

There is a fountain of youth: it is your mind, your talents, the creativity you bring to your life and the lives of people you love. When you learn to tap this source, you will truly have defeated age.
—SOPHIA LOREN
Sammie was a sunny little girl with a wide, happy smile. She was just entering fourth grade when her mother, Chris, took a job outside the home for the first time in years. Sammie was often overcome with anxiety. She became anxious when her mom had to work a little late, even though friends and family cared for her for the hour or two before Chris could get home. Then, seemingly out of nowhere, Sammie became obsessed with fear about getting sick. “Her anxiety was getting so intense,” Chris said, “that we scheduled an appointment with a therapist. It was odd because there was really nothing in our lives that had happened to this point that would cause her to worry like this. No sickness or death in the family or among friends.” Chris and her husband, Steve, reassured Sammie that it would be more likely that an “airplane would crash into their house” than that she would get seriously or fatally ill. Still, the inexplicable fears continued.

One Monday, Sammie came home from school describing a “big magnet machine” her class saw on a film in class, which scared her. “I told her it was an MRI machine,” said Chris, and calmly explained what it did. “Then we wrote down her fears together on a piece of paper and I asked her, ‘What do we do with our fears?’ Sammie wadded up the paper and threw it in the fireplace, a visual way to ‘toss fears away.’ ”
The next day, a Tuesday, Sammie took a spill on her Rollerblades. The following night her knee was very swollen, and she was frightened. Chris took her daughter to a clinic the next day. And that is when, to their shock and surprise, an “airplane crashed into their house,” so to speak.

The doctor asked Chris to call her husband for support when he realized the bulge in Sammie’s knee was a tumor. Sammie would be diagnosed with osteosarcoma, an insidious type of bone cancer. “Looking back,” Chris said, “though we didn’t see it as anything more than a phase of childish anxiety at the time, a few scenes flashed through my mind. There was a family outing when Sammie had some shortness of breath. On the Fourth of July, she’d not wanted to run with the rest of the kids.” Sadly, by the time the cancer had showed up on her knee, it had also gone to her lungs. This was followed by chemotherapy, every three weeks for five to seven days, for one very tough year. Along with the chemo came awful nausea, weakness, and hair loss. The doctors were able to save Sammie’s cancer-riddled leg, but 70 percent of her leg and knee was now titanium. She also had to have a thoracotomy, which is a painful major surgery that involved an incision in the chest and spreading of the ribs, so the surgeons could get to and remove the tumors in her lungs.
Sammie finished treatment in November of 2008 and was pronounced cancer free, but in January of 2009, she took a fall at the fairgrounds. The cancer had metastasized to her spine. More treatment, spine surgery, more thoracotomies, more agonizing pain, more of every parent’s worst nightmares, multiplied. The three-month scan showed the cancer had spread everywhere. In fact, the surgeon said that there were too many tumors to count. Even so, knowing that Sammie’s will to live was so strong, Chris and Steve agreed to try more chemo to slow the growth. However, one night, because she was so low in potassium from her many ordeals, Sammie went into cardiac arrest.
“We literally lost her,” Chris said, “as her life ebbed away in my arms.” Steve, however, knew CPR and managed to get her heart beating again. When she came to, Sammie reported seeing a bright light and thought the family was at Disneyland because it was such a happy place. Her glimpse of heaven? After this experience, there would be no more chemo, no more medical interventions.
“We had to shift from helping Sammie to live, to preparing our precious child to die,” said Chris. Talk about a task that no mother or father can fathom having to do.
Sammie lived seven more months, but these days were filled with horrendous pain, sickness, and depression. Eventually hospice came, and though Sammie had a glimpse of the happiness beyond death during her heart attack, she still fought hard to live to the very end. The last three days of her life were worse than Chris or Steve could have imagined. There were many seizures, and the long hours of watching their little girl fighting in vain for her life were devastatingly difficult. “Sammie wanted to die at home,” Chris explained, a catch in her voice, wiping at tears. “We did all we could for her up to the end, when she died as her father held her tight in his arms.”
Those last three days, along with the multiple ordeals over the last three and a half years, would be a trauma that would fill Chris’s mind with painful recurring memories that invaded her thoughts night and day.
There was a beautiful funeral, a celebration of Sammie’s courageous short life, but after Chris said her final good-bye to her daughter, in many ways she said good-bye to herself. “Sammie was our middle child,” Chris shared. “She has an older sister, Taylor, and younger brother, Ryan, and of course I did my best as a parent in crisis, but they were often put on the back burner of our lives, which revolved around saving their sister’s life and then helping their sister let go of her life. There was little or no thought of myself during those years as I poured every ounce of my strength into Sammie’s care.”
To try to numb the great loss, Chris began to eat and to drink alcohol. She had a hard time getting out of bed. “I sank into a depression so low that I told myself I would just make it to the anniversary of Sammie’s death and then find a way to end my life. I just didn’t feel I could go on. I was seeing a good therapist who worked with me every week, and promised me there would be a shift eventually that would help lessen this debilitating grief. He did not encourage medication, telling me, ‘There is no medication that can touch this kind of pain.’ But there were things I kept from the therapist, even, like my increased use of alcohol.”
Then one day Chris was visiting with a friend of her sister’s. “This lady was very fit and had a positive attitude.” Chris was short, just 51, weighing a little over 200 pounds and walking in a gloom so heavy she thought she’d never smile—and mean it—again. “This friend had a copy of the Change Your Brain, Change Your Body Food Journal,” Chris explained. “Flipping through it, I thought, ‘Okay, I like this. It makes sense to me. I have to start looking for the brighter side of life.’ After all, my choices at that point were to take my life, drink myself to death, or end up in rehab. And I was way too proud to go to rehab.”
Chris went home, found the book Change Your Brain, Change Your Body on the Internet, and downloaded it to read that evening. She read the whole book (not a short book!) in one night. “There was one part of the book, and I can still remember how I felt when I read the list of things that alcohol stops you from feeling, like empathy and compassion for others. I knew I needed to get my feelings of empathy and compassion back for my other children and husband. I needed to find a way to be happy and whole again for their sakes, and my own.”
Chris was a thirsty sponge and she absorbed everything written in the book. She said, “I went hard core into the plan. In fact, I did a twenty-eight-day cleanse. I tossed out all the alcohol, ate no processed food, and began taking fish oil and vitamin D.”
The change for Chris was fast and remarkable. “Within eight days I didn’t care if I never dropped a pound again. I was free! Because I was eating food that actually nourished my cells, the food and alcohol cravings stopped. I got rid of all the diet drinks and colas. I slept through the night for the first time in four years. And for the first time in years, I didn’t wake up in a panic.”
Chris continued, “I never looked past the trauma with Sammie for the reasons behind my depression and addiction. I blamed everything I felt on the loss and grief. But as I read Change Your Brain, Change Your Body, I took a broader inventory of my life and realized I’d struggled with anxiety for a long while. After the first eight days of getting rid of junk and dealing with ANTs (automatic negative thoughts) according to the methods in the book, my anxiety level dropped from a 10 to a 3. I can actually talk myself out of an anxiety attack now by asking myself questions such as, ‘Is it really true?” and ‘If even a part of it is true, is there anything I can do to change it?’ I also use other antianxiety techniques from the book, but honestly, it is usually so calm inside my brain now that I don’t need them often. And remember, I only began this program five months ago.”
Chris went from never having run before to running four days a week. She advises, “I really recommend running outside if at all possible. I also got myself some support by getting involved in a group called Running for Women where they taught me how to run and walk in intervals. I run 4.5 miles a day, four days a week. Sometimes I run with a bunch of women but sometimes alone. I don’t let anything deter me. I go no matter what because I need those endorphins to help me stay balanced! I may not ‘love’ the feeling of running while I do it, but I see it as an emotional investment that pays huge dividends. It only takes an hour, four times a week, and the payoff is a calmer brain and healthier body.”
In five months, Chris is down 35 pounds and four pant sizes, which she sees as a side benefit to getting her emotional life back thanks to nutritional changes and physical activity. “It’s not just that I am losing weight. I am changing the way I lose weight. I have lost 8 inches off my waist, my neck has slimmed, and my skin is brighter. Though I’d like to lose some more weight, if you saw me today, you’d never think, ‘Oh, there’s a woman who needs to lose some pounds!’ My weight, with the new muscle, has distributed itself well. I used to be a Weight Watchers gal, but I ate a lot of diet food on that plan, and it only increased my cravings. I’d always gain the weight back. On this plan I don’t have cravings because I am eating real food that satisfies. I finally look like I’m in the body I’ve always belonged in, and I am!”
Chris now admits that the depths of her depression had roots and patterns beyond the loss and trauma. She says, “I’m grieving now, but I’m grieving well.” She spoke of taking care of herself the way a mom would take care of a child. “Friends tease me about always having healthy snacks in my purse when we are out and about at kids’ events. Lord knows there’s nothing redeeming in most snack bars. Trust me, I’ve looked! I just ask them, ‘When your kids were little, did you ever leave the house without a diaper bag packed with everything your child might need, including healthy snacks and a sippy cup? You were prepared because you didn’t want to end up stuck somewhere with a cranky, crying baby, right? Well, I’m just treating myself as a good mom would treat her child because I don’t want to get stuck somewhere without nutritious food or drink and end up cranky and crying.’ ”
Chris’s daughter, Taylor, is now seventeen years old, and much of her teen years were spent without her parents’ full focus because of her sister’s major illness. Recently Taylor told her mom, “You are a joy to be around again!” Ryan is eleven now and so supportive of his mom as well. He told Chris, “You don’t have two necks anymore!” (Boys at eleven are honest, if anything.) He also told her one day that he wasn’t going to have dessert for a whole week as a way to support his mom’s efforts. Her husband, Steve, has stood by Chris through every moment of this long ordeal and he verbalizes how proud of her he is, that he knows that every morning she wakes up she has to make a choice to live happy and honor her daughter’s memory or slack up and go back to that dark place.
“I’m still grieving but I am grieving better, if that makes sense. When we spend time together as a family, going out somewhere fun, I really have to fight the ANTs. My automatic reaction is sadness and thinking about the hole in our family where Sammie used to be. But I take control of my thoughts and remind myself that Sammie is happy and wants us to be happy too. I focus on what we still have, including one another, and the good memories of Sammie, instead of what we don’t have.”
Chris has become a crusader for my new program, The Amen Solution—Thinner, Smarter, Happier with Dr. Daniel Amen! Her father, mom, and sister are on the plan. Taylor has lost 17 pounds as well. Friends sometimes approach her and say things like, “I can’t believe I’m telling you this because what you went through is worse than what I’m going through, but I’m feeling depressed and I can’t help but notice the change in you.” She then shares my books with them. “I keep a copy of The Amen Solution on my kitchen counter now because I refer to it so often for myself or for someone who asks me about what’s happened to me the last few months.”
When I was speaking at our northern California Clinic, Chris’s friend Mo, who is also the director of outcome research at the Amen Clinics, called Chris and encouraged her to come meet me and hear my talk. Chris’s ANTs said to her brain, “Oh, I have too much to do, I really can’t.” But immediately Chris recognized this as the “old Chris” talking and replied, instead, “I’d love to go.” I, for one, am so glad she did, as her story deeply and profoundly touched me.
When I first met Chris she started to cry, which almost made me cry. This happens to me a lot. People come up to me, start to cry, and then tell me how our work has changed their life or the life of one of their loved ones. This has always been the reason behind why I do what I do, despite some of the obstacles that have come our way.
Chris shared, “I’m honoring Sammie’s memory in a better way by taking care of myself, and everything else seems to be just falling into place. I don’t want to live in the realm of ‘childhood cancer.’ I want to help people enjoy their lives and overcome whatever issues are troubling them. Sammie didn’t want to be ‘the cancer kid’ or poster child for cancer either. She just wanted to be Sammie, herself.”
The family sold their home and moved to a new house shortly after Sammie died. In Chris’s case, the house was too full of sad memories and a new home represented a new chapter of life. As Chris began to ponder the other changes she wanted to make in her life, she looked for a job that would support her goals. She applied to work at a specialty shoe store where people get into the right running shoes for the shape of their foot. “I have a strong retail background and really wanted to work for this company, but were they going to hire a middle-aged woman in her forties who weighed 202 pounds? In years past, I would have let that thought intimidate me, but my focus was so strong on getting healthy and I’d been through the death of a child, so really, I felt I didn’t have anything to lose in applying, and I took a leap.”
Chris eventually secured the position and today absolutely loves her job. “The staff is gentle and kind, and we have a great time on the job together. I am stretching and growing my brain cells by learning so much new information.”
She continued, “I am creating a life that I desire instead of what was presented to me. I saw quite poignantly that there is much in life over which we have no control. So I’d better take control of what I can. So I am feeding myself well, taking myself for runs, being nice to myself. And this allows me to be the healthy, happy person who can now give joy to others again.”
Chris’s sister started a “bunny drive,” which happens every spring, when children’s hospitals are in most need of gifts for sick kids. The charitable project gathers all sorts of new stuffed animals (five thousand in 2011) and gives them to six local hospitals that care for children, making deliveries on Good Friday. When a child gets a hospital bed during this time, a stuffed animal lies on the pillow with a name tag that says, “From Angel Sammie.” For more information on how to help with the bunny drive and to read more of Sammie’s story, you can visit www.caringbridge.org/visit/sammiehartsfield.
Depression, grief, and chronic stress all take years off your life and make you look, feel, and think older than your age. Depression is one of the greatest problems and killers of our time, affecting fifty million Americans at some point in their lives. Nearly all of us have either suffered from depression or have known someone who has. Two of my best friends had fathers who killed themselves. Depression, all by itself, is a risk factor for Alzheimer’s disease, heart disease, cancer, and obesity. When depression accompanies heart disease, people are much more likely to die earlier than those without it. Grief causes your heart to go into abnormal rhythms, which is one of the reasons why people often experience physical chest pain with the loss of a loved one.
Chronic stress is associated with an increased production of certain hormones that cause metabolic changes that put more fat on your belly and diminish the part of the brain that helps get memories into long-term storage. Whenever you experience depression, grief, or chronic stress, think of it as a health emergency. These negative emotional states have a damaging effect on your physical body and have been associated with obesity, cancer, diabetes, heart disease, and dementia. Unless treated aggressively, depression, grief, and chronic stress will rob your ability to live a long, healthy life.
Chris’s story illustrates how these negative emotional states can overwhelm and steal your life, and how to work to heal them. When hit with a severe emotional trauma many people self-medicate the pain with toxic food, alcohol, drugs, or sex. The problem, of course, is that short-term solutions only eradicate the pain for a little while and make the situation worse in the long run.
Pastor Gerald Sharon lost his wife in December 2010 after a nine-month battle with colon cancer. It was hell for him. Yet his initial reaction to the crisis had been the opposite of Chris’s. Gerald had been a senior pastor for many years and had seen many people fall apart during the stress of crises. He knew that if he was going to survive and be able to take care of his wife and be there for his children he had to get healthy. So in the midst of the family emergency, he went to his physician, saw a nutritionist, got on a healthy-eating regimen, exercised, and lost 50 pounds. “I am a stress eater,” he told me. “I knew if I was not careful, I would gain 50 more pounds and die in the process as well.”
It is common to suffer physical and emotional exhaustion when mourning. Adapting to the loss of someone you love is one of life’s most difficult challenges. Your brain is being asked to adapt, sometimes suddenly, to new routines without the presence of your loved one. Grief can leave you thinking you may be going crazy at times. In her bestselling memoir The Year of Magical Thinking, the author Joan Didion writes candidly about the sorts of “tricks” her brain would play on her as she adjusted to the sudden loss of her husband after many decades of a happy marriage. “We might expect that we will be prostrate, inconsolable, crazy with loss,” she writes. “We do not expect to be literally crazy, cool customers who believe that their husband is about to return and need his shoes.” It will comfort you to know that you are not going crazy; but your deep limbic system, where your emotions of connection and bonding are stored, is going through withdrawal from the person you love as bad as that of any drug withdrawal.
Immediately following a major loss, your prefrontal cortex (PFC) may be overwhelmed by the limbic system (feeling and mood center) and temporarily cease to function well. Even creating a to-do list may feel taxing in the days, weeks, and months following loss or during times of high stress. Accept that you may need to radically shorten your to-do list, and give your brain and body vital time to adjust.
You do not have to react to a crisis with self-destructive behavior. You can respond with love—the type of self-love that opts for caring for your brain and body, so that you can deal with the stresses that will inevitably come your way.
Both Gerald and Chris give us guidance on how to naturally treat depression, grief, and stress. In addition to being kind and patient with yourself, it will help immensely if you can put “Take Exceptional Care of My Brain” at the top of your newly shortened and reprioritized to-do list. This one decision will help you cope better with all the other choices and adjustments you must make during a difficult time. Here are some ways to practice good self-care and brain care during stressful or sorrowful seasons:
• Eating proper food to nourish your body is critical during times of stress. Fruits and veggies will reduce inflammation that leads to more pain and illness. Protein will assist a strong transmission of nerve impulses in the brain and is a key fuel for healing and optimizing brain function. One of the amino acids in protein, tyrosine, will increase the levels of two important neurotransmitters, norepinephrine and dopamine. This habit will help your energy levels and you will feel better physically. If you don’t feel like eating solid food, a high-quality protein shake can come to your rescue. Sip on it as you can, even though you may not feel hungry at first. Though your appetite might not present during the worst days, your body needs nutrients now more than ever.
• Get physical exercise, which will help you withstand and heal emotional pain. Force yourself to put on those sneakers and walk, preferably outside so you can also get the benefit of sunlight. You may find, like Chris, that pushing past initial reluctance to get out of the house and move will pay big dividends. Listening to music or an audio book may help make the walk more enjoyable. Even if you don’t “love” walking while you are doing it, you will notice an improved mood during the day, which will make this investment in your brain health worth the effort. Yoga may also be soothing if you are feeling anxious as well as sad.
• Take healthy supplements. Smart supplementation is important, such as using omega-3s, optimizing your vitamin D level, and using targeted supplements depending on your own type of brain (more on this in a bit).
• Eradicating the ANTs that infest your mind is critical to keeping your mind fertile for long-term growth. (More on this later in the chapter as well.)
• Cry. Did you know that tears of sorrow have been shown to have toxins in them, where tears of happiness do not? This is one reason that you tend to feel better after a good cry when you are sad. So don’t postpone or push back the tears. Let the grief waves flow, and wash some of the pain out of your brain and body with a good cleansing cry.
• Set goals. Having a specific goal is critical for positive brain function. After that good cry, you’ll probably feel some lifting of sorrow and this is a good time to treat yourself to something you like to do, that is good for you. You need breaks from sadness! Meet an understanding friend for lunch, browse to your heart’s content at a bookstore, play or run with your dog. Watch a sitcom or read a light, funny book if you can. Do whatever soothes and offers even a small bit of joy.
• As soon as possible, learn something new. Perhaps take an art class, a gourmet cooking class, learn how to fly fish, or dance the samba. Learning anything new, especially something outside your comfort zone, will stimulate the growth of new cells and neural connections. When Chris pushed herself to apply for and learn a new job, her brain’s neurons responded with growth and healing feelings. If the new subject or skill really catches your attention, you may experience periods of “flow” where you feel almost transported away from worry, regret, and sorrow for a time. A fascinating new hobby or interest can give you mini-vacations from grief. One widow who was struggling to find a reason to live woke up one morning and thought, “I’d like to work at a horse rescue ranch.” She followed that small desire volunteering at just such a ranch and found the work to be meaningful and healing. As she comforted the animals, they in turn comforted her. It also put her in contact with compassionate people who shared her love of animals and nature.
• Hydrate. Water is crucial in brain function and will also keep your lymph system working to remove toxins from the immune cells and reduce the possibilities of infections when under stress.
• Make every effort to focus on what you can do to strive to be more loving and grateful. “In my thirty years of helping the bereaved,” says Dr. Louis LaGrand, a grief counselor and author of Love Lives On: Learning from the Extraordinary Experiences of the Bereaved, writes, “I am convinced that love is the single most effective coping strategy that will get you through any loss. For the brain, it will minimize, often eliminate, the power of negative thoughts to generate excessive and unnecessary emotional and physical pain.” In addition to the great advice of “loving more,” I would add, “purpose to be more grateful.” The emotions of love and gratitude literally block many negative emotions in the brain. It is hard to really feel grateful and negative or stressed at the same time.
Most of us will experience the pain grief brings at some point in our lives, either through the death of a loved one, unwanted divorce, or other rejection or loss. In time, most people move on. Though we never forget someone we loved deeply, as months and years pass, the memories of them are less attached to pain and more attached to warm and positive memories. This time varies for all of us, as human beings don’t grieve on a set schedule, but there is a syndrome that may perpetuate the grief process longer in some people than others.
In a UCLA study on bereavement, scientists proposed that in addition to normal grief, there is a syndrome called complicated grief. This is a sort of unrelenting grief that never allows for healing and moving on. It activates neurons in the reward centers of the brain (as well as the pain centers), possibly giving past memories addiction-like properties. After the loved one dies, those who adapt to the loss eventually stop getting this neural reward, but those who don’t adapt continue to crave it. This is not something people consciously do; it simply happens to some people (10–15 percent of the grieving population) and not to others.
Complicated grief can be debilitating, involving recurrent pangs of painful emotions, including intense yearning, longing, and searching for the deceased and a preoccupation with thoughts of the loved one. Some of these experiences are common to the newly grieving as well, as the brain strives to adjust to new realities. But if the brain doesn’t adjust, if grief is just as intense years later, additional help may be needed to process through grief and find a meaningful life again. Besides the “natural helps for grief and stress” listed above, someone whose grief has become complicated or has turned into a clinical depression may need therapy, supplements, and medication to move forward again.
Below is a chart that might help you determine if you or someone you care about is simply going through the normal grief process or may have complicated grief or clinical depression.
CHARACTERISTICS OF GRIEF OR DEPRESSION:
A SIDE-BY-SIDE COMPARISON
| Grief | Complicated Grief or Depression |
| A normal response to loss that causes distress | Generalized distress—loss of interest, pleasure |
| May experience some physical symptoms of distress | Physical distress, hopelessness, guilt |
| Still able to look toward the future | No sense of a positive future |
| Passive wish for death | Suicidal ideation not uncommon |
| Retains capacity for pleasure | Change in capacity to enjoy life or things that were formerly pleasurable Persistent flat affect, negative self-image |
| Still able to express feelings and humor | Bored, lack of interest and expression |
| Comes in waves | Constant, unremitting |
| Can cope with distress on own or with supportive listening Medication for grief is an exception, not the rule | May require combined therapy, supplements or medication |
Knowing the type of brain you have is critical to getting the right help. When I first started our brain imaging work at the Amen Clinics in 1991 I was looking for the one pattern that was associated with depression, ADHD, or bipolar disorder. But our brain imaging work clearly taught us that there was not one brain pattern associated with any of these illnesses. They all had multiple types. Of course, I then realized that there will never be just one pattern for depression, because not all depressed people are the same. Some are withdrawn, others are angry, and still others are anxious or obsessive. The scans helped me understand the type of depression, ADHD, bipolar disorder, overeating, or addiction a person had, so that I could better target their treatment.
This one idea led to a dramatic breakthrough in my own personal effectiveness with patients and it opened up a new world of understanding and hope for the tens of thousands of people who have come to the Amen Clinics and the millions of people who have read my books.
Basically, we see these eight brain types:
1. Impulsive
2. Compulsive
3. Impulsive-compulsive
4. Sad or moody
5. Anxious
6. Temporal lobe
7. Toxic
8. Post-traumatic stress
We see these in all sorts of combinations as well. This is exactly the reason why most psychological and psychiatric treatment programs do not work on a consistent basis. They take a one-size-fits-all approach to illnesses, such as depression, which judging from our brain imaging work makes absolutely no sense at all.
There is much more information, including a detailed self-test, on our website (www.theamensolution.com) and in my other books, such as Change Your Brain, Change Your Life, Healing ADD, Healing Anxiety and Depression, The Amen Solution, and Unchain Your Brain.
People with this brain type have low activity in the PFC. Think of the PFC as the brain’s brake. It stops us from saying stupid things or making bad decisions. Subsequently, people with this type of brain struggle with impulse control, attention, and disorganization. They have trouble thinking about the consequences of their behavior before they act, which can get them into all sorts of hot water with their health, relationships, work, and money.
One of my best friends is a perfect example of this type. He is on a diet every single day of his life. He wakes up every morning committed to the idea of eating right. He maintains the thought as he passes the first doughnut shop. He starts to sweat as he passes the second doughnut shop. By the third one, he has no willpower left. After completely giving up on his plans by noon, he utters the famous words of all impulsive overeaters: “I’ll start my diet tomorrow.”
This type is common among people who have ADHD, which has been associated with low dopamine levels in the brain. Research suggests that having untreated ADHD nearly doubles the risk for being overweight and having other medical problems. Without proper treatment, it is nearly impossible for these people to be consistent with any health plan.
My research team and I have published several studies showing that when people with ADHD try to concentrate, they actually get less activity in the PFC, which will cause them to have even less control over their own behavior. For these people, literally, the harder they try to lose weight, the worse it gets.
|
Normal Brain SPECT Scan 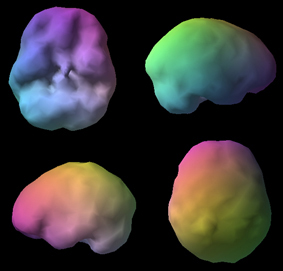
Full, even, symmetrical activity |
Impulsive Brain Type 
Low PFC at front of brain |
This type is helped by boosting dopamine levels in the brain to strengthen the PFC. Higher-protein, lower-carbohydrate diets tend to help, as do exercise and certain stimulating medications or supplements, such as green tea or L-tyrosine. Any supplement or medicine that calms the brain, such as 5-HTP (5-hydroxytryptophan), typically makes this type worse, because it can lower both your worries and your impulse control.
People with this type tend to get stuck on negative thoughts or negative behaviors. They often say that they have no control over their behavior and tend to worry, hold grudges, be rigid and inflexible, argumentative or oppositional. The main problem is that they have trouble shifting their attention, so they get stuck on bad thoughts and behavior.
I am often asked, what is the difference between people who are impulsive versus those who are compulsive? Impulsivity is when you get a thought in your head and you just act on it without thinking. Compulsivity is when you get a thought in your head and you feel as though you have to act on it.
The compulsive brain on SPECT scans usually shows too much activity in a deep part of the frontal lobes called the anterior cingulate gyrus. I think of this part as the brain’s gear shifter that helps us go from thought to thought or idea to idea. When it functions optimally, people tend to be flexible, adaptable, and go with the flow. When this part of the brain works too hard, usually owing to a deficit in the neurotransmitter serotonin, people tend to be rigid, inflexible, and get stuck on bad thoughts or bad behaviors.
|
Normal “Active” Brain SPECT Scan 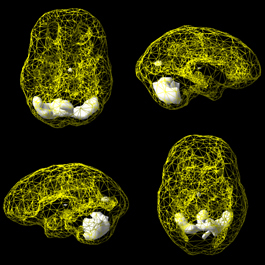
|
Compulsive Brain Type 
High anterior cingulate at front of brain |
Caffeine and diet pills usually make this brain type worse, because these brains do not need more stimulation. People with this type often feel as though they need a glass of wine at night, or two or three, to calm their worries.
Compulsive brain types do best when we find natural ways to increase serotonin. Serotonin is calming to the brain. Physical exercise boosts serotonin as does using certain supplements, such as 5-HTP or St. John’s Wort. 5-HTP actually has good scientific evidence that it can be helpful for depression, anxiety, and weight loss.
On the surface it seems almost contradictory. How can you be both impulsive and compulsive at the same time? Think of compulsive gamblers. These are people who are compulsively driven to gamble and yet have very little control over their impulses. It is the same with this brain type. Our scans tend to show too much activity in the brain’s gear shifter (anterior cingulate) region of the brain, so people overthink and get stuck on negative thoughts, but they also have too little activity in the PFC so they have trouble supervising their own behavior.
Barb struggled with oppositional and impulsive behavior as a teenager and still at age forty-eight got stuck on negative thoughts and had trouble controlling her impulses, especially in raising her own teenagers. Many people in her family struggled with alcohol and other addictions, which is very common with this brain type. Barb had tried a number of treatment programs before coming to the Amen Clinics without any success. She had tried stimulants for ADHD, which made her angry, and antidepressants that boosted serotonin, such as Prozac, Zoloft, and Lexapro, which seemed to make her more impulsive. After listening to her story and seeing her scans it was clear she had an impulsive-compulsive brain.
People with this type benefit from treatments that increase both serotonin and dopamine, such as exercise with a combination of supplements like 5-HTP (to boost serotonin) and green tea (to boost dopamine) or medications to do the same thing, such as a stimulant plus a serotonin-enhancing antidepressant at the same time. For Barb, this combination of supplements helped to balance her brain so she could feel emotionally stable. Giving her 5-HTP or green tea alone would have made her worse!
People with this type often struggle with depression, negativity, low energy, low self-esteem, and pain symptoms. On brain SPECT scans we often see too much activity, deep within the limbic or emotional part of the brain. With this type, when there are the external factors of stress or grief, the vulnerability is often depression. We often hear of depression running in families or being brought on by stressful early life events.
Gary struggled with chronic sadness and negativity. He remembers feeling sad as a child, which only worsened after he lost his grandfather at age thirteen. At age fifty-seven he felt older than his peers and suffered with arthritis. He had tried psychotherapy and several antidepressants with little effect before he came to see us. His SPECT scan showed too much activity in the limbic or emotional part of his brain, which is commonly seen in mood disorders. For this type, we have had good success by encouraging our patients to exercise, take high-dose fish oil (6 g), and certain supplements, such as SAMe (S-adenosylmethionine), to help improve mood, energy, and pain.
|
Normal “Active” Brain SPECT Scan 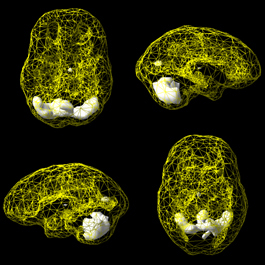
|
Sad Brain Type 
High deep limbic activity |
SAMe is a nutritional supplement that has good research demonstrating its effectiveness for both depression and pain. Of note, there is a clear connection with physical pain and depression, which SAMe appears to help, as does the antidepressant Cymbalta (duloxetine). When the limbic brain is combined with the compulsive brain, serotonin interventions seem to be the most effective.
People with this type struggle with feelings of anxiety or nervousness. They often feel tense, panicky, and stressed and tend to predict the worst. They are usually conflict avoidant and live with a feeling of angst and that something bad will happen. We often see too much activity in an area deep in the brain called the basal ganglia.
Doreen felt anxious most of the time. She was always waiting for something bad to happen, and she frequently suffered from headaches and stomach problems. Marijuana helped relax her, but it also gave her memory problems. She had tried antianxiety medications but quickly had the feeling that she was becoming dependent on them, a feeling she hated. Doreen’s SPECT study showed too much activity in the basal ganglia. This part of the brain is involved in setting a person’s anxiety level. When there is too much activity here, often owing to low levels of a chemical called GABA, people often have anxiety and a lot of physical tension.
|
Normal “Active” Brain SPECT Scan 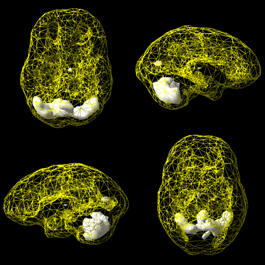
Most active areas in cerebellum |

High basal ganglia activity |
By soothing Doreen’s brain with meditation and hypnosis, plus using a combination of B6, magnesium, and GABA, she felt calmer and more relaxed and noticed a big boost in her energy.
The temporal lobes, underneath your temples and behind your eyes, are involved with memory, learning, processing emotions, language (hearing and reading), reading social cues, mood stability, and temper control. Trouble in the temporal lobes, often owing to a prior brain injury, can lead to memory problems, learning difficulties, trouble finding the right words in conversation, trouble reading social cues, mood instability, and temper problems. Temporal lobe problems are very common in resistant depression.
Beth, twenty-five, came to see us after her fourth suicide attempt. She had problems with depression and her temper since she was a child. Her moods would fluctuate wildly and she could never predict how she would feel. When she was three years old, she fell down a flight of stairs and was unconscious, but only for a brief period of time. Beth had been on many different antidepressants without success. Beth’s brain SPECT scan showed clear problems in her left temporal lobe. For many years now, we have seen trouble in this part of the brain be associated with dark, evil, awful, destructive thoughts, including both suicidal and homicidal thoughts. None of the medications she had been put on were specifically to help stabilize her temporal lobes.
|
Normal Brain SPECT Scan 
Full, even, symmetrical activity |
Temporal Lobe Brain Type 
Low left temporal lobe |
I have found antiseizure medications to be particularly helpful for this brain type. In addition, balancing blood sugar, by eating small meals four to five times a day, making sure to get good sleep, and eliminating sugar are also very helpful. With this combination of treatment, Beth’s moods stabilized and she was able to stay out of the hospital and restart college.
In this brain type we see overall low activity in the brain. There are many potential causes of this brain type, including:
• Drug or alcohol abuse
• Environmental toxins, such as mold, paint, or solvents
• Past chemotherapy or radiation
• Brain infections, such as meningitis or encephalitis
• Lack of oxygen, such as with a strangulation, near drowning, or sleep apnea
• Heavy metal poisoning, such as with lead, iron, or mercury
Patients with this pattern often feel depressed or sad, have low energy, and are mentally foggy and cognitively impaired.
Will came to see us for resistant depression and brain fog. He had seen six other psychiatrists and had tried numerous medications. He was feeling hopeless, helpless, and worthless. He had frequent suicidal ideas and his family was extremely worried about him. He looked much older than his sixty-three years. His brain SPECT scan showed overall low activity.
This is the classic pattern we see in a toxic brain. I met with him and his wife. He said, and she confirmed, that he did not drink or use drugs. Our first efforts needed to be directed at finding why he had such a toxic-looking brain. After extensive lab and environmental testing, we discovered that he had been working in an office that had extensive mold growth. The office had experienced a flood the year before he first became depressed. Other co-workers also suffered with cognitive impairment.
|
Normal Surface Brain SPECT Scan 
Full, even, symmetrical activity |
Will’s Toxic Surface Brain SPECT Scan 
Overall decreased activity |
The first step in treating this type of brain is to eliminate the toxin. If a person is drinking or doing drugs, that must stop in order to heal. If there is mold in the environment, that must be fully treated before the person can return to work. If there is severe anemia or hypothyroidism, it is essential to treat it. If there was a loss of oxygen from chemotherapy or radiation, then we know the culprit and can go straight into brain rehabilitation.
People who have experienced emotional trauma sometimes develop lifelong stress patterns in the brain, especially if they had vulnerable brains when the traumatic events appeared. On SPECT scans we see that the brain takes on a specific pattern. We call it the diamond-plus pattern, because on scans the pattern appears in the shape of a diamond:
• Increased activity in the anterior cingulate gyrus at the top of the diamond (negative thoughts)
• Increased activity in the deep limbic system at the bottom of the diamond (feelings of sadness)
• Increased activity on the outside of the right temporal lobe (this is the “plus” part of the diamond-plus pattern), where we think some traumatic memories are stored
|
Normal “Active” Brain SPECT Scan 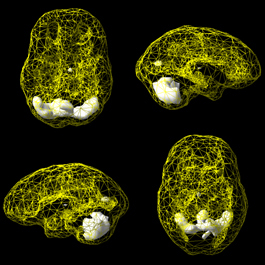
Most active areas in cerebellum at back of the brain |
PTSD Type 
Diamond-plus pattern |
The scans show a pattern where it looks as though the trauma or traumas get stuck in the brain.
Frank, sixty-six, was the CEO of a large company. He came to see us because his memory was poor and he struggled with anxiety, depression, and excessive alcohol use. His wife had given him an ultimatum to get help or she was going to divorce him. Frank denied having any emotional trauma in his history. His scan displayed the diamond-plus pattern. All of the overactivity in his brain helped us understand why he drank so much. He was trying to put out the fire in his brain that made him feel terrible. But the alcohol made him irritable, and his wife was nearly finished with the chronic stress he gave her. Seeing the diamond pattern led me to ask more pointed questions about past trauma. Again, he denied it. Being the persistent soul that I am, I asked him repeatedly. He kept saying no. When I brought his wife into my office, I asked her. She looked at her husband and said, “Frank has a bad relationship with his father.”
“Why is that?” I asked Frank.
“When I initially made a lot of money, I bought a home for my mother but not my father, and he has held a grudge against me ever since.”
“Why did you just do it for your mom?” I asked.
“When I was growing up in the poor part of Chicago, my parents were separated and I was raised by my mom. My dad was not around. But my mom was a drug addict and often not home. When I was a young adult, she got clean and I wanted to help support her getting well.”
“And you have no emotional trauma in your past?” I said, wondering how he could forget the years of being raised without a father by a drug-abusing mother. My, how the brain can block out pain; it is indeed a sneaky organ.
It was at that moment that Frank’s face changed and he started to sob. He had forgotten all of the times when his mother did not come home, when he was left alone, when he thought she was dead, or when she brought over men who were very scary to him. Frank was loaded with trauma he had never processed, and subsequently the trauma still lived, wreaking havoc, blocked in his emotional brain. His overactive brain caused him emotional pain and he used alcohol to try to put the brain fires out. Of course, the alcohol brought him all sorts of other problems and made him more distant from those he loved.
To calm the diamond-plus pattern and eradicate the past emotional traumas seen on scans, we often refer people to a special psychological treatment called EMDR, or eye movement desensitization and reprocessing. I published a study a number of years ago on using EMDR with six police officers who developed post-traumatic reactions after being involved with shootings. At the beginning of the study all of the officers were out of work on stress leaves. After eight to ten sessions their brains were calmer and they all went back to work. You can learn more about EMDR at www.emdria.org. We also have people engage in all the longevity and brain healthy strategies listed in this book.
It is common to have more than one of the eight brain types listed above. If that is true for you, work on the most painful type first and then the others. You can also join our online community at www.theamensolution.com to learn more about your own brain and what to do with combination patterns. Also, when people struggle with resistant problems, a brain SPECT scan can provide additional valuable information.
One of the techniques that significantly helped Chris heal from her grief was ANT therapy, or learning how to not believe every stupid thought that went through her brain. She learned how to challenge and question the negative thoughts running around her brain. At the Amen Clinics we call it learning how to kill the ANTs. When the ANTs, those negative thoughts that pop up in your brain automatically and seemingly out of nowhere, are left unchecked they steal your happiness, torment you, and can literally make you old, fat, depressed, and feebleminded.
The following exercise to kill ANTs is so simple that you may have trouble believing how powerful it is, but it can change your whole life. Your suffering diminishes and your health and happiness improve. A number of research studies have found this technique to be as effective and as powerful as antidepressant medication for depression.
1. Whenever you feel sad, mad, nervous, or out of control, draw two lines vertically down a piece of paper, dividing it into three columns.
2. In the first column write down the ANTs going through your brain.
3. In the second column identify the type of ANT. Therapists typically describe nine different types of ANTs (see table below).
4. In the third column, talk back, correct, and eradicate the ANTs. Were you good at talking back to your parents when you were teenagers? I was excellent. In the same way, you need to learn to be good at talking back to the lies you tell yourself.
| ANT | Type of ANT | Eradicate the ANT |
| I will never be happy again. | Fortune-Telling | I am sad now, but I will feel better soon. |
| I am a failure. | Labeling | I have succeeded at many things. |
| It is your fault! | Blame | I need to look at my part in the problem. |
| I should have done better. | Guilt Beating | I will learn from my mistakes and do better next time. |
| I am old. | Labeling | I am getting younger every day. |
Summary of the Nine Different Types of ANTs
1. Always Thinking: Thoughts that overgeneralize a situation and usually start with words like always, never, everyone, every time
2. Focusing on the Negative: This occurs when you only focus on what’s going wrong in a situation and ignore everything that could be construed as positive
3. Fortune-Telling: Predicting the future in a negative way
4. Mind Reading: Arbitrarily believing you know what another person thinks, even though she has not told you
5. Thinking with Your Feelings: Believing your negative feelings without ever questioning them
6. Guilt Beatings: Thinking in words like should, must, ought, or
have to
7. Labeling: Attaching a negative label to yourself or others
8. Personalization: Taking innocuous events personally
9. Blame: Blaming other people for the problems in your life
Another ANT-killing technique that I teach all of my patients is called the Work. It was developed by my friend Byron Katie and explained so well in her book Loving What Is. Katie, as her friends call her, described her own experience suffering from suicidal depression. She was a young mother, businesswoman, and wife in the high desert of Southern California. She became severely depressed at the age of thirty-three. For ten years, she sank deeper and deeper into self-loathing, rage, and despair, harboring constant thoughts of suicide and paranoia. For the last two years, she was often unable to leave her bedroom and care for herself or her family. Then one morning in 1986, out of nowhere, Katie woke up in a state of amazement, transformed by the realization that when she believed her thoughts, she suffered, but when she questioned her thoughts, she didn’t suffer. Katie’s great insight is that it is not life or other people that makes us feel depressed, angry, stressed, abandoned, and despairing: It is our own thoughts that make us feel that way. In other words, we live in a hell of our own making, or we live in a heaven of our own making.
Katie developed a simple method of inquiry to question our thoughts. It consists of writing down any of the thoughts that are bothering us or any of the thoughts where we are judging other people, asking ourselves four questions, and then doing a turnaround. The goal is not positive thinking but rather accurate thinking. The four questions are:
1. Is what I’m thinking true?
2. Can I absolutely know that it’s true?
3. How do I react when I believe that thought?
4. Who would I be without the thought? Or, put differently, How would I feel if I didn’t have the thought?
After you answer the four questions, you then take the original thought and completely turn it around to its opposite and ask yourself whether the opposite of the original thought that is causing your suffering is not true or even truer than the original thought. Then turn the thought around and apply it to yourself and to the other person (if another person is involved in the thought).
Here’s an example: Rosemary’s husband of thirty-four years died of cancer. Rosemary was the alumni director at my college and we have been friends for many years. After John’s death she was very sad and lonely. I helped her work through some of her grief. Two years after John died, Rosemary wanted to start dating again. She loved being in a close relationship. But she told me, “No one would ever want a seventy-five-year-old woman.” So we did the Work on that thought. First I asked her this series of questions:
1. Is it true that no one would ever want a seventy-five-year-old woman? “Yes,” she said. “I am too old to date.”
2. Can you absolutely know that it is true that no one would ever want a seventy-five-year-old woman? “No,” she said. “Of course I can’t know that for sure.”
3. How do you feel when you have the thought “No one would ever want a seventy-five-year-old woman”? “I feel sad, hopeless, angry at God, and overwhelmed by my loneliness,” she answered.
4. Who would you be or how would you feel if you didn’t have the thought “No one would ever want a seventy-five-year-old woman”? “Well, I would feel much happier, more optimistic. I would feel like my usual self,” she said.
Then I coaxed her to turn the original thought around. “No one would ever want a seventy-five-year-old woman.” What is the opposite? “Someone will want a seventy-five-year-old woman.” Okay, so which is truer? “I don’t know,” she said, “but if I act like no one will want me, then no one will want me.” After our exercise, Rosemary started dating again.
A year later she met Jack. When I sat with Rosemary and Jack for the first time it felt like I was with two fifteen-year-olds who had just fallen in love. They were married the next year and will soon celebrate their five-year anniversary.
All of us need a way to correct our thoughts. Just think about what would have happened to Rosemary if she hadn’t killed the ANTs that were stealing her happiness and robbing her joy. She would have died a lonely old woman. I have seen these four questions dramatically change people’s lives. They can do the same for you.
Leroy “Satchel” Paige overcame racial discrimination to break into major-league baseball as a pitcher at the age of forty-two. After a career spanning forty years, he was elected to the Baseball Hall of Fame in 1971. When asked about his prowess at an age when most players are long retired, Paige responded by asking: “How old would you be if you didn’t know how old you was?” Excellent question.
Research shows that people with positive, optimistic attitudes about aging outlive those who have a negative, pessimistic view of getting older, by an average of more than seven years.
How powerful is attitude? In the book Counter Clockwise, author Ellen Langer writes: “Simply having a positive attitude made far more difference than any to be gained from lowering blood pressure or reducing cholesterol which typically improve life span by about four years. It also beats the benefits of exercise, maintaining proper weight, and not smoking, which are found to add one to three years.”
Drowning out ANTs is vital in recovering from loss and the stresses of life, but it can also be a life-lengthening skill when it comes to how you think, specifically, about aging. Visualizing yourself happy, engaged, and healthy as you get older is a wonderful exercise that may add years to your life.
1. When going through stress, grief, or depression many people are tempted to self-medicate with alcohol, not realizing that alcohol is a depressant! It numbs you from the good, healing feelings of connection and empathy with others that help you traverse grief and pain. Excessive alcohol really only delays and multiplies pain. Say no to alcohol and yes to a healthy healing path.
2. Because loss takes such a hit on our brain and body, it may help you, like it helped Chris and Gerald, to focus on going “hard core” into getting healthy. Getting radically healthy gives your brain and body something positive to throw yourself into and yields positive rewards, emotionally and physically.
3. Long-term caretaking takes a huge toll on the caretaker. Remember to “nurture the nurturer,” and learn the art of radical self-care. If you do not replenish yourself while caring for others, you may not be there for them for long. Let others pitch in and take a break to go for a walk, read something inspiring, see a funny movie, or take a guilt-free nap.
4. Take Chris’s tip and make sure you don’t get stuck somewhere without nutritious food or drink. Almonds or walnuts are a great portable snack to keep in your car, briefcase, or purse. “Treat yourself like a good parent would treat a child so you don’t end up somewhere hungry, thirsty and cranky,” especially during stress or loss.
5. Don’t let a loss or tragedy leave you a one-dimensional person completely defined by your loss. You are a person who experienced and survived a great sorrow, yes. And you are a person with gifts, talents, and a boatload of compassion to share. Honor the memory of your loved one by taking care of your health and living a full, rich life of benevolence.
6. When you begin to feel anxious or upset you may be dealing with ANTs. Learn to develop an internal anteater to recognize and eliminate these pesky creatures.
7. Question your thoughts. One of the best ways to eliminate the ANTs is to constantly question your negative thoughts. Whenever you feel sad, mad, nervous, or out of control, write down your negative thoughts, ask yourself if they are really true, and start talking back to them. You do not have to believe every thought you have. This exercise can help shift your perspective from negative to positive in seconds and will begin to become automatic with practice.
8. Situational depression is a normal part of grief. Time, tears, reaching out to others, and taking care of yourself will normally ease the pain. But complicated grief or chronic depression that leaves you with suicidal thoughts or unable to cope after many months needs to be treated like a medical emergency. Seek help for this kind of grief immediately. We help many people who are “stuck in grief” through the wonderful resources at our clinics.
9. As Chris pointed out, there is much in life over which we have no control. All the more reason to take charge over what you can control: namely your health and happiness, especially after a setback or sorrow. Love yourself and tend to your brain by feeding yourself well, taking yourself out for nice walks or runs, and speaking kind words to yourself.
10. Because grief is draining, you may be tempted to say no to invitations from friends. Try saying yes more often, pushing past the automatic desire to seclude. Being with loving, patient people is healing to a brain overwhelmed by grief. Getting out also gives your brain much-needed “breaks” from overthinking and sadness.
11. The brain can become overfocused on the person you lost, to the exclusion of others who need you. When grief is new, try setting aside a specific time each day to focus on and think about the person you lost: Journal, cry, pray, or whatever you need to do. Then let it go, and turn your mind to others who need you to be fully present for them. Practice the art of “being here now.”
12. Don’t underestimate the power of changing your diet for the better, adding exercise and a few brain-smart supplements (like vitamin D and fish oil) to quickly turn a low mood around. Feeling better provides its own motivation. Once you experience a lift in mood after tending to your brain and body, you’ll be hooked on the feeling.
13. If you have an impulsive brain type, you will be helped by more dopamine. Higher-protein, lower-carbohydrate diets tend to help, as do exercise and certain stimulating medications or supplements, such as green tea or L-tyrosine. Calming supplements or medications can actually make this brain type worse.
14. If you have a compulsive brain type, you may have a very hard time letting go of painful negative thoughts. Serotonin is calming to this brain type. Physical exercise boosts serotonin, as does using certain supplements, such as 5-HTP or St. John’s Wort.
15. If you have an impulsive-compulsive brain type, you may impulsively reach for something unhealthy, then compulsively get “stuck” on doing it over and over. You need to increase both serotonin and dopamine. A combination of exercise with a calming supplement like 5-HTP (to boost serotonin) and green tea (to boost dopamine) can help balance the brain naturally.
16. If you have a sad or moody brain type, you tend to feel depressed, which can also make you feel achy all over and lethargic. For this type, we recommend exercise, a high-dose fish oil (6 g), and certain supplements, such as SAMe, to help improve mood, energy, and pain.
17. If you have an anxious brain type, you may feel tense, nervous, and unsettled inside. Exercise, meditation, hypnosis, and a combination of vitamin B6, magnesium, and GABA may be helpful.
18. If you have a temporal lobe brain type, you may struggle with memory and learning difficulties, mood instability, dark thoughts, and/or temper problems. Anti-seizure medications, along with balancing blood sugar and getting good sleep, are usu-
ally helpful.
19. If you have a toxic brain type, you may suffer with mental fogginess, low energy, and cognitive impairment. Drug or alcohol abuse and environmental toxins are two common causes. Eliminate the toxins and get on a brain healthy program.
20. Boost omega-3s (fish or fish oil) and vitamin D levels to help counteract a low mood.