes.
It is also important that diabetics with kidney problems not receive contrast materials (a substance that is typically used when your doctor orders special X rays) in their blood until receiving clearance from physicians. We know that these contrast agents can cause kidney damage in anyone, but we also know that those with diabetes are at an increased risk for this to occur. You should carry a medical alert card or something similar to identify you as a person with diabetes in case you require emergency treatment that involves contrast materials. A medical alert card, bracelet, or necklace will allow the medical team to take appropriate steps to protect you from potential harm.
Your doctor can monitor your kidney functioning by using lab tests, which include urine tests for glucose and protein. If your blood glucose is greater than 180 mg/dl, then glucose will appear in your urine; a urine test for elevated glucose levels can be helpful if blood glucose readings are unavailable. In fact, this is how many people with diabetes are initially diagnosed. As described previously, protein in the urine is usually indicative of kidney disease. Various methods of testing for protein in the urine include diagnostic test strips that are dipped into the urine and compared to standard colorimetric charts to determine estimated levels of substances including glucose and protein. This type of test is easy to use in the doctor’s office, takes little time to complete, and is relatively inexpensive. Another test, called the 24-hour urine test, is more accurate and gives more specific levels of protein in the urine. Your doctor will typically order this test if your dip strip test is positive. If your 24-hour urine test shows that there are more than 30 milligrams of protein (albumin), your kidneys are having trouble retaining needed protein, which is evidence that damage has taken place in the kidneys. If this is the case, then your doctor may choose to place you on a common blood pressure medication known as an ACE inhibitor or angiotensin receptor II antagonist, even if you have normal blood pressure. Studies have shown that this particular drug not only controls blood pressure but also protects the kidneys in those with diabetes.
Diabetes and Your Cardiovascular System
Those with diabetes are at high risk for heart and vascular disease. The heart is a muscle that pumps blood throughout the body to supply it with nutrients and oxygen and to take away by-products of metabolism, such as carbon dioxide. Compared to other muscles in the body, the heart consumes a high amount of nutrients and oxygen. It pumps blood to itself through specialized vessels called coronary arteries. These arteries are critical to the integrity of the functioning of the heart. We know that diabetes can cause harm to these vessels, called coronary artery disease. This disease can be in the form of thickening of the vessels that can cause decreased blood flow through the vessel or the formation of fatty material, commonly referred to as a plaque, that blocks the flow of blood through the vessel. Both of these conditions can lead to a decreased or arrested blood flow to the heart, which will cause severe impairment to this pumping muscle. This is referred to as a myocardial infarction, or heart attack.
Similar problems can occur in larger vessels in the body, such as those leading to your arms and legs. Problems such as these are classified as peripheral vascular disease. With this condition, the blood vessels leading to the arms and legs can be impaired by thickening of the walls of the vessels or development of fatty plaque on the inside of the vessels. Peripheral vascular disease can lead to decreased blood flow to the limbs, causing pain and changes in the tissues. This tissue damage can lead to infections. Pain is a common complaint when the blood flow is decreased to most tissues in the body. Sometimes this will occur during activities when the muscles require increased oxygen. For instance, you may have vascular disease, causing a decreased blood flow to your extremities. When you are at rest you may not have pain because the flow is good enough for muscles to function. But when you start walking, activating your muscles, the oxygen demand is greater than the flow of blood allows, causing pain in the leg muscles. If you develop any problems like this, your doctor will order a test to assess the blood flow in your vessels in the affected limb. This is typically done with a machine that uses ultrasonic waves to measure flow in a blood vessel. Other tests can measure the amount of oxygen in the blood that is flowing, which can provide information helpful to determining the health of the limb.
The results can be devastating when the vessels that are diseased are in the brain. The brain requires oxygen at all times. Even a short period of oxygen deprivation can cause significant damage, which is often irreversible. This condition is commonly referred to as a stroke, or a cerebrovascular accident. The carotid arteries in the neck that supply your brain with oxygenated blood can become diseased (called carotid artery disease) thus decreasing blood flow, which can result in a stroke. If your physician suspects you may be at risk for a stroke, he may order an ultrasound test similar to that used to assess blood flow in the arms or legs.
It is well known that all people with diabetes have an increased risk of infections. This risk is further increased with the presence of vascular disease. The body’s immune system consists of specialized cells that identify and destroy invading organisms. But when the blood flow that carries these cells to their destination is decreased, the ability of the cells to function normally is also decreased, leading to increased rates of infection.
Diabetes and Your Nervous System
In people with diabetes, the nervous system can be affected in many ways, causing multiple problems termed neuropathy. These problems can include numbness of sensation, increased pain sensation, decreased muscle control and function, and difficulty with control of other organs such as the bladder and bowel. There can also be significant problems with neurological control of the heart and blood vessels, which can lead to abnormal heart rhythms and significant fluctuations in blood pressure.
Those with diabetes who have decreased sensation can develop problems relating to the inability to sense pressure pain. For instance, if the soles of your feet do not sense pressure well, it will be difficult for you to know whether or not your shoe fits well. Therefore, when there is a specific pressure point on a part of your foot that you cannot feel, it will lead to significant breakdown of the skin, causing an ulcer that can become infected. This condition is called peripheral neuropathy; it is theorized that is directly caused by the by-products of hyperglycemia.
A decrease in sensation can also lead to a significant breakdown of joints, which in turn can lead to fractures and deformities. For example, if you moved a certain way that caused pain in your foot, you would investigate the cause and come up with the solution to stop the pain. But if you don’t have the ability to sense this pain (the body’s early warning system), you won’t notice the damage until a visible change occurs. Such a change may be anything from swelling and redness to a drop in your arch, causing a large deformity of your foot. Foot care is very important for all people with diabetes. Your doctor can order a test called an electromyelogram (EMG) to look at your peripheral nerve function and health.
Damage to the nerves that control certain body parts can occur, resulting in dysfunction of the specific areas. This is referred to as autonomic neuropathy. These areas can include organs such as muscles, heart, blood vessels, stomach, intestine, and bladder. For example, if the nerves to your hand muscles were damaged, you may notice that you have decreased ability to manipulate small objects such as writing utensils. Similarly, if the nerves that control gastric motility (which is required for normal food digestion) are damaged, you may experience symptoms ranging from nausea and vomiting to constipation or diarrhea.
Furthermore, if the nervous system’s interaction with the blood vessels is disrupted, this can result in the inability to control your blood pressure. The body’s blood pressure normally is lower while lying or sitting than when standing. The nervous system helps increase the blood pressure when we go to the standing position. If your nervous system is impaired from diabetes, you may notice symptoms such as light-headedness, dizziness, or even loss of consciousness when you attempt to go from a lying or sitting position to a standing position. More importantly, normal autonomic nerve function is critical to exercising safely. I will discuss this more in chapter 4.
Caring for Your Feet
Foot problems are common in those with diabetes because uncontrolled diabetes can cause poor circulation, leading to nerve damage. You need to start caring for your feet as soon as possible to prevent or significantly delay many foot problems. Not making foot care a priority only puts you at greater risk for serious problems, including amputation. If you currently have foot problems, you should see a doctor experienced in foot care, such as a podiatrist, to ensure that you are incorporating the best care possible for your feet.
Foot Exams
Your action plan should include daily foot exams. As with all planning, try to find a time of day when you will most likely have the time and will remember to do this task. Many people find it easiest to do their foot checks just after getting ready for bed. You, or someone else if you are unable, will need to carefully inspect your feet. If you are doing this for yourself, then it will be helpful to use a mirror to look at those areas that are difficult to see.
When looking at your feet, be sure that you have adequate lighting so that you don’t miss anything. Find a safe place to sit while doing the inspecting. Your goal during these sessions is to detect any evidence of skin lesions such as sores, scratches or cuts, swollen or red areas, calluses, corns, or any problem with your nails (such as ingrown or infected toenails). Look at all parts of your feet from the ankle down, including between each toe. Remember that you may not be able to feel some of the subtle pain that is typically associated with these foot problems. Report all cuts and scratches that do not start healing after 24 hours of discovery, or any painful, red, or warm areas to your physician immediately.
Foot Hygiene
Good hygiene is important in preventing foot problems. You should wash your feet each day. You may want to get a foot tub to clean your feet before you start the inspection process. Use warm (90 to 95 degrees Fahrenheit) rather than hot water, and use nondrying soap to clean your feet thoroughly. Do not soak your feet in water because this can wash away essential skin oils that give your feet natural protection. Dry skin will crack, and any openings in the skin can let bacteria and viruses in, causing infection. When you are finished washing your feet, rinse the soap off and thoroughly dry your feet with a clean and dry towel, being sure to dry between each toe. To ensure that your skin does not become overdry, apply a moisturizing cream or lotion to the tops and soles of your feet, gently rubbing it in and avoiding the areas between your toes. Lotion between your toes can lead to excessive moisture and cause the skin to break down, which may lead to an infection. Many people use talcum power to ensure that the areas between the toes stay dry.
After washing and inspecting your feet, trim your nails straight across to ensure that the edges do not become ingrown in the sides of the toes. If your nails are thick, you should have a podiatrist trim them for you. Before taking care of any corns or calluses (excess thick skin often found on the heel area), ask your podiatrist how you can do this at home. Using a pumice stone while your skin is still moist is helpful to gently smooth excess skin on your heels as well as calluses and corns. Avoid using over-the-counter chemical products to treat your calluses or corns, or using sharp instruments such as scissors, scalpels, or razor blades unless instructed by your doctor. These types of treatments may damage your skin, which can lead to infection.
If you find that you have calluses or corns on your heels and toes, this may be evidence of improper footwear. It is very important that your socks and shoes fit your feet well. Socks without thick seams or those that are seamless are better for your feet. Shoes that offer a wide toe box, smooth liners, good support, and breathable materials will be best for your feet. Vinyl and plastic are not good materials for shoes because they do not allow your feet to breathe. Furthermore, you should not wear shoes without socks because they will allow your foot to sweat and become too moist, which can lead to skin breakdown. Your socks offer extra protection from friction that your skin encounters inside a shoe, which will prevent blisters and cuts. Because of the increased risk of cuts, you should avoid going barefoot, especially in places where there may be broken glass such as in parks or at the beach.
Foot Care Basics
• Start your foot care plan now and make it a priority.
• Be sure to conduct a daily foot check.
• Have someone else check your feet if you are unable to do so yourself.
• Use a mirror to help you see those areas that are difficult to see.
• Check your feet in a well-lit room to make sure you can see any potential problems.
• Look for sores, scratches or cuts, swollen or red areas, calluses, and corn or nail problems.
• Remember to look between your toes.
• Tell your physician about all cuts that do not start to heal within 24 hours and all painful, red, or warm areas.
• Wash your feet every day with warm water and a nondrying soap.
• Do not soak your feet in water.
• Use a moisturizing cream or lotion on your feet. Avoid putting lotion between the toes.
• Trim your nails straight across to avoid ingrown nails.
• Always wear socks with shoes.
• Choose shoes with a wide toe box, smooth liners, good support, and breathable materials (cotton or leather).
• Avoid going barefoot.
• Protect your feet from excessive heat and cold.
• Don’t smoke.
Foot Protection
Protect your feet from the heat and the cold. Allowing your feet to become cold will decrease the sensation in them. In cold climates, wear thicker socks and shoes or boots that are lined with soft insulation. In addition, good blood circulation is important in keeping your feet warm. Avoid wearing tight socks or shoes and crossing your legs or standing in one place for extended periods. Especially avoid smoking tobacco because it decreases blood flow, resulting in cold feet. Protecting your feet from heat is just as important as protecting them from the cold. Avoid walking barefoot on heated surfaces such as hot asphalt or concrete. And remember to protect your skin by using sunscreen on your feet as well as on other exposed areas when you’re in the sun.
Being proactive by doing foot checks before you encounter a problem is the most important part of good foot care. Talk with your health care team after you come up with a plan for the care of your feet to ensure that you have covered all of your bases. To find more information on foot care, visit www.ndep.nih.gov (a Web site of the National Institutes of Health) and www.diabetes.org (a Web site of the American Diabetes Association), or do a search online for diabetic foot care.
Glucose Control
I realize that you may be very uneasy after reading this chapter. Do all people with diabetes get all of these problems? The simple answer is no. However, you are at greater risk of having these complications. I think the better question would be whether you can prevent diabetes from causing these problems. The scientific data suggest that with good glucose control, most if not all of these complications can be prevented or minimized. For some, glucose control may be as easy as starting an exercise program. But some of you may require initiation in an exercise program, diet modifications, and medications under the close supervision of your physician. No matter where you fall in the range of patients, you can develop an action plan to control your glucose.
Action Plan:
Making Glucose Control Your Goal
• Understand the effects of diabetes on various bodily systems:
• Vision
• Kidneys
• Cardiovascular system
• Nervous system
• Listen to your body and talk to your doctor about any suspicions you may have in any of these areas.
• Make it your goal to control your glucose as a means of preventing further health problems.
• Remember that good foot care can prevent significant health problems.