CHAPTER 6
Remember the Activators!: The Fat-Soluble Vitamins A, D and K2
Many empty calories that Americans eat come from foods and beverages that provide calories but few nutrients—such as desserts, sodas, and candies.” This statement appeared in 2016 at choosemyplate.gov, the USDA website dedicated to promoting the principles of the U.S. dietary guidelines.
On the surface it’s a statement we can all agree with—but then the “solid fats” are slipped in. “A great way to help you manage your body weight is to eat fewer empty calories. Empty calories are calories from solid fats, added sugars, or both… Added sugars and fats load these choices with extra calories you don’t need. Some foods and beverages provide essential nutrients, but may also contain some empty calories. For example, a cup of whole milk contains about 150 calories, with over 60 of them empty calories from fat. Fat-free milk has the same amount of calcium and other nutrients as whole milk, but with less than 90 calories and no fat or empty calories.”
Here’s how the guidelines define solid fats: “Solid fats are fats that are solid at room temperature, like beef fat, butter, and shortening. Solid fats mainly come from animal foods and can also be made from vegetable oils through a process called hydrogenation.” Along with a picture of butter on a plate, the website lists the following as empty, solid fats: butter, milk fat, beef fat (tallow, suet), chicken fat, cream, pork fat (lard), stick margarine, shortening, hydrogenated and partially hydrogenated oils, coconut oil, palm and palm kernel oils.*
Thus “solid fats” containing trans fats and made from vegetable oils—which are rightly condemned—get lumped in with “solid fats” from animal sources, like butter and lard; and healthy, natural whole milk gets lumped with sugary sweets.
The guidelines continue: “Besides contributing to weight gain… Animal products containing solid fats also contain cholesterol. Saturated fats and trans fats tend to raise “bad” (LDL) cholesterol levels in the blood. This, in turn increases the risk for heart disease. To lower risk for heart disease, cut back on foods containing saturated fats and trans fats.” Thus, according to official dogma, solid fats, no matter where they come from, contribute to obesity and heart disease.
But there is only one way officials can declare that animal fats are “empty” fats—by turning their backs on decades of scientific research into the important vitamins and other nutrients found uniquely in animal fats, including the fats in whole milk.
THE FORTUNES OF VITAMINS GO up and down. If there were a vitamin hit parade, vitamin A would be somewhere near the bottom today, maligned and misunderstood, but during the early 1900s, it stood at the top.
The discovery of vitamin A, and the history of its application in human nutrition, together represent a marriage of scientific inquiry at its best with worldwide cultural traditions. A key player in this fascinating story is the dentist, Weston A. Price, who traveled the world in the 1930s and 1940s to study healthy indigenous cultures. He discovered that the diets of healthy traditional peoples contained at least ten times more fat-soluble vitamins—vitamins found uniquely in animal foods—than the American diet of his day. His work revealed vitamin A as one of several “fat-soluble activators” present only in the fats and organ meats of land and sea animals, and necessary for the assimilation of minerals in the diet. Price noted that the foods held sacred by the peoples he studied, such as spring butter, fish eggs, seal fat and shark liver, were exceptionally rich in vitamin A. It is this same, essential vitamin A that exists in the butter fat in “empty, calorie-rich” whole milk, which ensures all the minerals in the milk are absorbed—nature doesn’t make mistakes.
Government agencies claim that fruits and vegetables contain vitamin A, but in fact only animal foods supply true vitamin A. The best sources include butter, cream and cheese from cows eating green grass, liver from various animals, egg yolks from chickens raised on pasture, and a number of seafoods, such as fish eggs and especially fish liver oil—all fatty animal foods and most of them rich in “solid fats.”
Vitamin A gets its proper name, retinol, from the role it plays in supporting vision in the retina. Many traditional cultures recognized the fact that certain foods could prevent blindness. In his pioneering work, Nutrition and Physical Degeneration, Dr. Price tells the story of a prospector who, while crossing a high plateau in the Rocky Mountains, went blind with xerophthalmia, due to a lack of vitamin A. As the man wept in despair, he was discovered by an American Indian, who caught a trout and gave him “the flesh of the head and the tissues back of the eyes, including the eyes.”1 Within a few hours the prospector’s sight began to return and within two days his vision was nearly normal.
Several years previous to the travels of Weston A. Price, scientists had discovered that the richest source of vitamin A in the entire animal body is that of the retina and the tissues in back of the eyes. Many cultures used liver, another excellent source of vitamin A, to prevent and treat various types of blindness.2 The Egyptians described a cure at least thirty-five hundred years ago: liver was first pressed to the eye and then eaten, a ritual through which the patient directed the healing powers of liver to the afflicted sense organ. Similar practices have been described in eighteenth-century Russia, rural Java in 1978 and among the inhabitants of Newfoundland in 1929. Other cultures used shark liver. Hippocrates (460–327 BC) prescribed liver soaked in honey for blindness in malnourished children. Assyrian texts dating from 700 BC and Chinese medical writings from the seventh century AD both call for the use of liver in the treatment of night blindness. A twelfth-century Hebrew treatise recommends pressing goat liver to the eyes and then eating it.
During the era of exploration and trade using sailing vessels, night blindness was a recurring problem among sailors on long voyages—by the advent of the great European navies, most people had forgotten the wisdom of traditional liver therapy. It took brave dedication to the scientific method to confirm the validity of the ancient treatments. The first to do this was Eduard Schwarz (1831–1862), a ship’s doctor on an Austrian frigate that was sent around the world for scientific exploration. Before the voyage, several physicians had asked Schwarz to test the old folk remedy of using boiled ox liver to combat night blindness. On the voyage, seventy-five of the three hundred fifty-two men developed the condition. Every evening when dusk came, they lost their vision and had to be led about like the blind. Schwarz fed them ox or pork liver, which restored the night vision of every sailor afflicted.
The cure was “a true miracle,” said Schwarz in his published report, which stated emphatically that night blindness was a nutritional disease. For this he came under vicious attack by the medical profession, which accused him of “frivolity” and “self-aggrandizement.” Three years after his return from the expedition, the discredited physician died of TB. He was thirty-one. The use of vitamin-A-rich foods for tuberculosis lay in the future.
In 1904, the Japanese physician M. Mori described xerophthalmia in undernourished children whose diet consisted of rice, barley, cereals “and other vegetables.” Xerophthalmia is a condition that progresses from night blindness to dissolution of the cornea and finally bursting of the eye. He treated the children using liver and cod liver oil, with excellent results. In fact, he found that cod liver oil was even more effective than liver in restoring visual function. Mori described it as “an excellent, almost specific medication… Indeed, in most cases, the effect is so rapid that by evening the children with night blindness are already dancing around briskly, to the joy of their mothers.” Cod liver oil also helped reverse keratomalacia, a condition associated with severe nutritional deficiencies and characterized by corneal ulceration, extreme dryness of the eyes and infection.
At the end of the First World War, a physician named Bloch discovered that a diet containing whole milk, butter, eggs and cod liver oil cured night blindness and keratomalacia. In one important experiment, Bloch compared the results when he fed one group of children whole milk and the other margarine as their only fat. Half of the margarine-fed children developed corneal problems while the children receiving whole milk remained healthy.
The actual discovery of vitamin A is credited to a researcher named Elmer V. McCollum. He was curious why cows fed wheat did not thrive, became blind and gave birth to dead calves, while those fed yellow corn had no health problems. The year was 1907, and by this time, scientists were able to determine the levels of protein, carbohydrate, fat and minerals in food. The wheat and corn used in McCollum’s experiments contained equal levels of minerals and macronutrients. McCollum wondered whether the wheat contained a toxic substance, or whether there was something lacking in the wheat that was present in yellow maize.
In order to solve the puzzle, McCollum hit upon the idea of using small animals like mice or rats rather than cows for nutrition experiments—rats ate less, took up less space, reproduced rapidly and could be given controlled diets. Like many good ideas, this one met with considerable opposition. McCollum worked for the Wisconsin College of Agriculture, whose dean ordered him “to experiment with economically valuable animals—the rat was a pest to farmers!” But McCollum worked secretly in the basement of the Agriculture Hall, where he studied the effects of various diets on colonies of rats. He discovered that rats fed pure protein, pure skim milk, sugar, minerals and lard or olive oil for fat failed to grow. When he added butterfat or an extract of egg yolk to their diets, their health was restored. He discovered a fat-soluble factor in certain foods that was essential for growth and survival, which he called “fat-soluble factor A” as opposed to other accessory dietary factors, called “water-soluble B.”
Research by Osborne and Mendel, published just five months after McCollum’s study, found that cod liver oil produced the same results as butter in rat studies, thus confirming the early work of Mori in Japan. Continued experiments helped scientists determine that “fat-soluble factor A,” or vitamin A, is colorless, but often present in foods containing beta-carotene, which is yellow. In the 1930s, researchers determined that colorless vitamin A is formed by the conversion of yellow beta-carotenes in the intestinal mucosa of animals and humans.
A number of brilliant scientists labored to elucidate the role of vitamin A in vision, beginning in 1877 with a German, W. Kuhne, who discovered that the purple retinas from dark-adapted frogs turned yellow when exposed to light. The purple color is then restored in a complex biochemical cycle involving vitamin A, and it is this process that makes vision possible. Other scientists demonstrated the role of vitamin A in cell differentiation, bone development, reproduction, hormone production and immune system function.
Due to the outstanding scientific work of these and many other researchers, the administration of cod liver oil to growing children—a tradition found among Arctic peoples such as the Scandinavians and Eskimos—became standard practice until after the Second World War. We can credit the widespread use of cod liver oil—given to reluctant children in schools, in refugee camps, at doctors’ offices and even at Sunday school—to the decline in deaths and side effects from measles. Early advertisements for cod liver oil recognized its role in supporting robust growth, strong teeth and strong bones in children, as well as in protecting them against infectious disease.
Ironically, while Americans have stopped giving cod liver oil to their children, or even feeding them butter, whole milk and eggs, programs to administer vitamin A to children in Africa and Asia have had astonishing success in preventing blindness and infectious disease. This vitamin A treatment program was the brainchild of Alfred Sommer, an ophthalmologist at Johns Hopkins University, whose work on vitamin A in the 1970s and 1980s, which showed wonderful effects of vitamin A supplementation in Indonesia and Nepal, led him to lobby for an international supplementation program.
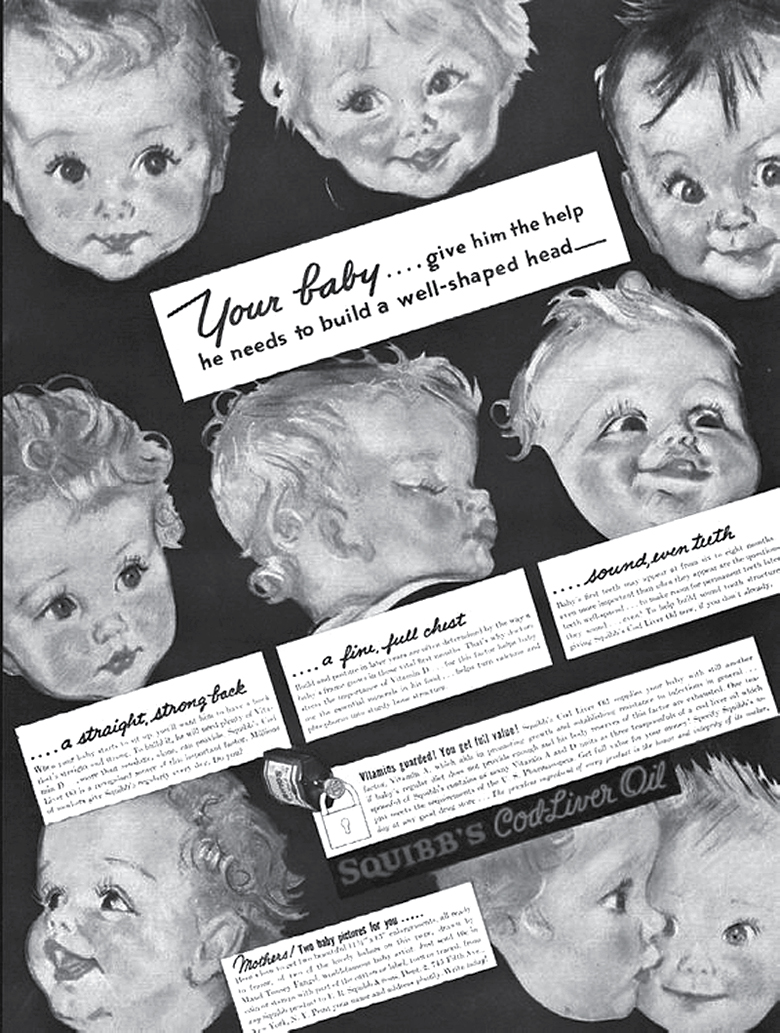
Ad for Squibb’s cod liver oil: “Your baby… give him the help he needs to build a well-shaped head—a straight, strong back… a fine, full chest… sound, even teeth… daily use is important.” Until after the Second World War, the medical profession recognized the importance of vitamin A in cod liver oil for optimal growth and development.
In recent decades, much vitamin A research has focused on its role in preventing cancer, and its use in combination with nontoxic therapies in the treatment of cancer. Unfortunately, few if any practicing oncologists today recognize the anticarcinogenic properties of vitamin A. Perhaps the most tragic example is Dr. Max Gerson, who treated many cases of terminal cancer with excellent results using raw liver juice, a rich source of vitamin A. In 1946, he testified before a U.S. congressional committee on the success of his treatment, but it was subsequently ignored.3 In 1973, Dr. Kanematsu Sugiura of the Sloan Kettering Institute published the results of studies on mammary tumors in mice using high doses of vitamin A and a derivative of apricot seeds called laetrile. He observed complete regression of all the tumors in a total of five mice. The final report noted that “Dr. Sugiura has never observed complete regression of these tumors in all his cosmic experience with other chemotherapeutic agents.” Nevertheless, just a few months later, spokesmen for Sloan Kettering flatly denied any value in the therapy.4
While the ongoing research into vitamin A and its effects is a boon to children and adults throughout the world, modern food processing conglomerates do not act on this knowledge. The food processing industry would rather use cheap vegetable oils than expensive animal fats. Some vegetable oils contain carotenes, but they do not contain true vitamin A. Yet healthy eating advocates continue to demonize natural “solid fat” sources of vitamin A, ignoring our cultural history and scientific understanding of its benefits.
UNFORTUNATELY, THE VAST MAJORITY OF popular books on nutrition insist that humans can obtain vitamin A from fruits and vegetables. Even worse, FDA regulations allow food processors to label carotenes as vitamin A. Just look at any can of tomatoes—the label clearly says it contains vitamin A, even though the only source of true vitamin A in the tomatoes comes from microscopic insect parts. The food industry, and the low-fat school of nutrition that the industry has spawned, benefit greatly from the fact that the public has only vague notions about vitamin A and where it occurs naturally.
Under optimal conditions, humans can indeed convert carotenes to vitamin A. This biochemical process occurs in the upper intestinal tract by the action of bile salts and fat-splitting enzymes. Of the entire family of carotenes, beta-carotene, found in carrots and many other fruits and vegetables, is most easily converted. Early studies indicated an equivalency of four to one of beta-carotene to retinol. In other words, four units of beta-carotene were needed to produce one unit of vitamin A. This ratio was later revised to six to one, and recent research suggests an even higher ratio.5 This means that you have to eat an awful lot of vegetables and fruits to obtain even the daily minimal requirements of vitamin A, assuming optimal conversion.
But the transformation of carotene to vitamin A is rarely optimal. Diabetics and those with poor thyroid function, a group that could well include at least half the adult U.S. population, cannot make the conversion. Children make the conversion very poorly and infants not at all—they must obtain their precious stores of vitamin A from animal fats6—yet today a low-fat diet is recommended for children. Strenuous physical exercise, excessive consumption of alcohol, excessive consumption of iron (especially from “fortified” white flour and breakfast cereal), use of a number of popular drugs, excessive consumption of polyunsaturated fatty acids, zinc deficiency and even cold weather can hinder the conversion of carotenes to vitamin A,7 as does the low-fat diet.
Carotenes are converted by the action of bile salts, and very little bile reaches the intestine when a meal is low in fat. The epicure who puts butter on his vegetables and adds cream to his vegetable soup is wiser than he knows. Butterfat stimulates the secretion of bile needed to convert carotenes into vitamin A, and at the same time supplies easily absorbed true vitamin A. Polyunsaturated oils also stimulate the secretion of bile salts but may cause rapid destruction of easily oxidized carotenes.8
Humans can only obtain sufficient, usable vitamin A from the fats and organ meats of land and sea animals. Depending on carotenes for vitamin A forces the body to call on large reserves of enzymes to make the conversion. In their fascinating book Nutrition and Evolution, Michael Crawford and David Marsh note that in animals, “If any function can be delegated to another organism it leaves the disk space free to perform some new function or to perform an old one better.” For example, cats do not synthesize vitamin A from carotenes. “If they had to synthesize their own vitamin A… it would take up a significant amount of their disk space.”9 Cats get vitamin A from their prey, whose ability to synthesize vitamin A from carotenes compromises other functions, such as night vision and quickness of movement. While medical orthodoxy claims that consumption of large amounts of carotenes has no downside, it is possible that dependence on carotenes for vitamin A, even in those who are good converters, compromises other biochemical functions in subtle ways.*
Studies led by the Agricultural Research Service during the past five years have found significant differences in beta-carotene uptake and conversion by physically similar volunteers. About half of the forty-five volunteers participating in one study didn’t take up much beta-carotene at all, and about half of the volunteers didn’t form much vitamin A from the beta-carotene they did absorb.10 Similar results were obtained by researchers at the USDA Western Human Nutrition Research Center, who found that only about half those studied converted significant amounts of beta-carotene.11 They also noted that the vitamin A activity of beta-carotene is surprisingly low in women.
The enzyme responsible for the conversion of beta-carotene to vitamin A is called beta-carotene 15, 15’-monoxgenase (BCOM1). Scientists from Newcastle University have found that almost 50 percent of females have a genetic variation that reduces greatly levels of BCOM and their ability to convert beta-carotene. “Vitamin A is incredibly important,” notes Dr. Georg Lietz, who participated in the study. “It boosts our immune system and reduces the risk of inflammation such as that associated with chest infections. What our research shows is that many women are simply not getting enough of this vital nutrient because their bodies are not able to convert the beta-carotene… Worryingly, younger women are at particular risk,” said Leitz. “The older generations tend to eat more eggs, milk and liver, which are naturally rich in vitamin A, whereas the health-conscious youngsters on low-fat diets are relying heavily on the beta-carotene form of the nutrient.”12
Carotenes from plant foods not only fail to meet our requirements for vitamin A, but may also reduce the effectiveness of true vitamin A. A team of researchers from Ohio State University has found that beta-carotene molecules can block certain actions of the true vitamin A.13 According to head researcher Earl Harrison, “These materials definitely have anti-vitamin-A properties, and they could basically disrupt or at least affect the whole body metabolism and action of vitamin A.” The discovery could explain why previous clinical trials have found that people who supplemented with beta-carotene had a higher incidence of lung cancer than participants who took no beta-carotene.14 Because vitamin A provides its health benefits by activating hundreds of genes, compounds contained in beta-carotene supplements could lower the activity of vitamin A. Says Harrison, “Too much beta-carotene could paradoxically result in too little vitamin A.”15
IT IS THEREFORE VERY UNWISE to depend on plant sources for vitamin A. This vital nutrient is needed for so many key bodily functions: it supports the growth and repair of body tissues, it helps protect mucous membranes of the mouth, nose, throat and lungs; it prompts the secretion of gastric juices necessary for proper digestion of protein; it helps build strong bones and teeth and supports the formation of rich blood; it is essential for good eyesight; it aids in the production of RNA; and contributes to the health of the immune system. Your health is at risk if you’re not getting enough.
Vitamin A is also involved in the conversion of cholesterol into sex hormones—estrogen, testosterone, progesterone, DHEA and many others.16 Without it, expect infertility, erectile dysfunction and problems of endocrine disruption, such as fibroid tumors and endometriosis. In one study, vitamin A and iron given to boys of short stature was just as effective as testosterone supplements in inducing growth.17 Various adrenal hormones that regulate the uptake of minerals, blood pressure and blood sugar levels also require vitamin A, as do the corticoid hormones that we need for healing and dealing with stress.18 Without plentiful vitamin A in the diet, we cannot heal properly; instead we must resort to alternatives like synthetic steroids, such as prednisone—with all their side effects—to resolve inflammation and manage pain. When we are under stress, we need even more vitamin A, and when vitamin A is lacking, every little thing can be stressful. The “solid,” vitamin A–containing saturated fats in butter support the efficient conversion of cholesterol into these vital hormones.
Vitamin A stores can rapidly deplete during exercise, fever, exposure to cold and periods of stress.19 Vitamin A is especially important for expectant mothers. Deficiency during pregnancy can result in offspring with eye defects, displaced kidneys, harelip, cleft palate and abnormalities of the heart and larger blood vessels.
Foods high in vitamin A are especially important for diabetics and those suffering from thyroid conditions. In fact, the thyroid gland requires more vitamin A than any of the other glands, and cannot form thyroid hormones without it.20 A diet rich in vitamin A will help prevent diabetes, and will protect those with diabetes from degenerative conditions associated with the disease, such as difficulty healing and deterioration of the retina and kidneys.21
Weston A. Price considered the fat-soluble vitamins, especially vitamin A, to be the catalysts on which all other biological processes depend.22 Efficient mineral uptake and utilization of water-soluble vitamins require sufficient vitamin A in the diet. Vitamin A supports the assimilation of iron, for example, and helps prevent anemia.23 Price’s research demonstrated that generous amounts of vitamin A ensure healthy reproduction and offspring with attractive wide faces, straight teeth and strong sturdy bodies. He discovered that healthy nonindustrialized peoples especially valued vitamin A–rich foods for growing children and pregnant mothers. The tenfold disparity that Price discovered between primitive diets and the American diet in the 1940s is almost certainly greater today, as Americans have forsworn butter and cod liver oil for empty, processed polyunsaturates.
Vitamin A deficiencies are widespread in Third World communities that have come into contact with the West. They contribute to high infant mortality, blindness, stunting, bone deformities and susceptibility to infection.24 These deficiencies occur even in communities that have access to plentiful carotenes in vegetables and fruits. As described by Price, a scarcity of good-quality dairy products, a rejection of organ meats as old-fashioned or unhealthful and a substitution of vegetable oil for animal fat in cooking all contribute to the physical degeneration and suffering in many developing nations that have adopted a Western diet high in processed foods.
Supplies of vitamin A are so vital to the body that humans are able to store large quantities of it in the liver and other organs. Thus it is possible for an adult to subsist on a fat-free diet for a considerable period of time before overt symptoms of deficiency appear. But during times of stress, vitamin A stores are rapidly depleted. Strenuous physical exercise, periods of physical growth, pregnancy, lactation and infection are stresses that quickly deplete vitamin A stores. Children with measles rapidly use up vitamin A, which can result in seizures or irreversible blindness.
Women need time to recover from the stress of pregnancy and to rebuild vitamin stores, especially stores of vitamin A. Dr. Price reported that throughout the South Seas and Africa, the villagers considered it shameful to have a child more than once every three years. This belief finds validation in modern science. In a study that gathered research from over two million pregnancies in eighteen different countries, researchers found that both mothers and their offspring had better health outcomes when births were spaced three to five years apart.25
One aspect of vitamin A that deserves more emphasis is its role in protein utilization. Ironically, high-protein, low-fat diets—the kind promoted by many modern diet gurus—are especially dangerous because protein consumption rapidly depletes vitamin A stores.26 Children brought up on high-protein, low-fat diets often experience rapid growth. The results—tall, myopic, lanky individuals with crowded teeth and poor posture, a kind of Ichabod Crane syndrome—are a fixture in America.27 Growing children actually benefit from a diet that contains considerably more calories from fat than from protein. A high-fat diet that is rich in vitamin A will result in steady, even growth, a sturdy physique and high immunity to illness.
High-protein, low-fat diets can even cause blindness, as occurred once in Guatemala where large amounts of instant nonfat dry milk were donated in a food relief program.*28 Many of the people who consumed the dried milk went blind from vitamin A depletion. Historically, cultures around the world instinctively understood the connection between vitamin A and protein, which is why they never ate lean meat and always consumed the organ meats of the animals that served them for food.29
The great discrepancy between what science has discovered about vitamin A and what nutrition writers promote in the popular press contributes to awkward moments. The New York Times has been a strong advocate for low-fat diets, even for children, yet a 1992 New York Times article on vitamin A noted that vitamin A–rich foods like liver, egg yolk, butter and cream confer resistance to infectious diseases in children and prevent cancer in adults.30 A 1994 Washington Post article hailed vitamin A as “cheap and effective, with wonders still being (re)discovered,” noting studies which found that vitamin A supplements help prevent infant mortality in Third World countries, protect measles victims from complications and prevent mother-to-child transmission of the HIV virus.31 The article lists butter, egg yolks and liver as important sources of vitamin A, but claims, unfortunately, that carotenes from vegetables are “equally important.”
Even worse than the claim that plant foods can provide vitamin A are warnings that vitamin A may be toxic in more than the minuscule RDA-recommended amounts. In fact, so great is the propaganda against the vitamin that obstetricians and pediatricians are now warning pregnant women to avoid foods containing vitamin A, like liver.
Recently an “expert” panel recommended lowering the RDA (recommended daily allowance) for vitamin A from 5,000 IU daily to about 2,500 IU and has set an upper limit of about 10,000 IUs for women. The panel was headed by Dr. Robert Russell of Tufts University, who warned that intake over the “upper limit” may cause irreversible liver damage and birth defects—a surprising statement in view of the fact that just a few decades ago pregnant women were routinely advised to take cod liver oil daily and eat liver at least one time per week. One tablespoon of cod liver oil contains at least 15,000 IU and one serving of liver can contain up to 40,000 IU vitamin A. Russell epitomizes the establishment view when he insists that vitamin A requirements can be met with one-half cup of carrots daily.32
The anti–vitamin A campaign for pregnant women began in 1995 with the publication of a Boston University School of Medicine study in the New England Journal of Medicine.33 “Teratogenicity of High Vitamin A Intake,” by Kenneth J. Rothman and his colleagues. The study correlates vitamin A consumption among more than twenty-two thousand pregnant women with birth defects occurring in subsequent offspring. The study received extensive press coverage in the same publications that had earlier extolled the benefits of vitamin A. “Study Links Excess Vitamin A and Birth Defects” by Jane Brody appeared on the front page of the New York Times on October 7, 1995; on November 24, 1995, the Washington Times reported: “High Doses of Vitamin A Linked to Babies’ Brain Defects.”
When a single study receives front-page coverage, it’s important to take a closer look, especially as earlier research points to the importance of vitamin A in preventing birth defects. In fact, the defects listed as increasing with increased vitamin A dosage—cleft lip, cleft palate, hydrocephalus and major heart malformations—are also defects of vitamin A deficiency.
In the study, researchers asked over twenty-two thousand women to respond to questionnaires about their eating habits and supplement intake before and during pregnancy. Food questionnaires are notoriously inaccurate, but their responses were used to determine vitamin A status. As reported in the newspapers, researchers found that cranial-neural-crest defects increased with increased dosages of vitamin A; what the papers did not report was the fact that in this study, neural tube defects decreased with increased vitamin A consumption, and that no trend was apparent with musculoskeletal, urogenital or other defects. The trend was much less pronounced, and less statistically significant, when cranial-neural-crest defects were correlated with vitamin A consumption from food alone.
The study is compromised by a number of flaws. Vitamin A status was assessed by the inaccurate method of recall and food questionnaires; and no blood tests were taken to determine the actual usable vitamin A status of the mothers. Researchers did not weight birth defects according to severity; thus we do not know whether the defects of babies born to mothers taking high doses of vitamin A were serious or minor compared to those of mothers taking lower amounts.
The most serious flaw was that researchers failed to distinguish between manufactured vitamin A in the form of retinol, found in supplements and added to fabricated foods, and natural vitamin A complex, present with numerous cofactors, from vitamin A–containing foods. Typically, synthetic vitamins are less biologically active, hence less effective, than naturally occurring vitamins. This is especially true of the fat-soluble vitamins like vitamin A, because these tend to be more complex molecules, with numerous double bonds and a multiplicity of forms. Natural vitamin A occurs as a mixture of various isomers, aldehydes, esters, acids and alcohols. Pure retinoic acid, a metabolite of vitamin A used to treat adult acne, is well known to cause birth defects.
The most serious problem with the Rothman study is the fact that it conflicts with other studies on vitamin A during pregnancy. A study carried out in Rome, Italy, found no congenital malformations among one hundred twenty infants exposed to more than 50,000 IU of vitamin A per day.34 A study from Switzerland looked at blood levels of vitamin A in pregnant women and found that a dose of 30,000 IU per day resulted in blood levels that had no association with birth defects.35
Warnings against vitamin A as a cause of birth defects are aimed at pregnant women; warnings that vitamin A is generally toxic are aimed at other adults. The following statement, posted at the University of Maryland Medical Center website, is typical of this orthodox medical view: “Vitamin A can be very toxic when taken in high-dose supplements for long periods of time and can affect almost every part of the body, including eyes, bones, blood, skin, central nervous system, liver, and genital and urinary tracts. Symptoms include dizziness, nausea, vomiting, headache, skin damage, mental disturbances and, in women, infrequent periods. Severe toxicity can cause blindness and may even be life-threatening. Liver damage can occur in children who take RDA-approved adult levels over prolonged periods of time or in adults who take as little as five times the RDA-approved amount for seven to ten years. In children, chronic overdose can cause fluid on the brain and other symptoms similar to those in adults… High consumption of vitamin A may also increase the risk of gastric cancer and the risk of osteoporosis and fractures in women.”36
The Merck Manual describes vitamin A toxicity in less hysterical terms. Acute vitamin A poisoning can occur in children after taking a single dose of synthetic vitamin A in the range of 300,000 IU or a daily dosage of 60,000 IU for a few weeks. Two fatalities have been reported from acute vitamin A poisoning in children, which manifests as increased intracranial pressure and vomiting. For the vast majority, however, recovery after discontinuation is “spontaneous, with no residual damage.”
In adults, according to the Merck Manual, vitamin A toxicity has been reported in Arctic explorers who developed drowsiness, irritability, headaches and vomiting, with subsequent peeling of the skin, within a few hours of ingesting several million units of vitamin A from polar bear or seal liver.* Again, these symptoms cleared up with discontinuation of the vitamin A–rich food. Other than this unusual example, however, only vitamin A from “megavitamin tablets containing vitamin A… when taken for a long time” has induced acute toxicity, that is, 100,000 IU synthetic vitamin A per day taken for many months.
Unless you are an Arctic explorer, it is virtually impossible to develop vitamin A toxicity from food. The putative toxic dose of 100,000 IU per day would be contained in three to six tablespoons of cod liver oil, two-and-one-half 100-gram servings of duck liver, about three 100-gram servings of beef liver, seven pounds of butter or three hundred nine egg yolks. Even synthetic vitamin A is not toxic when given as a single large dose or in small amounts on a daily basis. Children in impoverished areas of the world are routinely given two 100,000-unit doses of retinol per year for infants and two 200,000-unit doses for children over twelve months.
While scientists in America are creating confusion and fear about vitamin A, WHO and UNICEF vitamin A distribution programs in Africa and Asia have been extremely successful in reducing blindness and death among both children and adults. Vitamin A is more cost effective in saving lives and preventing suffering than immunizations and drugs, and it can be administered with two-cent capsules. The program does not undermine traditional cultures or foodways and is easily carried out on the village level. By some estimates, vitamin A supplementation programs in Third World countries save one million lives per year.37
The tragedy is that misplaced concern about vitamin A toxicity has led doctors to advise pregnant women to avoid foods containing vitamin A, and parents to avoid giving cod liver oil and liver to their babies. Yet early books on the dietary needs of pregnant women and infants recommended generous doses of cod liver oil and frequent liver consumption for pregnant women and two teaspoons of cod liver oil per day for babies three months and older.
Research on vitamin A is ongoing and the list of vitamin A miracles continues to grow: vitamin A supplements help children in Africa and Asia grow faster and attain better iron status; and vitamin A supplements have reduced the incidence of malaria in Papua New Guinea. Vitamin A plays a vital regulating role in the immune system; vitamin A deficiency leads to a loss of ciliated cells in the lung, an important first-line defense against pathogens; vitamin A promotes mucin secretion and microvilli formation by mucosa, including the gastrointestinal tract mucosa; vitamin A regulates T-cell production (needed for immunity) and apoptosis (programmed cell death).38
A study in Malawi, Africa, found that mothers with the highest levels of vitamin A had an HIV transmission rate of just 7.2 percent39; treatment with megadoses of vitamin A (100,000 IU per day) resulted in a 92 percent cure rate of menorrhagia (excessive menstrual bleeding) at Johannesburg General Hospital in South Africa40; vitamin A can be helpful in the treatment of psoriasis41; and in stroke victims, those with high levels of vitamin A (and E) are more likely to recover without damage.42
Vitamin A protects against lung and bladder cancers in men43; fourteen out of twenty patients with prostate cancer achieved total remission and five achieved partial remission using vitamin A as part of a natural cancer therapy in Germany44; vitamin A was used successfully to combat tropical ulcers in Uganda45; vitamin A has also been used successfully to treat a skin condition called Kyrle’s disease46; and elderly persons who consume adequate vitamin A are less prone to leg ulcers.47
The list continues: vitamin A inhibits the effects of phytic acid and increases absorption of iron from whole wheat (which is why it is a good idea to put butter on your bread)48; vitamin A supplementation increases absorption of iron and folic acid in women in Bangladesh49; use of vitamin A supplements reduces the risk of cataracts50; and a study of healthy centenarians found that these long-lived peoples were characterized by high levels of vitamins A and E in the bloodstream.51
In 2010, researchers discovered that vitamin A plays a role in the synthesis of ATP, the fuel in the mitochondria of our cells. When vitamin A is deficient, energy production reduces by 30 percent. “These results illuminate a hitherto unsuspected role of vitamin A in mitochondrial bioenergetics of mammals, acting as a nutritional sensor,” said the researchers. “As such, retinol is of fundamental importance for energy homeostasis. The data provide a mechanistic explanation to the nearly one-hundred-year-old question of why vitamin A deficiency causes so many pathologies that are independent of retinoic acid action.”52
Vitamin A not only supports good vision, but also good hearing. For example, a French study from as early as 1823 found that hearing levels were better among those who consumed the most vitamin A and also vitamin B12 from various foods, including red meat. A 1984 European study reported a five-to-fifteen-decibel improvement in patients with age-related hearing loss when given vitamins A and E. Other researchers reported that vitamin A deficiency results in a decline in the number of sensory cells in the nose, tongue and inner ear. A 1993 study reported in Science found that vitamin A can stimulate the regeneration of mammalian auditory hair cells. In 2009, Japanese researchers found that adults with the highest blood serum levels of vitamin A and carotenoids have the lowest risk for hearing loss. And, in 2014, researchers determined that vitamin A deficiency during pregnancy, especially during the early stages of fetal development, “may predispose offspring to inner ear malformations and sensorial hearing loss.”53
Vitamin A is critical for normal reproduction in both males and females. In vitamin A deficiency, the male reproductive organs develop pathological tissue and sperm don’t develop; and in severely vitamin A–deficient female rats, embryos do not form.54 Fertility clinics in the United States are filled with couples desperate to get pregnant. How many of them receive advice to consume a vitamin A–rich diet before trying more expensive and invasive measures?
Finally, vitamin A plays an important role in setting the body’s circadian rhythm and preventing insomnia. Light helps vitamin A bind to proteins in the rods and cones of the eye, thus allowing sight. It also helps vitamin A bind to a protein called melanopsin, needed for the conversion of serotonin to melatonin, the hormone that helps us get to sleep and sleep soundly throughout the night.55
As in America, British consumers get the same mixed messages about vitamin A. Researchers at Cardiff University looked at the effect of cod liver oil on cartilage health in thirty-one patients on a National Health Service waiting list for total knee joint replacement surgery. Half were given high-vitamin cod liver oil providing about 2,400 IU of vitamin A daily. At the time of surgery, samples of cartilage and joint tissue were taken from the knee joint and subjected to analysis. Markers for cartilage damage were significantly reduced in those taking cod liver oil. According to the researchers, “The data suggests that cod liver oil has a dual mode of action, potentially slowing down the cartilage degeneration inherent in osteoarthritis and also reducing factors that cause pain and inflammation.”56
Meanwhile, other British officials are warning against vitamin A overdose, claiming that vitamin A from foods like liver can weaken the bones. Surveys found that many Britons get “too much” vitamin A by eating liver. A single 100-gram serving of liver can contain up to 32,000 IU vitamin A, a dose that exceeds the puny 2,400 IU maximum recommended amount by as much as fifteenfold. Yet today we eat far less liver than in former times, and pregnant women were formerly encouraged to eat liver several times per week. The confusion has led health officials to consider whether to issue an advisory against eating liver to the general public—pregnant women already get warned by their doctors against eating this highly nutritious superfood.57
A frequent warning against vitamin A correlates vitamin A consumption with weak bones. Establishment nutritionists can indeed cite studies showing a connection between levels of vitamin A in the bloodstream and the risk of fractured bones. For example, a study of more than twenty-three hundred middle-aged Swedish men found that risk of any type of fracture was 64 percent higher in those with the most vitamin A in the blood. For hip fractures, the risk was increased by 147 percent.58 But the total number of fractures over thirty years was only two hundred sixty-six—about three fractures per thousand men per year—so the differences in fracture occurrence for various groups are actually very small. These figures may simply reflect the fact that people who consume lots of vitamin A are more physically active and more likely to end up in situations in which fractures occur—such as skiing. A study of more appropriate design looked at eighty healthy men ages eighteen to fifty-eight years who were randomly assigned to receive 25,000 IU per day of vitamin A or a placebo for six weeks. Compared with the placebo group, there was no significant change in the vitamin A group in various markers of bone formation and resorption.59 A 2005 study of elderly women found no evidence of any skeletal harm associated with vitamin A intake.60 In animal studies only enormous doses of vitamin A—equivalent to 7 million IU per day—induce bone disease, whereas amounts on the order of 100,000 IU per day do not affect bone health.
If there is a connection of vitamin A with poor bone health, the explanation lies in the fact that vitamins A and D work together—large doses of vitamin A in diets that provide little vitamin D can lead to further D deficiency with consequent effects on the bones. Fortunately, if you are eating nutrient-dense animal foods, you will be taking in both vitamins—A and D.
With so many miracles from vitamin A, one must question the motivation of those who pepper the Internet with warnings that vitamin A is toxic. Would a population nourishing itself on vitamin A–rich foods be filling hospital beds, populating lucrative nursing homes and swallowing dozens of pharmaceutical pills per day?
IN CONTRAST TO VITAMIN A, vitamin D today stands at the top of the vitamin hit parade, with many practitioners recommending large amounts of vitamin D from supplements—and offering few warnings about toxicity.
As vitamin A is associated with proper eyesight, so vitamin D is associated with bone health. Vitamin D—either from sunlight or food—plus adequate dietary calcium is necessary for prevention of rickets in children and osteomalacia (soft bones) in adults. Scientists consider overt rickets—with its characteristic symptom of bowed legs—a disease of the past in Western countries, solved with the addition of vitamin D to milk; however, subclinical rickets, characterized by easily fractured skull and bones, may be more common than realized, manifesting as shaken baby syndrome.61
American researchers Elmer V. McCollum and Marguerite Davis are credited with the discovery of vitamin D. In the early 1920s, the British doctor Edward Mellanby noticed that dogs fed cod liver oil did not develop rickets and thus concluded that vitamin A, or a closely associated factor, could prevent the disease. In 1922, McCollum took the study one step further, testing modified cod liver oil in which the vitamin A had been destroyed.62 The modified oil cured the sick dogs as well, so McCollum concluded the factor in cod liver oil that cured rickets was distinct from vitamin A. He called it vitamin D, the next letter in line after the discovery of vitamins A, B and C.
In 1925, researchers found that when a cholesterol precursor in the skin (7-dehydrocholesterol) is irradiated with light, a form of vitamin D is produced (now known as D3). Later researchers discovered that vitamin D has the structure of a sterol, very similar to cholesterol, with four ring structures, but with one of them opened.
In 1923, American biochemist Harry Steenbock at the University of Wisconsin demonstrated that irradiation by ultraviolet light increased the vitamin D content of foods and other organic materials. After irradiating rodent food, Steenbock discovered the rodents were cured of rickets. The form of vitamin D produced by irradiating yeast and other plant materials is D2.
In 1971–1972, scientists elucidated the further metabolism of vitamin D to its active forms. In the liver, vitamin D is converted to calcidiol, and calcidiol is then converted by the kidneys to calcitriol, the biologically active form of vitamin D. Since then, scientists have cataloged over nine hundred forms of vitamin D.63 Calcitriol circulates as a hormone in the blood, regulating the concentration of calcium and phosphate in the bloodstream and promoting—among many other roles—the healthy growth and remodeling of bone.
In addition to preventing rickets and osteomalacia, vitamin D seems to protect against many other conditions. These include hypocalcemia (low levels of calcium in the blood); convulsions, tetany and heart failure in newborns; osteoporosis and arthritis; heart disease and high blood pressure; cancer; chronic pain; depression and mental illness; muscular weakness; radiation poisoning; and diabetes and other autoimmune disorders. A systematic review of clinical studies shows a possible association between low vitamin D levels, cognitive impairment and a higher risk of developing Alzheimer’s disease.64 Deficiency has been linked to increased risk of viral infections, including HIV and influenza.65 Low levels of vitamin D in pregnancy are associated with gestational diabetes, preeclampsia and low-birth-weight babies.66
Researchers at the Harvard Medical School have discovered that low vitamin D is associated with an increased risk of heart disease. In one study, people with levels of vitamin D below 15 ng/ml had twice the risk of heart attack, heart failure and stroke compared to those with higher levels.67 German scientists have discovered that levels of the vitamin are up to 50 percent lower in the blood of patients with chronic heart failure.68 In adults, vitamin D leads to mood improvements and protects against depression.69 Vitamin D may protect against multiple sclerosis.70 And researchers at Harvard University’s School of Public Health found that low intakes of vitamin D were linked with the highest levels of lead accumulation in bones.71
Studies like these have propelled vitamin D to the top of the vitamin hit parade and generated enthusiasm among health-conscious consumers. But in reality, the world of vitamin D research is roiling in contradiction and controversy. For example, what is optimal daily vitamin D intake? Recommendations range from the conservative U.S. Institute of Medicine estimate of 200 IU per day for adults under fifty to amounts as high as 10,000 IU. Some leading vitamin D researchers recommend 3,000 to 4,000 IU per day as both necessary and safe.72 Is vitamin D relatively harmless, or “the most toxic of all vitamins” as some media outlets claim?73 And what is the optimal serum vitamin D level? Estimates range from 20 ng/ml (National Institutes of Health) to as high as 75 ng/ml.*74 Another question: what is the best way to get our vitamin D—sunlight, food or supplements?
And then there is the controversy regarding vitamin D2 or egosterol (made from irradiating yeast with ultraviolet light) versus vitamin D3 or cholecalciferol (the most common form, mostly found in animal fats). Most textbooks state that these two forms are equivalent. Vitamin D2 is much easier and less expensive to manufacture than D3, and the industry can indeed point to studies showing that it has biological effects. For example, a 2008 study showed that administration of vitamin D2 plus calcium to elderly patients resulted in a 23 percent reduction of the risk of falling.75 The industry can also point to a number of studies indicating that D2 is “just as easily absorbed”—just as able to raise serum levels—as D3. However, research shows that vitamin D3 is much more effective than vitamin D2 at raising levels of serum calcidiol—a much more active form of vitamin D.76
Synthetic vitamin D2 is not only less effective than D3, but it also may be potentially harmful. As early as 1937, scientists expressed concern about the possible toxicity of D2. In that year, Wayne Brehm presented before the Ohio State Medical Association the results of an experiment comparing the effects of the administration of cod liver oil with that of vitamin D2 to more than five hundred pregnant women. Vitamin D2, especially in conjunction with calcium, produced extensive abnormal calcification of the placenta, in one case extending into the uterine wall, and in three cases producing kidney stones within the developing fetus. Cod liver oil, by contrast, produced no more tissue calcification than seen in controls.77 From these experiments it would seem reasonable to conclude that vitamin D2 can cause toxic effects while vitamin D from cod liver oil is safe.*
Dr. E.W.H. Cruickshank’s 1951 book Food and Nutrition describes an important experiment with chicks. Three groups of chicks were fed the same diet. The first group received no vitamin D at all; the second group got D2; the third group received a natural vitamin D preparation made from cod liver oil. The chicks receiving no vitamin D gained 259 grams; those receiving the synthetic vitamin D2 gained 346 grams; and those that had the benefit of the natural vitamin D gained 399 grams. The most important finding was this: of the chicks receiving no vitamin D, 60 percent died; of the chicks receiving synthetic vitamin D, 50 percent died; while in the natural vitamin D group, no chicks died.
Giving D3 as a supplement (not as it naturally occurs in cod liver oil) can cause soft tissue calcification as well. An excess of vitamin D3 results in abnormally high blood concentrations of calcium, which can cause overcalcification of the bones and also of the soft tissues, such as the heart and kidneys. In addition, it can result in hypertension.78 Even overexposure to sunlight is associated with a condition linked to too much vitamin D: kidney stones.79 Other recent papers suggest additional dangers of taking vitamin D. For example, researchers found that vitamin D supplementation can inhibit gene expression and lead to autoimmune disease.80 “We have found that vitamin D supplementation, even at levels many consider desirable, interferes with recovery in these patients,” said J. C. Waterhouse, PhD, executive director of Autoimmunity Research, Inc. Another report blames brain lesions on vitamin D.81 A recent paper presented data indicating that the bioactivity of natural vitamin D in food is up to five times higher compared to vitamin D3 from supplements.†82
American research dating back to 1937 shows us that vitamin A protects us against vitamin D toxicity.83 Researchers fed rats various concentrations of vitamin A with toxic doses of vitamin D in various forms. The doses of vitamin D given to the animals were 4,000 IU per day or greater, which is the body-weight-adjusted equivalent of a typical human consuming over 5,000,000 IU per day. The researchers used both synthetic vitamin D2 and concentrates of the liver oils of tuna, cod, sea bass and halibut. Although vitamin D2 was most toxic, massive doses of all forms of vitamin D with only low doses of vitamin A decreased growth and bone mineralization and increased calcification of the lungs, heart and kidneys, while vitamin A consistently protected against these effects in proportion to its dose.
Subsequent research has shown that vitamin A provides protection against skeletal defects, bone demineralization and soft tissue calcification induced in rats by large amounts of both vitamin D2 and D3.84
It seems that vitamin D requires vitamin A in order to function, and that high doses of vitamin D cause toxicity by depleting vitamin A stores. In 2006, a team of researchers from Spain and Germany published a report showing that 9-cis-retinoic acid, one of the hormonally active forms of vitamin A, is an essential factor for the full functioning of vitamin D.85
Vitamin A protects against calcification, so if high doses of vitamin D use up vitamin A, that leaves less vitamin A for other important processes, such as preventing the calcification of the kidneys or arteries. Likewise, taking vitamin A without vitamin D will call on reserves of vitamin D, leading to weakening of the bones. This is another explanation for why studies from Scandinavia—where the “vitamin D winter,” the period when it is impossible to get vitamin D from sunlight, is long and where vitamin A is added to common foods like milk and cereal—show a correlation of vitamin A consumption and bone fractures.
The key takeaway is that we get vitamins A and D—two nutrients absolutely critical for good health—from high-fat animal foods. If we are eating a variety of these foods—egg yolks, animal fats and fatty fish for vitamin D, and butter, cream and organ meats for vitamin A—along with modest amounts of cod liver oil to ensure adequate supplies of both, we will have sufficient amounts and the right kind of balance to use vitamins A and D to the maximum effect and without side effects.
“HUMAN BRINGS CANNOT GET ADEQUATE vitamin D from food.” This is the assertion of the Vitamin D Council and similar groups who claim that we must get it either from sunlight, from vitamin D added to foods like milk or from supplements. This dogma begs the question of how our preindustrial ancestors obtained this critical nutrient during “vitamin D winters,” that is, periods of the year when the angle of the sun is too oblique for vitamin D production to occur, a period that lasts at least six months in temperate and Arctic zones. Even in warm months, humans like to cover themselves with clothing, and seek the shade or stay inside a dwelling during the hot part of the day. The fact is human beings have always obtained some, or even a large portion, of their vitamin D from food, or we would have died off long ago from vitamin D–deficiency diseases.
It is easy for proponents of vitamin D supplementation and fortification claim that we can’t get vitamin D from food, because food data tables in fact do not show much vitamin D in food. Typical values given in food composition databases are as follows:
Food: Cod liver oil
IU per 100 grams: 10,000 (500 per teaspoon)
Food: Oily fish
IU per 100 grams: 759
Food: Fortified cereals
IU per 100 grams: 333
Food: Egg yolks
IU per 100 grams: 218 (37 per yolk)
Food: Caviar
IU per 100 grams: 117
Food: Butter
IU per 100 grams: 136
Food: Cheese
IU per 100 grams: 110
Food: Lard
IU per 100 grams: 102
Food: Chicken liver
IU per 100 grams: 0
Source: U.S. Department of Agriculture Food Composition Databases
In 2015, the Weston A. Price Foundation had a number of foods tested for vitamin D content by two independent laboratories. One of the labs—which does considerable work for the USDA—gave very similar results (with results for some foods even lower), but the other lab gave significantly higher results:
Food: Cod liver oil
IU per 100 grams: 10,000–33,000 (500–5,500 per teaspoon)
Food: Conventional egg yolks
IU per 100 grams: 1,400 (77 per yolk)
Food: Organic egg yolks
IU per 100 grams: 2,300 (127 per yolk)
Food: Pastured egg yolks
IU per 100 grams: 2,700 (150 per yolk)
Food: Caviar
IU per 100 grams: 7,000–12,000
Food: Cheese
IU per 100 grams: 900–3,100
Food: Chicken liver
IU per 100 grams: 5–700
Food: Lard
IU per 100 grams: 0
Food: Butter
IU per 100 grams: 0
Using a different method, this same lab gave even higher—considerably higher—results on several food samples analyzed in 2009:
Food: Conventional egg yolks
IU per 100 grams: 9,240 (513 per yolk)
Food: Pastured egg yolks
IU per 100 grams: 69,560 (3,864 per yolk)
Food: Conventional lard
IU per 100 grams: 6,040 (857 per tablespoon)
Food: Pastured lard
IU per 100 grams: 74,560 (10,500 IU per tablespoon)
Food: Conventional butter
IU per 100 grams: 18,800 (2,667 per tablespoon)*
Food: Pastured butter
IU per 100 grams: 6,560 (930 per tablespoon)
Food: Caviar
IU per 100 grams: 116,480 (16,521 per tablespoon)
How could testing results be so different for the same foods? It turns out that vitamin D testing is very difficult. To get accurate results, the vitamin D must be extracted from the proteins or matrix in which it is bound, and different foods require different extraction methods; if the extraction is not performed with the right method, the resulting values may be low. Furthermore, the testing equipment often does not measure calcidiol, calcitriol and other forms of vitamin D and, if not calibrated correctly, will result in printout charts with overlapping peaks giving an underestimation of total vitamin D. For example, the type of vitamin D in butter is mostly the same type that is carried in the blood—calcidiol—and few if any labs specializing in measuring vitamin levels in food test for calcidiol.
Since government dogma insists that we can’t get vitamin D from food, we can’t discount the suspicion that lab certification organizations dictate testing procedures to give deliberately low results. What would happen if the public learned that egg yolks, especially egg yolks from pastured chickens, are powerhouses of vitamin D, or that just one tablespoon of lard could meet our vitamin D requirements better than dozens of capsules? Consumption of these foods would soar and sales of industrial substitutes would decline.
Several vitamin D researchers have expressed skepticism about the accuracy of laboratory tests for vitamin D. Esteemed vitamin D expert Hector DeLuca is especially outspoken in condemning laboratory analysis for determining the amount of active vitamin D in foods. Instead, these critics prefer the rat assay or “line” test, in which a vitamin D–containing substance is given to rats from which vitamin D has been withheld to induce rickets, and then after a fixed period, sacrificing the rats to ascertain the degree of healing in the bones. As early as 1929, these tests determined that cod liver oil had the highest antirachitic activity, followed by egg yolk from animals exposed to bright sunlight.† Most interesting, the early studies on vitamin D, which measured the antirachitic of various foods using the line test, found that butter and lard were both effective in curing rickets.86 This means that these foods carry a form of vitamin D, even though standard food tests find low or nonexistent levels.
TAKING COD LIVER OIL SEEMS old-fashioned, like something from another era. But modern scientific literature provides a surprising number of studies on this ancient superfood—our best source of vitamins A and D—and almost all of them are positive.
Cod liver oil seems particularly beneficial for rheumatoid arthritis. Cod liver oil supplements were better than controls in relieving arthritis pain87; cod liver oil allows reduction of nonsteroidal anti-inflammatory drug dosage and improves chief clinical symptoms, reducing pain and morning joint stiffness88; and use of cod liver oil decreased occurrence of morning stiffness, swollen joints and pain intensity in patients suffering from rheumatoid arthritis.89
For strong bones, cod liver oil protects against greater bone turnover, bone loss and obesity in winter months.90 One study found that cod liver oil supplementation was associated with a significantly lower risk of any fracture and no evidence to suggest any skeletal harm associated with increased vitamin A intake.91 Subjects in Norway with food consumption habits that included frequent mølje meals (consisting of cod liver and fresh cod liver oil) during the winter sustained satisfactory vitamin D levels in their blood, in spite of the long “vitamin D winter.”92
Diabetics can benefit from cod liver oil. Cod liver oil treatment in diabetic rats completely prevented endothelial deficiency and partly corrected several biochemical markers for cardiovascular disorders93; use of cod liver oil in mice played an important role in the prevention of diabetic nephropathy.94
Using data from the Norwegian Women and Cancer cohort study, researchers explored the relationship of supplement use and survival of cancer patients with solid tumors. They found that women who took cod liver oil were 44 percent less likely to die from cancer than those who did not take supplements. (Women who used supplements other than cod liver oil were 30 percent less likely to die.) Use of cod liver oil was also found associated with improved survival rates for patients with breast and colorectal cancer. Overall, consumption of cod liver oil for a year prior to diagnosis was associated with a 23 percent reduction in the risk of death in patients diagnosed with solid cancers.95
Cod liver oil offers excellent protection against coronary artery disease as well. One study looked at the effect of cod liver oil on the development and progression of coronary artery disease in swine.96 The animals were subjected to coronary balloon abrasion and fed an atherogenic diet for eight months. Analysis of coronary artery sections revealed significantly less disease in the animals fed cod liver oil compared to controls. Furthermore, blood markers for heart disease were significantly reduced in the cod liver oil–fed swine. Blood markers were similarly reduced in swine fed cod liver oil according to a subsequent study.97
Regular use of cod liver oil is associated with fewer symptoms of depression in the general population98—good news to the 10 percent of the population relying on antidepressants to manage the condition.
Pregnant women receive warnings against cod liver oil. But according to one study, women who used liquid cod liver oil in early pregnancy gave birth to heavier (and therefore more robust) babies, even after adjusting for the length of gestation and other confounding factors.99 Women using cod liver oil had significantly higher levels of docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) in their breast milk100 and maternal use of cod liver oil resulted in higher levels of fat-soluble vitamins in breast milk, especially vitamins E and A.101 Children born to mothers who took cod liver oil during pregnancy and lactation scored higher on intelligence tests at age four compared with children whose mothers took corn oil.102
Cod liver oil is especially important for growing children, as vitamins A and D work together to support healthy, growing bones. And there are many other benefits. Children supplemented with cod liver oil had a decrease in upper respiratory tract infections and pediatric visits over time.103 Use of cod liver oil in the first year of life was associated with a significantly lower risk of type 1 diabetes. Use of other vitamin D supplements during the first year of life and maternal use of cod liver oil or other vitamin D supplements during pregnancy were not associated with lower risk of type 1 diabetes.104 Children prone to earaches (otitis media) receiving cod liver oil plus selenium needed lower amounts of antibiotics during supplementation compared to before supplementation.105 In Arctic climates, supplemental cod liver oil during childhood may be protective against multiple sclerosis later in life.106 Reduced breast cancer risks were associated with increasing sun exposure and cod liver oil use from ages ten to nineteen.107
Newspaper articles on long-lived people usually credit “good genes,” as they did in a recent story on a family of eight brothers and sisters, ages seventy-nine to ninety-six, who have no history of heart attack, stroke, dementia or other diseases associated with getting old. Not one of them needs a cane. But is it good genes—or cod liver oil? “I don’t even remember having a medicine cabinet. No, we didn’t,” says Helen Hurlburt. “Just molasses on bread and cod liver oil. That’s about it,” says her sister Agnes. “We never had junk food. We always cooked, and we ate together in the evening,” says Helen.108 Miriam Tyler, of Timperley, UK, age one hundred, credits her longevity to “a spoonful of cod liver oil once a day, washed down with maluca honey.”109*
Cod liver oil plus real food starting in childhood and continuing into adulthood looks like the formula for optimal gene expression, meaning that we all have good genes, but often suboptimal expression of those genes due to poor nutrition.
IN 1945, DR. WESTON A. Price described “a new vitamin-like activator” needed to assimilate minerals, protect against tooth decay, support growth and development, optimize fertility, protect against heart disease and support brain function. Using a chemical test, he determined that this compound—which he called Activator X—occurred in the butterfat, organs and fat of animals consuming rapidly growing green grass, and also in certain seafood, such as fish eggs. Most importantly, he found the combination of cod liver oil and butter high in Activator X superior to that of cod liver oil alone. It turns out that Price’s Activator X is vitamin K2, produced by animal tissues, including the mammary glands, from vitamin K1, which occurs in rapidly growing green plants.*110
A growing body of published research confirms Dr. Price’s discoveries, namely that vitamin K2 is important for the utilization of minerals, protects against tooth decay, supports growth and development, is involved in normal reproduction, protects against calcification of the arteries leading to heart disease, and is a major component of the brain.
Just as true vitamin A from animal foods is vastly superior to carotenes from plant foods, and vitamin D from animal foods is superior to the vegetarian form of vitamin D, vitamin K2 from animal foods is manyfold more active in humans than the plant form, vitamin K1. Animals are “step-up transformers,” so to speak, converting plant forms of these important nutrients into more potent forms for humans, so humans do not have to use their own “disk space” to do it for themselves.
Originally, the medical community considered vitamins K1 and K2 as different forms of the same vitamin. The role of vitamin K2 in skeletal metabolism was not discovered until 1978 and it was not until 1997, nearly twenty years later, that scientists realized that vitamin K was “not just for clotting anymore.”111
Since the amount of vitamin K1 in typical diets is ten times greater than that of vitamin K2,112 researchers initially considered K2’s contribution to nutritional status insignificant. Yet over the last few years, a growing body of research is demonstrating that vitamins K1 and K2 are not simply different forms of the same vitamin, but in reality are two different vitamins: whereas K1 activates blood-clotting proteins, the main role of K2 is to place calcium where it belongs, in the bones and teeth, and prevent it from going where it does not belong, in the soft tissues, such as the arteries and kidneys.113
Plants contain vitamin K1 in a complex that is tied to both chlorophyll and beta-carotene. It plays a direct role in photosynthesis, and helps determine the richness in the green color of grass, its rate of growth and its brix rating (which measures the density of organic material produced by the plant). Animals grazing on grass will accumulate vitamin K2 in their tissues in direct proportion to the amount of vitamin K1 in their diet. The beta-carotene associated with vitamin K1 gives a yellow or orange color to butterfat; the richness of this color therefore indirectly indicates the amount of both vitamins K1 and K2 in the butter.
Weston A. Price demonstrated the synergy of Activator X with vitamins A and D. When put on a deficiency diet, chickens voluntarily consumed more butter and died more slowly when the butter was high in both vitamin A and Activator X than when it was high in vitamin A alone. Cod liver oil, which is high in both vitamins A and D, partially corrected growth retardation and weak legs in turkeys fed a deficiency diet, but the combination of cod liver oil and butter high in Activator X was twice as effective. Likewise, Price found that the combination of cod liver oil and a high–Activator X butter oil concentrate was more effective than cod liver oil alone in treating his patients for dental caries and other problems.
We now know that vitamin K2 works together with vitamins A and D—serving as the “activator” for vitamin A–and vitamin D–dependent proteins. While vitamins A and D act as signaling molecules, telling cells to make certain proteins, vitamin K2 activates these proteins by conferring upon them the physical ability to bind with calcium. In some cases these proteins directly coordinate the movement or organization of calcium; in other cases the calcium acts as a glue to hold the protein in a certain shape.114 In all such cases, the proteins are only functional after activation by vitamin K2. While vitamins A and D contribute to growth by stimulating growth factors and promoting the absorption of minerals, vitamin K2 makes an equal contribution to growth by preventing the premature calcification of the cartilaginous growth zones of bones.*115
Dr. Price’s main focus was the teeth. In his travels to remote corners of the globe, he found fourteen isolated groups that exhibited excellent dental health; they had very few cavities and all had broad faces and naturally straight teeth. At the same time, they exhibited “splendid physical development”: they had strong bones and exhibited excellent growth, good posture and good musculature. His research convinced him that rich dietary sources of vitamins A and D, along with Activator X, were responsible for this optimal development and freedom from dental caries.
Research into vitamins A, D and K2 now gives us the scientific explanation for Dr. Price’s findings. A child grows until the growth plates at the end of his bones calcify. It is vitamin K2 that prevents that calcification until the child reaches maturity. At the same time, the triumvirate of fat-soluble vitamins, along with adequate calcium, phosphorus and other minerals, ensures that the bones are densely formed and strong. A mineral-rich diet containing lots of fat-soluble activators from animal fats will ensure that the child grows not only tall, but also strong.†
There are also growth plates in the face, on either side of the maxilla (upper jaw bone). If these growth plates do not calcify too early, the face will end up wide and the cheekbones high and far apart—the hallmark of beauty. Vitamin K2 likely prevents calcification of the sides of the maxilla until optimal development is achieved. Set into the maxilla is the upper dental palate, and this will be wide if the maxilla is wide. The mandible (lower jaw bone) will be equally wide and strong with optimal prenatal and postnatal nutrition. A wide dental palate can accommodate all the teeth, even the wisdom teeth, without crowding—and these teeth will be well formed and strong as a result of the same nutrients, that is, abundant minerals and abundant fat-soluble activators.
Price and his colleagues in the 1930s and 1940s considered the teeth as the most accessible indicator of overall health. The mouth is the only interior part of the body that we can see. They reasoned that if the teeth are straight and free of infection, then the whole body is well formed and resistant to disease.
How does vitamin K2 prevent dental caries? Price found that the vitamin influences the composition of saliva. When he collected the saliva of individuals immune to dental caries and shook it with powdered bone or tooth meal, phosphorus would move from the saliva to the powder; by contrast, if he conducted the same procedure with the saliva of individuals susceptible to dental caries, the phosphorus would move in the opposite direction from the powder to the saliva. Administration of the Activator X concentrate to his patients consistently changed the chemical behavior of their saliva from phosphorus-accepting to phosphorus-donating. The Activator X concentrate also reduced the bacterial count of their saliva.
Thus, vitamin K in the saliva helps the teeth mineralize and also reduces bacteria that might play a role in causing cavities.* Price used the combination of high-vitamin cod liver oil and high–Activator X butter oil to reverse dental caries. This protocol not only stopped the progression of tooth decay, but completely reversed it without the need for fillings. The procedure caused the dentin to grow and remineralize, sealing what were once active caries. One fourteen-year-old girl completely healed forty-two open cavities in twenty-four teeth by taking capsules of the high-vitamin cod liver oil and Activator X concentrate three times a day for seven months.116
Likewise, Price used butter oil concentrate to cure rickets. In a four-year-old boy who suffered from rampant tooth decay, seizures and a tendency to fracture, the combination of a large helping of this concentrate and meals of whole wheat and whole milk rapidly resolved each of these symptoms.
Studies from Japan have shown that vitamin K2 completely reverses bone loss and in some cases even increases bone mass in populations with osteoporosis.117 It also reduces the incidence of fractures.118 Another study found that vitamin K2 protects against hip fractures and osteoporosis.119
Vitamin K2 protects us from heart disease by preventing calcification of the arteries. The Rotterdam Study, which prospectively followed just over forty-six hundred men ages fifty-five or older in the Netherlands, found that the highest intake of vitamin K2 was associated with a 52 percent lower risk of severe aortic calcification, a 41 percent lower risk of coronary heart disease (CHD), a 51 percent lower risk of CHD mortality and a 26 percent lower risk of total mortality.120 The conventional view is that foods rich in cholesterol and saturated fat cause heart disease, but these same foods—butter, aged cheeses, poultry liver and fat—provide vitamin K2, which strongly helps to prevent heart disease.
Price supplied several anecdotes suggesting that Activator X plays an important role in the nervous system. When he administered a daily meal of nutrient-dense whole foods supplemented with high-vitamin cod liver oil and high–Activator X butter oil to the children of impoverished mill workers who suffered from rampant tooth decay, the treatment not only resolved the tooth decay without the need for fillings, but also cured chronic fatigue in one boy and, according to the school teachers, produced a marked increase in learning capacity in two others.
Price also administered the butter oil concentrate to a four-year-old who suffered from rampant tooth decay, a fractured leg and seizures. A spoonful of the butter oil* served over whole wheat gruel with whole milk once before bed and five times over the course of the following day immediately resolved his seizures. Rapid healing of his fracture and dental caries followed soon after. The fact that these three symptoms appeared together and resolved following the same treatment suggests a common cause for each of them.
Sixty years later, modern research is now elucidating the essential role that vitamin K2 plays, not only in the dental and skeletal systems, but in the nervous system as well. The brain contains one of the highest concentrations of vitamin K2 in the body; only the pancreas, salivary glands and the cartilaginous tissue of the sternum contain more. Vitamin K2 supports the enzymes within the brain that produce an important class of lipids called sulfatides. The levels of vitamin K2, vitamin K–dependent proteins and sulfatides in the brain decline with age; the decline of these levels is in turn associated with age-related neurological degeneration.121 Comparisons of human autopsies associate the early stages of Alzheimer’s disease with up to 93 percent lower sulfatide levels in the brain.122 Animals that completely lack the enzymes to make sulfatides and a related class of lipids, cerebrosides, progressively suffer from growth retardation, loss of locomotor activity, weak legs and seizures.123
These observations suggest that deficiencies in vitamin K, especially vitamin K2, could result in fatigue and learning difficulties in humans, and that rare, extreme deficiencies of vitamin K2 in the brain could result in seizures. If this is the case, it would explain why Price observed tooth decay, bone fracture, learning difficulties and seizures to share a common cause and a common solution.
The highest concentration of vitamin K2 exists in the salivary glands and the pancreas, which suggests a role in activating digestive enzymes and regulating blood sugar.124 The testes of male rats also exhibit a high preference for and retention of vitamin K2,125 and human sperm possess a vitamin K–dependent protein with an unknown function.126 The kidneys likewise accumulate large amounts of vitamin K2127 and secrete vitamin K–dependent proteins that inhibit the formation of calcium salts. Patients with kidney stones secrete this protein in its inactive form, which is between four and twenty times less effective than its active form at inhibiting the growth of calcium oxalate crystals, suggesting that vitamin K2 deficiency is a major cause of kidney stones.128 Again we are seeing the role of K2 in calcium regulation—putting it in the bones, where it belongs, and preventing the formation of calcium deposits in soft tissues, like the kidneys.
A number of cell experiments have shown that vitamin K2 helps protect us against cancer.129 A study from Europe found that an increased intake of vitamin K2 can reduce the risk of prostate cancer by 35 percent. In addition, the potential benefits of K2 were more pronounced for advanced prostate cancer, while vitamin K1 offered no benefits.130 More recently, in a 2010 study involving over twenty-four thousand subjects, dietary intake of vitamin K2 was found to protect against cancer. The subjects were free of cancer at enrollment. On follow-up over ten years later, over seventeen hundred cases of cancer occurred, of which four hundred fifty-eight were fatal. Those with the highest intake of vitamin K2 had the lowest incidence of cancer, and the lowest cancer mortality, especially in men. The authors made the startling suggestion to consume cheese (a rich source of K2) as a way to prevent cancer!131
Most interesting of all is research suggesting that vitamin K plays a role in protecting skin elasticity and may help protect against skin aging and the development of wrinkles.132
In the Western diet, the best sources of vitamin K2 are aged, full-fat cheeses of animals that eat green grass, and the fat and livers of ducks and geese. Cheese is rich in K2 not only because it occurs in the butterfat, but because more is formed during the aging process.* Why the fat and liver of ducks and geese are good sources remains a mystery—but that doesn’t prevent us from enjoying goose liver pâté and potatoes cooked in duck fat. Lesser amounts occur in chicken liver, butter, egg yolks and meat fats—all those “empty calorie” delicacies the food police warn us not to eat.
The bottom line: “Solid fats” like butter, cream, whole milk and cheese, egg yolks, poultry fats and meat fats are not empty foods, but rich sources of vital nutrients—nutrients that contribute to optimal health and happiness, especially when combined with foods from the sea, like fish eggs, fatty fish, shellfish and especially cod liver oil. And the more naturally the animals are raised—outdoors, on green pasture—the more nourishing their fats and organ meats will be.