CHAPTER 45
Defibrillators
Introduction
A defibrillator is a medical device used to treat a variety of cardiac arrhythmias (abnormal heart rhythms) with an electrical shock. Defibrillators have a central role in ACLS (advanced cardiac life support) algorithms for the treatment of acute cardiac arrest and unstable heart rhythms.
The importance of early defibrillation for patients suffering from sudden cardiac arrest is emphasized in the guidelines for cardiopulmonary resuscitation (CPR) from the American Heart Association (AHA). Research has shown that survival decreases 7%-10% per minute prior to defibrillation. Because the standard of care for defibrillation is less than 3 minutes, it is important that all anesthesia technicians are familiar with the setup and operation of defibrillators.
Defibrillators send a current through the heart with the goal of simultaneously depolarizing all of the myocardial cells and resetting the cardiac conduction system. If defibrillation is successful, when cardiac electrical activity resumes, conduction can begin with the sinoatrial (SA) node (see Chapter 4, Cardiovascular Anatomy and Physiology) and travel through the cardiac conduction system to coordinate the subsequent depolarization and contraction of the remaining myocardial cells to restore blood flow. This does not always happen, particularly in the setting of injured myocardial cells. After massive depolarization by a defibrillator, electrical activity of the heart may not reset to a normal rhythm, but rather return to an abnormal rhythm. Two such abnormal rhythms include ventricular fibrillation (commonly referred to by medical personnel as “VF” or “v fib”) and ventricular tachycardia (commonly referred to as “VT” or “V tach”). VF is a life-threatening heart rhythm with disorganized cardiac electrical activity producing a quivering movement of the heart leading to loss of blood flow and pulse. VT is a rapid contraction of the ventricle independent from the normal electrical control system. VT occasionally produces a minimal amount of circulation; it commonly produces no circulation; it can at any time rapidly deteriorate into VF. Defibrillation of these particular arrhythmias can be lifesaving, and every second counts.
This chapter focuses on the setup, operation, and maintenance of defibrillators. More information about the overall management of cardiac arrest is found in Chapter 58, Cardiac Arrest. Although these devices are called defibrillators, they are also used in cardioversion. Defibrillation is emergency conversion of unstable rhythms. Cardioversion is an elective or semielective procedure to send electrical currents through the heart to convert abnormal rhythms other than VF into sinus rhythm. Defibrillators are also used for pacing abnormally slow and symptomatic heart rhythms.
Types of Defibrillators: Internal Defibrillators, External Defibrillators, and Automatic External Defibrillators
Defibrillators can be external, which pass energy through the patient’s chest to reach the heart through wires attached to pads or paddles, or internal devices, which are surgically implanted devices that pass energy directly to the heart. Some internal devices can be used during surgery when the heart is exposed (i.e., open heart surgery or thoracotomy), while other internal defibrillators are attached with electrodes that travel through the venous system to the heart. A generator is then attached to the electrodes and secured beneath the skin of the patient. Internal implantable cardioverter-defibrillators (ICDs) that are placed in patients who are at high risk of VF/VT are discussed in Chapter 46, Pacemakers and Implantable Defibrillators. External defibrillation may still be necessary for patients with ICDs if the device has been disabled, is malfunctioning, or is ineffective.
Another category of external defibrillators is automated external defibrillators (AEDs). These are designed for use by individuals with minimal training, allowing for use by the general public. By contrast, defibrillators used in the hospital and the operating room (OR) are more complex and are intended to be used by people trained in ACLS. Awareness of the lifesaving potential of rapid defibrillation in sudden cardiac arrest has led to campaigns to deploy AEDs in public settings and to train the lay public in recognizing cardiac arrest and using AEDs.
The majority of this chapter will be devoted to external defibrillators and AEDs, since these are the devices that every anesthesia technician should be comfortable with.
Electrical Energy
Older defibrillators are called “monophasic,” and newer defibrillators are called “biphasic” based on the waveform of the electrical shock they deliver. Monophasic machines have an optimal defibrillation success with an energy output of 360 J (2-4 J/kg for pediatric patients). The newer biphasic defibrillators are more effective in successful termination of VF at lower energy levels. These devices are usually operated with an output energy of 120-200 J. The manufacturer specifies the exact recommended setting for defibrillation. While new external defibrillator units are likely to be biphasic, a significant number of older units remain in use. Anesthesia technicians should be familiar with the type of defibrillators that are in use at their facility as well as the manufacturer’s recommended energy setting.
Basic Features
Features commonly available on defibrillators (in addition to defibrillation capability) include electrocardiogram (ECG) and heart rate monitoring, the ability to switch between AED and manual modes, cardioversion, transcutaneous pacing of slow heart rhythms, and pulse oximetry. In the near future, many defibrillators may come equipped with continuous capnography. Another common feature of most devices is the ability to provide data collection during use, with the option of printing both the vital signs and/or ECG rhythm strips both during and after use. Analysis of cardiac rhythm may be more accurate from printed strips during events. Newer devices also allow for storage of this data on memory cards and, in some instances, transfer of the data via wireless networks to a central server or the electronic medical record. This may be very useful for record keeping after cardiac arrest situations.
Use of the Defibrillator
Attaching the Pads or Paddles
Defibrillators display the heart rhythm when defibrillator paddles, hands-free pads, or the ECG leads of the defibrillator are properly placed on the patient’s chest (Fig. 45.1). The standard lead displayed on the monitor is often lead II, although this can be changed on some devices. It is critical to know the source of the defibrillator ECG signal. The defibrillator may be reading the ECG signal from pads, paddles, or ECG leads that are not attached. The displayed waveform from unattached leads could look like VF or asystole. Most defibrillators are only able to sense a rhythm or deliver energy, but cannot do both actions simultaneously through the pads or paddles by themselves. Accessory ECG leads are therefore necessary to sense native rhythms and deliver shocks for external pacing or cardioversion. As with standard monitors, the size of the ECG waveform or the lead from which the unit is obtaining the ECG signal may be adjusted to improve the identification of the cardiac rhythm.
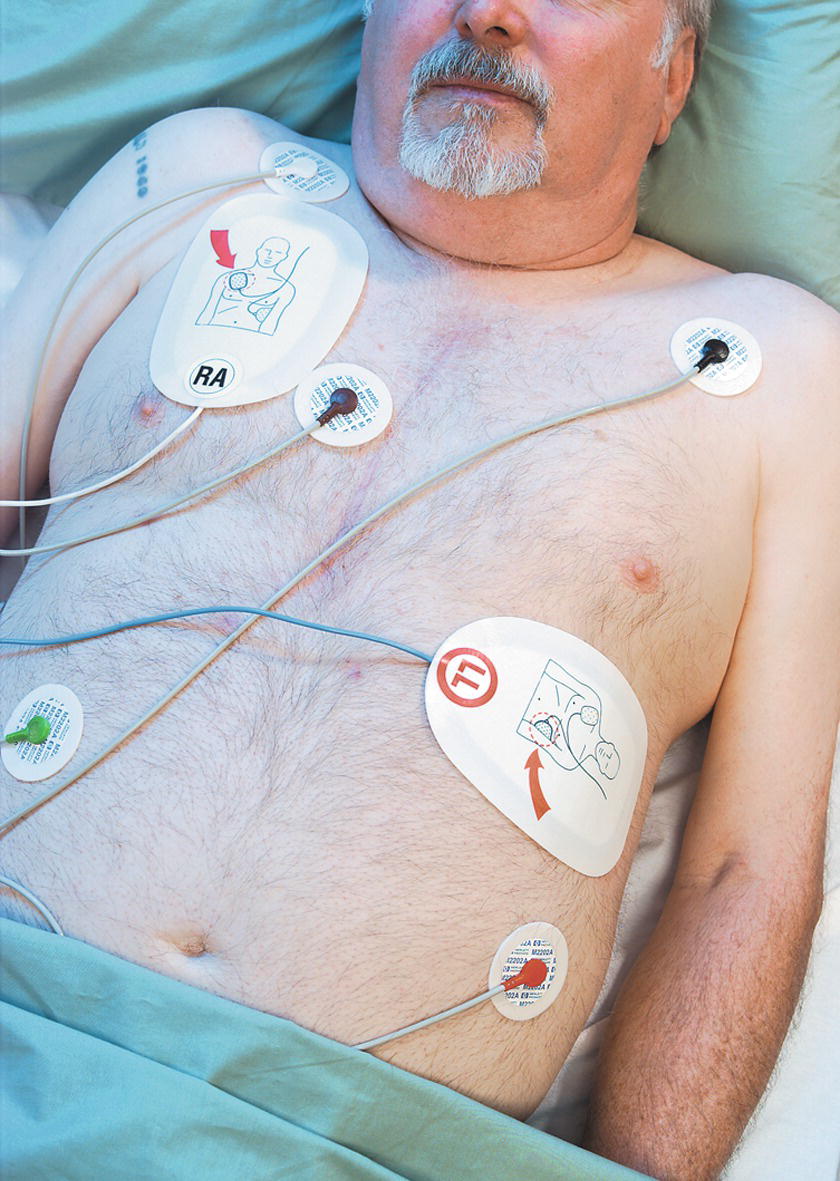
FIGURE 45.1. Anterolateral pad placement. (Courtesy of Philips Healthcare.)
Energy from external defibrillators can be delivered via disposable pads or reusable paddles. Adhesive gel pads can be attached to the chest and allow for both observation of ECG rhythm and delivery of electricity. Alternatively, external paddles may be applied to the chest wall, or in cases where the chest has been opened surgically, smaller internal paddles can be applied directly to the heart. Internal paddles require a significantly lower-energy setting because the current is delivered directly to the cardiac muscle. If the higher 200-J currents used for external defibrillation are applied directly to the heart, this can cause direct electrical injury to the myocardial cells and cause patient harm.
If adhesive gel pads are being used, there are four AHA-approved pad placement locations on the thorax. For anterolateral placement, one pad is placed over the right anterior chest, to the right of the sternum and below the clavicle, and the second adhesive pad is placed on the left side of the chest, lateral to and below the nipple (and under the breast), as shown in Figure 45.1. Both are applied to the patient’s bare skin. The three other AHA-approved pad placement locations are anteroposterior, anterior-left intrascapular, and anterior-right intrascapular. None of these pad positions have been proven to be more effective at defibrillation or cardioversion than the anterolateral position. Note that in all of the positions, the heart lies between the pads. This optimizes the amount of energy that passes through the heart. Occasionally, the sterile draping for a surgical or electrophysiology procedure (e.g., in shoulder surgery or kidney surgery) will mean that the surgeon, cardiologist, or anesthesiologist will look for locations for the pads that do not interfere with draping. The goal of pad or paddle placement is always to pass current directly through the heart.
When attaching the pads, remove them from their packaging, place them on the patient’s bare skin, and make sure that they are in good contact with the patient’s skin (press them down firmly to attach them). The adhesive on the rim of the pads will hold them in place. Hands-free pads must be kept in special packaging. If the packaging has been opened, the conductive gel layer on the pads may dry out, and the adhesive may no longer work. For patients with significant body hair, it is recommended to use hair clippers on pad sites to allow for the most optimal contact. Avoid placing pads/electrodes on top of implanted devices such as pacemakers, ICDs, implanted pain pumps, or venous access ports. There are specially sized pads for pediatric and adult patients.
If hands-free pads are not available and the device has paddles, the paddles can be manually held in place to perform ECG monitoring and defibrillation. Apply electroconductive gel to the paddles before they are applied to the bare chest, or apply an electroconductive gel pad on the patient’s chest where the pads will be placed. The gel lowers the resistance and allows the energy to pass from the paddles through the skin. Improperly applied paddles or paddles used without gel can prevent sufficient energy transfer through the skin to reach the heart. This can not only lead to ineffective defibrillation but can cause burns to the patient’s chest where the paddles contact the skin. When placing the paddles, apply about 25 pounds of pressure to hold them firmly against the chest. The most common position for external paddle placement is the anterolateral position (Fig. 45.2). If standard or internal paddles are to be used, additional ECG leads are needed to allow for rhythm analysis when the paddles are not touching the chest or heart. Standard lead placement as discussed in Chapter 31, ASA Standard Monitors, can be followed.

FIGURE 45.2. Anterolateral paddle placement.
Troubleshooting pads and paddles: The most common problem with pads and paddles is improper connection to the defibrillator. Always check to make sure that the connection from the pads or paddles (whichever is being used) is connected to the defibrillator (Fig. 45.3). In many instances of equipment problems, the operators were attempting to defibrillate with the pads, but the paddles were the ones that were connected (or vice versa). Many defibrillator units are left with the pads unattached to the device, and when used in an emergency, personnel forget to attach the connector to the defibrillator. Also, at times the connection between the machine and cables is not fully engaged, despite appearances of them being connected. Modern defibrillators will display an error message if the pads are not attached and the operator attempts to defibrillate. Unfortunately, in the high-pressure situations when defibrillators are employed, many operators do not notice the warning displayed on the screen or the verbal prompt by the device. Other common problems include lack of conductive gel (surgical lubricants will not work) or dried-out pads. You should practice connecting and disconnecting both pads and paddles in a nonemergency situation: it is not easy to do it quickly and properly, and it will frequently be your role as the anesthesia technician to switch between the two.

FIGURE 45.3. Connection of defibrillator pads to the back of the machine.
Once the pads are in place, the ECG leads should be attached if time allows. Of note, many defibrillators will defibrillate without ECG leads but will require connected ECG leads to perform external pacing or cardioversion.
Turn the Power ON
If the unit is not already on, turn on the power switch. The vast majority of defibrillators will operate on battery power and have sufficient power to deliver multiple shocks. Most facilities leave manual defibrillators plugged into the wall power when not in use to keep the battery charged. If possible, plug in the defibrillator during a code situation so that battery drainage is not an issue; however, be sure the defibrillator remains in close proximity to the patient. AEDs usually have an indicator light to indicate battery status and do not have external cords that can be plugged in.
Rhythm Analysis
Once the unit has been turned on and an ECG signal can be read, the rhythm must be analyzed by the resuscitation team. If the defibrillator is an AED, it can use computer software to analyze the ECG signal. Most modern AEDs will automatically perform a rhythm analysis once an ECG signal has been detected through the pads. Older units may require the operator to press a button to cause the unit to begin its analysis. Modern manual defibrillators often come with an AED mode. The resuscitation team can analyze the rhythm visually or select a button to cause the defibrillator to go into the AED mode and perform the analysis by computer. In both manual and AED analysis of the heart rhythm, it is important to not move the patient during the analysis. Even minimal patient movement can introduce large artifact in the ECG signal confusing the computer or person attempting to analyze the ECG. This is one of the reasons for a break in CPR for rhythm checks in the ACLS algorithm. It is important to keep breaks extremely brief (10 seconds) as they interrupt oxygen delivery to the brain.
Energy Selection
Once the resuscitation team has determined that a shock is warranted, the operator must select the energy level. The team leader will determine the energy level to be used based on the type of rhythm, location of the paddles, and outcome of prior attempts at defibrillation. AEDs do not allow manual selection of the energy level. In order to deliver lower-energy shocks to children or infants, the operator must place child pads instead of adult pads. These child pads attenuate the amount of energy that is delivered to the patient. Manual defibrillators require selection of the desired energy (Fig. 45.4). Typically 200 J is the recommended selection for biphasic defibrillators and 360 J for monophasic defibrillators.

FIGURE 45.4. Use up or down arrows to select the energy level.
Charge the Defibrillator
Once the energy level is selected, the device must be charged prior to delivery of a shock. During charging, the device loads the energy from the power source and prepares to deliver a shock. The charge and shock delivery buttons can be found on the device, on the external paddles, or in some models in both places (Fig. 45.5). The charging process may take 3-5 seconds depending upon the unit. Modern units charge more quickly than older units. Chest compressions should be continued while the device is charging. Once charged, most defibrillators will sound an audible tone and “hold” the charge for up to 1 minute. If the shock is not delivered in that period, the device will sound a warning and then dispose of the charge internally without shocking the patient. If a shock is desired, the device will have to be recharged by pressing the charge button again. In some devices, changing the energy level once the unit is charged will cause the unit to dump the charge internally and require recharging. AEDs will automatically charge if a shockable rhythm is detected and give an auditory and visual readout of this process.
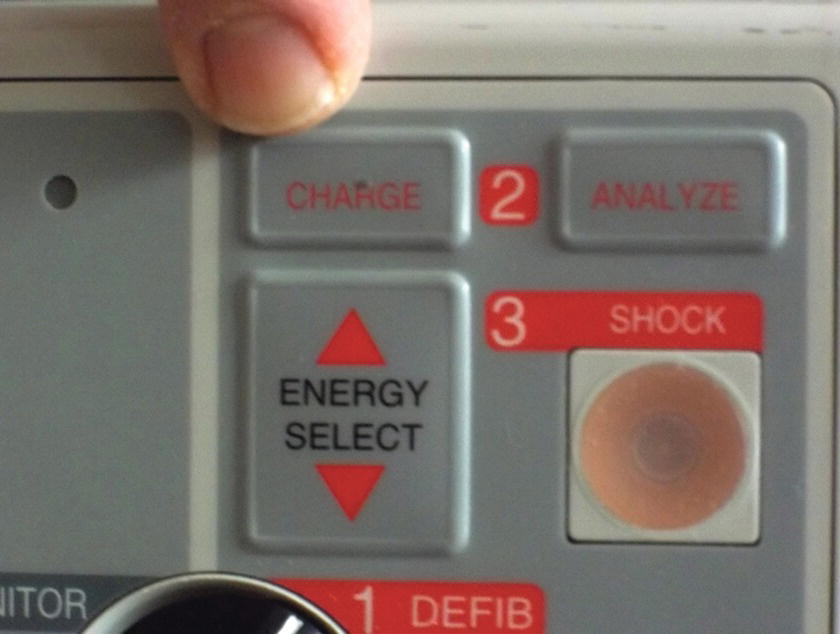
FIGURE 45.5. Press the charge button after setting the energy level.
Deliver the Shock
Once the device is charged, delivery of the shock is triggered by pressing the shock button on the defibrillator base if using pads and via trigger buttons on the paddles if they are being used. If cardioversion is desired instead of defibrillation, the device must be synchronized to the patient’s underlying cardiac rhythm prior to discharge of the shock. The devices have a button allowing synchronization, indicated by marks on the ECG monitor above or below each QRS complex (Fig. 45.6). It is extremely important that no one is touching the patient or any equipment connected to the patient when the device discharges the electrical current. The importance of this is discussed further under the section “Complications.”
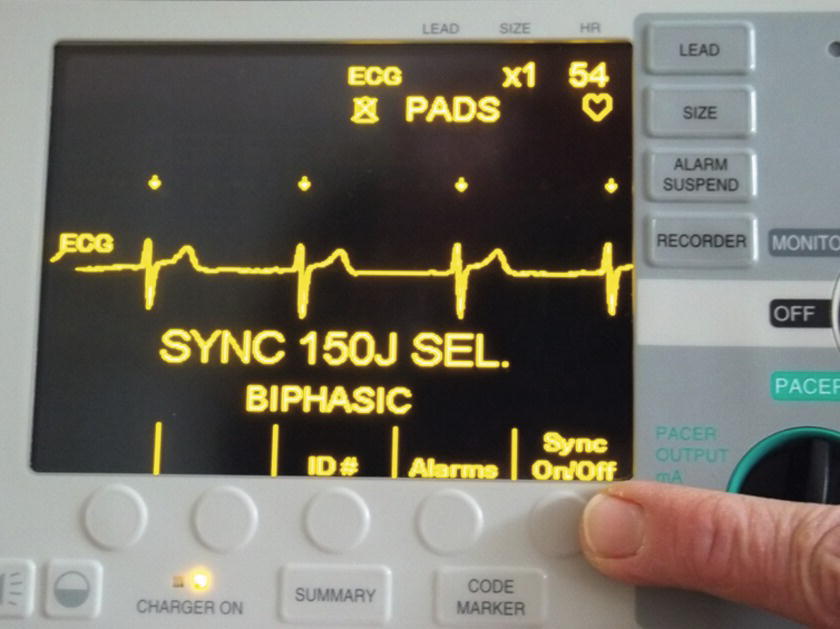
FIGURE 45.6. Synchronization button. Note arrows above each QRS complex.
If an AED is in use and a shockable rhythm has been detected, the unit will sound an audible notification that it is charging. Once the charge has been loaded, the AED will give audio instructions that rescuers should not touch the victim and for the operator to push the shock button on the AED. In many devices, the shock button will be flashing. Some AEDs are fully automatic and do not require the operator to push a shock button. The AED will deliver audible warnings to not touch the victim and state that it is going to deliver a shock. After a suitable warning period, a fully automatic AED will deliver the shock.
Complications
Inadvertent spread of electrical current to people other than the patient can pose a life-threatening risk to you or anyone involved in the resuscitation. More than 80% of the energy supplied to the patient is shunted to areas of the body other than the heart. Therefore, people in contact with the patient, stretcher, or monitors connected to the patient are all possible sites of electrical current spread. Additionally, special care must be taken in the OR environment where there might be water, fluids, or blood that can lead to easy propagation of electrical energy away from the patient. The risk of injury should not be underestimated, and it is the responsibility of all people involved in the resuscitation and, most importantly, the operator of the device to ensure that there is no inadvertent contact with the patient, support equipment, or water during the delivery of the shock.
Multiple case reports of fires caused by defibrillators have been reported, and the likely cause was avoidable. In these cases, it appeared that the paddles were incorrectly applied or applied without conducting gel, resulting in the formation of sparks in an oxygen-rich environment. Use of adhesive gel pads can help minimize the risk of spark formation, and if possible, a closed oxygen delivery device should be used.
Another important complication is the inappropriate delivery of a shock. An electrical shock to a normally functioning heart can cause the heart to fibrillate. In addition, all rhythms except VF and pulseless VT require delivery of the shock with precise timing during the cardiac cycle. The defibrillator “synchronizes” the shock with patient’s ECG rhythm to deliver the shock at the appropriate time. This is accomplished differently in varying models but most commonly by pressing a “sync” button on the defibrillator as discussed above. This is another reason it is important to be familiar with your particular model ahead of time and know how this is done. Figuring this out for the first time during a crucial, often high-stress moment can lead to the delay of a lifesaving intervention. The defibrillator will indicate that it is synched with an indicator on the screen and a mark on each QRS signal on the ECG indicating the device has detected the QRS complex. If the patient is not in VF or pulseless VT, and an asynchronized shock is delivered, the patient can be converted from a rhythm that is perfusing (i.e., helping to circulate blood) to nonperfusing (not circulating any blood) like VF.
Troubleshooting
Troubleshooting of a defibrillator should focus on obvious sources of error such as inadequate power supply and improper connection of cables both to the machine and to the patient. Good maintenance and checkout procedures will often eliminate the common sources of trouble with the defibrillator. Additionally, knowing the location of multiple devices in the area will ensure that a working defibrillator is always readily available in the case of malfunction of one machine. When basic troubleshooting does not identify the problem, the individual device manuals provide a detailed troubleshooting guide for assistance. One common error when attempting to defibrillate a patient in VF is when the defibrillator is in the sync mode. In the sync mode, the defibrillator will attempt to identify a QRS complex. If it cannot do so, it will not allow delivery of a shock. Turn the sync mode off to deliver an unsynchronized shock to a patient with VF or pulseless VT. Another common error when attempting to cardiovert a patient is when the additional “sensing” ECG leads are forgotten. Without additional ECG leads, the defibrillator cannot sense the native heart rhythm and deliver electrical energy at the same time.
External or Transcutaneous Pacing
Many modern defibrillators also have the ability to pace the heart through the same hands-free pads that can be used for defibrillation or cardioversion. Pacing mode must be selected on the device (Fig. 45.7). Many units require selection of the pacing energy to be delivered (often in milliamperes or mA) and the pacing rate. These are usually two separate dials or buttons. Other units also require the “pacing mode” to be selected. Demand mode will only deliver the pacing if the patient’s detectable QRS rate is lower than the pacing rate. Asynchronous pacing mode will deliver the pacing shock regardless of the patient’s native ECG. Lastly, many devices require that the operator depresses a “start pacing” button once the mode, energy, and rate selections have been made before the unit will begin delivering pacing energy.

FIGURE 45.7. Selection of the pacing mode.
Maintenance
Each manufacturer has specific recommendations for maintenance of a defibrillator, and the anesthesia technician should be familiar with the specific protocol for the devices used in his or her facility. Additionally, the anesthesia technician should be familiar with the hospital’s policy on device maintenance, and periodic testing should be followed. At the start of each shift, the availability and working status of the defibrillators must be confirmed to ensure that the device is connected, the battery is fully charged, the device is operating correctly, and all needed accessories are present. The checkout process for each device is specific, and reference to the individual device manual is recommended. It is necessary to confirm the presence of all components of the defibrillator:
1. Multiple sets/sizes of unexpired adhesive gel pads with connecting cables
2. Paddles and electrode gel
3. ECG cables with electrode pads
4. Fully charged battery installed in the device as well as a charged backup battery
5. Integrity of all wires including AC power cord
6. Recorder paper
7. Alcohol wipes
8. Hair clippers
Defibrillator Summaries by Manufacturer
Philips Healthcare Defibrillators
Philips Healthcare manufactures a line of both automatic and manual external defibrillators under the trade name “HeartStart.” The manual external defibrillator models include the HeartStart XL defibrillator as well as the HeartStart MRx monitor/defibrillator (Fig. 45.8), which includes defibrillator functions along with more advanced monitoring capabilities. Like other manufacturers, the Philips line of defibrillators may include such optional features as noninvasive pacing, continuous end-tidal CO2 monitoring, noninvasive blood pressure, pulse oximetry, invasive pressure monitoring, and CPR measurement and feedback tools. Further details and specifications regarding the operation and maintenance of the HeartStart line of Philips products can be found at www.healthcare.philips.com.

FIGURE 45.8. Philips defibrillator. (Courtesy of Philips Healthcare.)
Physio-Control Defibrillators
Medtronic offers both manual and automatic external defibrillators through its subsidiary Physio-Control, with the Lifepak 20e being the most advanced product it offers (Fig. 45.9); the ability to monitor oxygen saturation, carbon monoxide, and methemoglobin levels is a feature available through Physio-Control. They also have a CPR rhythm guide to help providers time chest compressions and ventilation and a “Code Management Module” that includes wireless connectivity. Further details and specifications regarding the Lifepak line of Physio-Control products can be found at www.physio-control.com.

FIGURE 45.9. Lifepak Physio-Control Defibrillator. (Courtesy of Physio-Control, Inc.)
Zoll Defibrillators
Zoll manufactures automatic and manual defibrillator models, ranging from the Zoll E Series defibrillator designed for the emergency medical services (EMS) personnel up to the Zoll X Series monitor defibrillators that combine the features of advanced vital sign monitoring with the defibrillator unit (Fig. 45.10).

FIGURE 45.10. Zoll defibrillator. (Courtesy of Zoll Medical Corporation.)
Other optional features of Zoll defibrillators that may be encountered include noninvasive pacing, continuous end-tidal CO2 monitoring, and specialized adhesive gel pads called “CPR-D-padz,” which provide guidance on the quality of CPR chest compressions being provided when connected to the new advanced models. Zoll also offers the ability for the defibrillator to work as a transport monitor with optional pulse oximetry as well as invasive and noninvasive blood pressure monitoring. Further details and specifications regarding the operation and maintenance of the Zoll line of defibrillators can be found at www.zoll.com.
AEDs
AEDs are manufactured by many companies including Philips, Zoll, Physio-Control, and Defibtech. Each manufacturer has slightly different designs; however, all models have pads that are attached to the chest and automated programs that determine if there is a shockable rhythm and deploy a shock with minimal interaction from the first responder. This design makes the device easy to use by almost anyone, even with little to no medical training, and saves lives by minimizing the time from arrest to delivery of defibrillation in appropriate situations. Many hospitals keep AEDs in outpatient and visitor areas of the hospital, as rapid shock (possibly even by a layperson) is so critical to survival from cardiac arrest. Most public facilities (airports, large stores, subway stations) also prominently display AEDs, and you should not hesitate to ask for and use one; they are truly easy to use, and you may save a life.
Phillips AEDs
Philips AEDs include the HeartStart line, which includes voice prompts and CPR coaching.
The HeartStart line includes several AED models targeted to community use (i.e., lay persons), first responder use (with event data collection capabilities and training modules), and clinical use (with patient-specific guidance for CPR or defibrillation) (Fig. 45.11). More details can be found at www.heartstart.com.
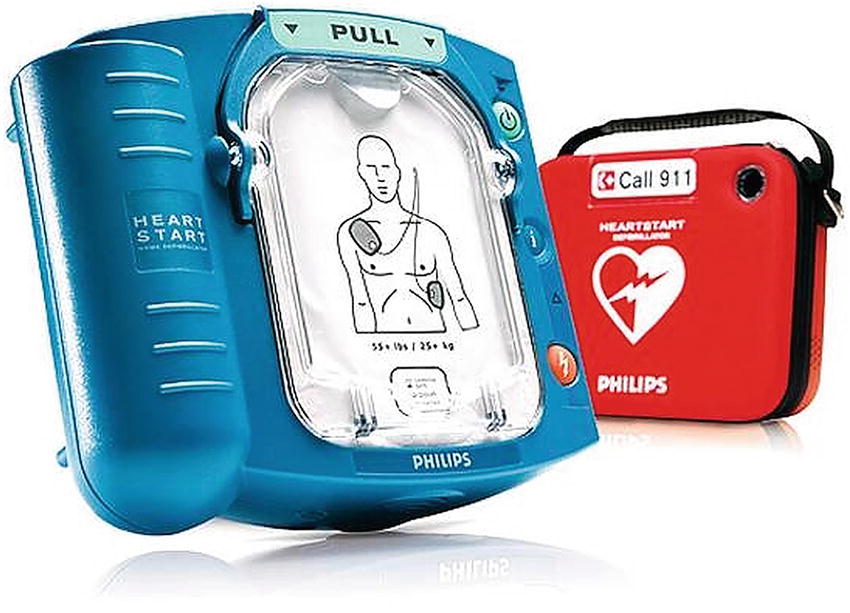
FIGURE 45.11. Philips HeartStart AED. (Courtesy of Philips Healthcare.)
Zoll AEDs
Zoll offers AEDs targeted to hospital professionals, first responders, and laypersons, many of which include real-time CPR feedback (Fig. 45.12).
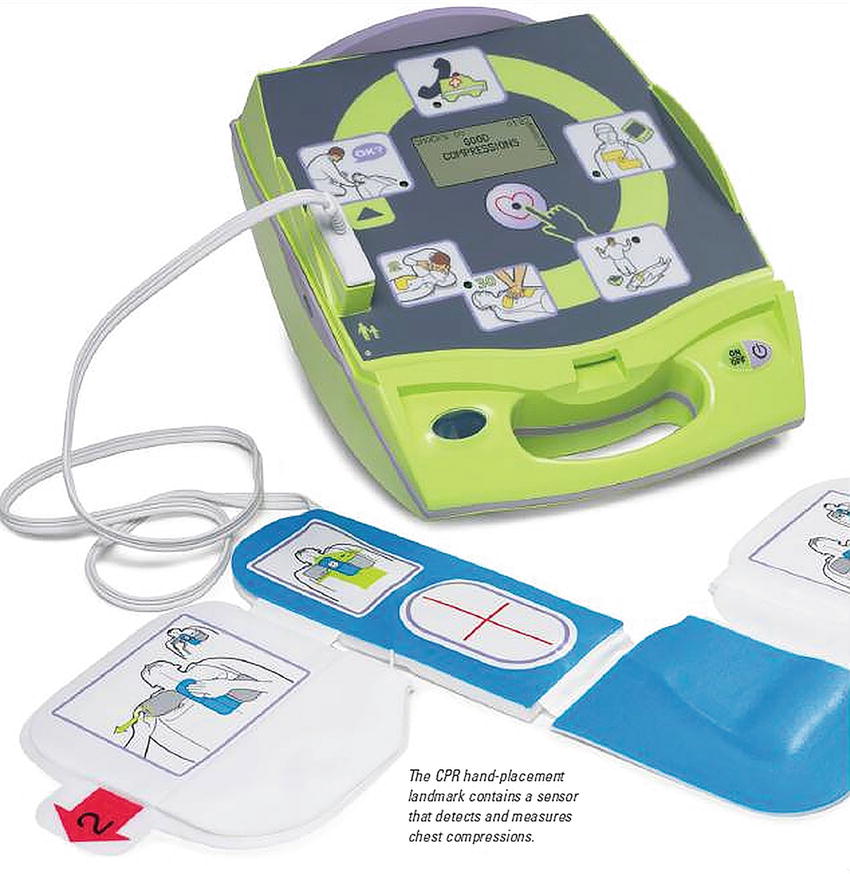
FIGURE 45.12. Zoll AED. (Courtesy of Zoll Medical Corporation.)
More information can be found at Zoll.com.
Physio-Control AEDs
Physio-Control AEDs include the Lifepak line that offers AEDs for lay and professional first responders (Fig. 45.13).

FIGURE 45.13. Physio-Control AED. (Courtesy of Physio-Control, Inc.)
Information on Physio-Control AEDs can be found at www.physio-control.com.
Defibtech AEDs
Defibtech offers the Lifeline series of AEDs that range from simple automated AEDs to ones with color display for ACLS guidance and rhythm display (Fig. 45.14).

FIGURE 45.14. Defibtech AED. (Courtesy of Defibtech AED.)
Further details can be found at defibtech-lifeline.com.
Summary
Most health care providers outside of the cardiac catheterization, electrophysiology laboratory, cardiac ORs, intensive care units, or rapid response teams do not regularly use defibrillators. Defibrillators are the first line of treatment for certain life-threatening arrhythmias. Anesthesia technicians are often responsible for the maintenance and deployment of these critical pieces of equipment and, as members of the anesthesia team, may be called upon to assist with resuscitation. Therefore, as an anesthesia technician, you should be familiar with defibrillator operation. Although there are several different manufacturers of these devices, they share several common steps to operate them: turn the power on, attach pads and ECG leads, analyze the rhythm manually or automatically, select the energy level, select synchronization if necessary, charge the device, and deliver the shock once confirming no surrounding responders are touching the patient and no water or other environmental hazards exist.
Review Questions
1. How does an AED differ from a manual external defibrillator?
A) User is provided guidance about whether the cardiac rhythm should be treated with defibrillation.
B) External pacing is automatically started without any user input.
C) Shock is applied without any user input.
D) All of the above.
Answer: A
AEDs have a computer that can analyze the cardiac rhythm to determine if it is VT or VF. If the computer determines that it is one of these two rhythms, it will give the user a prompt that a shock is advised. Most modern manual defibrillators come equipped with an AED mode as well.
2. On a monophasic manual external defibrillator, the optimal dose for defibrillation of an adult patient is
A) Device specific
B) 120 J
C) 200 J
D) 360 J
E) None of the above
Answer: D
Monophasic defibrillators should be set to 360 J for defibrillation. Biphasic defibrillators should be set to the manufacturer’s suggested energy level, which is usually between 120 and 200 J.
3. Compared to defibrillation using adhesive gel pads, defibrillation using internal cardiac paddles requires
A) No change in energy output setting
B) Increase in energy output setting
C) Decrease in energy output setting
D) A specific defibrillator for internal defibrillation
E) None of the above
Answer: C
Because internal paddles are applied directly to the heart, the energy setting is much lower than that used by external paddles or pads.
4. What type of training is required to operate an AED?
A) ACLS certification
B) BLS certification
C) None
D) Should only be operated by a physician
E) Should only be operated by cardiologists
Answer: C
AEDs are designed to be operated by individuals without any (or minimal) training. A series of audio prompts and visual instructions will be given once the device is powered up.
5. How frequently should a defibrillator and the associated equipment be tested for functionality?
A) Monthly
B) Weekly
C) Daily
D) At the change of every shift
E) Only after they have been used
Answer: D
Because of the lifesaving nature of this equipment, most institutions require that it be checked at every shift change. In addition, a record of the testing results should be kept in a log.
6. When adhesive gel pads are placed in the standard anterolateral position, the anterior pad should be placed
A) Directly over the heart
B) To the right of the sternum below the clavicle
C) On the right chest, lateral to and below the nipple
D) Directly over the sternum
E) On the anterior abdomen
Answer: B
The anterior pad should be placed just to the right of the sternum and below the clavicle. Multiple positions of the pads are acceptable including anterolateral and anteroposterior.
7. Prior to the delivery of a defibrillating shock with a manual defibrillator, the device must first be
A) Charged
B) Synced
C) Paced
D) Analyzed
E) None of the above
Answer: A
Prior to delivery of a shock, the device must be charged. Most devices will have a default energy level that may have to be adjusted depending upon the clinical situation. Although analysis should be performed prior to shock delivery, the best answer is charging the device.
8. Complications that can occur from improper use of a defibrillator include
A) Fire
B) Electrical shock of responding medical personnel in contact with the patient
C) Skin burns to the patient
D) All of the above
Answer: D
Vigilance is required to minimize the risk of complications associated with defibrillator use such as inadvertent spread of electrical current that can cause injury to responding medical personnel or ignition of a fire, as well as to prevent injury to the patient such as skin burns.
9. Research has shown that for every minute defibrillation is delayed, survival decreases by
A) 1%
B) 2%-3%
C) 4%-6%
D) 7%-10%
Answer: D
Research has shown that survival is decreased by 7%-10% for every minute defibrillation is delayed.
10. Manual analysis of the patient’s rhythm by the medical team can occur
A) During chest compressions
B) Only when in a “synchronous” mode
C) Only when the patient is not being moved
D) Only when using an AED
Answer: C
It is important to only analyze the patient rhythm after ensuring the proper leads/pads are connected to the patient and that interference is not occurring while the patient is being moved such as during chest compressions. Otherwise this may lead to health care providers inaccurately thinking the patient is in asystole during a disconnection or in VF/VT during excessive interference.
SUGGESTED READINGS
Blom MT, Beesems SG, Homma PC, et al. Improved survival after out-of-hospital cardiac arrest and use of automated external defibrillators. Circulation. 2014;130:1868-1875.
Brooks SC, Anderson ML, Bruder E, et al. Part 6: alternative techniques and ancillary devices for cardiopulmonary resuscitation: 2015 American Heart Association Guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015; 132:S436-S443.
Link MS, Atkins DL, Passman RS, et al. Part 6: electrical therapies: automated external defibrillators, defibrillation, cardioversion, and pacing: 2010 American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(suppl 3):S706-S719.
Philips Electronics N.V. Philips HeartStart XL Instructions for Use. M4735-91900 Edition 7. Eindhoven, The Netherlands: Koninklijke Philips Electronics N.V.; 2006.
Physio-Control, Inc. Physio-Control Lifepak 20e Defibrillator/Monitor Operating Instructions. Redmond, WA: Physio-Control, Inc.; 2010.
Wald DA. Therapeutic procedures in the emergency department patient with acute myocardial infarction. Emerg Med Clin North Am. 2001;19:451-467.
Zoll Medical Corporation. Zoll M Series Operator’s Manual. 9650-0200-01 Rev YH. Chelmsford, MA: Zoll Medical Corporation; 2010.