

DOMESTIC AND CHILD VIOLENCE, DRUG OVERDOSE, AND SUICIDE
Sometimes emergencies occur that test us both physically and mentally. Domestic violence is a national disaster and a national disgrace. It can happen in any household, to the elderly, adults, and children alike. Victims often feel helpless and hopeless. You may be, in fact, a victim. Abuse can occur at the hands of a spouse, loved one, or family member, and there may be threats of death that compound a victim’s inability to act on their own behalf.
Violence can take the form of physical abuse, beatings, even rape, but it can also be psychological and verbal abuse that breaks down the victim and immobilizes them with shame and fear. Sometimes the abuser threatens to kill a beloved pet, a child, or a family member as a power play to get the victim to accept the abuse and keep quiet about it.
According to the Centers for Disease Control and Prevention, one in four women and one in seven men will experience physical violence at the hands of their partner in their lifetimes.
One in ten women will be raped or sexually assaulted and abused by their partner in her lifetime.
Eight percent of all men will experience sexual abuse at the hands of an older person, even a relative.
Approximately 10 percent of all women and almost 3 percent of men have been stalked.
Nearly half of all women and men in the United States alone will experience some form of psychological abuse in their lifetime.
Domestic violence of every kind occurs to whites, people of color, lesbians, gays, heterosexuals, all ages, all creeds, all nationalities. There don’t seem to be any boundaries or exemptions when it comes to this type of crime. Intimate-partner sexual abuse can turn into murder or murder-suicide. Family members, friends, and neighbors may have no idea of the turmoil that goes on behind closed doors until it makes the nightly news.
With adult domestic violence, the abuse often begins slowly and builds up over time as a systematic pattern of control and power. Frequency of abuse can vary and often is hard to predict, even if the abuser is drunk or abusing drugs. Anger and rage seem to be a predecessor, and abusers often take out their own deep problems using others as their punching bags. What makes abuse so difficult is that often the abuser will apologize profusely for their actions and beg forgiveness, promising never to do it again. In addition, if the abuser is the “breadwinner,” the spouse will take the abuse because they simply don’t have anywhere else to go, especially if they have no supportive friends or family to turn to. Or the victim will be so afraid they will be killed, they give in to the abuser’s every whim. Even when an opportunity to escape presents itself, they are numb and blind to it because of how they have been conditioned and weakened to a state of absolute helplessness.
Often people comment on how strange it is that victims of abuse stay and don’t leave sooner. Unless you have experienced the pervasive and often insidious types of abuse to body, mind, and spirit, you cannot possibly know what keeps victims from acting on their own behalf, and often it comes down to just not knowing there is the option of escaping the abuse. Psychological torture may not be as visible as bruises on the skin or a broken arm, but the aftereffects are agonizing and soul-destroying to the already terrified victim. Some signs of abuse are:
•Showing extreme jealousy if the victim goes out with friends
•Telling the victim they are worthless and cannot do anything right
•Controlling who the victim sees and what they wear
•Taking the victim’s money from a job and keeping it
•Shaming the victim in public with put-downs
•Forcing sex on the victim
•Stalking and monitoring the victim’s every move, including cell phone use
•Threatening to kill the victim’s pet, child, mother, father, friends
•Not permitting the victim to leave the house
•Not allowing the victim to have a say in anything
•Pressuring the victim to use alcohol or drugs
•Destroying the victim’s personal property
Whether it is outright beatings or psychological abuse, you have an obligation to yourself and your sanity and health to leave someone who is hurting you and find a safe place.
Abuse can range from subtle pressure to outright brutal beatings. The only way for a victim to survive is to get out and get help. It is easier said than done, but if you are the victim, call a friend or loved one who can come and help you pack up your things and your children when the abuser is not home and get you to a safe place. If you have been beaten, call the police and press assault charges. Do not be taken in by false apologies.
If you have children, you must get them to safety. Do not confront your abuser. Work behind the scenes to get out and get to a safe place.
If you cannot call anyone, try to text someone or alert a neighbor that you are in trouble and need help.
Do not call the abuser later and tell them where you are, no matter how much you miss them.
The National Domestic Hotline Number is available twenty-four hours a day, seven days a week, for anyone who is not sure what steps to take to get out and get safe. Call 1-800-799-7233 (SAFE).
Don’t wait for things to get better. They won’t. If the abuser isn’t getting help, you can be assured the abuse will not only continue, but possibly get worse, and you may end up dead.
Don’t depend on a restraining order to keep the abuser away. Protect yourself, and buy a weapon if you feel you need to. Learn how to use it properly. Many victims end up dead after leaving an abusive relationship because they get back in contact with the abuser or let the abuser know where they are.
If you suspect someone else is being abused, ask them directly. If you get the feeling they are being evasive, offer to help them get to safety. They may still refuse your help out of fear for their own life, and possibly even fear for yours if you get involved. Let them know you are willing to help and that they can come to you when they feel safe doing so.
If someone has bruises and broken limbs, and you know they are from domestic abuse, call the police. Too often we ignore the signs or brush them under the rug so as not to make waves, only to find out later the victim was beaten to death. Make the waves and let the police step in.
If you take someone in, realize you may be putting yourself in danger. It is best that you get the victim away from the abuser, but get them to a domestic violence shelter where they are equipped to deal with threats you may not be.
Child abuse is even more challenging. Often we see other people being abusive to their children in public, and we don’t know whether it crosses the line. If a child looks terrified, has bruises and broken bones, and cowers when struck by the adult, it might be safe to assume they are being abused at home too. It is hard to know what to do in this situation. You can step in and tell the parent you are going to call the police, or if you know the child, keep a record of times you’ve suspected abuse, and make a case. You can go to a child’s teacher in confidence and discuss your concerns.
Child abuse often goes unreported, so actual accurate statistics are difficult to find. Children between the ages of 4 and 7 and between 12 and 16 are at the greatest risk, according to the National Child Traumatic Stress Network. However, very small children, including infants, are the most susceptible to serious, if not grave, injuries.
Like adult domestic abuse, child abuse can be physical, sexual, psychological, or a combination of all three. Children will often be covered in bruises beneath their clothing, but sometimes the bruises are visible enough to concern someone. If a child ever tells you they are hit at home or being abused in any way, call the police and child protective services in your area immediately. Do not confront the parents. Get the child help so an authority figure can take the child away from the abuser before it is too late.
Some signs of abuse include:
Physical marks and bruises, bite marks, burns, lacerations, abrasions, loose and missing teeth, broken teeth and bones, black eyes, split lips, difficulty sitting or walking, and excessive crying.
Psychological marks include withdrawal, not speaking, cowering when touched, cringing when touched, not looking you in the eye, not looking away from the abusive parent, staying home from school often, and general anxiety and fear.
Children who are being hit by their parents will not in general want to implicate their parents and may lie. They also fear more abuse if they tell an adult what is happening. Often parents excuse abuse as “spanking” or disciplining a child, but abuse is abuse and often involves a parent’s lack of patience and inability to control anger and temper. But sometimes the parent is just cruel and vicious.
Ask a child open-ended questions about any bruises or marks you see. Look for inconsistencies in their answers, and see if their explanation matches the injury. Ask them if they sleep well or have nightmares. Often abused children suffer from nightmares and night terrors and appear very sleepy during the day. They may also act out aggressively, especially against pets and other children they feel they have some power and control over. Abused children have trouble concentrating and often worry excessively, to the point of paranoia, about themselves and their parents, especially if the parents are not the abusers. The child may feel that they need to know where the parents are at all times and feel unsafe and vulnerable when they are not protected, such as at school or a friend’s house.
A child will not open up to you if you are a stranger or they feel unsafe around you. They may not even open up to close relatives such as aunts and uncles. But the signs of abuse are there if you are alert and aware, and if you see the child all the time, patterns will reveal themselves in their behaviors, actions, and reactions. If you think a child you know may be a victim of abuse and are not sure what to do, contact the Childhelp National Child Abuse Hotline at 1-800-422-4453. In imminent dangerous situations, call 911.
Be careful if you try to get the child out of the home yourself. Parents don’t give up their children easily, and you may be mistaken about the situation in the first place. Even if you aren’t, the parents may resort to violence against you.
DRUG AND ALCOHOL OVERDOSE
Millions of Americans are addicted to alcohol, hard drugs, and prescription drugs. Addiction has become a pandemic that grows in size and scope every year. Because many people don’t seek treatment, we have no real way of knowing just how many people are out there drinking and drugging to extremes until something happens. They bottom out and end up on the side of the street, beaten up and robbed, in detox in the downtown police station, or worse.
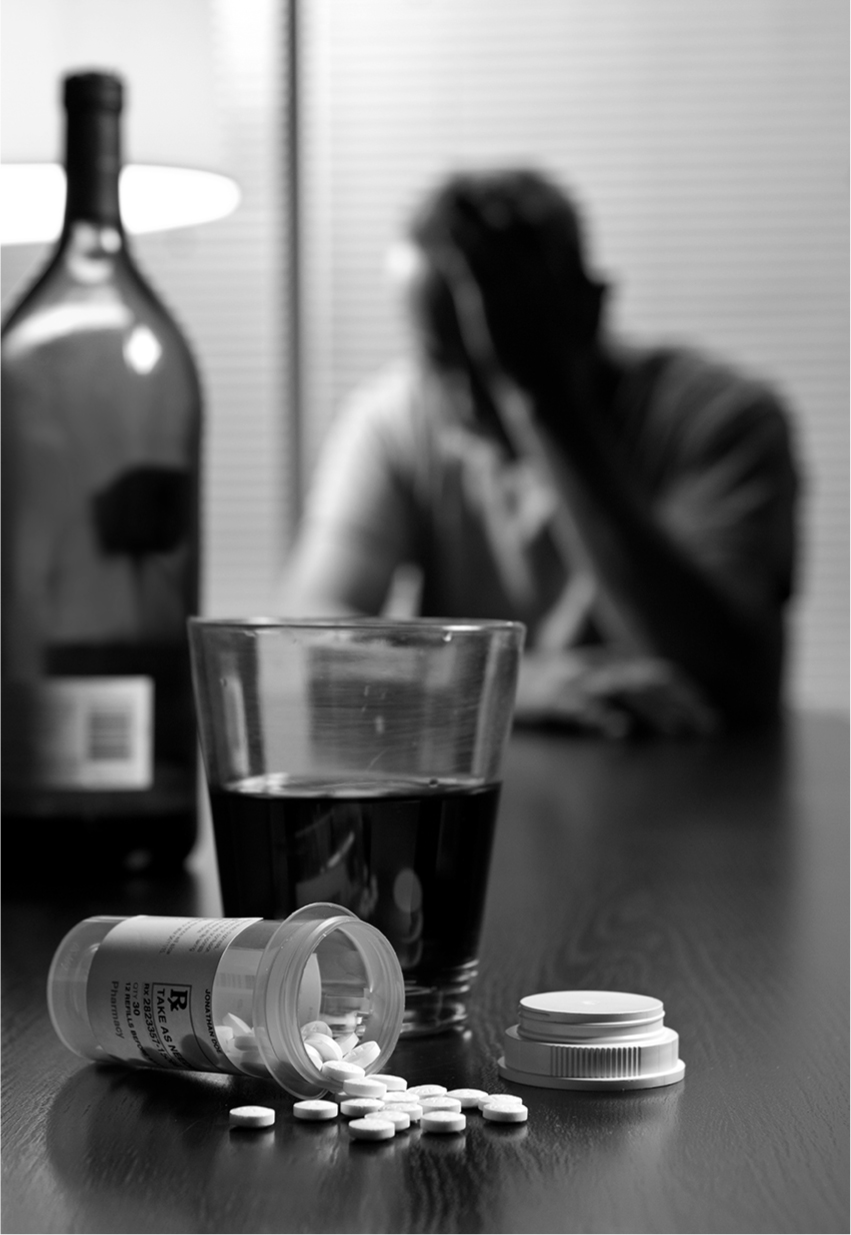
In a society in which going out for drinks or using prescription drugs is considered normal, it can sometimes be difficult to assess if someone is descending into addiction.
Drug abuse plagues all age groups, genders, and nationalities. Drug dependency is considered a disease and requires serious treatment at a rehab facility or hospital or even a twelve-step program. But too many drug and alcohol abusers continue to believe they can handle their addictions and get better either by going cold turkey or slowing it down a bit. It doesn’t usually work out well.
Drugs can be taken orally as pills and liquids or inhaled or injected. There are always signs that someone is abusing drugs and alcohol, but in our society, where we go for drinks at the drop of a hat and consider popping prescription pills for every symptom imaginable, it can be hard to distinguish between someone who has a problem and someone who doesn’t.
Overdoses occur after the fact, sadly, and sometimes it is too late to save a person by then. But the best prevention for overdosing is helping yourself or a loved one or friend get help for their addiction before things go too far. You can assist them in seeking an outpatient or inpatient rehab facility, preferably one their insurance will cover or partially cover, and even go with them to twelve-step meetings and encourage them to speak and tell their stories. You can remove drugs and alcohol from the home, but expect a real abuser to find them elsewhere.
If someone is abusing drugs or alcohol and becomes violent, you can call the police and have them taken in, usually to an overnight detox. Don’t ever allow violence of any kind to exist in your home, especially when children are involved. Turning someone in is often the best thing that could happen to them, as most abusers need to “bottom out” in order to admit they have a problem and seek help.
Whatever you do, don’t let anyone drink or drug and get behind the wheel of any vehicle.
If someone overdoses, you will either find them conscious or unconscious. If they are unconscious, begin checking their ABCs, and call 911 immediately. Give rescue breathing and CPR as needed. If you have help, have the other person look around for signs of the drug used, such as needles, cocaine powder, heroin residue, spoons, tinfoil and matches, prescription bottles, and empty alcohol bottles and containers. Have those ready for the emergency responders when they arrive so they know the cause of the overdose.
If the person is conscious, keep them awake, and elevate their legs above heart level to avoid shock. Do not move them, and keep them as calm and quiet as you can. If they can speak, ask what happened. Often the victim took an accidental overdose of too many prescription pills. But sometimes they were having suicidal thoughts. Do not leave them alone until help arrives, and let EMS know what the person’s intentions were. Often a medical sensitivity can cause symptoms of an overdose, so the more information you can give EMS, the better.
In the case of chemicals, plants, or toxic substances inhaled or ingested to get a “high,” the higher the dose and the longer the body is exposed to the toxin, the worse the poisoning will be. Act quickly to get help. If you can identify what was inhaled or ingested, be ready to report that to EMS.
Young children can overdose on drugs too, and it is imperative that medications be kept out of their reach. Toddlers often find bottles of pills and share them with other kids, thinking they are candy. Children put everything into their mouths, so this is playing with danger in the most extreme way. Sticking pill bottles on a high shelf may not be enough, because children are curious and will find a way to get to something that catches their eye. If a child overdoses, get help immediately. Their bodies are smaller, and the toxin will act more powerfully.
Effects of alcohol poisoning are:
•Seizures
•Vomiting
•Loss of consciousness
•Low body temperature
•Bluish tint to the skin
•Irregular or slow breathing
Effects of cocaine or crack:
•Sweating profusely
•Fast and irregular heartbeat
•High blood pressure
•Jitters
Effects of heroin/opiates:
•Slow breathing
•Difficulty breathing
•Weak pulse
•Low blood pressure
•Tiny, pinpoint pupils
•Disorientation
•Loss of consciousness
Effects of methamphetamine (meth):
•Confusion
•Jitters
•Aggression
•Convulsions
•Extreme paranoia
•Rapid heart rate
•Rapid breathing
•High body temperature
Even before an overdose, an abuser may display changes in their sleep patterns, the way they dress, their hygiene, behavioral changes that border on the extreme, withdrawal from family and friends, talk of suicide and death, lying and stealing, violent or criminal behavior, and extreme mood swings. These are all indications that something is wrong and needs to be addressed in order to avoid an even worse situation. As with domestic violence and child abuse, there are many red flags with drug and alcohol abuse. It is just a matter of being aware enough to see them.
One possible sign of drug addiction is when you notice a family member or friend no longer cares about their appearance or keeping their living space clean.
Often teenagers who are using drugs and alcohol to try to cope with life will become strangers to their parents. They may even stop seeing their friends and participating in school activities they once loved. They no longer care if they shower, how they look, and even their eating patterns may change. Their rooms are a mess, and often a parent with hawk eyes will find evidence of substance abuse. If you suspect your teenager is using, confront them but do it with care and compassion. Ask to see their phones if you think they are buying from friends. Check into their Web use, and breach privacy boundaries, because you might be saving their lives by doing so.
Teens do drugs and drink alcohol to feel better, but also to fit in, so watch the behavior of their friends, and if you suspect one of their friends is using drugs and encouraging your child, confront the other child’s parents. Don’t be an ass. Believe it or not, they may be asking the same questions about your child. Try to find the source of the drugs and alcohol, and refuse to allow your child to interact with those persons.
If someone appears to be overdosing, call for help and try to keep them calm. If they are having seizures, move dangerous objects out of the way so they don’t injure themselves. Keep them calm, and try to keep them still until help arrives. Try to find out what the substance is and how much of it they consumed. Keep the person warm and watch for possible shock. Someone who is on meth will be all over the place. If you can safely keep them somewhat restrained, it will keep them safe until help arrives, but if you are alone, simply do the best you can, and always protect your own health and safety first and foremost.
If the victim overdosed on prescription drugs, there may be instructions on the pill bottle for what to do in the event of an overdose. There should also be a number for poison control: 800-222-1222. Don’t call your local doctor or pharmacist to ask what you should do. Call 911 so that the victim will get help quickly, as you don’t know what they took or how much or how it will interact with their metabolic system. They may have even mixed drugs intentionally or by accident.
Prescription Drug Abuse
Prescription drug abuse is a growing problem in this country. Most people don’t bother to keep their prescription medications out of the reach of children, teenagers, and anyone who might be having suicidal thoughts. But how can we safely dispose of meds we don’t need to use? Throwing them away is the easiest thing to do, but is it the best?
According to “How to Safely Dispose of Unused Medication” in the Fall 2017 issue of Lifelines, the magazine of the American Association of Retired Persons (AARP), some medications will actually include disposal instructions on their labels or on the dosage information sheet that comes with the medication. Follow those instructions, because not doing so could cause unintentional harm to others.
Flushing medications is no longer suggested, because of the overwhelming amounts of prescription drugs found in our nation’s water sources. This is becoming a big medical problem as drugs containing hormones, sedatives, and painkillers get flushed into our wastewater and then out into rivers and even the ocean. You are better off throwing the pills away, but first take the pills out of their original packaging, and place them in a small bag with dirt or cat litter covering them. Seal the bag, and then throw it in the outdoor trash bin so that children and pets cannot dig the pills out of the trash inside the house.
Last, but not least, you can participate in a local Take Back program. Your pharmacist will know of these programs. This allows you to drop unwanted medications off at various local collection sites, usually at clinics or hospitals, where they can be safely disposed of. You can find a local Take Back program by calling the Drug Enforcement Administration at 1-800-882-9539.
Be aware that under the Good Samaritan law, if someone is in a life-threatening situation, you must call 911 immediately, so do that first before anything, unless you have help who can do that while you try to administer life-saving techniques. Some states may not have this law, so know the rules in your area. In any event, if you have any reason to fear getting involved, just get away, and call for help. If it’s a drug deal gone bad or the abuser is out of control, it could put your life at risk or put you in a very dangerous situation.
After the person gets immediate help, and they are treated by a hospital, encourage them to get professional rehab help. You may even want to do an intervention if it is a family member and the pattern of abuse continues. Ongoing drug and alcohol abuse take a toll on more than just the abuser. Users and addicts are adept at trying to downplay their diseases and won’t ask for help unless they hit bottom, and maybe not even then. If they don’t get help, they risk not only their own lives, but the lives of innocent others they may harm in a DUI or a bad drug deal.
It is one of the top ten leading causes of death in the United States, with over 44,000 people dying each year. It can happen to anyone, regardless of race, color, creed, social status, gender, or age. It costs the nation over $50 billion annually, and for every one suicide, there are approximately twenty-five more failed attempts.
Suicide is a topic nobody wants to talk about, but it is pandemic, and statistics show it is on the rise. According to the American Foundation for Suicide Prevention, approximately 13 in 100,000 people take their own lives, with men three times more likely than women to die, but women three times as likely to attempt suicide. There are on average 121 suicides each day, almost half of which involve the use of firearms. The rate of suicide is highest in middle age, and white men are hit the hardest. In 2015, 19.6 percent of suicides were among adults between the ages of 45 and 64, with the second highest percentage, 19.4 percent, being people over the age of 84. We think of suicide as a teenage crisis, and it indeed is, but it truly does affect everyone. Suicide is the second highest cause of death in children and young adults between the ages of 15 and 34.
The method of suicide is often firearms, almost 50 percent in 2015, with suffocation (including hangings) second at 26.9 percent, and poisoning third at 15.4 percent. Attempted suicides sent over 500,000 people to local hospitals from injuries due to self-harm, and these were only those who chose to seek help. So many others suffer, or die, in silence.

Suicide is pandemic in the United States. It affects people of all ages, not just troubled teenagers, with about 44,000 dying annually in America alone.
Suicide is rampant, and now with cyberbullying, it is something we need to pay even closer attention to with our children, who may be influenced by total strangers to go out and end their lives.
Ninety percent of those who die by suicide have some type of mental health disorder at the time of death, and had they been able to seek or receive treatment, it might have spared their lives. When it comes to preventing suicide, it is critical we all learn the signs of behavior that may be leading up to such a drastic cry for help and often an attempt to end suffering and pain we may not even know the person was in.
According to the National Institute of Mental Health, some of the risk factors we can look for (in ourselves and others) are:
•Depression and anxiety disorders
•Family or marital problems
•Drugs and alcohol abuse
•Family history of suicide
•Guns and firearms in the home
•Family violence and past abuse
•Incarceration
•Chronic health issues and chronic pain
•Prolonged stress from job, bullying, school, expectations of others, abuse
Someone who may have just suffered a huge personal loss, such as the death of a loved one, a bankruptcy, loss of a job, or a natural disaster, can be at high risk as well. This is especially true for seniors who are mourning the passing of a spouse.
Signs someone may be contemplating suicide include:
•Direct threats
•Veiled threats
•Withdrawal from normal activities
•Loss of interest in hygiene and eating and sleeping
•Sleeping disturbances
•Behavioral changes
•Depression and despair
•New behavior patterns
•Drinking and drugging
•Isolating themselves from friends and family
•Acting out aggressively
•Contacting people to say goodbye
•Aggression
•Purchasing guns
•Feelings of humiliation and worthlessness
•Rage
•Mental health symptoms such as bipolar, or manic-depressive, behaviors, conduct disorder, and even antisocial personality disorder
•Excessive use of the Internet, which can indicate possible cyberbullying and attempts to stop it
Getting treatment means first getting help. Whether you fear that you may take your own life or that someone you love may take their life, get help immediately. You can start by calling the toll-free National Suicide Prevention Lifeline at 1-800-273-TALK (8255), which is available twenty-four hours a day, seven days a week, and is free and completely confidential. There is also a crisis text line, 741741. You can also talk to your doctor about getting mental health treatment set up, which can involve medications for depression and anxiety, talk therapy, cognitive behavioral therapy, or other kinds of healing modalities such as psychotherapy, electroconvulsive therapy, alcohol and drug abuse counseling, and more. If an at-risk person is given a medication, they need to be monitored for possible side effects that might increase their desire to end their lives.
To start, here are five steps recommended by the National Institute of Mental Health:
1.Ask the person if they are thinking of suicide. This does not increase their desire to do so, and may open the door to allow them to express the feelings that are making them feel hopeless.
2.Keep the person safe by removing anything they can use to commit suicide, such as guns, knives, pills, etc.
3.Be there for them if they want to talk, and listen carefully. Just acknowledging suicidal thoughts can help reduce the thoughts.
4.Help them connect and get help by giving them the suicide hotline number and naming other trusted individuals they can turn to if you are not available.
5.Stay connected even after they have gotten help and are back home feeling better. Studies show that suicide deaths decrease when someone follows up with an at-risk person.
Going beyond suicide, we need to be aware of the dangers of mental illness that is not being addressed or treated, as it can make the victim feel alone, vulnerable, ashamed, and worthless. Knowing the signs can help us help others and possibly give them the hope they are missing and the feeling of being cared for. Suicide is a double-edged sword that not only takes the lives of those we love, but in a way, destroys our own lives as well. If someone you love or know commits suicide, be sure to reach out for the help you may need to process and heal from the sudden and shocking death. You may suffer from the guilt and shame that comes from feeling as though you should have known or you could have stopped it. Know that if someone is determined to take their life, they will do so no matter what in many instances, and it is impossible to know the innermost thoughts going through someone’s mind, especially if they are acting normal on the outside.
Grieving the death of a loved one is hard, but even harder when they died by their own hand and those left behind are wondering how and why. Be gentle with yourself, reach out and talk about it with trusted friends, and get professional help if you are having trouble moving on from the tragedy.