IN THIS CHAPTER
Planning ahead for your first weeks of breastfeeding
Designing your breastfeeding spaces
Buying bras, shirts, and gowns
Making your first attempt at breastfeeding
If you’re reading this chapter, you’ve probably weighed the positives and negatives of breastfeeding and have decided to at least try it. This chapter helps you look at your post-delivery schedule and how breastfeeding will fit into your life, offers advice on how to set up a functional nursery, and makes a few wardrobe and paraphernalia suggestions that can make breastfeeding easier and more comfortable. This chapter also helps you through the first breastfeeding after delivery.
Evaluating Your Postpartum Schedule — Realistically!
What do you imagine happening after you deliver your baby? If your life were a TV show, you might find yourself in a dreamy haze, sitting in a rocking chair with your baby sleeping peacefully in your arms. Perhaps you’d wear a long dress and have your hair pulled back in a soft, matronly style. Your baby would be dressed in a rose pink (or sky blue) handmade outfit. The hard work would be over, and you’d finally be able to relax.
Well, forget it. The end of pregnancy is the start of your new, sleep-deprived existence. And if you plan on returning to work, you have to consider how to breastfeed while you work.
Time management tips
Yes, new motherhood is an exciting, sweet time, but then there’s all the rest. Many women go wrong by setting themselves on a post-delivery course that no woman could possibly maintain without a staff of four to help.
 The time to consider postpartum time management techniques is long before you ever feel the first labor pain. Consider these examples:
The time to consider postpartum time management techniques is long before you ever feel the first labor pain. Consider these examples:
- You may be feeding the baby every two to three hours when you first get home, so don’t plan to host a major event — your parents’ 40th anniversary party or a Cub Scout Jamboree — in your house for at least several weeks.
- If you have older children in school or daycare and belong to a carpool, try to beg off for a few weeks. If your child’s nursery school has after-school care, consider utilizing it a day or two each week so you can catch up on sleep — or at least get the kitchen cleaned.
- Ask your partner to take time off work if his workplace offers paternity leave. If that’s not possible, ask your mom, sister, or best friend to help out for a few days.
- If your church or another social group has a program that provides meals for the sick, take advantage of it; a casserole or two may last through the better part of the first week home.
- Hire a cleaning service once a week for the first few weeks. Looking at dust and clutter can push you over the edge when you’re sleep deprived.
- Don’t view your maternity leave as a wonderful time to get major household projects done, such as remodeling the bathroom. You may think you’ll have lots of time for this sort of thing, but you won’t!
- Sleep whenever possible. Really.
The need to rest can’t be overemphasized, so don’t try to jump right back into your old routine the minute you get home. Too much running around decreases your milk supply, slows your healing, and makes you cranky!
Considering your return to work
The last thing you may be thinking about as you prepare to deliver your baby is what life will be like when you have to go back to work. But continuing to breastfeed after you return to work is a challenge, so you’d be wise to consider your situation before you go on maternity leave.
Ask yourself these questions:
- Where is the best place to pump? An office with a door that locks is ideal, but if you don’t have that luxury, you’ll need to get creative.
- Are your supervisors and coworkers supportive of breastfeeding? If you don’t know the answer to that question, now is the time to start having conversations about your plans.
- Can you arrange your schedule to go home at lunchtime and nurse?
- Has anyone in your office ever breastfed? If so, ask that person for advice.
Arranging Your Space and Amassing Supplies
When you start arranging your nursing space, you’ll probably set up two areas. First, of course, is the baby’s room. You’ll probably do most of your night feedings here, and visitors usually want to see this space first so they can oooh and ahhh over the cute decorating job. During the day, you may spend most of your time in your family room or living room.
Nesting in the nursery
Curtains that match the crib sheets are very nice and will satisfy your form over function needs, but other items are more essential for a comfortable breastfeeding experience:
- Topping the list is a comfortable place to sit, whether you prefer an upholstered chair, a wooden rocker, or a glider.
- A footstool or ottoman elevates your feet and knees, bringing the baby closer to your breasts. This position can reduce neck, shoulder, and back strain. Some ottomans are too high for comfort, so you may want to look for a special nursing stool. Alternately, you can get creative and make your own from a kitchen step stool.
- A table by your chair is a must, because you need burping cloths, baby wipes, a clock, and receiving blankets within arm’s reach. And having a drink next to you at each feeding is a great reminder to keep your fluid intake up while you’re breastfeeding.
Setting up space in the family room
Hide and seek is fun when you’re 10 but not when you’re a new mom and you have to disappear into the nursery to breastfeed every time company arrives. Arranging your nursing space in the family room is the start of public breastfeeding. Setting up a comfortable spot allows you to feed the baby discreetly and still be part of the action in the house.
 Having a nursing spot set up in the middle of the action is good only if you’re comfortable with it. When you first come home from the hospital, you may feel comfortable nursing only in front of your partner — and maybe not even him! Be direct about your needs for privacy, even if that means kicking everyone out of the family room for a while. Ask your partner for help telling your family and friends to give you space; he may enjoy having an active role to play as “keeper of the gate.”
Having a nursing spot set up in the middle of the action is good only if you’re comfortable with it. When you first come home from the hospital, you may feel comfortable nursing only in front of your partner — and maybe not even him! Be direct about your needs for privacy, even if that means kicking everyone out of the family room for a while. Ask your partner for help telling your family and friends to give you space; he may enjoy having an active role to play as “keeper of the gate.”
If you have other children, you need to decide if you’re comfortable nursing in front of them. Of course, depending on their ages, you may not have a choice.
 If you have toddlers, arrange your nursing area so they can sit next to you. That way, they won’t climb on top of the kitchen cupboards every time you nurse. Have favorite books or puzzles handy, prepare a snack for them before you begin nursing, and encourage them to watch the baby make funny faces.
If you have toddlers, arrange your nursing area so they can sit next to you. That way, they won’t climb on top of the kitchen cupboards every time you nurse. Have favorite books or puzzles handy, prepare a snack for them before you begin nursing, and encourage them to watch the baby make funny faces.
If you plan to nurse in front of your children or other people, you may want to arrange the furniture in your family room so your nursing chair isn’t center stage. Perhaps set your table and chair behind the couch or in a corner. Unless you want all eyes on you, definitely don’t put your chair right next to the TV! Keep in mind, also, that as the baby grows, he’ll be distracted by what’s going on around him. He may nurse better if you’re away from the action.
Your furniture and equipment needs for the family room are similar to those in the nursery:
- A comfortable chair is still a must, although you may choose to use the corner of the couch. Your impulse might be to go for a great overstuffed chair, but be warned: Many overstuffed chairs are too deep to sit in comfortably, unless you’re tall. If you’re short, your feet will stick straight out in front of you — not comfortable for the long haul!
- A table within easy reach will hold not only the breastfeeding essentials but also the remote control, a magazine, and a snack or two!
- Lots of extra pillows are helpful, especially when you’re just learning how to nurse.
Breastfeeding in your bedroom
If you choose to share your room with your baby, at least for the first few months, keep the following in mind:
Breastfeeding paraphernalia
In addition to a comfy chair and a quiet place, you need a few more things to stock your breastfeeding nursery.
A breast pump
Every nursing mom, whether staying at home or going back to work, should have a breast pump. How exotic the pump is up to you. You can buy a manual, battery operated, or electric breast pump:
- Manual pump: Manual pumps may work for occasional pumpers. They’re easy to find and easy to assemble, but they’re not always easy to use. The big plusses of manual pumps are that they’re inexpensive, compact, portable, and quiet. They don’t have moving parts that could break, and they don’t require electricity or batteries to operate. They’re also easy to find; most pharmacies have them in stock. The downside? Many women are able to get only a scant amount of milk using a manual pump, and some pumps can bruise or scrape your nipples.
- Battery-operated pump: These tend to have more disadvantages than advantages. Their energy is supplied by AA batteries, so you may need to buy stock in a battery company. It takes eight to ten seconds to build up suction, so a battery-operated pump takes longer to use than a regular manual pump. They’re also slower than electric pumps because they have less power. The advantage of a battery-operated pump is it’s easier to maneuver than a manual pump and just as portable. If you don’t think that you’ll need to pump on a regular basis, a battery-operated pump may work for you.
- Electric pump: If you pump frequently, an electric pump is the only way to fly! It requires only one hand to use; imitates your baby’s sucking action, even down to number of sucks per minute (48 to 60); and comes in models that allow you to pump both breasts at one time. Most women find electric pumps more effective than other pumps in getting milk out of their breasts. The disadvantages? They’re larger, making them less portable and more conspicuous; they’re more expensive than others ($200 to $300 isn’t uncommon); and they’re not quiet. These pumps are work horses, and they often sound like it!
 If possible, don’t start pumping until your milk supply is well established — at least four weeks after delivery.
If possible, don’t start pumping until your milk supply is well established — at least four weeks after delivery.
Discuss pumps with a lactation consultant before purchasing one; she’ll probably recommend that you get your feet wet with breastfeeding before investing in a pump. Pumps can be expensive, and you can’t return them after they’ve been used, so you want to make as informed a decision as possible. The consultant can also provide information about renting a pump; be sure to ask.
Resting on nursing pillows
To be comfortable while nursing, you’ll probably want to tuck pillows behind you for back support and under your arms to help support the baby. A pillow on your lap brings your baby closer to the breast. You can use plain bed pillows for this purpose, or you can splurge with special nursing pillows.
 Make sure the pillow you use is firm; if it’s too soft, the baby will sink into it and not get any higher on your lap. A plastic cover over the pillow is essential. (No matter how much disposable diapers improve, they still can leak!) Most nursing pillow covers are washable, and some pillows are as well.
Make sure the pillow you use is firm; if it’s too soft, the baby will sink into it and not get any higher on your lap. A plastic cover over the pillow is essential. (No matter how much disposable diapers improve, they still can leak!) Most nursing pillow covers are washable, and some pillows are as well.
Stocking Your Wardrobe
No one ever said nursing shirts and nursing bras were glamorous, but they’ve made great strides over the last 20 years. Whether you’re a stay-at-home mom or chair of the board, you need to get dressed in the morning in clothes that are comfortable and conducive to nursing.
Trying on nursing bras
 Wearing the proper nursing bra provides breast support and makes you more comfortable. You should buy two or three all cotton nursing bras in the final weeks of your pregnancy. At this time, your cup size will be its closest to your post-delivery size.
Wearing the proper nursing bra provides breast support and makes you more comfortable. You should buy two or three all cotton nursing bras in the final weeks of your pregnancy. At this time, your cup size will be its closest to your post-delivery size.
Most maternity shops, department stores, and undergarment specialty stores carry nursing bras. Wherever you go, make sure that the person helping you knows how to measure and fit you. Proper fit is the key to comfort with any type of bra.
 When you try on a nursing bra, bend over and gently “shake” your breasts into the cups. A well-fitted bra should cover the entire breast; no part of the breast should spill out. The bottom band should be snug, but the bra shouldn’t put pressure on your breasts. If the bra is too tight, it could cause a milk duct to become plugged or mastitis (infection) to develop. The bra shouldn’t ride up in the back, and the straps should keep your breasts elevated without cutting into your shoulders.
When you try on a nursing bra, bend over and gently “shake” your breasts into the cups. A well-fitted bra should cover the entire breast; no part of the breast should spill out. The bottom band should be snug, but the bra shouldn’t put pressure on your breasts. If the bra is too tight, it could cause a milk duct to become plugged or mastitis (infection) to develop. The bra shouldn’t ride up in the back, and the straps should keep your breasts elevated without cutting into your shoulders.
 When considering cup size, keep in mind that you may need room for a breast pad or breast shell. For band size, buy a bra that you can fasten on the inside row so you have more hooks to expand to after your milk comes in.
When considering cup size, keep in mind that you may need room for a breast pad or breast shell. For band size, buy a bra that you can fasten on the inside row so you have more hooks to expand to after your milk comes in.
Make sure your bra flaps are easy to open and close. You don’t want a bra that requires neighborhood assistance to open! Opening the flap should be a one-hand operation; you want to be able to hold your baby in one arm and slip up your top and undo the flap with the other. Some bras have clips, and some have snaps to hold the flap up; you may want to try them both to see which is easier for you to manage.
Nursing bras can be expensive but are worth the investment. Don’t be surprised if you need to buy bras in different sizes as time goes by. You may even find yourself back in your regular bra months down the road. At this point, you can use the lift and load routine — just lift your bra up off the breast and load the baby on.
 You don’t have to wear a bra. Some women like that born free (or hang free, at least) feeling. But wait until you’re an advanced breastfeeder before ditching your bra. Your breasts need support in the beginning — at least for the first month. Some women even wear their bras to bed in the beginning because it’s more comfortable.
You don’t have to wear a bra. Some women like that born free (or hang free, at least) feeling. But wait until you’re an advanced breastfeeder before ditching your bra. Your breasts need support in the beginning — at least for the first month. Some women even wear their bras to bed in the beginning because it’s more comfortable.
Looking chic in nursing shirts
Nursing shirts (and gowns) can be helpful, especially at first. When you wear a nursing shirt, you don’t have to bare all to feed the baby. There’s a slit in the front of the shirt; you just slide the slit over your breast to give the baby access. The time may come when you feel so comfortable with nursing that you wouldn’t care if the President of the United States were in the same room with you. But until then, these “peek-a-boob” aids are helpful.
 Of course, you don’t need special shirts to nurse. If you’re comfortable, just place a receiving blanket over your baby, and he’ll cover the rest.
Of course, you don’t need special shirts to nurse. If you’re comfortable, just place a receiving blanket over your baby, and he’ll cover the rest.
Using pads, shields, shells, and creams
Breast pads, nipple shields, and breast shells all fit into your bra, but they have very different functions. The simplest and the one almost everyone needs? Breast pads.
Stopping leaks with breast pads
In the first few weeks of nursing, you may experience a considerable amount of leakage! Breast pads are absorbent cotton pads that collect milk that leaks out of the nipple until your let-down reflex (see Book 5, Chapter 1) is better controlled. Breast pads (also called nursing pads) bear a strong resemblance to sanitary napkins, which can actually be cut down to size and used for this same purpose.
 You can purchase boxes of disposable breast pads, or you can choose washable cotton pads, which are more cost-effective if you don’t mind adding to your laundry pile.
You can purchase boxes of disposable breast pads, or you can choose washable cotton pads, which are more cost-effective if you don’t mind adding to your laundry pile.
Some pads are contoured, and some are more like flat circles. If you buy contoured, keep in mind that the contour of the pad may not fit your particular contour! On the other hand, flat pads slide around more easily and are more noticeable through your shirt. Some brands come with sticky strips to hold them in place in your bra.
Covering your nipples with a shield
Nipple shields are sometimes recommended to help draw out flat or inverted nipples (refer to Book 5, Chapter 1) or protect sore nipples. The shields are made of soft plastic or silicone and fit over the entire areola. You need to moisten the back of the shield to help it adhere to your skin. You wear the shields while breastfeeding. Nipple shields should be used only as a last resort.
 Most lactation consultants agree that sore and cracked nipples are caused by poor positioning and/or improper latch-on (see Book 5, Chapter 1). Nipple shields are only a temporary measure to help your nipples heal or help your baby latch on when all else fails. Using shields for long periods may decrease your milk supply, so use them only under the supervision of a lactation consultant or physician.
Most lactation consultants agree that sore and cracked nipples are caused by poor positioning and/or improper latch-on (see Book 5, Chapter 1). Nipple shields are only a temporary measure to help your nipples heal or help your baby latch on when all else fails. Using shields for long periods may decrease your milk supply, so use them only under the supervision of a lactation consultant or physician.
Wearing breast shells
Breast shells are quite different from nipple shields. Shells are never worn while nursing; they’re used between feedings or before the baby arrives to help draw out flat or inverted nipples or to collect leaking milk.
Shells come in several pieces, as shown in Figure 2-1. The piece that fits next to the breast puts gentle compression to help draw out flat or inverted nipples (discussed in Book 5, Chapter 1). The outer piece fits over the top and usually has air holes to allow circulating air to keep the nipple drier. Leaking milk collects in the shell; some brands have a little spout you can use to pour the milk into a bag or bottle if you’re storing breast milk.
 Unless you’re able to dump the milk immediately after it leaks, don’t save it. Milk that sits in the shell may grow bacteria.
Unless you’re able to dump the milk immediately after it leaks, don’t save it. Milk that sits in the shell may grow bacteria.
 Make sure the spout points upward when you put the shell on, or milk will pour all over you when you remove it! Also make sure the air vents are at the top; if they’re on the bottom, milk comes right back out through the little holes.
Make sure the spout points upward when you put the shell on, or milk will pour all over you when you remove it! Also make sure the air vents are at the top; if they’re on the bottom, milk comes right back out through the little holes.
During nursing, you can wear a breast shell on the breast you’re not using, to prevent you from getting soaked during let-down and also to help collect milk.
Coating your nipples with creams
Sometimes all you need to heal sore nipples is a little air drying; other times, you may need lotions or creams. Most creams are food grade and lanolin-based. Food grade means the cream doesn’t need to be removed before you feed the baby.
One disadvantage to creams is that they’re often yellow and somewhat greasy, meaning they can stain your clothes. Wear a breast pad, unless you’re not concerned with staining your nursing bras, and try to keep the baby’s clothes away from the cream. You need to use only a tiny dab of cream; it spreads a little easier if you warm it by rolling it between your fingertips before applying.
 Some types of creams absolutely should not be used on your breasts when nursing. Among them are alcohol-based products, which make nipples more prone to crack; petroleum-based products, which don’t allow the skin to breathe; and vitamin E-based products, which may be toxic to the baby. Look for ultra-purified lanolin ointment, which is pharmaceutical grade and safe for breastfeeding.
Some types of creams absolutely should not be used on your breasts when nursing. Among them are alcohol-based products, which make nipples more prone to crack; petroleum-based products, which don’t allow the skin to breathe; and vitamin E-based products, which may be toxic to the baby. Look for ultra-purified lanolin ointment, which is pharmaceutical grade and safe for breastfeeding.
 One of the best things you can use to help heal your nipples is free: your own breast milk! Dab a little of your milk on sore nipples and let it dry thoroughly.
One of the best things you can use to help heal your nipples is free: your own breast milk! Dab a little of your milk on sore nipples and let it dry thoroughly.
Nursing for the First time: Breastfeeding at the Hospital
In some hospitals (or if you deliver at home), your baby is placed on your naked abdomen immediately after delivery. With your doctor, nurse, partner, and mom all staring expectantly at you, you try to position the baby to nurse. Watch out — he’s slippery! What on earth is your doctor doing down there? Is that the placenta? This tender moment may be a little awkward, with everything else that’s going on distracting your efforts.
Starting off on the right foot
 Try to ignore everything else going on around you and concentrate on the baby. Eye-to-eye and skin-to-skin contact are the best ways for you and the baby to get acquainted. If possible, don’t be rushed. Sometimes nurses want to give you a one-minute token bonding session and then grab the baby away to be weighed, measured, eye-dropped, cleaned, and brought back after the doctor has put you back together. Sometimes space is tight in labor and delivery, and two or three more couples are waiting for your room.
Try to ignore everything else going on around you and concentrate on the baby. Eye-to-eye and skin-to-skin contact are the best ways for you and the baby to get acquainted. If possible, don’t be rushed. Sometimes nurses want to give you a one-minute token bonding session and then grab the baby away to be weighed, measured, eye-dropped, cleaned, and brought back after the doctor has put you back together. Sometimes space is tight in labor and delivery, and two or three more couples are waiting for your room.
Obviously, if your baby isn’t breathing well or needs to be evaluated immediately, you won’t be able to hold him right away. But if at all possible, hold him for a little bit. He may or may not be ready to nurse right after delivery; watch for clues, such as rooting (turning his head looking for the nipple) or sucking his hands, which show he’s ready to start nursing. Doing so may save you from some frustrating first attempts to nurse before he’s ready.
If your baby is taken to the warmer to be cleaned up first because that’s the way things are done at Rules-Oriented Hospital, don’t get upset. When the nurses finish, they’ll bring the baby back to you.
 If you’re too distracted by the doctor pulling and tugging as he sews up your episiotomy or any tears, wait to start breastfeeding until he’s finished. Try to concentrate on one major event at a time. Some women are uncomfortable and afraid to hold the baby while the doctor is stitching; if that’s the case, ask your partner to hold the baby close to you so you don’t have to worry about dropping him.
If you’re too distracted by the doctor pulling and tugging as he sews up your episiotomy or any tears, wait to start breastfeeding until he’s finished. Try to concentrate on one major event at a time. Some women are uncomfortable and afraid to hold the baby while the doctor is stitching; if that’s the case, ask your partner to hold the baby close to you so you don’t have to worry about dropping him.
Sooner or later your doctor will finish putting you back together, and you can concentrate on the baby. After a minute or two of gazing into each other’s eyes, you’re ready for the big moment: your first breastfeeding.
Positioning the baby for comfort
Right after delivery, a healthy baby who is left alone will crawl up to his mother’s breast, find his own position, latch on, and begin suckling. If you’re giving birth in a hospital, your baby probably won’t be given that opportunity.
Most likely, a nurse will hand you your baby after the initial weighing and measuring rituals are out of the way. Unless you’ve had a cesarean delivery (refer to Book 2, Chapter 5), you’ll probably be sitting up or semi-reclining, and you’ll naturally cradle the baby in the crook of your arm to get ready to breastfeed.
 You can position the baby for breastfeeding in many different ways, and changing positions helps the baby empty different duct areas in the breast. The positions described here are most common, but as you become more experienced, you can certainly try others.
You can position the baby for breastfeeding in many different ways, and changing positions helps the baby empty different duct areas in the breast. The positions described here are most common, but as you become more experienced, you can certainly try others.
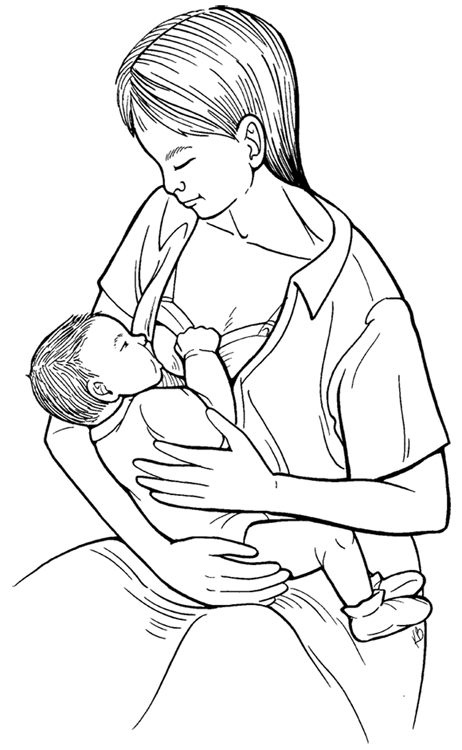
The cradle hold position
The cradle hold (or Madonna position) is the traditional baby holding position. With the cradle hold, the baby’s head rests on the crook of your arm, and you support his legs and back with your forearm (see Figure 2-2). If you’re using the left breast, his head is in your left arm. Turn the baby toward you, chest to chest. (Skin to skin is wonderful if you can manage it.) You may want to put a pillow under the baby to support his weight and bring him up to breast level. Fold a pillow in half and place it under your arm, with the fold up along your side. This keeps your arms at breast level and supports them comfortably during the feeding. Use your free hand to position and support your breast.
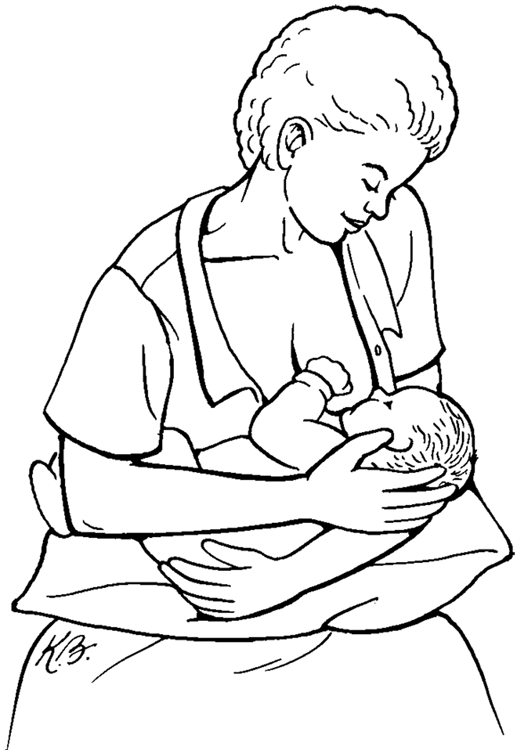
The cross cradle hold
With the cross cradle (or reverse cradle) hold, the baby’s head is supported with the left hand if you use the right breast. The baby’s body is supported by the rest of your arm (see Figure 2-3). If you’re feeding off the right breast, your right hand supports the breast. Turn the baby toward you, chest to chest. This position works well for a baby who has trouble latching on, because you have control of his head and can see his mouth better. This is also a good position if your baby arrives early; a preterm baby’s head is big in relation to the rest of his body, and his neck muscles are weaker.
Latching on properly — the key to breastfeeding success!
Getting the baby to latch on to your breast properly is crucial. Latching on properly helps prevent sore nipples and ensures that your baby gets enough milk.
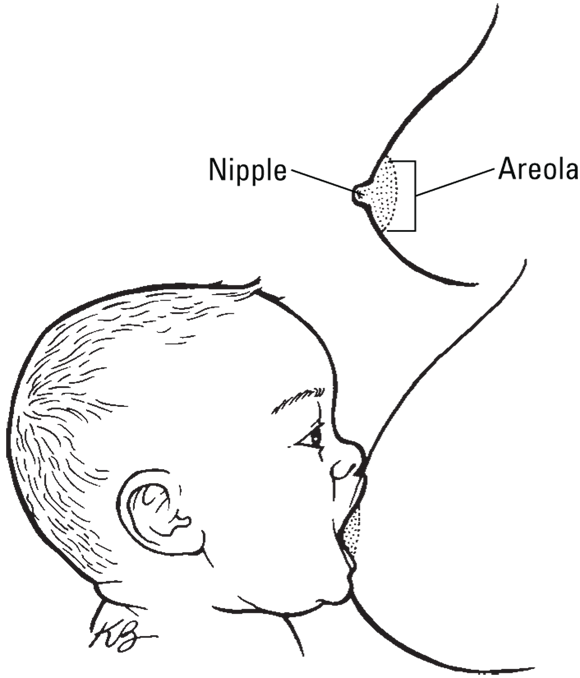
Make sure you’re comfortable in the bed. If you’re lying at a funny angle or don’t have a good grip on the baby, adjust yourself. Hold the baby on his side so he doesn’t need to turn his head to reach the nipple. You and the baby should be chest to chest. Bring the baby close to your breast, with his nose lined up with your nipple.
You may need to use your fingers to support your breast and make it easier for the baby to grasp the nipple. Place your thumb on the top of your breast and, forming a C, place your other four fingers below the breast to lift up. Make sure your fingers and thumb are resting on the breast tissue, not on the areola. If your breasts are very large, place a rolled-up towel in the fold underneath to give support.
 Don’t touch both the baby’s cheeks at the same time in an effort to turn his head in the right direction. He’ll turn toward anything touching his cheek, and if you touch both, you’ll confuse him. Tickle his lips with the nipple; don’t try to force it into his mouth.
Don’t touch both the baby’s cheeks at the same time in an effort to turn his head in the right direction. He’ll turn toward anything touching his cheek, and if you touch both, you’ll confuse him. Tickle his lips with the nipple; don’t try to force it into his mouth.
Some babies bobble their heads back and forth wildly, looking for the nipple; others find the nipple easily but don’t seem all that interested in sucking. Try to calm the bobbler down by teasing his lower lip with the breast so he’ll turn toward it. If you have a bobbler, try using the cross cradle hold, which gives you better control to guide his head where it needs to go. If he finds the nipple but doesn’t seem all that interested, give him a little time. Some babies want to lick the nipple for a few minutes before they nurse.
When your baby opens his mouth wide, move his mouth toward the nipple. Move the baby, not the breast. If you have a perfect baby who’s read all the books, he’ll turn slowly toward the nipple, open his mouth wide, pull the areola and the nipple into his mouth, and begin sucking. More likely, he’ll find the nipple, open his mouth halfway like a guppy, and get frustrated and turn away because he can’t get it into his mouth. Or he’ll root wildly, passing the nipple a dozen times but never grabbing onto it. Keep trying — it’ll happen eventually!
When the baby is latched on well, an inch or so of the areola is in his mouth. His lips are rolled out, his tongue is under the breast, and his chin is touching your breast. His nose should be resting on top of your breast, not buried in it. Figure 2-4 shows what a proper latch-on looks like.
Several things need to take place in a perfect latch-on:
- The baby needs to open his mouth wide.
- He needs to close his mouth on the areola, not just the nipple.
- He needs to begin sucking so that the nipple and areola are pulled into his mouth to form a teat. The nipple makes contact with a spot where the baby’s hard and soft palate meet; touching this spot stimulates more sucking.
- The baby needs to coordinate his ability to suck and swallow.
Removing the baby from the breast
 If you need to remove the baby from your breast, break the suction by inserting your finger between your breast and the baby’s mouth. Press gently on the areola and remove the nipple from the baby’s mouth. If you pull the baby off without breaking the suction first, you could injure your nipple.
If you need to remove the baby from your breast, break the suction by inserting your finger between your breast and the baby’s mouth. Press gently on the areola and remove the nipple from the baby’s mouth. If you pull the baby off without breaking the suction first, you could injure your nipple.
Feeling frustrated? It’s normal
If your baby hasn’t read any of the books and doesn’t seem to understand the concept of nursing at all, don’t worry. If your baby is the wild man type, throwing his head back and forth like the MGM lion but never getting near the nipple, don’t worry. If she just brushes past the nipple without even opening her mouth, don’t worry. Immediate success is nice, but it’s not essential.
Try not to get upset at yourself or the baby. You’re both brand-new at this, and breastfeeding is a coordinated, learned activity. Remember how long it took you to learn to ride a bike? Think of nursing the same way.
Relaxing during the first feeding
The point of the first nursing is for you and your baby to get to know each other. You’re not going anywhere, and neither is the baby. You don’t absolutely need to complete the first feeding in the first hour after delivery, although the baby may be very alert in the first hour or two and then sleep deeply for several hours.
 If you feel as though you’re accomplishing nothing in your first feeding, rest assured that’s not the case. You’re establishing contact; the baby begins to know your smell. You’re starting the bonding process. If your baby nurses well, he gets some high-calorie colostrum to carry him through the next few hours and begins to learn the mechanics of breastfeeding. Even if the baby just licks the nipple, you’re starting to stimulate milk production, and you’re stimulating your uterus to contract.
If you feel as though you’re accomplishing nothing in your first feeding, rest assured that’s not the case. You’re establishing contact; the baby begins to know your smell. You’re starting the bonding process. If your baby nurses well, he gets some high-calorie colostrum to carry him through the next few hours and begins to learn the mechanics of breastfeeding. Even if the baby just licks the nipple, you’re starting to stimulate milk production, and you’re stimulating your uterus to contract.
All that, on top of labor and delivery! You’ve had a busy day, so have something to eat and drink and take a nap. Your next nursing attempt will go better if you’re taking care of yourself.
 The time to consider postpartum time management techniques is long before you ever feel the first labor pain. Consider these examples:
The time to consider postpartum time management techniques is long before you ever feel the first labor pain. Consider these examples:  Having a nursing spot set up in the middle of the action is good only if you’re comfortable with it. When you first come home from the hospital, you may feel comfortable nursing only in front of your partner — and maybe not even him! Be direct about your needs for privacy, even if that means kicking everyone out of the family room for a while. Ask your partner for help telling your family and friends to give you space; he may enjoy having an active role to play as “keeper of the gate.”
Having a nursing spot set up in the middle of the action is good only if you’re comfortable with it. When you first come home from the hospital, you may feel comfortable nursing only in front of your partner — and maybe not even him! Be direct about your needs for privacy, even if that means kicking everyone out of the family room for a while. Ask your partner for help telling your family and friends to give you space; he may enjoy having an active role to play as “keeper of the gate.”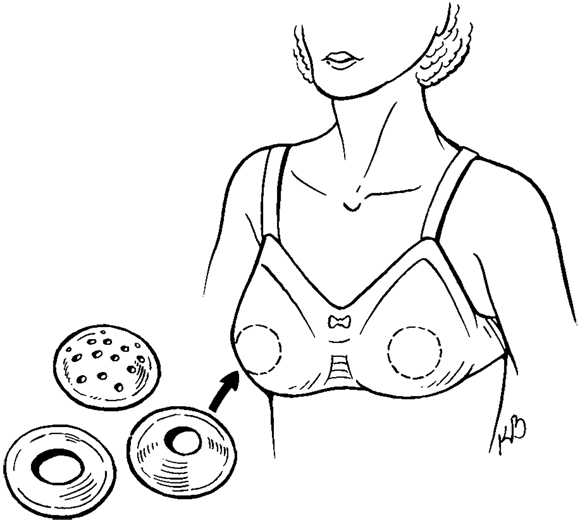
 Unless you’re able to dump the milk immediately after it leaks, don’t save it. Milk that sits in the shell may grow bacteria.
Unless you’re able to dump the milk immediately after it leaks, don’t save it. Milk that sits in the shell may grow bacteria.