CHAPTER 35
Blood Gas Analyzers and Point-of-Care Testing
Introduction
Point-of-care testing (POCT) is defined as tests designed to be used at or near the site where the patient is located; they do not require permanent dedicated space, and they are performed outside the physical facilities of the clinical laboratories. POCT has grown in popularity as advancements in computer chip technology have made POC devices more affordable, portable, and easy to use. Examples include circulating blood glucose monitors (glucometer), blood gas analyzers, activated clotting time (ACT) monitors, and heparin concentration monitors (Hepcon). There are a myriad of other POCTs used in and out of the operating room that are not discussed in detail in this chapter. Some examples of these POCT devices include those for testing hemoglobin A1c (HbA1c), microalbumin, cardiac enzyme markers, cholesterol, and infectious disease. POCT can be found almost anywhere patients need quick and cost-effective testing such as a physician’s office, ICU, emergency rooms, hospital wards, and even in a patient’s home. However, this chapter gives a brief overview on POCT equipment that is commonly found in or around the operating room. The main emphasis of this chapter is on the organization of POCT from initial startup to daily operations.
The operating room is a unique environment in which a life-threatening situation needs to be identified and treated immediately. For example, hypoglycemia can lead to poor neurologic outcomes, cardiovascular collapse, and death if not identified and treated promptly. The clinician cannot wait for the long turnaround time required for tests sent to a central laboratory. Even STAT labs have a much longer turnaround time than POCT. A handheld glucometer allows the clinician to quickly detect the patient’s circulating blood glucose and perform the appropriate intervention. The most efficient use of POCT occurs when an abnormality is quickly detected and an intervention is performed before any harm or escalation of patient care has occurred.
POCT is composed of five essentials: equipment, personnel (not trained as certified laboratory personnel), procedure, quality control, and records and reports. It is governed by the College of American Pathologist (CAP) and Clinical Laboratory Improvement Amendments (CLIA). CLIA issues the certificate that allows the laboratory to function, and CAP is the regulatory body that governs daily operations. The POCT laboratory allows no disruption of patient care, samples never leave the immediate patient care area, and the results are immediate. Clinicians must guard against interpreting POCT as having the same accuracy as the main laboratory. When there is a question of the results, the best rule of thumb is to draw another sample and perform a test on the POCT machine and to send a sample to the central laboratory for comparison.
Blood Gas Machine
A blood gas machine is a portable system that analyzes whole blood for pH, partial pressure of CO2 and O2, bicarbonate levels (HCO3−), electrolytes, lactate, and hematocrit. There are a multitude of clinical scenarios in which an anesthesiologist may need these values to assess a patient. A blood gas sample may be obtained from an artery or a vein depending on the clinical situation as the blood gas values will differ and will yield different information for the clinician. Arterial blood gases are most commonly obtained from the radial artery, as it is easily accessible. Figure 35.1 shows a modern POC blood gas machine.
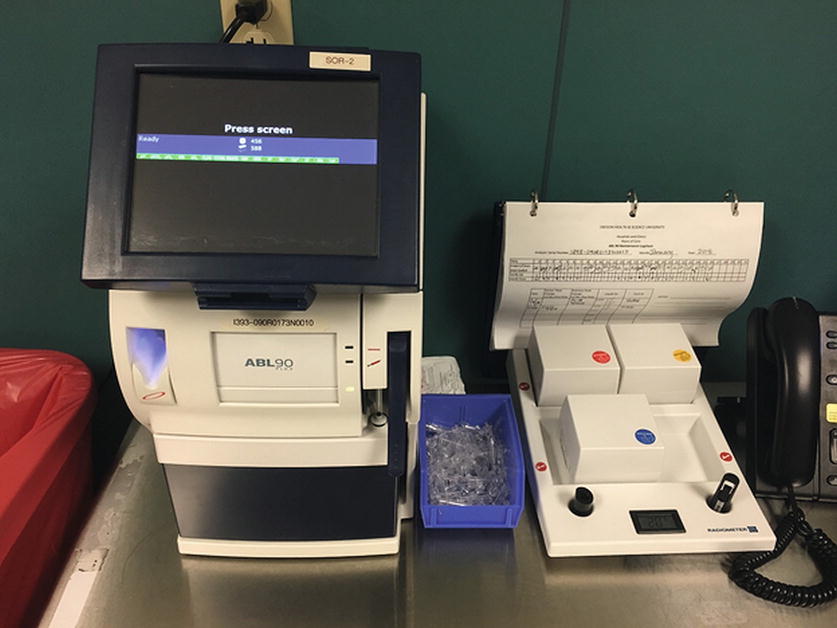
FIGURE 35.1. A modern blood gas machine. Notice that this machine has QC supplies and logbook nearby, also a phone to relay urgent results.
The blood sample is drawn into a heparinized syringe to prevent the blood from clotting. A patient identifier should be placed on the syringe if it is transported away from the operating room. The blood sample is then taken to the blood gas analyzer where the sample is drawn into the machine for analysis. Blood gas analyzers today are fast and accurate. Most instruments are fully self-contained, consisting of the machine and disposable cartridges containing reagents, sensors, waste containers, and quality control (QC) pack. Usual systems are fully automated with self-calibration and self-quality control.
Although today’s blood gas analyzers are accurate, there are many preanalytic errors that can occur, which can give erroneous results:
1. Make sure the correct patient’s blood is being sampled. Often, anesthesia technicians in a busy service area must multitask and perform multiple blood gas samples at one time. Reporting the results for the wrong patient could have serious consequences.
2. Excess anticoagulant. The heparin used to prevent the blood from clotting can cause erroneous low CO2, low bicarbonate levels, and low base excess. Excess heparin can also bind to cations, yielding a lower value.
3. Inadequate removal of flush solution during the blood draw can cause dilution of the sample, resulting in erroneously low values.
4. Air bubbles in the sample syringe normally cause an erroneous increase in PaO2 levels.
5. A delay of more than 10 minutes, with the sample sitting in a plastic syringe, can yield a PaO2 level difference of more than 10 mm Hg to the actual PaO2.
Malfunctions such as calibration errors, failed quality control, and bad sensors are usually identified during machine-initiated calibrations or quality controls. These problems are corrected by most current blood gas machines with a “lockout” feature that will not allow further sampling. In some cases, the machine will allow a sample but without the faulty “locked-out” analyte. High and low settings are set internally during the machine setup prior to initial use. The high/low settings are agreed upon with the main laboratory, and in the case of hematocrit and glucose, a reading outside those settings will require a sample to be drawn and double checked with the main laboratory.
Note: High and low settings are set by the main laboratory and reflect the range of normal values. While the patient is in the operating room, it is not unusual for PCO2, PO2, hematocrit, and other values to be out of the “normal” range due to a variety of circumstances encountered during surgery.
Activated Clotting Time
The ACT detects clot formation. Patients who are having certain invasive procedures, such as cardiac bypass, require anticoagulation with heparin to prevent catastrophic thrombosis formation while on bypass. The heparin required to achieve a specific target level varies with individual patients and must be closely monitored.
As with many POCTs, there are some instances that can cause false values:
1. The ACT monitor is not warmed to 37°C. A monitor that is inadequately warmed will give an erroneously high ACT.
2. Inadequate removal of flush solution during the blood draw will give falsely elevated ACT.
It should also be noted that there are two major manufacturers of ACT monitors. The ACT is not a standardized measurement, so an ACT of 300 seconds from one manufacturer does not correlate with an ACT of 300 seconds from another manufacturer. An example of one manufacturer’s ACT machine can be seen in Figure 35.2.
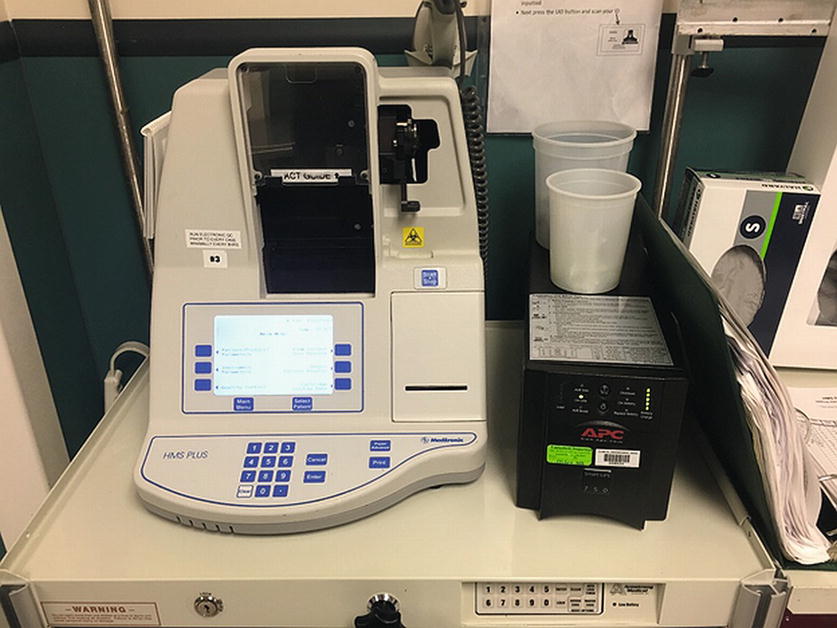
FIGURE 35.2. ACT machine connected to a UPS with a QC logbook and other supplies nearby.
Hepcon
The heparin concentration (Hepcon) monitor is a device that measures the actual concentration of heparin in the patient’s blood. Hepcon is another POCT equipment that is used to gauge the adequacy of anticoagulation for certain procedures such as cardiopulmonary bypass. Hepcon is an integrated system consisting of a component for tracking clot detection and computing results, a component for sample delivery, and the single-use test cartridges for actual performance of the tests.
The causes of faulty Hepcon readings are essentially the same as those that occur with the ACT machine.
Thromboelastography
Thromboelastography (TEG) is a device that allows the clinician to evaluate the patient’s ability to maintain hemostasis. In order for a patient to form a fibrin clot that is sufficient in strength to maintain hemostasis, the body depends on the interaction of enzymatic proteins (clotting factors) and platelets. Laboratory tests such as international normalized ratio (INR), partial thromboplastin time (PTT), ACT, and Hepcon measure the integrity of the clotting factors, whereas the TEG evaluates the entire coagulation process including platelet function. The TEG is generally used to monitor defects in the coagulation process and help guide the clinician to the appropriate treatment for those defects. Less commonly, the TEG can be used to monitor the adequacy of anticoagulation for patients undergoing procedures such as cardiac bypass.
The TEG evaluates the ability to form clots by measuring the tensile strength of the fibrin-platelet complex. A sample of blood is placed into a cuvette with a metal pin in the center. The cuvette is slowly rotated at approximately 6 cycles/min. An activator is added to the sample, and clot begins to adhere to the side of the cuvette and the metal pin. This creates resistance to rotation, which is then measured and plotted on a graph. The shape of the graph and time to when clot is formed give the clinician information on the integrity of hemostasis and the presence of specific deficiencies.
There are several preanalytical errors that can cause erroneous values for the TEG:
1. Patient identification. As with all lab tests, care should be taken to make sure the sample and results are performed on the correct patient.
2. Inadequate removal of flush solution during the blood draw can cause dilution of the sample, which will inhibit the sample from forming clots.
3. Agitation, such as pneumatic tube transport of the sample, can cause the blood to prematurely start forming clots.
Appropriate blood samples for the TEG include whole blood, citrated blood, or heparinized blood. Each sample type is used in different clinical situations. Care should be taken to ensure the proper anticoagulant is used in the sample.
International Normalized Ratio
The INR is a test that measures the adequacy of anticoagulation for patients taking warfarin. Many patients presenting for surgery are taking warfarin for the treatment or prevention of thrombosis. Patients having invasive procedures or surgery normally stop taking warfarin 5-7 days prior to surgery. These patients need to have their INR checked the day of surgery as the effect of warfarin is highly variable from patient to patient. The INR is often sent to a central lab that may take hours to run the sample; POCT can give an accurate measurement of INR within minutes. This can decrease the time and complexity for patients who need to coordinate the timing of lab draws and the time of surgery. The handheld INR machine, CoaguChek XS Pro, can be seen in Figure 35.3.
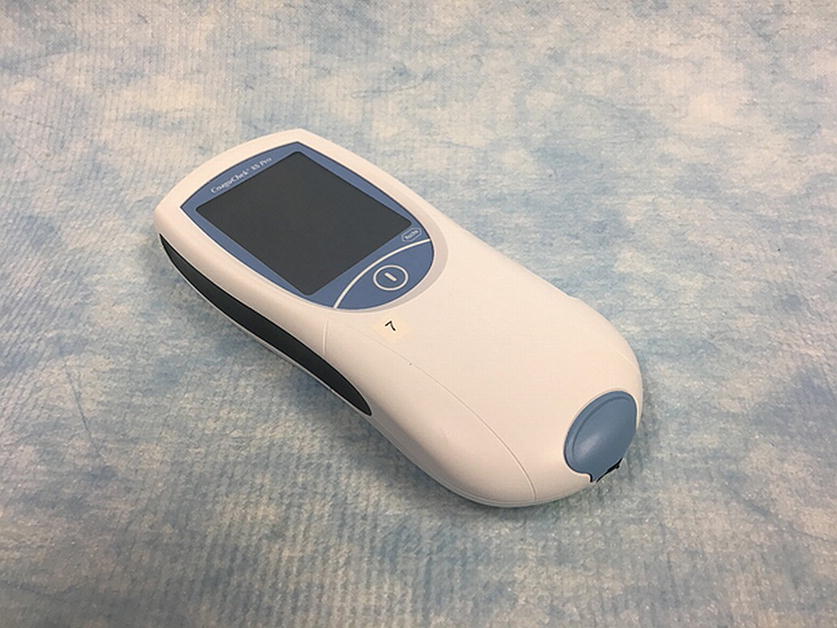
FIGURE 35.3. Handheld INR machines like this one allow for bedside checks greatly reducing the wait for lab tests often needed before surgery.
The INR is analyzed on a portable coagulometer much the same way that a patient’s circulating blood glucose is analyzed. A sample of blood is placed on a test strip after a finger stick is obtained. The test strip is then placed in the coagulometer at which time the sample is mixed with a thromboplastin reagent, causing a clot to form. There are several coagulometers available, and each has its own operating principles. However, all devices are accurate and can give results in under 3 minutes.
Blood Glucose Machine (Glucometer)
A handheld glucometer is a medical device for determining the approximate concentration of glucose in the blood. It is a key element of hospital and home blood glucose monitoring by people with diabetes mellitus or hypoglycemia. Glucometers are very accurate; however, a glucose reading from the main laboratory is always considered the gold standard. Figures 35.4 and 35.5 show a hospital grade handheld glucometer. Diabetic patients may bring their own glucometers to the hospital: once the patient has arrived in the hospital, these cannot be used by hospital personnel for decision-making, as POC devices and testing procedures undergo strict regulatory requirements (see below) before use. The accuracy of a glucose value from a home device is unknown.

FIGURE 35.4. A glucometer like this allows providers to monitor trending changes in glucose levels without having to draw repeated labs.
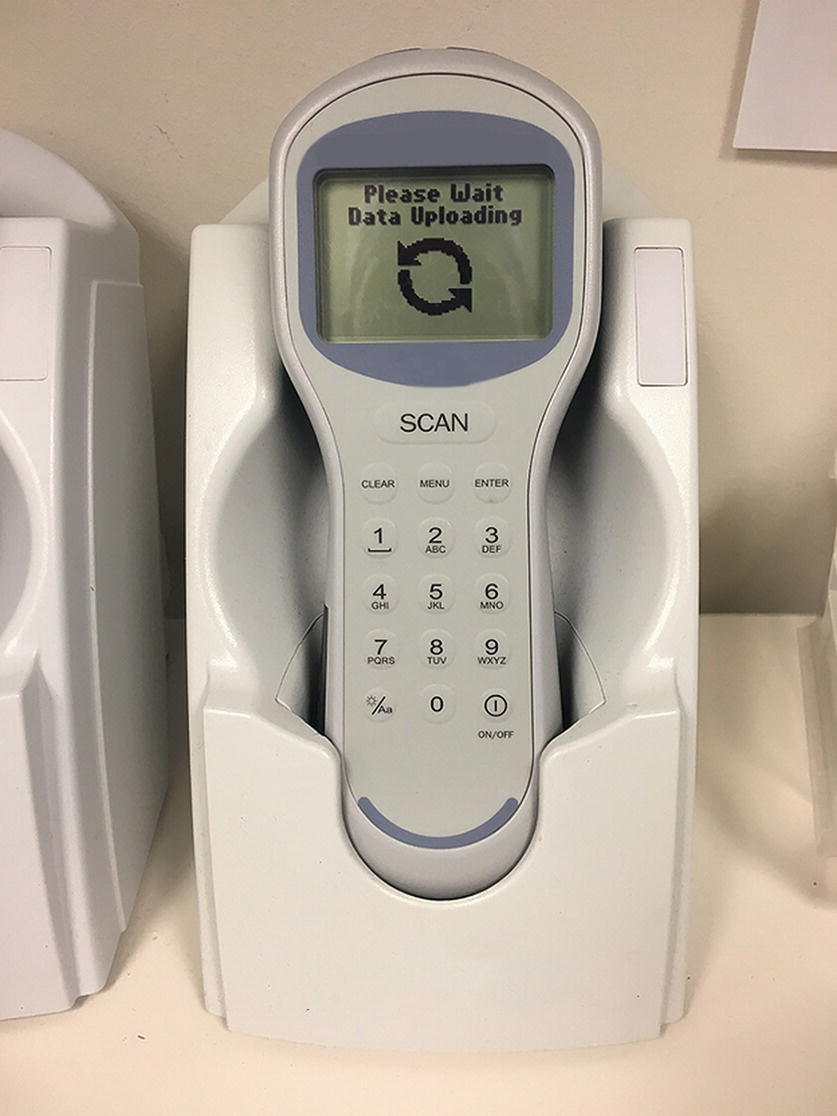
FIGURE 35.5. Data docks allow the upload of test results directly to a patient’s medical record, preventing problems from potentially erroneous hand transcription.
With a hospital glucometer, daily quality controls are required prior to use, and most meters have a lockout system until the quality controls are complete. Quality control fluids are generally good for 90 days after opening or the expiration date, whichever comes first.
Future POCT
POCT is evolving with new tests being developed such as DNA testing, immunoassay, microbiology, and endocrine tests. Although most of these new technologies will be used outside of the operating room, some of them may find use in the OR. Future technologies that may be beneficial in the operating room are coagulation analyzers that guide transfusion therapy and platelet function analyzers that will help guide platelet transfusion. When these technologies become available, the same principles for setup, maintenance, and quality control should be followed.
New Equipment
Device Selection
The key element to a successful program is a liaison between the main laboratory director, the POCT coordinator, and the anesthesia providers. POCT is a partnership between the main laboratory and anesthesia providers; however, inspectors hold the site performing the test and CLIA director responsible for noncompliance. This marriage of need is compelled from the moment the desire for a POCT site is recognized until the POCT site is decommissioned. Initial meetings between the main laboratory director, his or her POCT coordinator, and the anesthesia providers will establish a listing of acceptable analytic equipment. This analytic equipment must meet the standards of the laboratory and the needs of the anesthesia providers. Equipment standardization between the laboratory and POCT will minimize the number of different devices and be helpful when acceptance correlation verifications are required. With standardization, one policy can be shared among sites as well as a central data management system, operating procedures, clinical limitations, and reference intervals (normal values). Standardization will simplify training and competency for staff.
When deciding on analytic devices, pay close attention to what extent they require operator interactions for calibration, quality control, temperature monitoring of the machine, quality controls that require monitoring of the expiration dates and materials that have opened dating, and special refrigeration or storage needs.
Questions to ask when selecting a device are as follows:
1. Can the product be trialed?
2. What disposables are needed and their cost?
3. What is the projected cost per test?
4. Does the device self-prompt the operator and does the machine have automatic lockouts? These lockouts should include a lockout of anyone not qualified to operate the device and lockout of a specific analytic if it fails quality control.
5. Does the device perform automatic quality control or do personnel have to run daily shift quality controls? The automatic quality control mode with lockout would be preferred since it eliminates human error and releases the staff to other works.
6. What are the manufacturer’s requirements for calibration, quality control, and preventive maintenance?
7. Will special power and/or computer hookup be required? An uninterrupted power supply system is highly recommended.
8. Is there a secure data management system to capture quality controls and test results? Is there special software and licensing required?
9. How much training will be provided to the operators? Who will perform this training? Will the manufacturer provide startup assistance for the initial days?
10. Contact the Clinical Technology Services (CTS) department and ask CTS personnel to check medical device alerts for any product selected and establish any required training needed to maintain the device. Typically, CTS personnel check the device against the Emergency Care Research Institute (ECRI) database, which includes product repair information nationwide.
11. Where will the quality control material be stored and what special handling will be required?
Once the device is selected, you should begin to write clear procedures and competencies and verify the procedure with the main laboratory POCT coordinator prior to going active, thereby reducing any problems that may arise. Define the quality control requirements and schedule, calibration cycle, and preventive maintenance schedule. The main laboratory may have a policy/procedure that can be tailored to the POCT area. At the very least, it will have a template for new lab policies and procedures that can be used as a starting point. The time spent in this initial phase will save the POCT director or his or her designee hours of time in the future. Once a good foundation is set, the program will run smoothly if you stay current with practices and perform internal audits. It may be helpful to establish a centralized POCT repository with all of the tools necessary to manage POCT.
Arrival of New Equipment
Once newly purchased devices arrive, acceptance testing between the POCT device and the main laboratory device must be performed. Acceptance testing requires correlation verification between the POCT device and a main laboratory device. A minimum amount of acceptance testing is required and is set by the main laboratory or the manufacturer’s recommendations. Results are documented between the POCT device(s) and the main laboratory device. Results must be within a set parameter established by the main laboratory or the manufacturer’s recommendations. These documented results are retained for the life of the device.
Review the operating manuals to validate manufacturer’s requirements for calibration, quality control, and preventive maintenance. CTS repair personnel should be consulted for preventive maintenance. Identify the equipment using hospital-accepted identifying numbers for future preventive maintenance.
Training for the operator prior to use must be accomplished and documented. A competency form for initial and ongoing training must be completed and retained for 3 years. The main laboratory POCT coordinator will initiate external proficiency testing. Review your policies/procedures prior to the activation date of the device.
Personnel
Operators need initial and ongoing training and certification. Identify only those operators who are required to perform the test to be authorized users. Large numbers of operators increase the amount of work to manage documentation and associated regulatory requirements.
The job of training and proficiency testing will fall on the POCT director who is a physician or a doctoral scientist. The director or his or her designee will be responsible for developing initial training requirements, initial and ongoing competency, and the related documentation for both. This training must be accomplished prior to the initial use of any POCT device. Operators must document that they have read the policies and procedures for the facility, the main laboratory, and the new POCT. Each individual’s performance must be evaluated by an authorized user. This includes, but is not limited to, patient identification and preparation and specimen collection, handling, processing, and testing. Each individual must be monitored recording and reporting test results. The POCT director ensures each operator conducts external proficiency testing and conducts ongoing monitoring of each operator performing tests, reporting results, and documenting results. This proficiency monitoring must be documented. A current list of POCT personnel that delineates the specific tests, levels, and methods that each individual is authorized to perform must be documented (authorized user list) and a copy sent to the main laboratory director.
The competency of each person to perform the duties assigned must be assessed following training before the person performs patient testing. Semiannual competency during the first year of an individual’s duties is required. After an individual has performed duties for 1 year, competency must be assessed at least annually.
Ongoing supervisory review is an acceptable method of assessing competency for certain elements. Competency assessment may be documented in a variety of ways, including a checklist completed by a supervisor.
Quality Management
The quality management (QM) program for POCT must be clearly defined and documented. The program ensures quality throughout all phases of testing and should cover patient identification, specimen collection, identification, and processing, as well as how to report results. The QM program must be capable of detecting problems and opportunities for system improvement. The POCT program must be able to develop plans of corrective/preventive action based on data from its QM system. Documentation should be maintained for all identified problems, corrective actions taken, and the outcome of those corrective actions.
There must be a system in place that detects and corrects clerical errors and analytical errors in a timely manner. The usually accepted manner is to employ automatic quality controls with a lockout feature that will not allow a specific analyte to be tested if an error is detected. Each device will also have internal high and low limits set for each analyte. The quality assurance test will indicate if an analyte is higher or lower than acceptable limits.
Manufacturer’s Procedure Manual (User Manual)
A copy of the user manual should be located at the laboratory workbench for quick reference when there are questions or problems. A copy of the policies/procedures should be located with the user manual and reviewed annually by all authorized users. A copy of the annual review signature sheet should be retained with the user manual. When changes are made to the base policies/procedures, a review by the main laboratory director and the POCT director should document that the changes are acceptable.
Specimen Handling
A step-by-step procedure for specimen collections should be documented within the procedure and reference needle safety, how to identify the patient, how the test is requested, how the specimens are handled and identified, and how the results are reported.
Results Reporting
Reference ranges specific for age, sex-specific normal values, and interpretive ranges (normal ranges) must be reported with patient test results; however, it is not necessary to include reference ranges when test results are reported as part of a treatment protocol that includes clinical actions (such as a surgical procedure), which are based on the test result. The test results must be recorded.
After careful evaluation, the POCT site should set formal reference ranges and retain documentation of this evaluation. These reference ranges are set with the cooperation of the main laboratory. Critical limits must be established for appropriate tests, so that immediate notification of a physician or other clinical personnel responsible for patient care occurs. These must be documented in the policies/procedures and within the procedures, a clear indication of how notification of a critical element is done and documented. The users must be familiar with critical limits for procedures that they perform. Personnel performing the test must be identified. This is usually accomplished with the assignment of a unique user code to access the test device.
Quality Control
Daily staff performing external controls must be run as follows:
1. For quantitative tests, two controls at two different concentrations must be run daily, except for coagulation tests (two controls required every 8 hours).
2. For qualitative tests, a positive and negative control must be run daily.
Daily controls may be limited to electronic/procedural/built-in (e.g., internal, including built-in liquid) controls for tests meeting the following criteria:
1. For quantitative tests, the test system includes two levels of electronic/procedural/built-in internal controls that are run daily.
2. For qualitative tests, the test system includes an electronic built-in internal control run daily.
3. The system is Food and Drug Administration (FDA) cleared or approved and not modified by the laboratory.
4. The system is not classified as highly complex under CLIA.
5. The laboratory has performed and documented studies to validate the adequacy of limiting daily QC to the electronic built-in controls. Initial validation studies must include comparison of external and built-in controls. The laboratory director is responsible for determining the sample size for the other devices. The laboratory director is responsible for determining criteria for acceptability and other details of the validation.
6. External controls are run for each new lot number or shipment of test materials and after major system maintenance and after software upgrades. Regarding the positive external control for qualitative tests, best practice is to run a weak positive control, to maximize detection of problems with the test system.
7. External controls are run at a frequency recommended by the test manufacturer or every 30 days, whichever is more frequent.
The laboratory director or his or her designee must review QC data at least monthly.
If the laboratory/POCT program uses more than one instrument to test for a given analyte, the instruments are checked against each other at least twice a year for correlation of results. This requirement applies to tests performed on the same or different instrument makes/models. This comparison must include all nonwaived instruments. The laboratory director must establish a protocol for this check.
Calibration
A written procedure defining the use of appropriate calibration and calibration verification materials is needed. Criteria for calibration typically include the following:
1. Changing of reagent lots, unless the user can demonstrate that the use of different lots does not affect the accuracy of patient test results and the range used to report patient test data or the control value.
2. When indicated by quality control data.
3. After major maintenance or service.
4. At least every 6 months.
5. As recommended by the manufacturer.
Summary
POCT provides faster test results with the potential for improved patient outcome, but the quality of results is a concern. An organized POCT program is required to manage the quality of results supervised by laboratory staff (not dictated by the laboratory). This program should manage the validation of devices, training of operators, and day-to-day activities required for POCT to meet medical needs. POCT errors can occur in similar ways to laboratory errors. Training and QI programs should monitor the frequency of errors and act to improve detection and prevention of errors. Strategies to make POCT a part of routine patient activities have greater success at regulatory compliance and improved quality outcomes.
Review Questions
1. All of the following can cause an erroneous value on a blood gas analyzer except
A) Excess anticoagulant in the sample tube
B) Inadequate removal of flush solution during blood draw
C) Excessive blood drawn into the sample tube
D) Delay of more than 10 minutes before running blood gas sample
E) None of the above
Answer: C
Excess blood in the sample tube will not cause any problems. Flush solution can dilute the actual sample. A delay of more than 10 minutes can allow continued metabolism in the red blood cells and alter values.
2. Which of the following statements is true regarding the ACT analyzer?
A) The ACT measures the time to clot formation in seconds.
B) The ACT analyzer should be cooled to 32°C prior to running the sample.
C) Dilution of the blood sample has minimal effect on the results of the ACT.
D) All ACT analyzers are standardized, so values from one manufacturer can be compared to values from another manufacturer.
E) None of the above.
Answer: A
The ACT is measured in seconds. The ACT analyzer should be warmed up prior to use. Failure to do so can produce faulty values. Similar to blood gas analysis, dilution of the sample can cause erroneous values. Two different ACT manufacturers have different methodologies to measure the ACT and the values cannot be compared.
3. Which of the following statements are true in regard to the TEG?
A) The TEG measures time to clot formation in seconds.
B) The main advantage of the TEG compared to ACT is that heparin or citrated blood does not affect the results.
C) The TEG does not evaluate the integrity of platelets on the clotting process.
D) Excessive agitation of the blood sample can cause premature clot formation.
E) All of the above.
Answer: D
Agitation of the sample can cause premature clot formation and is a common source of errors with TEG measurements. The TEG results are plotted on a graph and not reported as a time. One of the advantages of the TEG is that it measures platelet function.
4. When there is a question about the validity of a test result, the best rule of thumb is
A) Assume the values are true because today’s POCT machines are highly accurate.
B) Recalibrate the POCT machine in question.
C) Draw two samples, reanalyze one on the POCT, and send one to the central lab for comparison.
D) Check to make sure the calibration reagents are not out of date.
E) None of the above.
Answer: C
If there is any doubt about the accuracy of a POCT device result, the best course of action is to perform another sample and to compare the result to a result obtained from the central lab.
5. Which statement is true regarding the INR?
A) It is measured by a TEG.
B) It evaluates the body’s ability to form clot as a whole dynamic process.
C) It measures the adequacy of anticoagulation for patients taking warfarin.
D) The blood sample must be drawn from an artery.
E) None of the above.
Answer: C
The INR is a measurement of a portion of the clotting cascade that is affected by warfarin. Thus, the INR is a common test for evaluating warfarin anticoagulation. The INR does not test the entire clotting process (e.g., another limb of the clotting cascade or platelet function). Blood samples for INR testing can be drawn from an artery or a vein.
6. A blood gas machine would most likely analyze which of the following parameters?
A) HCT, NA+, PO2, lactate
B) HCT, NA+, PO2, INR
C) HCT, NA+, PO2, ACT
D) HCT, NA+, PO2, platelets
Answer: A
Blood gas machines regularly test for hemoglobin/hematocrit, electrolytes, and gas values. Different specialized machines would be required to test INR, ACT, and other blood components or coagulation parameters.
7. Which of the following tests are not available on POC machines in the OR?
A) Blood glucose
B) INR
C) ACT
D) Type and screen
E) Thrombelastography (TEG)
Answer: D
A type and screen is a specialized lab test to determine the ABO type and Rh factor of the blood. It is performed in the main laboratory and can take as long as 45 minutes to perform.
8. When performing POC testing, you do not have to follow universal precautions and perform two patient identifiers because the test is not being performed in the lab.
A) True
B) False
Answer: B
When drawing blood or working with patient fluids, you should always following universal precautions. Checking two patient identifiers ensures that you are performing the correct test on the correct patient.
SUGGESTED READINGS
College of American Pathologist. Point-of-Care-Testing Checklist. Northfield, IL: College of American Pathologist; 2015.
Hutchson AS, Ralston SH, DryBurgh FJ, et al. Too much heparin: possible source of error in blood gas analysis. Br Med J. 1983;287:1131-1132.
Mueller RG, Lang GE, Beam JM. Bubbles in samples for blood gas determinations—a potential source of error. Am J Clin Pathol. 1976;65(2):242-249.
Picandet V, Jeanneret S, Lavoie JP. Effects of syringe type and storage temperature on results of blood gas analysis in arterial blood of horses. J Vet Intern Med. 2007;21(3):476-481.
Wallin O, Soderberg J, Grankvist K, et al. Preanalytical effects of pneumatic tube transport on routine haematology, coagulation parameters, platelet function and global coagulation. Clin Chem Lab Med. 2008;46(10): 1443-1449.