Conducting Your Own Insomnia Self-Assessment
In this chapter, you will cultivate your sense of control over sleep by conducting your own insomnia self-assessment. This assessment, which is the same one I conduct with my patients, is invaluable in learning to conquer insomnia, for it will assist you in evaluating your present sleep pattern, identifying your particular thoughts and behaviors that are causing insomnia, and determining if medical or mental health problems may be contributing to your insomnia.
By conducting your own insomnia self-assessment, you will increase your awareness and understanding of the thoughts and behaviors causing your insomnia. This will help you cultivate a greater sense of control over your sleep. You will feel more relaxed and empowered and will sleep better as a result. Then, in the chapters that follow, we will investigate how these thoughts and behaviors cause insomnia and examine step-by-step techniques for changing these habits.
The first step in conducting your insomnia self-assessment is to accurately establish your current sleep pattern, or what is called your baseline sleep pattern.
First, you will need to complete the sleep diary on the following page for seven consecutive mornings. I call this the 60-Second Sleep Diary because it will require only about one minute of your time to fill out each morning when you get out of bed. Take a few moments to review the 60-Second Sleep Diary; it is the same diary used by my patients. (You will need to make seven copies of the diary.)
Most of the items on the 60-Second Sleep Diary are very straightforward. However, three require some additional explanation that will make it easier for you to complete the diary each morning.
1. If you fill out the diary on Monday morning, write “Sunday” in the space marked “night”; if you fill it out on Friday morning, write Thursday in the space marked “night,” and so on.
2. Question 7: record the number of hours you allotted for sleep by determining the number of hours elapsed between the time you turned the lights off to go to sleep (question 1) and the time you got out of bed (question 5). For example, if you turned the lights off at 11:00 P.M. and got out of bed at 7:00 A.M, you allotted eights hours for sleep.
3. Question 9: record the dose and the number of prescription or over-the-counter sleeping pills that you took before going to sleep or during the night.
Keep in mind that the 60-Second Sleep Diary is not meant to promote clock-watching. If you are overly concerned about how long it took you to fall asleep or how long you were awake during the night, you may feel more anxious about your sleep. That’s
why you need only estimate within thirty minutes the time it took you to fall asleep or the length of a nighttime awakening.
60-SECOND SLEEP DIARY
Night ______ Date ____________
1. Last night, what time did you get into bed? ____________
Turn the lights off? __________________________
2. About how long did it take you to fall asleep? __________
_________________________________________________
3. About how many times did you awaken during the night?____
_________________________________________________
4. For each awakening, about how long were you awake?
1st ____________ 2nd __________________
3rd ____________ 4th __________________
5. What time was your final wake-up this morning? ________
What time did you get out of bed? _________________
6. Approximately how many hours did you sleep last night? ____
_________________________________________________
7. How many hours did you allot for sleep last night (time elapsed from “lights out” to “out of bed”)? _________________
8. Rate the quality of last night’s sleep:
9. Sleep medications taken _______________________
After you have completed the 60-Second Sleep Diary for seven consecutive mornings, you are ready to determine your baseline sleep pattern. Using your seven sleep diaries, answer the following questions:
• How many nights per week do you have difficulty falling asleep? _____ On these nights, how much time, on average, does it take you to fall asleep? ___________________________
• How many nights per week do you wake up and have difficulty
falling back to sleep? ___ On these nights, how often do you typically wake up?_____ On average, what is the total amount of time that you lie awake during the night after these awakenings?
_________________________________________________
• How many days per week is your final wake-up earlier than desired?
_________________________________________________
• On nights when you have insomnia, how many hours on average do you sleep? ____________________________
• On nights when you don’t have insomnia, how many hours on average do you sleep? __________________________
• How many nights per week do you experience a good night of sleep? _________________________________
• How many nights per week do you take sleeping pills? _____ On these nights, what is the average number of pills you take? _____ What is the typical dose? _____________________
• What is your average sleep-quality rating on a scale of 1 to 5?
_________________________________________________
Your answers to these questions represent your baseline sleep pattern, which will serve as an objective reference point that will allow you to monitor the improvements in your sleep during this program. Therefore, it is important to keep a record of your baseline sleep pattern for future reference. There is another benefit to objectively assessing your baseline sleep pattern: you may realize that you are actually sleeping better than you think!
Once you have established your baseline, you should continue to fill out the 60-Second Sleep Diary each morning throughout the six-week program described in the following chapters. Completing the diary throughout this program is essential for tracking improvements in your sleep and aiding you in using many of the techniques described subsequently.
Once you have established your baseline sleep pattern, you are ready to assess the factors that are disturbing your sleep. Let’s begin by assessing your sleep-scheduling behaviors.
Your Sleep-Scheduling Behaviors
Your sleep-scheduling behaviors include when you go to bed, how much time you spend in bed, when you get out of bed, and whether you nap. In an effort to cope with insomnia, many insomniacs, such as Jonathan, engage in multiple sleep-scheduling behaviors that disturb sleep.
Jonathan believed that the best way to compensate for insomnia was to go to bed early and to sleep later on weekends in an effort to catch up on the sleep he lost during the week. And even though Jonathan averaged only five hours of sleep per night, he routinely spent eight hours in bed each night. Because Jonathan worked at home two days a week, he also took long afternoon naps in an effort to catch up on his sleep.
Although these strategies may have helped Jonathan to cope with insomnia in the short term, he didn’t realize that, in the long run, these sleep-scheduling behaviors were actually exacerbating his insomnia by altering his body-temperature rhythm and weakening his brain’s sleep system.
To assess your sleep-scheduling behaviors, answer the following questions using your sleep diaries as a reference.
• What time do you usually get into bed? ______________ Get out of bed? __________________________
• Does the amount of time that you spend in bed exceed the amount of time that you actually sleep? ___ If so, by how much? ______
• Do you have an inconsistent rising time or sleep later on weekends compared to weekdays? ___________________________________
• Do you nap? ______ If yes, how many times per week and for how long? __________________________________
Later, we’ll explore in detail how these maladaptive sleep-scheduling behaviors cause insomnia and how to improve your sleep by changing these behaviors.
Is Your Bedroom a Learned Cue for Wakefulness?
Mary did all of her television viewing in her bedroom. She also graded her students’ papers and spent a lot of time talking on her telephone while lying on her bed. During the hour prior to bedtime, Mary and her husband often discussed emotionally charged topics. When she couldn’t sleep, Mary simply stayed in bed in the belief that if she simply tried harder, sleep would eventually come.
Contrary to what many insomniacs think, these behaviors do not aid sleep. Rather, they disturb sleep and heighten insomnia by causing bedtime, the bedroom, and the bed to become learned cues for wakefulness rather than relaxation, drowsiness, and sleep. Assess whether you are engaging in similar behaviors that are contributing to insomnia:
• Do you use your bedroom as an office, for watching television, or for talking on the telephone? _____________________
• Do you go to bed when your spouse/significant other does or because the 10:00 or 11:00 P.M. news is over rather than because you are drowsy? ______________________________
• Do you toss and turn and try to force sleep when you can’t fall asleep? _______________________________
• Do you fall asleep easily anywhere except your bedroom?
• Do you work on the computer, pay bills, or discuss problems or emotional issues with your spouse/significant other during the hour before bedtime? _________________________
Later, we will explore proven techniques for improving sleep by changing these sleep-incompatible behaviors.
How Do You Think About Your Sleep?
Next, assess whether the way you think about your sleep is exacerbating your insomnia.
• Are you anxious about insomnia or perhaps do you fear it?
• Do you tell yourself you won’t be able to function during the day if you don’t sleep well?
• Do you tell yourself you must have eight hours’ sleep to perform effectively?
• Do you always blame poor daytime functioning on insomnia?
As we will soon explore, negative stressful thoughts about sleep only serve to exacerbate insomnia. You’ll learn how to recognize and challenge these distorted, negative thoughts and replace them with more positive, accurate thoughts about sleep. These positive thoughts will relax you and improve your sleep.
In this section, you will assess lifestyle behaviors that affect your sleep and determine whether your sleep environment is conducive to sleep.
First, do you engage in regular physical activity such as walking, running, or other forms of aerobic exercise? Or do you lead a sedentary lifestyle? Whereas regular exercise and physical activity can improve sleep by causing your body-temperature rhythm to rise and fall during the day, lack of physical activity can contribute to insomnia by causing a flattening of your body-temperature rhythm. Exercise may also contribute to more healthy sleep by improving your mood.
David came to my program because he routinely woke up for two or three hours in the middle of the night. Although he had been thinking about starting an exercise program, it wasn’t until he learned
that exercise can have a beneficial effect on sleep that he started jogging. Within a week, David noticed that he was sleeping more deeply and was waking for significantly shorter periods of time. Within a month, David’s sleep was significantly improved.
We will review the positive effects of exercise on sleep. We will also explore various types of exercise, how to start an exercise program, and the beneficial effects of exercise on mood and health.
Consider another factor: do you receive regular exposure to sunlight? Recall that sunlight is an important timing mechanism for sleep. Light is also important for improving mood and energy. If you work indoors, you may be exacerbating insomnia by restricting your exposure to sunlight. We will soon examine the beneficial effects of light on sleep, mood, and health. We’ll also review techniques for strengthening your sleep rhythm by increasing exposure to sunlight or artificial bright light.
How about your use of caffeinated beverages in the late afternoon or early evening? Do you drink more than two caffeinated beverages per day? Caffeine can impair sleep by virtue of its stimulant and withdrawal effects.
Lee often felt wide awake at bedtime and usually took at least an hour to fall asleep. When Lee was asked about his caffeine use, he replied that he routinely drank coffee or cola in the afternoon and ate chocolate before bedtime. Lee did not realize that the caffeine in coffee, cola, and chocolate was probably making it more difficult for him to fall asleep.
Shortly, you will learn about the effects of caffeine-containing beverages, foods, and medications on sleep and how to minimize these effects.
And what about your consumption of alcoholic beverages in the evening? How many do you drink and how often? As we will explore in chapter 7, alcohol may help you fall asleep more easily, but it can diminish deep sleep and cause you to wake up during the night. And if you are abusing alcohol, you may be contributing to long-term impairment of your sleep.
Here are four questions to determine if you are abusing alcohol.
1. Have you ever felt you should cut down on your drinking?
2. Have people annoyed you by criticizing your drinking?
3. Have you ever felt bad or guilty about your drinking?
4. Have you ever had a drink first thing in the morning to steady your nerves or to get rid of a hangover?
If you answered yes to any of these questions, you may be abusing alcohol and should consider seeking professional evaluation and treatment.
Smoking is another lifestyle behavior that can disturb sleep. If you smoke near bedtime or after waking during the night, the stimulant and withdrawal effects of nicotine may keep you awake. Smokers experience more sleep problems than nonsmokers, and smokers who quit smoking usually experience improved sleep. In chapter 7 we will explore the effects of nicotine on sleep and how to minimize these effects.
Finally, assess whether or not your sleep environment is conducive to sleep.
1. Is your sleep routinely disturbed by noises such as those made by family members, neighbors, or traffic?
2. Is the temperature of your bedroom comfortable at night?
3. Is your bedroom dark?
4. Is your bed comfortable? If you sleep with a partner, is your bed large enough?
Excessive noise and light can disturb sleep. So, too, can a bedroom that is too warm or too cold, an uncomfortable bed, and sleeping with a partner in a bed that is too small. In chapter 7 we will explore techniques for creating the ideal sleep environment.
Andrew had another stressful day. It started with a broken button on his shirt collar. Then, on the way to work, a broken water main
caused a traffic jam. After arriving late to work, Andrew received e-mail informing him that he would not be receiving a cost of living raise this year. And when he went to the credit union at lunch, the computers were down and the line was out the door.
When Andrew got home, his kids were fighting and his wife was upset that he had forgotten to pick up the dry cleaning. The grass needed to be cut and the toilet was running again.
By the time Andrew went to bed, his mind was racing and he had a headache. No wonder it took him several hours to fall asleep.
As Andrew’s story illustrates, we face a multitude of stressors in our work, family, and personal lives. Although some people cope well with daily stress, others experience negative emotional and physical responses that can disturb sleep, health, and well-being.
Stress and insomnia are inextricably linked: insomnia often begins in response to a stressful life event such as a death or divorce; it is one of the first warning signs of excessive daily stress; and many chronic insomniacs have a harder time sleeping after a stressful day.
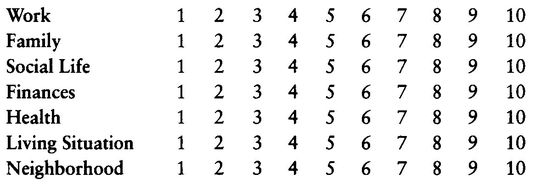
To assess your current stress level, complete the following two stress inventories; they are the same ones I use with my patients.
STRESS INVENTORY 1
For each area of daily stress, circle the number that corresponds to your perception of stress with 1 being no stress and 10 being the worst possible stress.
STRESS INVENTORY 2
The following is a checklist of some common stress warning signs. Check those that you experience on a weekly basis.
Feelings of frustration or anger ___
Racing or pounding heart ___
Feelings of agitation ___
Shallow or irregular breathing ___
Feeling on edge ___
Headaches ___
Stiff neck or shoulders ___
Upset stomach, excess gas, indigestion, diarrhea, or constipation ___
Cold or sweaty palms ___
Frequent urination ___
Racing or pounding heart ___
Feelings of agitation ___
Shallow or irregular breathing ___
Feeling on edge ___
Headaches ___
Stiff neck or shoulders ___
Upset stomach, excess gas, indigestion, diarrhea, or constipation ___
Cold or sweaty palms ___
Frequent urination ___
If you circled an 8 or higher on at least two of the scales on Stress inventory 1 and you checked at least two of the warning signs on Stress Inventory 2, you are probably experiencing high levels of daily stress.
The stress-management techniques described in subsequent chapters will teach you to manage excessive stress by learning to relax your mind and body each day. You will also learn to manage stress by recognizing and changing negative stressful thoughts and by developing stress-reducing attitudes and beliefs. By gaining more control over stress, you’ll sleep a lot better and your state of mind and health will also improve.
One of the central themes of this book is that thoughts and behaviors play the primary role in most cases of chronic insomnia. However, medical and mental health problems, certain underlying sleep disorders, and various drugs can contribute to disturbed sleep or even
play a primary role in some cases of chronic insomnia. Therefore, assessing whether these factors are affecting your sleep is an important part of your insomnia self-assessment.
Even if a medical or mental health problem, an underlying sleep disorder, or a drug is playing a role in your chronic insomnia, it is important to keep in mind that your thoughts and behaviors are still playing a primary role in your insomnia. Therefore, the techniques in this book should be used in conjunction with any treatment you receive for medical or mental health problems that may be disturbing your sleep.
Medical Problems That Can Affect Sleep
A wide range of medical problems can disturb sleep. Sometimes, the medical causes of poor sleep are obvious, such as pain from arthritis. At other times, the deleterious effects of medical problems on sleep are not so obvious, as in the case of hyperthyroidism.
The following is a list of some common medical problems that can disturb sleep. If you suspect that you have any of these problems, or if you haven’t seen your doctor in a while, schedule a thorough medical evaluation so that he or she can more thoroughly evaluate whether any of these problems may be affecting your sleep.
• Angina, a condition in which the heart receives insufficient oxygen, thereby causing pain that can disturb sleep
• Asthma, bronchitis, and emphysema, conditions that disturb sleep by interfering with breathing
• Allergies, congestion, or coughing
• Indigestion, reflux, or ulcers, which are gastrointestinal conditions that disrupt sleep by causing heartburn or acid regurgitation; these conditions can be treated with dietary changes and medication
• Bladder problems such as frequent urination
• Arthritis and chronic pain conditions
• Headaches
• Epilepsy, which causes abnormal electrical activity in the brain that can disturb sleep
• Hyperthyroidism, a condition caused by an overproductive thyroid gland
• Kidney disease
• Diabetes and hypoglycemia
• Dementia or Alzheimer’s disease, both of which can cause nighttime agitation, confusion, and insomnia
Medical Conditions Specific to Women
There are a number of women’s medical conditions that can disturb sleep. For example, insomnia is common during the last trimester of pregnancy. This can be caused by the stress of the pregnancy and anticipation of the birth or by fetal movements and the physical discomfort of pregnancy.
Patti, who was eight months pregnant, did not look forward to bedtime. She had a hard time falling asleep, in part because she could not get comfortable and because she often found herself thinking about the stress of labor. Once asleep, Patti woke up repeatedly during the night, either because she felt hot or because of the pressure on her bladder caused by her fetus. By the time Patti woke up in the morning, she felt exhausted. Even though she believed caffeine was not good for her fetus, she often drank a cup of coffee in the morning to get herself going.
Although some insomnia is normal and unavoidable during pregnancy, regular insomnia like Patti’s, during the last trimester, can be managed by using the techniques in parts II and III of this book. These techniques can also ensure that short-term insomnia during pregnancy doesn’t evolve into chronic insomnia. The stress-management techniques in part III can also be a valuable asset in managing the stress and anxiety that many women (and men!) experience during pregnancy.
Menopause is another medical condition that can disrupt women’s sleep. The hormonal changes associated with menopause may be one cause of these sleep difficulties; another is the hot flashes of menopause, which result in sensations of increased body temperature
and night sweats that are disruptive to sleep. Many women also experience emotional changes and depression during menopause that can contribute to insomnia.
If you are menopausal, talk with your doctor about the available treatments for menopause, which may lead to improved sleep. You should also practice the techniques in this book to minimize menopause-related sleep disturbances and to prevent short-term insomnia from becoming chronic. Recent research suggests that the relaxation techniques described in part III can be effective in reducing the frequency and severity of menopausal hot flashes.
Premenstrual syndrome (PMS) is another medical condition that can disrupt sleep. For some women, sleep difficulties coincide with the onset of the menses and the negative mood that can occur at this time. Many of my female patients have found the techniques in this program to be effective for minimizing PMS-related sleep problems.
Prescription and Over-the-Counter Drugs
A significant number of prescription and over-the-counter (OTC) drugs can disturb sleep either by causing stimulant or withdrawal effects. Drugs can also impair the quality of your sleep by suppressing deep sleep or dream sleep.
If you are taking prescription drugs, ask your doctor if the drugs may be disturbing your sleep and whether modifying the medication dose or even switching to another related medication that won’t adversely affect your sleep is possible. In some cases, simply taking the medication earlier may eliminate sleep problems. If you are taking an OTC, read the medication label carefully or ask your pharmacist if you are uncertain whether it contains sleep-disrupting ingredients.
Listed below are some common types of prescription and OTC medications that can disturb sleep.
• Analgesics that contain caffeine, such as Anacin and Excedrin
• Prescription diet pills
• Steroids
• Beta blockers and some other drugs used for treating high blood pressure
• Nasal decongestants that contain stimulants
• Asthma medications that have stimulating effects
• Thyroid hormones
• Some antidepressant medications
• Drugs for Parkinson’s disease
Illicit Drugs
Illicit drugs such as cocaine and amphetamines (speed) have powerful stimulant effects that can make it harder to fall asleep. These drugs can also compromise sleep quality by reducing deep sleep and dream sleep. Because cocaine and amphetamines are highly addictive, they can also cause withdrawal effects that affect sleep.
Marijuana is a widely used recreational drug that can have variable effects on sleep. For some users, marijuana can have relaxing, sedating properties; for others, it can act as a stimulant and make it harder to fall asleep. Research also suggests that long-term marijuana use can impair sleep by reducing dream sleep.
If you are using illicit drugs, your sleep may improve if you stop. If you can’t quit, you should consider seeking professional treatment.
Mental Health Problems
DEPRESSION Everyone feels sad or blue at times. However, about 10 to 20 percent of Americans experience serious depression at some point in their lives, and the numbers are growing. Serious depression, called major depression, can be caused by a variety of factors, including genetics, loneliness, lack of social support, alcohol or drug use, negative life events, and negative thinking.
Insomnia, particularly sleep-maintenance insomnia and early morning awakening, is a hallmark symptom of major depression. Some depressed individuals may instead exhibit excessive sleep, called hypersomnia.
Depressed people exhibit a number of other sleep disturbances, including reduced deep sleep, increased light sleep, and excessive REM sleep. They enter REM sleep earlier in the night and spend a greater percentage of time in REM sleep than nondepressed people. Recent
research also suggests that the dream content of depressed people is more depressing than that of nondepressed people.
These findings concerning REM sleep disturbances in depression, coupled with the fact that antidepressant drugs work in part by suppressing REM sleep, suggest that abnormalities in dream sleep may be a cause of major depression. Interestingly, research has demonstrated that REM sleep deprivation (accomplished by waking people whenever they start to dream) can produce the same antidepressant effects as antidepressant medications. Unfortunately, REM sleep deprivation is unpleasant and impractical.
Another physiological abnormality associated with depression is a flattened body-temperature rhythm; that is, a depressed person’s body temperature doesn’t rise and fall as much during the day as that of a nondepressed person. As you will recall, insomniacs exhibit the same problem with their body-temperature rhythm. This irregular rhythm in depressed people, which may be the result of the increased fatigue and reduced physical activity that accompany depression, may ultimately exacerbate insomnia and depressed mood.
Major depression doesn’t just affect sleep, it also affects the way we think, behave, and interact with others. When one is depressed, one feels hopeless, helpless, and experiences little pleasure or joy in life. Depressed people are also at greater risk for a variety of health problems, such as cardiovascular diseases and lowered life expectancy. Depression also weakens our immune systems and is a risk factor for suicide. Therefore, if you are experiencing major depression, it is essential that you seek professional evaluation and treatment.
To help you determine whether you have major depression, think about whether you have experienced any of the following symptoms nearly every day for a two-week period in the past few months.
1. A relatively prominent, persistent depressed mood that is characterized by feeling sad, blue, hopeless, low, down in the dumps, and irritable
2. Loss of interest or pleasure in all or almost all usual activities and pastimes
3. Poor appetite or significant weight loss when not dieting or increased appetite and significant weight gain
4. Insomnia
5. Restlessness or lethargy that is observable by others
6. Loss of interest in sexual activity
7. Fatigue or loss of energy
8. Feelings of worthlessness or guilt
9. Diminished ability to think or concentrate
10. Thoughts of death or suicide
If you have experienced symptom 1 or 2 and at least four of symptoms 3-10, you may have major depression and should seek professional evaluation and treatment.
Major depression can be successfully treated in several ways. One treatment involves the use of antidepressant medications such as Prozac, which are highly effective in about 70 percent of cases. These medications, which are not addicting, usually take a few weeks to lessen depression and may cause some temporary side effects, such as dry mouth and constipation.
The most effective nondrug treatment for depression is cognitive therapy. The word cognitive relates to your thoughts. Cognitive therapy is based on the premise that our negative moods and stress come from our negative, distorted thoughts. Cognitive therapy for depression involves learning to recognize, challenge, and change the negative, distorted thinking patterns that cause depressed moods. For many depressed people, cognitive therapy can be as effective as antidepressant medication—without the side effects. In some cases, the most effective treatment for depression involves a combination of cognitive therapy and antidepressant medication.
If you have some but not all of the symptoms of major depression, you have what is called mild or moderate depression. Sometimes, chronic insomnia can be the cause; in these cases, using the techniques in this book to improve sleep will also result in improved mood. As we will explore later, exercise can also be effective in alleviating mild to moderate depression.
ANXIETY Anxiety is another prevalent mental health problem that can disturb sleep. Anxiety is a feeling of apprehension, worry, or fear that differs from stress in a fundamental way. Whereas stress
involves a reaction to an identifiable external stressor or event, anxiety occurs in the absence of any identifiable event or precipitator.
Some anxiety is beneficial. It allows us to plan, search for alternatives, rehearse actions, and prepare for negative outcomes. But when we experience too much anxiety, our sleep, work, sense of pleasure, and relationships can suffer.
Excessive, maladaptive anxiety that interferes with daily living is called generalized anxiety disorder (GAD). GAD is characterized by persistent, excessive, unrealistic, uncontrollable worry that causes the person to constantly feel on edge. People with GAD cannot relax and enjoy life; they feel chronically irritable, have a harder time concentrating on things, report more sleep problems, and are at greater risk for numerous health problems such as high blood pressure, abnormal heart rhythms, heart attacks, and sudden death from heart disease.
The physical symptoms of GAD include
• Shakiness, jitteriness, trembling, or jumpiness
• Eyelid twitching, furrowed brow, or strained face
• Heart pounding or racing, sweating, cold and clammy hands, or dry mouth
• A knot in the stomach, a lump in the throat, or a fast breathing rate
The most common treatment for GAD is antianxiety medication, which is helpful in controlling the problem. However, like sleeping pills, these medications can have side effects such as dependence and tolerance. Some people attempt to self-medicate their anxiety by drinking alcohol. However, alcohol actually increases anxiety.
For many people, cognitive behavioral therapy, in which the individual learns to change the thoughts, behaviors, and bodily responses associated with GAD, can be a highly effective nondrug treatment. The self-help techniques described in part III can also be highly effective in controlling anxiety. In fact, research has consistently shown that these techniques can be as effective as, or more effective than, antianxiety medication. Other self-help techniques for managing anxiety include cutting back on caffeine and exercising, which we will explore in chapter 7.
POST-TRAUMATIC STRESS DISORDER (PTSD) A less common mental health problem that can cause insomnia is post-traumatic stress disorder (PTSD). In PTSD, a traumatic event (such as physical or sexual abuse, war, or a natural disaster) is continually reexperienced emotionally. This chronic “reliving” of the trauma results in fear, anxiety, physical stress responses, insomnia, and nightmares. If you have experienced a trauma and think that you may be suffering from PTSD, you should seek help from a mental health professional who specializes in this condition.
Underlying Sleep Disorders
SLEEP APNEA James, a fifty-year-old man, complained of excessive daytime sleepiness. He was also overweight, had high blood pressure, and often awakened in the morning with a headache. James’s wife reported that he snored loudly and often woke briefly during the night, making choking or gasping sounds. James denied any knowledge of this behavior; in fact, he believed he was a sound sleeper.
James has a syndrome called sleep apnea, which is more prevalent in older individuals, men, and overweight people. This sleep disorder causes breathing to stop during sleep for anywhere from ten seconds up to several minutes. These pauses in breathing, called apneas, can occur hundreds of times a night and are more likely to occur in certain positions, particularly when sleeping on the back. If apnea is severe enough, the sleeper wakes gasping for breath and may never get more than five minutes of uninterrupted sleep all night.
When apnea occurs, the cessation in breathing causes a drop in blood oxygen levels, forcing the heart to labor harder to keep the blood oxygenated. For this reason, sleep apnea is a risk factor for hypertension, strokes, and heart disease. It can also cause chronic sleep disruption that may leave the patient feeling exhausted and sleepy during the day. In some cases of sleep apnea, daytime sleepiness can be severe enough to cause car accidents. In fact, a recent study found that people who have sleep apnea are seven times more likely to get into a car accident than the rest of the population. Therefore, if you
experience symptoms while you sleep such as loud snoring interrupted by periods of silence for ten seconds or longer, feeling unable to breath, or making gasping sounds, you may have sleep apnea and should be evaluated at a sleep disorders center.
There are multiple causes of apnea. These include a problem in the brain’s respiration center; obstruction of the breathing passages caused by the tongue, tonsils or adenoids, fat deposits, or excess tissue in the throat; and structural abnormalities in the throat or jaw. The self-help treatments for apnea include avoiding sleeping on your back (by wearing a T-shirt to bed that has a tennis ball sewn into the back of it, you will be less likely to sleep on your back), using pillows to keep the head elevated, abstaining from alcohol and sleeping pills (which exacerbate sleep apnea), and losing weight.
The most effective medical treatment for sleep apnea is Continuous Positive Airway Pressure (CPAP), in which the person wears in bed a nasal mask that is attached to a machine that pushes air through the nose to keep the breathing passages open. In severe cases of apnea, surgery may be necessary to increase the size of the breathing passages or to correct structural abnormalities in the upper airway.
PERIODIC LIMB MOVEMENTS (PLM) PLM is another disorder that can disturb sleep. PLMs are not the same as the occasional body jerks, called hypnic jerks, that some people experience at the onset of sleep. Rather, PLMs are episodes lasting from a few minutes to several hours during sleep that involve the legs or arms twitching, jerking, or even kicking repeatedly. Like sleep apnea, the interruptions in sleep caused by PLM can leave the person feeling exhausted and sleepy during the day. If you wake up with your bedcovers in disarray, or if a bed partner has told you that you jerk or kick during sleep, you may have PLM and should be evaluated at a sleep disorders center.
Sleep researchers don’t really know what causes PLM. Warm baths before bedtime are sometimes helpful in alleviating PLM symptoms. However, muscle-relaxing medications are the most effective treatment. These medications suppress the PLMs or help the person sleep through them, but the medications don’t cure PLM and can become addicting. Unfortunately, no satisfactory nondrug treatment for PLM currently exists.
DIAGNOSING SLEEP APNEA AND PLM USING ALL-NIGHT SLEEP STUDIES Sleep apnea and PLM can be definitively diagnosed only by an all-night sleep study. These studies are conducted at a sleep disorders clinic, which has private rooms that resemble a bedroom or hotel room complete with bathroom, television, and radio. On the night of the study, the patient arrives an hour before his or her usual bedtime and is hooked up for the sleep recording. This procedure involves attaching several electrodes to the scalp to create an electroencephalogram (EEG), which measures brain waves, and to the chin and around the eyes to measure muscle tension and eye movements. Sensors are also placed on the body to measure blood oxygen levels (this is usually done by attaching a meter to the earlobe), respiration, heart rate, and leg movements. An all-night sleep study is called a polysomnogram, because multiple physiological measures are recorded while the individual is asleep.
Once the patient is hooked up, he or she is asked to go to sleep while the multiple physiological measurements are obtained throughout the night. In the morning, the polysomnogram is analyzed by a sleep specialist, who can determine whether the patient actually suffers from sleep apnea or PLM.
RESTLESS LEGS Restless legs is a disorder that causes unpleasant sensations in the legs while lying down. These sensations, which are often described as a creeping or crawling sensation in the calves, typically occur at bedtime when the person is still awake, and can therefore make it difficult to fall asleep. Many people with PLM also have restless legs syndrome, and almost all people with restless legs have PLM.
The sensations of restless legs result in a strong urge to move the legs, massage them, or walk around, all of which alleviate the discomfort. Self-help techniques for this disorder include exercise, elimination of caffeine, and some dietary supplements such as iron, calcium, and folic acid. The usual medical treatment for restless legs involves various types of sedative medications that can reduce the severity of this condition but can’t cure it.
DELAYED PHASE DISORDER Individuals with this disorder can’t fall asleep until late at night, often around 3:00 or 4:00 A.M. Once
asleep, however, they usually sleep well for seven or eight hours and awaken feeling refreshed.
The opposite of delayed phase disorder is advanced phase disorder. This condition, which is most common among the elderly, is characterized by falling asleep early in the evening, around 8:00 P.M. for example, then waking in the predawn hours and being unable to fall back to sleep.
Delayed and advanced phase disorders are caused by a body-temperature rhythm that either falls too late or too early at night, respectively. These disorders are treated at sleep disorders centers by using artificial bright-light boxes to normalize the body-temperature rhythm.
NIGHTMARES A nightmare is a frightening dream that usually involves themes of danger, being chased, being killed, or falling. Because our muscles are paralyzed when we dream, we feel trapped during a nightmare and therefore wake up feeling fearful and agitated. Nightmares usually occur in the second half of the night, when dream sleep is more prominent.
Although occasional nightmares are normal, frequent nightmares are not. They are caused by a number of factors, including traumatic events such as abuse or natural disasters, or by underlying psychological conflicts that have not been adequately resolved.
One treatment for nightmares is the use of psychotherapy to alleviate the underlying conflict causing them. Another treatment involves behavioral therapy in which the nightmare sufferer is trained to write down the content of the nightmare, rewrite it with a different outcome, and to mentally rehearse this new outcome daily.
BRUXISM (TOOTH GRINDING) If you grind your teeth while you sleep, you may have bruxism. This disorder can result in tooth damage and morning jaw pain or headaches. The most common treatment is a rubber mouth guard that is worn to bed to prevent the grinding. However, bruxism also seems to be exacerbated by stress. Many patients who practice the stress-reduction techniques in part III of this book report significant improvement in symptoms of bruxism.
You have now completed your insomnia self-assessment. You should have a greater understanding of the particular thoughts and behaviors that are causing your insomnia. Now you are ready to begin the six-week program presented in chapters 5 through 10, in which you will learn more about why these thoughts and behaviors cause insomnia and, most important, step-by-step techniques for changing them.
You will begin this program by learning one of its most powerful techniques: cognitive restructuring. This technique will teach you how to improve your sleep by changing the way you think about your sleep. It will also be the initial catalyst for improving yourself and your life in a number of important ways.