1
Dead Crows Falling from the Sky
Medical detective Annie Fine was reluctant to venture out to Queens for a routine check on a few encephalitis patients at a neighborhood hospital in Flushing. The patients suffered from an inflammation of the brain that is typically triggered by some type of infection, and it was her task to make sure that the cases were not linked. She felt sure the long weekend of work would result only in a hodgepodge of unrelated cases—and a big waste of time. However, she was the epidemiologist “on call” for the New York City health department, and her friend and boss Marcelle Layton—Assistant Commissioner of the NYC Bureau of Communicable Diseases—had asked her to come along. To Fine’s surprise, it turned out to be one of the most fascinating episodes in her career, equal in interest to the investigation of the anthrax incidents of 2001, still two years in the future.
Something Strange
Though Fine did not realize it at the time, there actually would be two investigations—one about humans and one about birds—that moved on parallel tracks for a few hectic weeks and then converged into a surprising (and satisfactory) conclusion. The human track began on Monday, August 23, 1999, when Dr. Deborah S. Asnis, chief of infectious diseases at Flushing Hospital in Queens, called the NYC health department to report two cases of encephalitis in elderly patients, which included fever, headache, and mental confusion. Both patients had been previously active and healthy. One patient had a fairly unusual condition, flaccid paralysis (extreme muscle weakness) of the type that used to be associated with polio but is now more often a sign of botulism poisoning. He required a mechanical ventilator to breathe. Based on the totality of the symptoms, it looked like viral encephalitis. But if his illness were botulism (a potentially fatal bacterial disease), antitoxin should be administered right away, without waiting for test results. By Thursday, the second encephalitis patient was on a ventilator too.
New York City’s Communicable Diseases Program actively encourages doctors to call when they observe something unusual. Although the Assistant Commissioner’s staff was fairly small, her policy was to have a doctor respond to each call. This time, Layton, an internist trained in infectious diseases, took the call herself. She enjoyed keeping her hand in by speaking with local clinicians like Asnis, who (as one of the only infectious diseases specialist for adults in Queens) saw a lot of interesting cases. Asnis said the patient’s muscle weakness was not of the descending type, beginning in the upper body and gradually spreading downward, as expected with botulism.
Because the NYC public health laboratory did not test for viruses, Layton asked Asnis to send blood and cerebrospinal fluid samples to the virology laboratory at the New York State (NYS) Department of Health, which had initiated a program for testing specimens from people with undiagnosed encephalitis, in association with the Centers for Disease Control and Prevention (CDC). Layton also sent a staff member to Queens to review the patient’s chart and confirm that the symptoms suggested viral encephalitis rather than botulism. Asnis had noticed that several spinal taps had been ordered that summer to test for encephalitis or meningitis in elderly patients at Flushing Hospital. This stood out to her, as typically only two or three are ordered per year, most often when meningitis is suspected in a child or young adult.
Four days later, on Friday, August 27, Asnis called Layton to report a third case of encephalitis with muscle weakness in an elderly person at Flushing Hospital. During the call, she was interrupted by a neurologist colleague who had just returned from the New York Hospital Medical Center of Queens, where he had seen a fourth case of encephalitis, diagnosed as Guillain-Barré syndrome, an autoimmune condition sometimes triggered by infection. The coincidence was definitely strange! Layton spoke with foodborne disease experts at the CDC, who agreed that Asnis’ cases did not sound like botulism.
Fewer than ten cases of encephalitis are reported in New York City in an average year. Yet within the span of a week four patients from a small corner of Queens had been diagnosed and put on ventilators. Something was not right. Though fieldwork is not a regular part of an assistant commissioner’s job, Layton cancelled her weekend plans and called in Annie Fine.
The Investigators
Both Marci Layton and Annie Fine are primary-care doctors who came to New York City on two-year assignments as “EIS officers,” trainees in the CDC Epidemic Intelligence Service, the national training program for medical detectives. Layton, who grew up in the suburbs of Baltimore, became actively interested in science and medicine in her early teens. Inspired by the social ideals of the 1960s, she volunteered at hospital emergency rooms, local nursing homes, and summer programs for the mentally and physically disabled. As she grew from teenager to young adult, an ongoing succession of volunteer projects and short-term jobs opened her mind to the diversity of other lives—rich and poor, sick and well, American and foreign—-and to the diversity of medical practice. Her experience in rural areas in the United States reinforced her love of the outdoors, while her overseas experiences in Asia revealed the boundless possibilities of international travel. Both provided an intimate view of the huge impact of infectious diseases in poor communities.
As a medical student, Layton’s volunteer adventures included a summer at a rural clinic in West Virginia, where she roomed with a woman called Granny Parsons who had never before met a Jew or ventured more than a few miles from her “holler.” Layton also worked on the Navajo Reservation in the Four Corners area of the American southwest, where one of her mentors was Bruce Tempest, the Indian Health Service physician who (a few years later) reported the first cases of a previously unknown respiratory disease (see Chapter 7).
After her first long-term post-residency job—an unsatisfying stint in an understaffed family-care clinic in Providence, Rhode Island—Layton completed an infectious disease fellowship at Yale and decided to enter public health. When she joined EIS in 1992, Thomas Frieden, the outgoing EIS fellow assigned to NYC—who later became the director of the CDC—recommended New York as a place where an epidemiologist can work on a variety of diseases without leaving home. Layton thought of her EIS assignment as another short-term venture and did not expect to like New York, which she associated with the fancy shops and skyscrapers of midtown Manhattan. But over time she came to enjoy the unending challenges of working at the NYC health department, where she was hired as Assistant Commissioner upon completing her EIS fellowship. Today she is the “go-to” person for anyone seeking the big-city perspective on infectious disease issues in public health.
Annie Fine also came to public health after working as a primary-care doctor. Fine—who is currently settled in Brooklyn and is the mother of twins—had lived in many different East Coast cities as a child and teenager. After completing a residency in pediatrics in San Francisco, she planned to remain in the Bay Area to work in medically underserved areas of Richmond and Oakland. However, she was unhappy practicing medicine under the managed-care system, where she felt like a factory worker on a human conveyor belt, with fifteen minutes to “fix” each child. Seeking a more effective way to use her training, she moved back east and entered the EIS program.
Fine loved New York City and loved working with Layton. Moreover, she soon began dating another doctor, a dermatologist raised in New Jersey, who admired and supported her decision to continue working in public health. But there was only one job open at Communicable Diseases when her EIS training ended, and Fine was not sure she wanted it. The Department of Health was looking for a person to serve as liaison to the Office of Emergency Management (OEM), which was developing a city-wide bioterrorism response plan and organizing emergency response exercises.
When Fine completed her EIS training—three years before the terrorist attacks of September 11, 2001—New York was already deeply engaged in terrorism preparedness activities. The 1993 World Trade Center bombing confirmed NYC’s attractiveness as a target of terrorism, and the 1995 nerve gas attack on the Tokyo subway underscored its vulnerability as a big city. The Port Authority of New York and New Jersey took steps to increase security procedures at the World Trade Center, and Mayor Rudolph Giuliani, who took office in 1994, made terrorism preparedness a priority. In 1996, Giuliani initiated plans to build the ill-fated Emergency Command Center and bunker at 7 World Trade Center, across the street from the twin towers. He also shifted responsibility for emergency preparedness from the NYC police department to the newly established OEM, whose first leader was Jerry Hauer, a former emergency management administrator for the State of Indiana. A high-powered man with a forceful personality, Hauer was more successful at competing for resources with New York’s Finest than any of the OEM directors who have so far succeeded him.
Although Fine was not happy about switching from disease investigations to bioterrorism preparedness, she didn’t want to leave her professional connections or life in New York City. However, despite its crazy hours, the liaison job proved unexpectedly absorbing and interesting. Fine worked with police, firefighters, and hazmat personnel on planning drills that simulated such scenarios as plague attacks, truck bombs, and hoaxes. She also made presentations to community and professional groups. In August 1999, her main focus was a huge, million-dollar, live-action drill called “CitySafe,” scheduled to take place in a quiet Bronx neighborhood in September, with volunteers acting as victims stricken by airborne anthrax spores. The drill was a major production—federally-funded, the first of its kind—with high-level participation from the U.S. Army. It was even rumored that President Clinton might attend.
CitySafe was only two weeks away when Layton asked Fine to accompany her to Flushing Hospital.
The Field Investigation
On Saturday morning, August 28, Fine and Layton drove to Flushing Hospital in northern Queens. As Layton got out of the passenger side of the car, near the curb, she stepped over a large, dead black bird—an image that would recur in the days ahead. They went straight to the intensive-care unit, where the chief resident awaited them, standing in for Asnis, who was out of town taking care of a family emergency. He described the encephalitis cases, reviewing each medical chart in detail.
It was immediately evident how unusual and how similar the cases were. The patients were all older people, all previously healthy and active. Although encephalitis is often accompanied by inflammation of the meninges, the membranes that surround the brain and spinal cord, these patients did not exhibit typical meningitis symptoms such as severe headache and a stiff neck. The patients experienced fever, stomach pains, nausea, and diarrhea, followed by mental confusion, muscle weakness, and breathing difficulties, necessitating ventilatory support. One patient came to the emergency room thinking he was having a heart attack because of the breathing difficulties and pain. In each instance the illness developed slowly, over several days to a week. In contrast, the symptoms of botulism poisoning usually occur within eighteen to thirty-six hours of eating a contaminated food.
The laboratory clues were also remarkably consistent. In each case, analysis of the cerebrospinal fluid indicated the presence of white blood cells and a higher-than-normal level of protein—two signs of infection. Under the microscope, the white blood cells were identified as primary lymphocytes, which is a sign of viral rather than bacterial infection.
Once the chart review was complete, Layton and Fine interviewed the patients’ families. Strangely enough, not long after they began, a shouting elderly patient was wheeled in on a stretcher, angry and combative. He, too, had fever and encephalitis: a possible fifth case of the mysterious disease.
Layton and Fine were unable to talk directly with the patients at Flushing Hospital, because three were on ventilators and the newly admitted patient was delirious. Fortunately, the team was able to rely instead on information from each patient’s worried family visitors. Eager for any type of lead, Fine and Layton began by asking what the patients had been doing the week before they fell ill, hoping to find an activity they might have in common. Did they attend parties, visit relatives, attend church, go shopping, go to a movie, or go to a restaurant? What did they eat and what medications did they take? What were their hobbies? It quickly emerged that the patients and their families were not acquainted with each other. The only common factor was that they all lived within a densely populated area of about four square miles in Queens.
As they spoke with the patients’ families, Layton and Fine were struck once again by similarities among the four cases. The patients were elderly, but not at all debilitated. They were active people who spent considerable time outdoors. One was tanned from long hours of gardening in his backyard. Another took long walks every day. A third had been exiled to the porch by her son, who didn’t want her to smoke indoors. The fourth patient liked to sit in his front yard, watching and kibitzing as a swimming pool was built next door.
Afterwards, Layton—a considerate boss—asked Fine to drop her off at the New York Hospital Medical Center of Queens and go home to Brooklyn while Layton visited the last patient. It was now late in the day, visiting hours were over, and the New York Hospital Medical Center was fairly empty. This patient, like the others, was on a ventilator and unable to speak. Layton quickly reviewed his chart, which told a similar story, with a similar progression of symptoms and laboratory findings from the analysis of the cerebrospinal fluid.
Troubled, but hopeful, Layton walked to the Flushing subway station. Passing the Queens Botanical Garden, she walked in on impulse to collect her thoughts. It was not yet dark, and the minaret of a mosque was visible above the trees. She sat on a bench in the Rose Garden and took stock of what she needed to do next. Suddenly hungry, having missed both lunch and dinner, she entered the first eating place she passed after leaving the Garden, a Vietnamese restaurant, and tried something new: Vietnamese iced coffee, served hot but poured over ice, strong and sweetened with condensed milk.
Layton returned to her office and called Fine at home to tell her about the patient at the New York Hospital Medical Center. Layton and Fine were now more certain that something strange was going on, and that there was no time to lose in figuring out what it might be. They would contact the CDC in the morning and also check in with other NYC hospitals to find out if there were any similar cases. By mid-morning Monday, Layton’s staff had identified four more cases of encephalitis with muscle weakness—in Queens and the South Bronx—bringing the total to nine.
Taking Stock
Fine and Layton reviewed local data to determine whether the encephalitis cases were as unusual, statistically speaking, as they seemed to be. One hundred to 120 sporadic cases of viral meningitis are reported in NYC each year, with the number of cases increasing in July as the temperature rises, and then going back down. However, the small number of reported NYC cases of viral encephalitis without meningitis—only seven or eight per year—makes it difficult to draw conclusions about seasonality, although an upswing in August did not seem atypical. (Reporting of both diseases depends on voluntary reporting by healthcare providers, and both diseases are generally believed to be underreported.)
Next, Fine and Layton reviewed medical textbooks for information about the symptoms, signs, and differential diagnoses of viral encephalitis. They confirmed that flaccid paralysis is not a common manifestation of most types of viral encephalitis and that the diverse (and ubiquitous) members of the Enterovirus genus are the most common viral cause of encephalitis. However, all of the Queens patients were elderly, and enteroviral infection occurs mostly in babies and children, possibly because older people acquire immunity to enteroviruses through years of mild infections. (In contrast, “hot babies” seen in emergency rooms in July and August often have enteroviral infections.) Moreover, enteroviruses typically cause meningoencephalitis (combined encephalitis and meningitis), rather than encephalitis alone. Nevertheless, it was possible that the Flushing cases involved an uncommon enterovirus with unusual clinical manifestations.
Layton and Fine were aware of other, more exotic causes of viral encephalitis reported overseas, such as Nipah virus (a paramyxovirus related to measles and mumps), which had been identified the previous spring in Malaysia and Singapore. Moreover, the leading cause of viral encephalitis in Asia—the mosquito-borne Japanese encephalitis virus—had spread into Australia less than a year before. Japanese encephalitis is one of several encephalitic viruses that are zoonotic (transmitted from animals to humans) and arboviral (transmitted by arthropods, such as mosquitoes and ticks). Like enteroviruses, arboviruses most often cause meningoencephalitis rather than encephalitis alone. Although arboviral diseases have not been a problem in New York since the yellow fever outbreaks of the 1800s, Layton and Fine knew that unusual illnesses from other parts of the world sometimes turn up in New York City.
Later that day, Fine’s fiancé found a tiny paragraph in Harrison’s Principles of Internal Medicine on a mosquito-borne viral disease called St. Louis encephalitis (SLE), which occurs most often in elderly people and can cause muscle weakness and mental confusion. Looking back, Fine says, “David was the first to get it wrong.”
St. Louis encephalitis in Queens? The idea seemed very far-fetched. SLE had never been reported in New York City and is so rare upstate that it was not on the list of diseases monitored by the New York State Arthropod-Borne Disease Program.1 The virus that causes SLE is a member of the Flavivirus genus (family Flaviviridae) carried by birds; its overseas “cousins” include the Japanese, Kunjin, Powassan, and West Nile encephalitis viruses, as well as two hemorrhagic fever viruses known worldwide: dengue and yellow fever. About thirty sporadic cases of SLE are reported in the United States each year, with occasional outbreaks in hot, wet places like the Mississippi Valley and the Gulf Coast.
Nevertheless, Layton and Fine agreed that a mosquito-borne disease would be consistent with the patients’ histories of outdoor activities. Coincidentally it had also been good weather for mosquitoes, with a mild winter, wet spring, and unbearably hot, dry July (the hottest on record). In fact there had been two unusual incidents of mosquito-borne malaria, one involving two eleven-year-olds at a Boy Scout camp in Long Island. Moreover, the last time NYC had experienced similar weather conditions, during the summer of 1993, Layton’s office had investigated three cases of malaria in adults in Queens. However, there were no surveillance data to confirm an upswing in the local mosquito population, because NYC’s pest control program had been sharply reduced in the early 1990s. Although some funding was restored in 1997, it was mostly allotted to rat control.
Consultation
Layton called the CDC’s twenty-four-hour emergency hotline number on Sunday morning. Not certain which division to contact—since the causative agent of the encephalitis cases was unknown—she asked to speak to Ali Khan, a CDC colleague she had worked with in the past. But the CDC operator did not put her through to Khan, who was currently in charge of bioterrorism surveillance. Instead, she was connected with an expert on arboviruses and then (on a second try) with an expert on enteroviruses. Neither one was interested, because the Flushing cases did not fit the expected profile for either arboviral or enteroviral infection. Still worried, Layton sent an e-mail to Khan, and copied the others. Khan responded by arranging a Monday morning conference call that included scientists with expertise on enteroviruses, arboviruses, bioterror agents, and “special pathogens” (a catch-all category covering rare and unknown microbes).
On the phone that morning, the CDC experts dismissed the idea of a mosquito-borne outbreak in New York City. They recommended that a neurologist review the cases, ignoring the fact that a neurologist had examined Asnis’ patients before she called Layton. They asked Layton to send blood and cerebrospinal fluid samples to the CDC, as well as to New York State.
A second call did not go well either, although Khan offered to send an EIS officer from the CDC’s Bioterrorism Surveillance Branch to assist in the investigation. By this time, Layton’s staff had turned up several additional suspected cases—the first trickle of what would soon become a flood—by phoning specialty departments at each city hospital (adult and pediatric emergency medicine, intensive care, infectious disease, neurology, and infection control practitioners) and by issuing a “broadcast fax” (a useful mechanism in the days before e-mail came into common use) to physicians and nurses throughout the city. After the phone call ended, Layton and Fine heard their CDC colleagues talking on the still-open line: It’s not an outbreak. . . . There would be meningitis as well as encephalitis. . . . There have been no outbreaks of arboviral diseases in New York City for more than a hundred years.…
Still mystified, and wanting to assess the possibility of a mosquito-borne disease, Layton asked Veruni Kulasekara, a medical entomologist at the American Museum of Natural History, to help evaluate the mosquito situation in Queens. Kulasekara, a chic Sri Lankan married to an American rock star (the base guitarist of the Violent Femmes), had met with Layton earlier that summer to discuss the potential risk of local malaria transmission, given the hot, wet weather. Accompanied by an EIS officer and a public health veterinarian, Kulasekara set off Tuesday morning to examine the homes of Asnis’ patients (as well as other newly identified patients with unexplained encephalitis) for mosquito breeding sites. The patients lived in the adjacent neighborhoods of College Point and Whitestone, on the northern coast of Queens. College Point is located just above Flushing (the site of Shea and Arthur Ashe stadiums), close to LaGuardia Airport, and separated from the South Bronx by a narrow stretch of the East River; Whitestone is just west of College Point. Both neighborhoods contain block after block of modest-but-comfy one- and two-family homes with front lawns and small backyards, bordered by concrete sidewalks with openings for maple trees and flower beds.
That evening, Layton went to Fine’s apartment in Park Slope, Brooklyn, to await the return of the EIS officer on Kulasekara’s team, a chronic disease specialist named Denis Nash who was filling in for a colleague from the Bureau of Communicable Diseases. (New to NYC, Nash had never been to Queens and knew little about mosquitoes.2 However, his EIS training had taught him how to follow the disease trail wherever it might lead.) While they waited, they ordered in Thai food and discussed the invitation list for Fine’s upcoming wedding in Brooklyn’s Prospect Park.
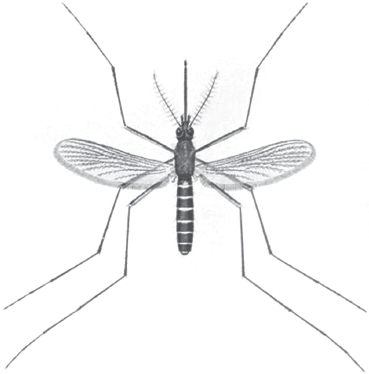
Arriving just in time for a late-evening dinner, Nash reported that the NYC investigators had no difficulty finding mosquito breeding sites in the College Point area. There were piles of tires with water in the doughnut holes, and backyard swimming pools with just enough stagnant water to create attractive habitats for mosquitoes. They found an open plastic barrel in the backyard of the sickest patient—the avid gardener whom Layton and Fine had visited at Flushing Hospital—who had been collecting rainwater to use on his plants. In a scoop of rain-barrel water Kulasekara showed them mosquito larvae of the Culex genus, a type of mosquito that can transmit arboviruses such as SLE virus. One member of this genus—Culex pipiens, the northern, or common, house mosquito—is frequently seen in urban areas.
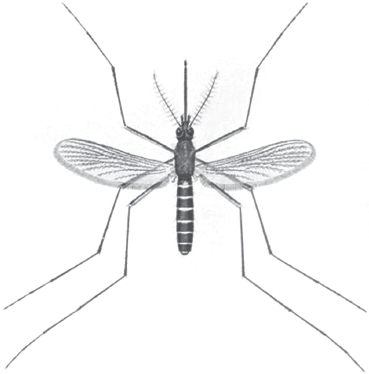
Culex pipiens. Source: CDC Public Health Image Library.
After discussing Nash’s conclusion—that a mosquito-borne disease was a distinct possibility—they turned to the practical problem: how to triage and investigate the growing number of suspected cases, which rose to more than sixty by week’s end. Lacking a diagnosis, they would have to rely on “syndromic surveillance,”3 which is case-finding based on a characteristic group of signs and symptoms rather than on laboratory testing. They devised a case definition on the basis of four clinical criteria: fever, altered mental status, muscle weakness, and laboratory test results consistent with a viral cause. A patient whose illness fit all four criteria was designated as a definite case; a patient who fit three, as a probable case; two, as a possible case; and one, as an unlikely case.
At the office the next day, Layton assigned several field investigators—including Denis Nash (borrowed from the Bureau of HIV/AIDS); the EIS officer assigned to Communicable Diseases; and a third EIS officer sent, as promised, by Khan—to interview the families of patients with definite and probable cases, review medical records, assess clinical findings, and collect demographic data (age, sex, and occupation). They also collected blood and cerebrospinal fluid samples that were packaged by the NYC health laboratory and sent to the CDC and to the NYS encephalitis laboratory. The EIS officer from the CDC took charge of the paper-based line listing of suspected cases and transferred it into an Excel spreadsheet, along with the demographic, clinical, and laboratory clues.
There was more bad news as the week went on. The avid gardener died on Tuesday evening, and the woman who smoked on her porch died a few days later. Fine called Hauer to give him a heads-up that a deadly encephalitis agent might be carried by mosquitoes. If so, it could be a serious problem for CitySafe—the big, live-action bioterrorism preparedness drill—which was supposed to take place outdoors.
The Diagnosis
On Thursday, two days before Labor Day weekend, preliminary test results arrived from the New York State virology laboratory. To their amazement, blood samples from two patients tested positive for SLE—just as Fine’s fiancé had suggested! Was this really true? The state laboratory had used an indirect test called the immunofluorescent antibody (IFA) assay, which detects antibodies to particular viruses or bacteria. Although IFA can give false positives (when antibodies specific for one microbe cross-react with antibodies specific for another), all of the clues (medical, entomologic, and laboratory) fit together fairly well: encephalitis in older adults with muscle weakness (a rare SLE symptom, but mentioned in Harrison’s); Culex mosquitoes; and an IFA positive for SLE. It was certainly possible that a NYC mosquito had taken a blood meal from an SLE-infected bird that migrated in from a southern state. But it was still very odd to have an SLE outbreak in NYC, where there had never been a case before—especially when no cases of SLE had been reported elsewhere in the country.
There is no drug treatment for SLE, so medical care is supportive, aimed at mitigating the most serious symptoms (brain inflammation and breathing difficulties) until the patient recovers on his or her own. From a public health perspective, the main response is mosquito control—not a small or inexpensive undertaking, especially with no pre-existing program in place. Because this diagnosis was so surprising and unexpected, the NYC health department decided to wait for confirmation from the CDC, promised for the next day, before taking action. Duane Gubler, head of the CDC Fort Collins laboratory, was using a different blood test, the virus-specific, enzyme-linked immunoabsorbant assay (ELISA), which gives fewer false positives than IFA. The ELISA test panel would include North American arboviruses from three viral genera: Alphavirus (eastern, western, and Venezuelan equine encephalitis viruses), Orthobunyavirus (La Crosse and California encephalitis viruses), and Flavivirus (Murray Valley and Rocio viruses, as well as SLE). All of these viruses are endemic to the United States, but most are uncommon in the northeast.
Sick with suspense, Fine waited for the official diagnosis from the CDC. When the call came confirming SLE, Fine raced down the hall, feeling like Paul Revere rousing the troops: It’s positive! It’s positive! Now that they knew what was going on they could do something about it. Layton spoke with Hauer, who put the resources of the OEM and Emergency Command Center at the health department’s disposal. A few days later, Hauer canceled CitySafe.
The Public Health Response
The diagnosis came on the Friday before Labor Day weekend, a time for traditional outdoor activities such as backyard barbeques, block parties, and concerts in city parks. Mayor Giuliani quickly held a press conference to get the word out about the outbreak and the measures the city was taking to rid the city of mosquitoes. Fine rode in the health department’s official black sedan with psychiatrist Neal Cohen, the NYC Health Commissioner, to meet Giuliani and Hauer in College Point.
It was an uncomfortable ride. The commissioner was nervous, and the driver was unsure of the directions. Fine was on the car phone with Layton, who was back in her office, talking on two lines at once, participating in a conference call with the CDC, whose experts were recommending a pesticide called malathion. Fine was concerned about the decision. She had been in California in 1994 when malathion was sprayed on medfly-infested orchards, causing environmental damage. She relayed the CDC’s advice to the commissioner, explaining about the pesticide issues in California in case there were questions from reporters.
In College Point, while they waited for Giuliani to arrive, a neighborhood resident came up to Fine and asked her a strange question: Had she heard about the dead birds in Queens? Lots of crows and robins? Did she think there was a connection between the dead birds and the sick people? Fine said she didn’t know anything about the birds. SLE is carried by birds, which seemed like an obvious connection, but Fine was pretty sure that SLE doesn’t kill birds, which are its natural host and reservoir.
Fine briefed Mayor Giuliani, who relayed the public health information to the reporters and the crowd of local residents. He described the three confirmed cases of SLE, expressed sadness at the death of the gardener, and asked everyone to cooperate in the city’s effort to “wipe out the mosquito population.” Flanked by Hauer and Cohen, he announced that several neighborhoods in northern Queens and nearby areas of the South Bronx would be sprayed in the evening and around dawn, when Culex pipiens mosquitoes are most active. He suggested that city residents, especially the elderly, stay indoors or wear pants and long sleeves when going out. He demonstrated the use of insect repellent—splashing it on his face and arms—and asked that people rid their yards of standing water from pools, tires, or other containers surfaces.
Later, Fine returned to the office where she and Layton and their colleagues planned out what they would need to do in the coming week and how to make the best use of OEM resources. Their immediate concern was to send the latest set of patient specimens to Fort Collins without delay. Because FedEx would not deliver on the holiday weekend, OEM chartered a plane to deliver the specimens to a private home in Fort Collins, where the father-in-law of a CDC scientist would be waiting to sign for them.
Fine spent the rest of the day at a newly activated OEM hotline at the Emergency Command Center at 7 World Trade Center, which had opened the previous June. The Command Center was a modern, high-tech facility with corporate décor—a far cry from the shabby, institutional-yellow offices of the NYC health department. Fine sat in a comfortable, ergonomically correct office chair and answered call after call from local doctors and worried parents. The call she remembers best was from a woman in Queens who asked her the same question as the woman at the press conference: What was going on with the birds? The woman quoted from a neighborhood paper that described “droves of crows falling from the sky” in Queens and Nassau County, Long Island, in the Bronx and even further north, up into Westchester. Was there a connection with the mystery disease in College Point? Fine said she didn’t know, but she would find out.
That task, however, would have to wait until tomorrow; it had been a very long day. When Layton and Fine returned home to Park Slope, by subway, very late, Layton dropped Fine off on her stoop and hugged her good-bye.
The Birds
Fine called Roger Nasci, a CDC vector-borne disease expert, the day after the press conference to follow up about the birds. What did he think was going on? It seemed unlikely that the bird and human outbreaks were simply a coincidence, but there were a few things that did not fit. First, SLE virus is carried by birds, but it doesn’t make them ill. Second, the birds were dying over a fairly large area—Queens, the Bronx, and Long Island—but human encephalitis cases had been reported only in Queens.
Nasci is a mild-mannered, unpretentious scientist, described by one of his colleagues as salt of the earth. He was not disparaging or dismissive when he reiterated that SLE would not sicken the birds that are its natural reservoir. But he admitted that he had no idea what type of illness was killing the birds. He said he was coming to Queens to measure the density and distribution of Culex pipiens and any other mosquito species that might be transmitting SLE. He would also help New York City use surveillance data to determine whether the malathion spraying was effective. When he later arrived at LaGuardia Airport, a police escort was waiting for him, courtesy of OEM, with lights flashing and sirens blaring.
Fine also called the New York State Arthropod-Borne Disease Program to ask whether its staff would test a dead crow dropped off at an OEM mobile command unit in Queens. They referred her to Ward Stone at the Wildlife Pathology Unit at the state’s Department of Environmental Conservation in Albany. A wildlife enthusiast with a mad-scientist swirl of white hair, Stone’s duties included performing necropsies (animal autopsies) and sending tissues to veterinary laboratories for testing. For the NYC health department, he mostly conducted toxicology tests on dead pigeons possibly poisoned in city parks.
Stone accepted the NYC shipment but did not mention that he had already received lots of dead birds—four hundred or more through the month of August—and was sufficiently alarmed to alert his counterparts in New Jersey and Connecticut. The dead birds came from zoo officials in Queens and the Bronx, as well as from private citizens, including a highway cleaning crew in Long Island. Tracey McNamara, the head pathologist at the Bronx Zoo—a research veterinarian with an intense and animated way of speaking—had called him several times. Two weeks earlier, on August 19, Stone told her he had identified several different causes of illness but “no common thread”4 that would explain why the birds were dying.
Tracey McNamara had much reason for concern. On Wednesday, August 25—three days before Layton and Fine began their investigation in Flushing—an owl and an eagle living in an outdoor cage at the Bronx Zoo had died of unknown causes. More zoo birds died over Labor Day weekend after exhibiting strange behaviors, such as a wobbly gait, tremors, and abnormal head postures. The dead birds included Chilean flamingoes, a ring-necked pheasant, and a Guanay cormorant that swam in circles for several hours before it died. McNamara was especially worried because one of her assistants stuck himself with a syringe needle while trying to medicate a jerking flamingo.
By the time Fine contacted Stone, McNamara had already ruled out two major killers of U.S. poultry (Newcastle disease and avian influenza) on the basis of routine blood tests. She had dissected several birds and found signs of encephalitis (i.e., bleeding from the brain) and damage to the heart muscle. This led her to consider eastern equine encephalitis, a mosquito-borne encephalitis virus. However, equine encephalitis is highly dangerous to emus (a large, flightless bird, related to the ostrich), and the Bronx Zoo emus were fine. Besides, encephalitis suggested a connection to the human cases in Queens. McNamara called the CDC on the Thursday after Labor Day, described the necropsy data, and asked for help in taking care of her assistant.
The head of the CDC epidemiology unit in Fort Collins asked her to send a serum sample from the employee and a plasma sample from the sick flamingo to help evaluate the assistant’s risk of contracting disease. (Fortunately, the employee did not develop any symptoms.) However, he was not used to working with zoo officials and (like his colleagues) did not take her concerns about the human-bird connection seriously. He told her the same thing Nasci told Fine: bird die-offs have many possible causes, and the two outbreaks were probably a coincidence. He went on to say that his laboratory was extremely busy with the human SLE cases in New York City and did not have time or resources to investigate illness in birds. He referred her to the National Veterinary Services Laboratory (NVSL) in Ames, Iowa, which is the major U.S. Department of Agriculture laboratory concerned with farm animals. This was the same laboratory recommended to Ward Stone by the veterinary laboratory at Cornell University, a back-up facility to the New York State virology laboratory, which (like the CDC) does not have diagnostic reagents or responsibility for testing diseases in birds and animals.
As time went on and more zoo birds died (including ducks, laughing gulls, and magpies), McNamara—unable to interest the CDC, despite calling every day for a week—set in motion an extensive veterinary investigation that expanded to include another state laboratory (the Connecticut Agricultural Experiment Station), the federal agricultural laboratory (NVSL), and two federal laboratories concerned with wildlife and bioterror agents. The wildlife laboratory was the National Wildlife Health Center (NWHC) in Madison, Wisconsin, which is operated by the U.S. Geological Survey, Department of the Interior, and the bioterrorism laboratory was part of the U.S. Armed Forces Institute for Infectious Diseases (USAMRIID) in Fort Detrick, Maryland. Although USAMRIID generally does not take requests from civilians, a USAMRIID veterinary pathologist eventually agreed to accept Bronx Zoo bird specimens as a special favor to McNamara.
Layton and Fine would not hear about these activities for another two weeks, by which time the veterinary investigation had circled back to Fort Collins. By Thursday, September 23, three of the veterinary laboratories—NVSL, NWHC, and the Connecticut Agricultural Experiment Station—had isolated viruses they could not identify and had called the CDC for help.
The Mosquitoes
Rising to its first major challenge involving a public health emergency, the NYC Office of Emergency Management had a mosquito-control program underway within twenty-four hours. This was a significant achievement because OEM had to start from scratch, without city pest-control experts or mosquito surveillance data to guide its actions. After consulting with specialists from Suffolk County, Long Island, and the CDC, OEM purchased huge amounts of malathion and borrowed a Suffolk County airplane to survey Queens for potential mosquito breeding sites. Helicopters were rented, loaded, and readied for immediate use. OEM advised NYC residents to stay indoors with windows closed and air conditioners turned off for two hours after spraying.
Mosquito-control measures were front-page news in all local papers. The health department tripled its staff at the hotline at 7 World Trade Center and provided health department personnel with their first cell phones. Throughout Labor Day weekend, the health department and OEM sent mobile command units to talk with people in affected neighborhoods; distribute insect repellent at police and fire stations; and disseminate press releases, fact sheets, and flyers. Because the risk to any given person was small, no events—except CitySafe—were canceled. Nevertheless, health officials urged residents of Queens (especially the elderly) to avoid outdoor celebrations and encouraged people attending Central Park concerts, the U.S. Open at Arthur Ashe Stadium, or baseball games at Shea Stadium to wear skin-covering clothes and use insect repellent (some provided courtesy of the Mets).
Lacking historical data on mosquito habitats—and with new surveillance efforts just underway—the health department and OEM used the locations of confirmed human SLE cases to decide where spraying would do the most good. They anxiously awaited each set of diagnostic reports from the arbovirus laboratory at the CDC, which was providing results on individual patients using the ELISA. (This was a departure from the CDC laboratory’s usual role as a public health reference facility, but the NYS virology laboratory did not have experience with the ELISA test for SLE.) Each afternoon, Layton, Fine, Hauer, and health department colleagues squeezed into a third floor conference room with an open speakerphone to hear John Roehrig—their main CDC contact—read off daily case results, one by one. (Roehrig, who had not worked with the NYC health department before, at first confused Fine’s and Layton’s voices on the phone and referred to them as “the sisters.” In person, he would have seen that Layton and Fine are dissimilar in look and manner, though both are petite brunettes. Layton is wavy-haired, quietly observant, and diplomatic in her persistence, while Fine is curly-haired, outgoing, and direct.)
Everyone’s ears pricked up when Roehrig announced a positive case in Sunset Park, Brooklyn—the first case outside of Queens and the South Bronx. Cell phones flicked open all over the room, and people began to get up and leave. Layton, sitting at the head of the table, was soon the only one left. “Got to call you back,“ she said and hurried to her tiny office, where she found Hauer and Cohen and some of their staff crammed into the space around her desk, staring at her paper wall-map with its color-coded push pins. The Brooklyn case was twelve miles away from the cluster of cases in Queens and the Bronx, which might mean that the outbreak was spreading.
Layton sent an EIS officer to interview the Brooklyn patient, a Central Asian immigrant who spoke Russian and Farsi. As luck would have it, the EIS officer assigned to Communicable Diseases was an Iranian-American who spoke fluent Farsi and had no trouble conversing with the patient and his family. He confirmed that the patient had not left Brooklyn for weeks, which meant that he had been infected in Brooklyn and not in Queens or the Bronx.
On the following day, September 9, a third patient at Flushing Hospital died from viral encephalitis. Cohen informed Layton that Giuliani was holding a second press conference to announce that spraying would be expanded to cover Brooklyn and Manhattan. The commissioner wanted her to attend and bring her famous wall-map.
It was a rainy, cold day, and Layton’s EIS officer wrapped the fraying wall-map—pushpins and all—in plastic. She stood by Cohen’s side as he showed Giuliani the map and the updated list of definite, probable, and possible cases. “These numbers don’t add up,” Giuliani barked. The EIS officer was shocked, unsure what he meant. Layton then sat down beside Giuliani and reviewed the numbers, case by case. The mayor backed down and apologized. After that, the reputation of the health department rose at City Hall, because the mayor reportedly told his staff that the health department was OK: “Their numbers always add up.”
Over the next ten days, cases of unexplained encephalitis were confirmed throughout the city, and pesticide was sprayed in all five boroughs. In Manhattan, where skyscrapers interfered with the aerial approach, ground-spraying trucks were used in place of helicopters.
An Unresolved Issue
The next several weeks were a blur of activity at the NYC Bureau of Communicable Diseases. Layton’s staff continued to conduct active case-finding, investigate suspected cases, and track laboratory results, which was a bookkeeping nightmare because the CDC and the NYC health department used different sets of identifying numbers. They also continued to prepare daily case updates for Giuliani, checking each patient, each day, by phone, to get a status report. If they learned that a patient had died, they arranged for autopsy tissue samples to be sent to the NYS and CDC laboratories. Later on, they conducted retrospective surveillance to determine whether the outbreak had been underway before Asnis noticed the cluster of cases in Flushing. Retrospective surveillance involved tracking hospital discharge diagnosis codes for paralysis, encephalitis, and neurologic conditions. Just one retrospective case was found: in a woman hospitalized in Queens during the first week in August.
Layton’s staff also continued to assist the mayor’s office with press releases and TV appearances. During the run-up to another press conference, Fine—in full last-minute wedding-planning mode—squeezed in a thirty-minute fitting for her vintage wedding gown. Layton accompanied her so they could continue refining the mayor’s talking points. The people in the dress shop were fascinated by the conversation and by Fine’s noisy work paraphernalia—three beepers and a cell phone—which she peeled off her belt before trying on the dress.
Meanwhile, Layton and Fine were also grappling with an unresolved issue—in addition to the mystery of the birds—related to the laboratory testing of the suspected SLE cases. It seemed fairly easy to spot a highly probable case of SLE, because the constellation of symptoms characteristic of the initial patients (fever, mental confusion, muscle weakness) was quite distinctive. (A case was only classified as “definite” after it was laboratory-confirmed.) Nevertheless, many probable cases came back as “indeterminate” or even “negative.” Something did not seem right. As Roehrig rattled off one day’s results, Fine wondered if there could be something wrong with the test. Roehrig, though also puzzled, treated it as a joke: “Would you quit saying that!!”
As it turned out, public health experts at the NYS virology laboratory were also unhappy with the SLE results. On Monday, September 13, Fine was invited to participate in the first day of a teleconference on encephalitis cases of unknown origin, associated with the CDC Unexplained Deaths Project. In view of recent events, the participants—from state laboratories in California, Minnesota, New York, and Tennessee—were eager to hear about the SLE cases in New York City. The New York State contingent told Fine they had been unable to confirm their SLE-positive IFA results using the polymerase chain reaction (PCR) technique. This didn’t make sense because PCR is more direct and specific than an antibody-based blood test, involving amplification of a tiny piece of viral genetic material (a gene fragment) characteristic of a given virus or virus strain. As far as they knew, CDC had not confirmed the IFA and ELISA results either. In fact, CDC had not reported any SLE-positive results obtained with PCR, viral isolation studies, or the plaque-reduction neutralization assay, a quantitative test that measures the ability of the antibodies in a patient’s serum to decrease viral activity. (Although plaque-reduction is also a “serologic” test, based on detection of antibodies, is less prone than IFA and ELISA to false positives caused by cross-reactions with antibodies from other flaviviruses.) It was also surprising that SLE virus had not been isolated from autopsy samples, though this might be because the level of virus in SLE-infected human brains is usually very low. (Eventually, the CDC did try to confirm the ELISA results with plaque-reduction assays, but the results were negative for SLE.)
On the last day of the teleconference (not attended by Fine or Layton), the New York State scientists decided to send autopsy tissues to W. Ian Lipkin, a molecular biologist at the University of California at Irvine. For the encephalitis workgroup, involving Lipkin would solve two problems at the same time. It would be a good test of the PCR-based methods Lipkin was developing for identifying encephalitis viruses, and it might shed light on the reasons for the discrepancies in SLE testing.
The Veterinary Investigation
Layton and Fine still had no information on what was killing the birds. The bird illness did not seem like a major issue at the time, because they accepted what the experts told them—that SLE did not kill birds and that the avian and human illnesses were unrelated. They waited to hear more and meanwhile encouraged further testing of dead birds that came to the attention of the health department. On Friday, September 10, Fine asked a vertebrate ecologist at the CDC for his take on the situation. (She had learned nothing further from Ward Stone, although by this time, urged on by McNamara, he had sent Bronx Zoo and Department of Environmental Conservation bird samples to the federal agricultural and wildlife laboratories [NVSL and NWHC]). The ecologist still thought the bird and human outbreaks were a coincidence, but he decided to visit Queens himself to get a look firsthand. He was planning to take blood samples from live birds, rather than dead ones, in an effort to identify host species carrying SLE, as well as figure out the cause of the mysterious avian illness. He did not see how SLE could be making the birds sick.
Before his bird survey was well under way, however, a major clue emerged from another source: the Connecticut Agricultural Experiment Station, which had revived its mosquito-control program in 1996 to cope with an outbreak of eastern equine encephalitis. Theodore Andreadis, an entomologist at the Station, had found a dead crow near a puddle full of mosquitoes on a golf course in Greenwich. When he necropsied the bird he found clear evidence of encephalitis. (Like Layton and Fine, he was unaware of similar findings by McNamara in zoo birds.) He was now trying to isolate a virus from the crow’s brain and also from the mosquitoes.
As it happened, Andreadis was not the only one trying to isolate a virus from a bird that had died from encephalitis. By mid-September, scientists from both NVSL and NWHC, unable to detect a known animal pathogen in Stone’s and McNamara’s bird specimens, had begun their own viral isolation studies. They injected bird tissues into embryonated chicken eggs and looked for viruses in the eggs’ allantoic fluid. Under the electron microscope, both laboratories saw the same thing, a virus of the same genus as SLE: a flavivirus. Andreadis’ laboratory also isolated flaviviruses from the golf-course crow and from the near by mosquitoes. All three laboratories contacted Duane Gubler in Fort Collins.
Andreadis and the NWHC scientists wondered if this might be a new, bird-killing variant of SLE, or perhaps an entirely new virus never seen before. The NVSL scientists made an additional suggestion: Could it be a human pathogen not previously known to infect birds? (The opposite situation, where a known animal pathogen is found to cause illness in humans, is not uncommon. Examples include monkeypox, Rift Valley Fever, and avian influenza A[H5N1]viruses.) The upshot was that NVSL sent its flavivirus—isolated from the brain of a Bronx Zoo flamingo—to the CDC.
By this time, having spoken multiple times with McNamara, Andreadis, and colleagues at NVSL, NWHC, and USAMRIID (who had also isolated a non-SLE flavivirus)—and having viewed the plaque-reduction results—Gubler was convinced that the initial diagnosis of SLE had been premature. The disease agent was certainly a flavivirus but which flavivirus was unclear.
Gubler is a friendly, outgoing man—a genial combination of down-home, small-town American and world-renowned public health authority. Raised in a tiny Utah town, he married a local girl who expected to be a rancher’s wife but ended up a world traveler when her husband developed an interest in tropical diseases. They had lived in Hawaii, India, Indonesia, and Puerto Rico, where Gubler investigated mosquito-borne diseases such as filariasis and dengue hemorrhagic fever. For the past ten past years, he had headed the CDC Fort Collins laboratory, which studies diseases carried by insects and animals and provides outbreak assistance to state and local health departments throughout the United States.
Since Labor Day, Gubler had followed the standard Fort Collins investigative protocol for arboviral outbreaks, deploying a field entomologist to collect mosquito specimens and a vertebrate ecologist to identify host animals (in this case, birds) for further testing. Now, as he waited for the NVSL virus to arrive, he and Roehrig began re-testing the human blood samples from New York City, using an expanded ELISA panel that included Old World flaviviruses from Africa (e.g., West Nile virus), Asia (Japanese and Powassan viruses), and Australia (Kunjin virus). As they talked over the new developments, they agreed that brushing off McNamara had been a major mistake.
Resolution
Everything came together quickly after that. On Thursday, September 23, Gubler called Layton to let her know that the CDC would announce new findings during a conference call the next morning. Layton and Fine assumed that meant a new diagnosis—probably a different flavivirus—and they speculated about what it could be. The unusual hush-hush quality of Gubler’s message inspired wild thoughts to go through their minds, including the possibility of bioterrorism.
Layton spent all night working in her office and flew to Maryland early the next morning to fulfill a prior engagement as a panelist on a USAMRIID videoconference on the public health response to bioterrorism. It was uncomfortable to answer questions about the NYC outbreak when she didn’t know what the punch line was going to be. Afterwards, a fellow panelist—C.J. Peters of the CDC Special Pathogens Laboratory—speculated that the virus might be a close relative of SLE, such as West Nile virus (WNV) or Kunjin virus.
After her panel ended, Layton found a small private office in the studio and dialed into the CDC conference call—as did Fine and the rest of the team in NYC—and heard McNamara’s story for the first time. They were both fascinated and a bit surprised to learn about the veterinary investigations that had taken place without their knowledge. McNamara described the bird deaths at the Bronx Zoo, her necropsy data, and her repeated efforts to get federal authorities to take notice. She made an especially interesting observation that explained how a virus whose natural host is birds could kill so many of them. The birds that died belonged to New World species like the Chilean flamingo and the Guanay cormorant. If the mysterious flavivirus were an Old World pathogen, unknown in the Americas, local birds would have no natural immunity to it. In that case, the introduction of an alien virus into the local bird population would be the veterinary equivalent of the catastrophic introduction of smallpox into Native American villages in the 16th century. Not so surprising, then, that wobbly, disoriented birds would “fall out of the sky in droves.”
Gubler spoke next. He said that the CDC had confirmed the detection of West Nile virus in birds and suspected that the same pathogen—West Nile virus or a “West-Nile-like” virus—might be causing the human outbreak as well. But they would not be sure until his laboratory had re-tested blood and cerebrospinal fluid samples from several of NYC’s highly probable but SLE-negative or indeterminate cases, using the expanded ELISA panel.
Gubler said that his laboratory was also comparing a large (1278 base-pair) viral gene fragment amplified from NYC birds, mosquitoes, and human autopsy samples, to further confirm that the NYC-area bird and human outbreaks were due to the same arbovirus. As Layton learned later, Gubler’s laboratory had already begun sequencing the complete eleven thousand base-pair genome of the flamingo virus isolated by NVSL, starting with the gene for a structural (“envelope” or “coat”) protein called the E-glycoprotein. Meanwhile, he had sent a one hundred base-pair E-glycoprotein gene sequence to two flaviviral experts—J. S. MacKenzie at the University of Queensland, Australia, and Vincent Deubel at the Pasteur Institute in Paris—who would soon confirm that it was an almost perfect match to the equivalent sequence from a West Nile virus strain isolated from an Israeli goose in 1998. The goose sequence had not yet been published, possibly because a scientist had taken the goose from Israel to France illegally (i.e., without declaring it to customs officials). The E-glycoprotein sequence from the NYC flamingo isolate was also a close match to viruses isolated from humans and mosquitoes during a Romanian WNV outbreak in 1996.
Gubler concluded the phone conference by explaining that the CDC planned to announce the findings in birds on Saturday, but wait until Sunday to announce the new human diagnosis, to have sufficient time to generate new ELISA test results on hundreds of suspected human cases.
At last! Layton’s and Fine’s remaining questions were answered. The outbreak of human illness was caused not by SLE virus but by West Nile virus, which explained the bird deaths and resolved the discrepancies between the clinical data and the laboratory findings. The exotic West Nile virus had multiplied in crows and other susceptible birds, and the mosquitoes that fed on the blood of infected birds had passed the virus on to humans.
Layton and Fine were relieved to realize that NYC officials and health-care workers were already doing what was necessary to treat patients and prevent disease spread. WNV is an Old World cousin to SLE—found in Africa, the Middle East, India, France, and the northern Mediterranean area—that usually causes milder symptoms in humans and has a slightly lower fatality rate (3–10 percent instead of 3–15 percent). Supportive care for WNV encephalitis and SLE is the same. Moreover, WNV is transmitted by the same Culex mosquitoes that transmit SLE (night-biters that breed in polluted water) but is also thought to be carried by Aedes vexans mosquitoes (day-time-biters that breed in rivers). Efforts to decrease the numbers of NYC mosquitoes that could carry SLE virus or WNV were already well under way (and by late September, temperatures were beginning to fall, along with mosquito counts).
However, the day’s surprises were not yet over. Arriving back in New York, Layton received a confusing call from Lipkin, the scientist at the University of California, Irvine—whom she had not met or heard of before—who invited her to join him in a press conference about the new diagnosis. He spoke very fast and she had difficulty following him, but she thought he said that the cause of the human outbreak was a mixture of West Nile and Kunjin viruses, and that the viruses could have been intentionally released. She was not sure she understood him correctly.
She phoned her office, the NYS health department, and then the CDC. Her NYS colleagues explained about sending Lipkin the autopsy tissues for PCR testing. While the veterinary laboratories had focused on the bird samples, Lipkin had studied the ones from humans. He had isolated RNA from frozen brain tissues and devised a PCR technique, as Gubler had done, to amplify a gene fragment that varies in a characteristic way among different flaviviruses. He then compared the amplified sequences to sequences in GenBank—the National Institutes of Health databank that contains all publicly available DNA and RNA sequences—and found two near-matches: West Nile virus and Kunjin virus, a closely related virus endemic to Australia. He was hoping to announce his results as soon as possible. (Lipkin didn’t know about the unpublished sequence from the Israeli goose virus, which was the reason that Gubler and his colleagues were able to classify the NYC virus as West Nile.)
Layton declined to participate in Lipkin’s press conference. Although she did not care whether Lipkin or Gubler received credit, she wanted to make sure New Yorkers received the same information about WNV from New York City, New York State, and the CDC.
That night, she was awakened at 1 AM by an official from the health department press office who called to tell her that a New York Times reporter had requested confirmation of a statement from Lipkin that would run in the morning paper. Layton phoned Gubler in Fort Collins, where it was 11 PM, to give him a heads-up. The next morning, Lipkin’s account of a mixture of two viruses appeared in the early edition of The New York Times, and a new version ran in the afternoon edition with a different headline and quotes from both Lipkin and Gubler.5
An official NYC-NYS-CDC press conference took place on Sunday morning, as scheduled, with several big guns in attendance, including Mayor Giuliani, Commissioner Cohen, and NYS Health Commissioner Antonia Novello. Layton and Fine were on hand to answer questions. They had spent all day discussing McNamara’s data and reviewing the CDC’s figures for the new case count, which had more than doubled as old cases (from NYC and Nassau and Westchester counties) were re-classified as positive. The day before, with the human-bird connection confirmed, Layton had called an emergency meeting of the entire Communicable Diseases Program staff (except for Fine, who was ironing out the final details for her fast-approaching wedding). They needed to set up a surveillance system for dead birds. Before, they had used the location of human cases (a “human surveillance system”) to decide where to target mosquito-control efforts. Now they would use dead crows (a “dead bird surveillance system”) to identify neighborhoods where humans were most at risk. Dead bird jokes were the order of the day.
The Aftermath
Two weeks later, Fine and her fiancé were married outdoors, as planned, at dusk, in Prospect Park. The days had begun to get colder, and there were fewer mosquitoes, though the day itself was unseasonably warm. They were reassured by the CDC’s estimate (incorrect, according to a later study)6 that only one out of one thousand mosquitoes carried West Nile virus. They joked about supplying the guests with “goody bags” containing insect repellent.
As it turned out, they need not have worried, because the outbreak was already over, with no new cases of human illness identified after the third week in September. The final tally was sixty-two people with laboratory-confirmed West Nile disease, out of a total of 710 suspected cases in New York City and 229 suspected cases outside of New York City. Thus, only about 6 percent of the suspected cases turned out to be caused by West Nile virus. Of the sixty-two persons with confirmed cases, all but three were hospitalized. Forty-five hospitalized patients lived in New York City, with thirty-two in Queens, nine in the Bronx, one in Manhattan, and three in Brooklyn. One of the Queens patients was a tourist from Canada who visited Queens in early September and fell ill during the flight home. Fourteen more confirmed cases were hospitalized in the NYC suburbs, with eight in Westchester and six in Nassau County. Seven people died, including five in NYC, one in Westchester, and one in Nassau.
Over the winter, the NYC health department continued to monitor the after-effects of the outbreak and prepare for what might happen the following year. A human serosurvey in northern Queens conducted in association with the CDC indicated that about 2.6 percent (or between 1.2 and 4.1 percent) of the 46,220 people in the surveyed area had antibodies in their blood indicative of past infection with WNV. This meant that between five hundred and two thousand people in the surveyed area (corresponding to about nine thousand in the whole NYC outbreak area) had been exposed to the virus through mosquito bites, and that the sixty-two confirmed cases represented only the “tip of the iceberg,” the most severe manifestations of disease. Many of the people who gave blood for the survey reported more concern about the possible ill effects of pesticide-spraying than about the possibility of infection with WNV—an attitude that mystified Hauer and Giuliani.7 In fact, malathion killed off many insects besides mosquitoes, including butterflies, moths, and bees needed to pollinate trees and plants, and possibly also sea life. A class-action suit claiming that pesticides washed into Long Island Sound by Hurricane Floyd had caused a mass die-off of lobsters was not settled until April 2008. The timing of the die-off (September–October 1999) was suggestive, but the scientific evidence was inconclusive.
The NYC findings were roughly consistent with findings from previous studies in other countries suggesting that one in five people infected with WNV develops a mild illness with fever and headache (called “West Nile fever”), while about one in 150 infected people (usually the elderly) develop the symptoms seen by Asnis in Queens: encephalitis, muscle weakness, and mental confusion (“West Nile severe disease” or “West Nile neuroinvasive disease”). However, the sixty-two cases in NYC were unexpectedly severe. Fifty-nine of the sixty-two patients had West Nile neuroinvasive disease, and many of those who recovered were ill for as long as two months. Moreover, many remained weak or had difficulty concentrating after eighteen months.
What would happen next year? Once a zoonotic or arboviral pathogen enters the local insect and wildlife populations, it can be nearly impossible to stop. Although mosquitoes stop flying with the first autumn frost, they can survive freezing weather through a form of insect hibernation called “overwintering,” in which they cling to protective surfaces such as the underside of ledges and pipes. PCR-testing of thousands of hibernating Culex mosquitoes in New York City detected only one WNV-positive mosquito, but left open the possibility that a hibernating WNV-positive mosquito might awaken in the spring and lay WNV-infected eggs. Intensive mosquito surveillance and control efforts after winter’s end and during the following spring probably contributed to the smaller number of severe human cases (eighteen) in New York City in 2000, most of which were in the borough of Staten Island.
However, WNV quickly spread far beyond the New York area, apparently carried by birds (in addition to mosquitoes), who spread the virus along the Atlantic flyway and inland westward year by year, reaching all the West Coast states by 2003. WNV also spread south to Latin America and north to Canada, becoming endemic throughout the Western Hemisphere. Today, it is a leading cause of epidemic encephalitis in North America, and mosquito control has been re-instituted or enhanced in many localities.
In January 2000, the CDC Fort Collins laboratory issued public health guidelines for surveillance, prevention, and control of WNV infections and established a National West Nile Virus Surveillance System—now a component of ArboNET8—that monitors WNV in humans, birds, mosquitoes, horses, and sentinel chicken flocks. (Chickens are easily infected but do not fall ill, while horses can be severely affected. An outbreak that affected about twenty-five horses on Long Island in August and September 1999 was also traced back to infection with West Nile virus.) Screening for West Nile was instituted at blood banks and transplant centers after WNV was detected in donated blood and in transplanted organs.9 Human cases of WNV infection in the United States rose to a peak in 2003, when 9,862 severe cases were reported; the numbers fell to 2,500 to 4,200 per year until 2012, when the United States experienced a major outbreak affecting thirty-eight states, with three-fourths of the cases reported in Texas, Mississippi, Louisiana, South Dakota, and Oklahoma.10
So where did WNV come from and how did it end up in New York City? Perhaps the most likely explanation is that it arrived by plane at La Guardia Airport (about four miles from College Point) or JFK Airport (fewer than ten miles away). WNV could have traveled inside a mosquito that “hitch-hiked” on a flight from a place where the virus circulates in the local bird population, such as southern France, India, or Israel. (In 2001, Asian tiger mosquitoes—the vector of dengue hemorrhagic fever—arrived in California in the cargo hold of an airplane, inside shipping boxes containing a Chinese plant called “lucky bamboo.”) Or, the virus could have traveled inside an exotic bird that was smuggled into the city, avoiding both quarantine and inspection. Another possibility is that WNV arrived inside a human traveler.
The theory that the virus came by plane—inside a bird, mosquito, or person—from an area in which it is endemic is bolstered by the close match between the 1999 NYC strain of WNV and the strain isolated from the Israeli goose in 1998 (when there were no human cases in Israel) and between the NYC virus and human WNV isolates obtained during an Israeli outbreak in 2000. However, it is also possible that WNV was carried into Queens by a migrating bird. A map of migratory routes of common New World birds suggests that New York serves as an avian as well as a human travel hub, crossed by bird routes that go north into Canada and south into Mexico and many parts of South America. Although most birds migrate north and south (rather than east and west across the Atlantic), it is possible that WNV could have entered a different part of the Americas by plane, boat, or bird at some unknown time in the past, traveled to Queens by bird, and only revealed itself when favorable circumstances—a weather-induced increase in mosquitoes in a densely populated urban area—led to a small outbreak. In fact, the NYC outbreak was so small that it might have gone undetected if an astute physician in Queens had not put two and two together and called her local health department. So it is certainly possible that other small undetected human WNV outbreaks had previously occurred in other places. Arguing against this theory is the absence of reports of unexplained bird die-offs during the 1990s that would likely have occurred around the same time as a human outbreak (the basis of the “dead bird surveillance system”).11
One more theory—that the WNV was released into New York by terrorists—has been raised and discredited several times. Early on, Layton and Fine explained to the local FBI agent in NYC that the presence of mosquito vectors and the distribution of cases were consistent with a natural SLE outbreak. Moreover, SLE, with its generally mild symptoms and low fatality rate, seems a poor choice for a bioweapon. However, the idea was raised again by Richard Preston, the author of The Hot Zone (a best seller about Ebola hemorrhagic fever), after the diagnosis changed from SLE to West Nile fever. Writing in the October 18 issue of the New Yorker, Preston drew attention to a book excerpted in a London tabloid in April 1999 in which the author—who claimed to be a former bodyguard and body-double for Saddam Hussein—asserted that a highly virulent strain of WNV was part of Saddam’s bioterrorism arsenal. Despite the strange timing, with the book appearing about six months before the NYC outbreak, neither intelligence officials nor arms inspectors turned up any public evidence that Iraq had tried to weaponize WNV.
The possibility of bioterrorism was re-visited three years later, in fall 2002, during the run-up to the U.S. invasion of Iraq. (By this time, Layton had developed a close working relationship with a local FBI agent, due to 9/11 and the anthrax incidents.) An article in Business Week reported that in 1985, when the U.S. and Iraq were allied against Iran, the CDC had shipped samples of West Nile virus to medical researchers at the University of Basra. However, when biologists at the CDC compared the sequence of the strain sent to Iraq in 1985 to the 1999 NYC strain, they were relieved to find that the two strains were not alike.
Lessons Learned
A major lesson of the 1999 WNV outbreak is that sometimes epidemiologists need to ignore the old medical adage: When you hear hoofbeats, think horses, not zebras. SLE was an unusual diagnosis for New York City, and West Nile encephalitis was stranger still. Although exotic pathogens have traveled throughout history, attacking nonimmune populations and spreading havoc in their wake, microbial travel is easier and faster today because of air travel, urbanization, and increased human contact with animals and insects that live in rain forests and other wilderness areas. Also, we now have the molecular tools to confirm that something is new or rare.
Fine says that another lesson—or maybe the same lesson put another way—is that sometimes it’s good for an epidemiologist to be somewhat naïve, so that he or she is not blinded by traditional ways of thinking about a particular disease (e.g., that avian encephalitis viruses don’t kill birds, that West Nile virus only causes mild illness, or that it is not worth including exotic viruses in a test panel). Perhaps it’s a good thing that most epidemiologists are generalists who investigate many different types of infectious outbreaks and may not be as aware of (or invested in) current dogma as a specialist might be.
Layton and Fine agree that the biggest take-home lesson of the 1999 WNV outbreak is the need for public health and animal health officials to work together and share information on a regular basis. Due to the lack of communication, Layton and Fine conducted a complex outbreak investigation, potentially affecting millions of New Yorkers, while remaining unaware of important clues developed by veterinary colleagues. In retrospect, the delay did not have major consequences in New York City, because the diagnosis of SLE set in motion mosquito control measures that were also effective against WNV and because clinical care for SLE and West Nile encephalitis is the same. Moreover, it is likely that the SLE testing discrepancies would have eventually led to a reconsideration of the diagnosis (e.g., via Lipkin’s work) even in the absence of the veterinary investigation. As Stephen Ostroff, a high-level CDC official, explained to a New York Times reporter, confusion is a completely normal part of a public health investigation, which can take many twists and turns before everything becomes clear.12
Nevertheless, the delay in making a connection between the bird deaths and cases of human disease did delay recognition that human cases were occurring beyond New York City. Areas outside of the city that experienced significant bird die-offs—including Westchester County, Nassau and Suffolk counties in Long Island, and parts of Connecticut and New Jersey—did not institute mosquito control efforts until the end of September or early October. Two of those areas had confirmed human cases (nine in Westchester and six in Nassau).
As many public health experts have noted,13 the great majority of emerging diseases discovered in recent years have been caused by zoonotic pathogens (like severe acute respiratory syndrome [SARS]) or by human pathogens that arose from animal reservoirs (like HIV/AIDS). It is therefore imperative that public health authorities keep abreast of outbreaks and health issues not only in humans but also in livestock, wildlife, zoo animals, and pets.14 Fortunately, this lesson has been taken to heart by public health and veterinary professionals who advocate an integrated approach to the protection of human and animal health.4 Today, the NYC health department has a public health veterinarian who is charged with outreach to the animal health community, and federal, state, and local public health laboratories are officially linked with high-level agricultural, wildlife, and military reference laboratories through the Laboratory Response Network (LRN), which was founded by the CDC in partnership with the Association of Public Health Laboratories and the FBI. Conceived in 1998 as part of the national bioterrorism preparedness effort, the LRN has proved to be just as important, if not more so, in responding to naturally occurring outbreaks as to human-made ones, just as OEM proved invaluable to the West Nile response, although the impetus for developing OEM was bioterrorism.
This is not surprising, because all outbreak investigations require the same epidemiologic and laboratory skills—and control efforts require the same logistic and financial resources—whether the cause of the outbreak is a well-known virus, a new or drug-resistant bacterium, or a weaponized pathogen. But bioterrorism looms large in the public imagination, and fear of bioterrorism is a greater spur to public health investment than the fear of a naturally occurring illness, such as an exotic arboviral disease that has found an ecologic niche in the Western Hemisphere. From a public policy point of view, therefore, the West Nile outbreak illustrates that investments in bioterrorism preparedness can be especially valuable if states and cities are allowed to use them flexibly to address whatever public health crisis may arise.