Cannabinoids and the Respiratory System
Introduction
Marijuana use is steadily on the rise in the United States for both medical and recreational indications. This has been largely driven by increasing legalization and direct to consumer mass marketing. According to recent survey data, there is not only increased prevalence of marijuana use – up to 13% – but also decreased concern that marijuana use poses any threat for health risks or negative impact [1, 2].
Current data on the respiratory impact of marijuana inhalation is incomplete. However, the pulmonary manifestations of disease related to cannabis use are of utmost importance since inhalation is the most popular form of use. This chapter seeks to discuss known literature and clinical experience.
Lung Cancer
An area of concern and active investigation is the potential carcinogenicity of inhaled marijuana. The risk of inhaled cigarette smoke and the development of pulmonary malignancy have been well established [3]. This is also something that is well understood by the general public and well advertised on product packaging and additional avenues such as online and television public service announcement style advertising.
There are currently a limited amount of published data evaluating cannabis use and development of pulmonary malignancy. Retrospective databases have been evaluated. According to database review in the United States, Canada, the United Kingdom, and New Zealand, there is a suggestion for increased risk of adenocarcinoma with increased daily use of inhaled marijuana. However, there was no distinct risk with increased number of years. The authors note that the confidence intervals on the accumulated data were very wide due to small sample sizes of the retrospective cohorts [4].
Additional data point to an increased risk of development of pulmonary malignancy with increased frequency and intensity of inhaled marijuana use. Among a cohort of men from North Africa, an odds ratio of 2.4 was found after correcting for multiple variables including tobacco smoke. Of note, in this study all cannabis users were also tobacco smokers. The study suggested that lung cancer risk increased with increasing joint-years. A “joint-year” is quantified by the number of marijuana products (joints, bowls, bongs, etc.) smoked per day for the course of a year. However, the authors note that the residual effects of tobacco smoking remain a significant confounding factor [5].
Other studies appear to come down more firmly on the risk that marijuana smoke poses for malignancy. One retrospective cohort in New Zealand demonstrated an 8% increase in lung cancer risk for each joint-year of cannabis smoking even after adjusting for cigarette smoking. These data are especially compelling as all 79 individuals with lung cancer in the cohort were under the age of 55, which represents a demographic characterized by a low prevalence of primary pulmonary malignancy [6].
Another retrospective case control study containing over 300 subjects found a significant link between current lung cancer and past cannabis smoking. The risk for development of pulmonary malignancy was significantly increased in the cohort of cigarette smokers with prior cannabis use than for cigarette smokers who had never smoked cannabis (OR 65.0 vs 15.3) [7].
A recent large meta-analysis that included over 20 studies and a total of over 13,000 individuals with cancer of any type demonstrated a significant association between cannabis smoke and development of both lung and testicular cancer. For testicular cancer, there was a notable relationship of risk for individuals who smoked cannabis for greater than 10 years [8].
There are striking case reports regarding chest malignancy in cannabis smokers. One such report is that of a 26-year-old man with extensive cannabis smoking history but negligible cigarette smoking history that was diagnosed with small cell lung cancer. This patient was aggressively treated but unfortunately ultimately succumbed to his disease [9].
In summary, the net effect of cannabis smoke on risk for chest malignancy remains incompletely understood due to limited prospective data as well as significant overlap of tobacco smoking among individuals who smoke marijuana [10]. However, multiple observational studies have demonstrated an elevated risk of cancer development as it relates to cannabis smoking. This area certainly requires ongoing investigation especially in light of those data, which do suggest a causative role of cannabis in the development of pulmonary malignancies.
Finally, healthcare professionals should educate their patients on the potential carcinogenic risk of cannabis smoke exposure.
Lung Function
Inhalation of combustible substances and small particles is known to have ramifications for pulmonary function. However, the effects of smoking cannabis on pulmonary function remain poorly understood.
Lung function is complex and dynamic. It is affected by the ability of air to flow unobstructed through the tracheobronchial tree in order to reach the distal alveolar sacs. From the alveolar space, gas must be able to diffuse efficiently into the capillary bed where oxygen is bound by hemoglobin within red blood cells and carbon dioxide is diffused from the blood back into the alveolar space in order that it might be exhaled into the environment. This process of ventilation is delicate and can be affected by many variables and disease states. Environmental exposures such as dust, smoke, and ozone – to name a few – play a vital role in disease within the lung.
Pulmonary function can be assessed by multiple dynamic tests such as spirometry, plethysmography, and diffusion limitation of carbon monoxide. These tests evaluate the different aspects of ventilation and oxygenation as described above and give the clinician a view into rapid cellular processes that would otherwise be indiscernible.
Early data on the effects of smoking marijuana point to an acute improvement of airflow through the tracheobronchial tree. Marijuana smoke with 1–2% THC results in an acute increase in airway conductance that remains present for as long as 60 min. Ingested THC of 10–20 mg has been shown to result in a similar acute increase in airway conductance that lasts for as long as 6 h. This is in contrast to the effects of inhaled tobacco smoke, which results in an acute decrease in airway conductance [11]. Of note, the concentration of THC in inhaled products has significantly increased with the evolution of the industry. In Colorado, THC content now routinely pushes 30% for smoked flower and in other types of inhalation such as butane hash oil (BHO) – discussed further later in the chapter – the THC content has been seen to surpass 60%. The pulmonary physiologic effects of high-dose THC are currently an area of much needed investigation [12, 13].
More recent data evaluating the effects of chronic inhaled marijuana use demonstrate similar findings. This data was contained in a large study using NHANES cohort data wherein individuals underwent a standardized questionnaire regarding cannabis and also underwent standardized spirometry. Marijuana use duration was measured in joint-years. In the 1–5 joint-year and 6–20 joint-year cohorts, a statistically significant increase in FVC was found. There appeared to be no significant influence on FEV1. In the 6–20 joint-year cohort, a decrease in FEV1/FVC ratio to less than 70% was detected; however this was felt to be more likely attributable to a rise in FVC than a decrease in FEV1. A finding in this study which deserves mentioning is that although there appeared to be no decrement in pulmonary physiologic indices, researchers found that “current marijuana smokers were more likely to be male, younger, of lower socioeconomic and education levels, to concurrently smoke tobacco, to have first tried marijuana at an earlier age, and have a history of a chronic respiratory illness” [14]. This at-risk nature of current marijuana smokers will be further discussed later in this chapter.
Multiple other studies have demonstrated similar pulmonary function testing results, which are notable for a persistently elevated FVC in cannabis smokers, which is not demonstrated in tobacco smokers [15, 16].
There are non-spirometric data suggesting that marijuana affects the pulmonary endothelium in ways similar to tobacco use. One study demonstrated a decrease in exhaled nitric oxide (eNO) in active or recent cannabis smokers. Spirometry was also performed in these individuals, but similar to other studies, these individuals were found to have an increase in FVC. This study was not powered to show a dose-response relationship. The authors of this study contend that given the vital role of NO in vascular and immune response pathways a better understanding of the clinical role of decreased NO would be beneficial [17].
Finally, a finding that deserves mentioning and will be further addressed in the next section: chronic cannabis smokers develop a heavier burden of pulmonary disease when compared to the general population. According to a large retrospective analysis of cannabis smokers, in spite of the early bronchodilation demonstrated on spirometry, there was a late development of chronic bronchitis symptoms. These symptoms were increased cough, wheeze, and sputum production, all of which are suggestive of obstructive lung disease [18].
COPD/Emphysema
Whether or not inhaled cannabis use results in chronic lung disease is incompletely understood. Many professional respiratory societies discourage smoking marijuana due to the sparse data on long-term outcomes, but very real concern that its use leads to development of worsening respiratory symptoms of cough, sputum production, and wheeze [19, 20].
One study noted that inhaled cannabis use resulted in a decreased FEV1/FVC ratio, but it had no direct effect on FEV1 – very similar to the data described above. However, this study did suggest hyperinflation as demonstrated by increases in both FVC and TLC with inhaled marijuana. In addition, standardized cross-sectional imaging was performed and demonstrated increased apical lucency in the lung fields of cannabis smokers. There was not a distinct association with inhaled cannabis use and presence of macroscopic emphysema. However, one cannabis only smoker with a greater than 400 joint-year smoking history did show evidence of macroscopic emphysema [21].
This finding was corroborated in a Dutch study of individuals under the age of 50 years who developed primary spontaneous pneumothorax. The 53 study subjects underwent high-resolution chest CT following treatment of their pneumothorax. Imaging findings were striking. Bullae were present in 87% of cannabis users, in contrast to 57% in tobacco-only smokers and none in nonsmokers [22]. There are also case reports of young individuals with minimal tobacco smoking histories that develop significant paraseptal emphysema. This is compelling because all of these individuals had significant cannabis smoking history. In addition, the demonstrated paraseptal pattern differs from the typical centrilobular pattern seen in individuals who develop pulmonary emphysema later in life as a result of chronic tobacco smoking [23].
Similar results were demonstrated in a Swiss study retrospectively evaluating spontaneous pneumothorax. The investigators observed a significant correlation between duration of cannabis smoking, development of emphysema and bullous disease, and incidence of spontaneous pneumothorax in young adults [24].
A key issue with inhaled cannabis and its currently poorly understood effects is the significant practice overlap of tobacco smoking with cannabis smoking. Recent data suggests that cannabis use is associated with tobacco smoking initiation, persistence, and relapse [25]. This is not only a confounding variable but also appears to have a synergistic effect in the development of chronic lung disease. A study in Canada evaluated the development of obstructive lung disease in individuals who smoked only cannabis, only tobacco, and those who smoked both cannabis and tobacco. Compared to never smokers, individuals who smoked tobacco cigarettes were more likely to have chronic lung disease and worse spirometric indices as well more symptoms of chronic respiratory disease such as cough, sputum production, wheezing, and dyspnea. In cannabis only smokers who had smoked at least 50 marijuana cigarettes, there was no significant risk for development of obstructive lung disease by pulmonary function testing or worsening respiratory symptoms. However, in those individuals who had smoked tobacco as well as cannabis, there was a significantly elevated risk of both outcomes. According to the authors, this suggests a synergistic effect between inhaled cannabis and tobacco smoke on the development of chronic lung disease [26].
Another study from the United Kingdom builds upon these data. This study also evaluated the development of COPD and chronic respiratory symptoms among tobacco and cannabis smokers. In the overlap group, when tobacco use was fully adjusted for, there remained a 0.3% increased prevalence in COPD attributable to cannabis smoke. In addition, COPD was found to be more prevalent at an earlier age among those who smoked both tobacco and cannabis. According to the study: “in the age range 25–34 years, 6% of tobacco-only users compared with 14% of tobacco and cannabis users met COPD criteria; in the 35–44 years age range, these proportions rose to 16% and 29%, respectively” [27].
A large retrospective review and meta-analysis of English language studies spanning from 1973 to 2018 concluded that there is insufficient evidence currently to establish a risk for COPD due to cannabis smoking alone. However, this analysis did demonstrate that there is at least low-strength evidence suggesting that individuals who smoke marijuana suffer more chronic pulmonary symptoms such as cough, wheezing, dyspnea, and sputum production [28].
This increased burden of respiratory symptoms due to cannabis smoke inhalation has been demonstrated in the primary care setting as well [29].
In summary, the data on cannabis smoking and chronic lung disease is inconclusive. Spirometric data is relatively sparse. However, from the data available, we can surmise that cannabis smoking, although not detrimental to spirometric indices, does appear to have a negative effect on the pulmonary system as represented by a higher burden of chronic respiratory symptoms of cough, wheeze, dyspnea, and sputum production. It is also evident that small particles result in the destruction of lung parenchyma as evidenced by findings of increased apical lucency, pulmonary bullae, and overt emphysema. This pattern is especially true in co-occurring tobacco and cannabis smokers.
Vaping
Electronic cigarettes came to market in 2007 and since then have continued to grow in popularity [30]. Vaping is the act of inhaling vapor produced by heating the oil within a cartridge or device of an electronic cigarette.
The pattern of use of cannabis from available literature and population data suggests that smoking is the most common means of ingestion followed by other forms such as edibles and vaporized products [31, 32].
Vaporized marijuana has gained in popularity due to the individual’s ability to inhale a deodorized product as well as the popular opinion that using vaporized marijuana gives a more intense psychoactive experience [33].
This anecdotal information of its intense psychoactive effects is supported by the data. A clinical trial in healthy adults who infrequently use cannabis demonstrated that vaporized cannabis resulted in higher serum concentrations of THC as well as more pronounced psychoactive effects [34].
However, there is still much to be learned about the vaporized products inhaled by means of e-cigarettes. Vaping has begun to represent an underappreciated public health risk. This is due at least in part to the minimal standardization and oversight present in the vaporized product market. The electronic cigarette market has dramatically expanded in recent years and is fast outpacing the ability of appropriate biomedical research to ensure safety.
The vaporized product market is very broad due to a wide-ranging variety of flavors. These flavors are produced by the addition of synthetic flavoring agents, namely, diacetyl. This is very notable given diacetyl’s known risk for causing bronchiolitis obliterans after a major outbreak of this disease among popcorn factory workers. This prompted development of the informal name “popcorn lung.” This resulted in the removal of diacetyl from the flavoring process of popcorn. Unfortunately, diacetyl is known to be present in the flavoring of vaporized compounds for direct inhalation. In a recent study, diacetyl was detected in 39 of 51 flavors studied that are popular among teens and adolescents [35]. The Food and Drug Administration has taken notice of the damaging effects of these “kid-friendly” flavors and has start limiting their availability [36].
Additionally, another recent study demonstrated that dangerous carbonyl compounds formaldehyde and acetaldehyde were present in large amounts in the thinning agents used in vapor oil [37]. These compounds are formed during the heating process of the oil much as would be seen when the oil is heated to vapor and inhaled.
Still other studies have demonstrated contamination by microbial toxins. One study demonstrated significant contamination of electronic cigarette products with endotoxin and 1,3 B-D glucan. Concentrations of these microbial toxins were above the limit of detection in 23% and 81%, respectively, in a cohort of e-cigarette oil products sold in the United States [38].
Trace metals evaluations of electronic cigarette aerosols have demonstrated the presence of nickel at a higher concentration than is seen in traditional smoking modalities [39].
It is perhaps due to these toxic substances that e-cigarette-related acute lung disease has become so prominently noticeable. One such incidence was in Wisconsin and Illinois when 14 teens and young adults were hospitalized for acute respiratory failure after vaping. Several of the teens and young adults required intubation and mechanical ventilation [40].
There are reports of similar patterns of disease outbreak resulting in hospitalization in New Jersey, Texas, Colorado, and North Carolina among young adults without any significant history of lung disease or other respiratory exposures [41–43]. Of most concern, at the time of this manuscript, 48 individuals have died as a result of e-cigarette/vaping product-associated lung injury (EVALI) [44]. In response to this outbreak, the Centers for Disease Control and Prevention (CDC) released this statement: “The CDC recommends that people should not use THC-containing e-cigarette, or vaping, products, particularly from informal sources like friends, family, or in-person or online dealers” [45]. According to the CDC, THC-containing vaping products are the most commonly used vaping product used by individuals suffering from EVALI [45].
While the etiology of acute lung disease in the affected individuals has not yet been fully elucidated, there are specific pathologies known to be associated with vaping-induced acute lung injury. A recent case was reported wherein surgical lung biopsy samples of individuals suffering from vaping-induced lung injury demonstrated respiratory bronchiolitis interstitial lung disease (RB-ILD) [46].
Additionally, there are reports of vaping-induced lung injury due to diffuse alveolar hemorrhage, acute eosinophilic pneumonitis, and lipoid pneumonia [46–49]. Vitamin E acetate has been proposed as an etiologic agent as it has been isolated from bronchoalveolar lavage from many individuals suffering from EVALI [50].
One study evaluated the effects of single episode vaping on individuals with severe chronic obstructive pulmonary disease (COPD). Inhaling 35 mg of vaporized THC had no significant spirometric or symptomatic effects on individuals with severe COPD [51].
A major public health concern in the consideration of electronic cigarettes is the large prevalence of teenage and young adult users. Market research supports the role of aggressive advertising campaigns on social media platforms as being highly effective at dramatically increasing the use and popularity of electronic cigarettes in recent years [52]. The extreme popularity of certain brands such as JUUL among youth suggests a correlation between effective marketing campaigns and adolescent susceptibility to such trends [53]. Additionally, there are strong data to support that the “low risk” of electronic cigarettes is attracting youth to tobacco smoking who otherwise would not consider cigarette smoking [54].
Whereas the risks of electronic cigarettes and cannabis smoking are still poorly understood, the risks of tobacco smoking are well known. Electronic cigarettes have been trumpeted as a means to tobacco cessation and an alternative to cigarette use. Unfortunately, preliminary studies of teenagers demonstrate that electronic cigarette use is a substantial risk factor for future cigarette smoking as well as experimenting with other illicit substances including alcohol, prescription narcotics, and hallucinogenic drugs [31, 55]. There is equally as compelling data in adults that the use of inhalational cannabis significantly increases likelihood for concomitant tobacco abuse [25].
Vaping cannabis by means of electronic cigarette poses a major only recently appreciated public health crisis. This is due to its prevalence among young adults, its underreported ramifications for respiratory health due to both psychoactive substance (cannabis or nicotine) and contaminant, and finally its known overlap with initiation and persistence of tobacco smoking. In spite of clever marketing schemes and positioning itself as a “safe alternative” to smoking combustible substances, vaping has been recurrently found to be unsafe and a poor choice for lung health. It is for this reason that the American Lung Association takes a strong stance against electronic cigarettes and states that it is “very concerned that we are at risk of losing another generation to tobacco-caused diseases as the result of e-cigarettes” [56].
Lung Health
The effects of cannabis smoke on respiratory airflow and lung cancer development remain incompletely understood. However, its effects on general lung health have been adequately demonstrated to be overall deleterious.
Individuals who smoke marijuana on a regular basis have been found to demonstrate a bronchitic phenotype with increased wheeze, cough, and sputum production [57]. As discussed above, this has not yet been associated with an increased incidence of obstructive lung disease. These findings of bronchitic phenotype have been reproduced in multiple studies [58].
Marijuana inhalation has been demonstrated to have a negative impact on mucociliary clearance and immune cell function. This results in decreased host defenses and increased propensity for infection and likely contributes to the chronic bronchitis frequently observed in individuals who chronically use marijuana [59, 60].
Not only does inhaled marijuana alter host respiratory defense but has also been demonstrated to increase infectious risk in community clusters due to microbial contamination. Case report evidence documents infectious outbreaks of Aspergillus spp. and Mycobacterium tuberculosis directly related to marijuana use [61–63].
Cannabis smoking has also been associated with acute lung diseases such as recurrent necrotizing bronchiolitis and hemoptysis [64, 65]. There is an increasing recognition of cannabis inhalation resulting in acute pleural disorders such as pneumothorax and pneumomediastinum. This is thought to be due to inhalational technique which often results in coughing against a closed glottis. In addition, there is an association with emesis, which is a known complication of marijuana use. Several studies evaluating etiology of spontaneous pneumothorax found a significant correlation between cannabis use in young adults, development of lung bullae, and subsequent development of spontaneous pneumothorax [22, 24, 66].
Alternate forms of cannabis inhalation have also been demonstrated to be damaging. Butane hash oil (BHO) refers to an extraction technique of concentrating THC to much higher levels through extraction with butane. In a process known colloquially as “dabbing,” this extraction is then inhaled after being superheated and vaporized. Studies evaluating lung availability of phytocannabinoids such as THC and CBD have demonstrated THC concentrations in excess of 60% in dabbing versus 19–27% in marijuana flower smoking [13]. This form of inhalational use has been associated with acute lung injury, which mimics pneumonia. The BHO process results in residual butane as well as terpenes. When terpenes are heated, they degrade into methacrolein and benzene. It is hypothesized that high levels of these substances result in the acute lung injury, which has been observed in the dabbing process [67].
There are additional concerns regarding cannabis product contamination. Studies evaluating cannabis purity have demonstrated shockingly high recovery of pesticide residue within the cannabis smoke, which would be inhaled by the user. Recovery of permethrin from glass pipe smoked cannabis was found to be approaching 70% [68]. In dab preparations, over 80% of tested samples were found to have significant residual pesticide and solvent contamination [69]. One study evaluated self-identified cannabis smokers for the increased presence of toxic combustion by-products. In this study, cannabis smokers were found to have significantly elevated urinary concentrations of polycyclic aromatic hydrocarbons (PAHs) and volatile organic compounds (VOCs) when compared to nonusing control subjects [70]. Finally, there are firsthand reports from cannabis workers of industrial cannabis growers using illegal pesticides such as Eagle 20, which has a residue that is known to break down into hydrogen cyanide when it is heated and smoked [71].
Environmental Considerations
The environmental impact of rapidly increasing volume cannabis growth and use must be considered in regard to its implications for lung health. One recent study created leaf enclosures to replicate on a smaller scale the growing conditions inside of cannabis cultivation facilities. Ambient measurements of biogenic volatile organic compounds (BVOCs) were obtained and were demonstrated to be elevated above baseline. The authors of the study hypothesize that if the results of their data are extrapolated to the large scale, then the production of BVOCs from cannabis cultivation could result in a doubling of atmospheric BVOCs in a large production city such as Denver, Colorado [72]. This data is very meaningful because BVOCs are precursors to ozone and particulate matter. Volatile organic compounds have been demonstrated to increase airway inflammation in mouse models and have also been demonstrated to have a significant negative impact on the spirometric indices of elderly individuals [73, 74].
Additionally, vaping products have been shown to have detrimental effects on local indoor air quality. Electronic cigarette use results in aerosolization and distribution of significant volumes of multiple polluting substances such as 1,2-propanediol, glycerine, nicotine (in the setting of nicotine electronic cigarette use), PM2.5, and carcinogenic PAH molecules [75, 76]. One quantitative study of air quality at an indoor vaping event demonstrated that the degree of air pollution and amount of particulate matter present were similar to that found in the setting of extreme air pollution such as wildfires or industrial pollution [77]. This level of air pollution is certainly detrimental to both the lung and general health of individuals and communities.
Cannabis has also been demonstrated to be a mild allergen, resulting in the development of allergic response both among users and secondhand exposed individuals. There are reports of children with uncontrolled asthma related to passive cannabis exposure. Disease was notably improved following removal of exposure [78]. There are case reports of lifelong nonusers who develop cannabis allergy due to secondhand exposure. Symptoms include rhinoconjunctivitis and ingestion-related allergies as evidence of cross-reactivity [79]. One report from a Colorado allergy practice found that up to 12% of individuals who have never smoked marijuana demonstrated evidence of cannabis allergy. This number increases to 26% for past smokers, and as much as 50% of current smokers that experience symptoms and demonstrate findings of cannabis allergy [80].
Secondhand cannabis smoke exposure is also an area of growing concern. Studies regarding secondhand smoke exposure in the home have demonstrated a significant trend toward increased respiratory morbidity for exposed children. These children were found to have a trend toward higher incidence of ear infection, asthma, bronchiolitis, and eczema and emergency department visit for cough or dyspnea [81]. Animal studies on brief passive smoke exposure have shown vascular endothelial dysfunction. The degree of dysfunction is similar to that caused by cigarette smoke [82]. Another study on nonsmoking individuals found that exposure in varying levels of room ventilation demonstrated inverse proportions of sedative effects, impaired cognitive performance, and detectable serum/urine THC concentration related to degree of ventilation (i.e., better ventilation results in lower adverse outcome detection) [83].
Air quality has become an area of increasing public interest due to its known impact on the health of communities. A recent report by the American Thoracic Society cited excess morbidity and mortality related to air quality. The American Thoracic Society has called for even more conservative reduction thresholds for ozone and particulate matter [84]. The respiratory impact of large-scale cannabis growth in communities, vaping, carcinogen and particulate matter production, as well as first- and secondhand cannabis allergy, and secondhand smoke exposure must be considered in discussions of lung health as it relates to air quality.
Conclusion
In summary, although cannabis has been propagated as safe for inhalation, it has been seen to have detrimental effects not only on individual lung health but also on community health given its impact on air quality. Cannabis smoke inhalation by any means puts its users at undue respiratory risk due to mitigation of respiratory immune defense, increase in respiratory secretions, and development of pulmonary syndromes such as bronchitis, COPD, emphysema, necrotizing bronchiolitis, pneumothorax, pneumomediastinum, fungal pneumonia, tuberculosis, and lung cancer. These illnesses are not due to cannabis alone but undoubtedly to the significant contaminant burden inhaled by its users. Enhanced awareness among the general public but also certainly among healthcare practitioners is absolutely necessary to decrease the unnecessary development of acute and chronic respiratory illnesses due to cannabis smoking. Healthcare providers should consider screening high-risk individuals for inhalational marijuana use and educating their patients on the above findings. Based on this body of evidence, patients should be counseled in accordance with the ALA position: “Due to the risks it poses to lung health, the American Lung Association strongly cautions the public against smoking marijuana” [85].
THC & CBD Decomposition and Terpene Hazards While Vaping or Dabbing
Introduction
In order to solve a complex problem, sometimes the cause(s) and solution(s) are more easily discovered when one begins with the fundamentals. In light of the current vaping epidemic, some of the possible answers to this crisis may be found by simply beginning the investigation at the atomic level of matter.
Basic Chemistry-Organic Molecules and Compounds
Organic molecules are the building blocks of life and center around chains of carbon atoms. There are four main groups of organic molecules that combine and form compounds necessary for life to exist, namely, carbohydrates, proteins, lipids (fats, oils, and waxes), and nucleic acids. In addition to living matter, organic molecules are also found in non-living matter. Fossil fuels, derived from crude oil, which are formed from the remains of once living organisms, are comprised of organic molecules too [86]. In general, organic chemicals always contain carbon atoms, most contain hydrogen atoms, and many also contain oxygen atoms [87].
Decomposition of Organic Chemicals, Specifically Lipids
Smoke point temperatures of various cooking oils [93]
Oil (lipid) | Temperature |
|---|---|
Extra virgin olive oil | 325–410°F (163–210°C) |
Vegetable shortening | 360–410°F (180–210°C) |
Margarine | 410–430°F (210–221°C) |
Refined avocado oil (one of the highest smoke points) | 520–570°F (271–299°C) |
Incandescence (Emission of Visible Light as a Result of a Body’s Temperature)
Visible color of steel when heated [95]
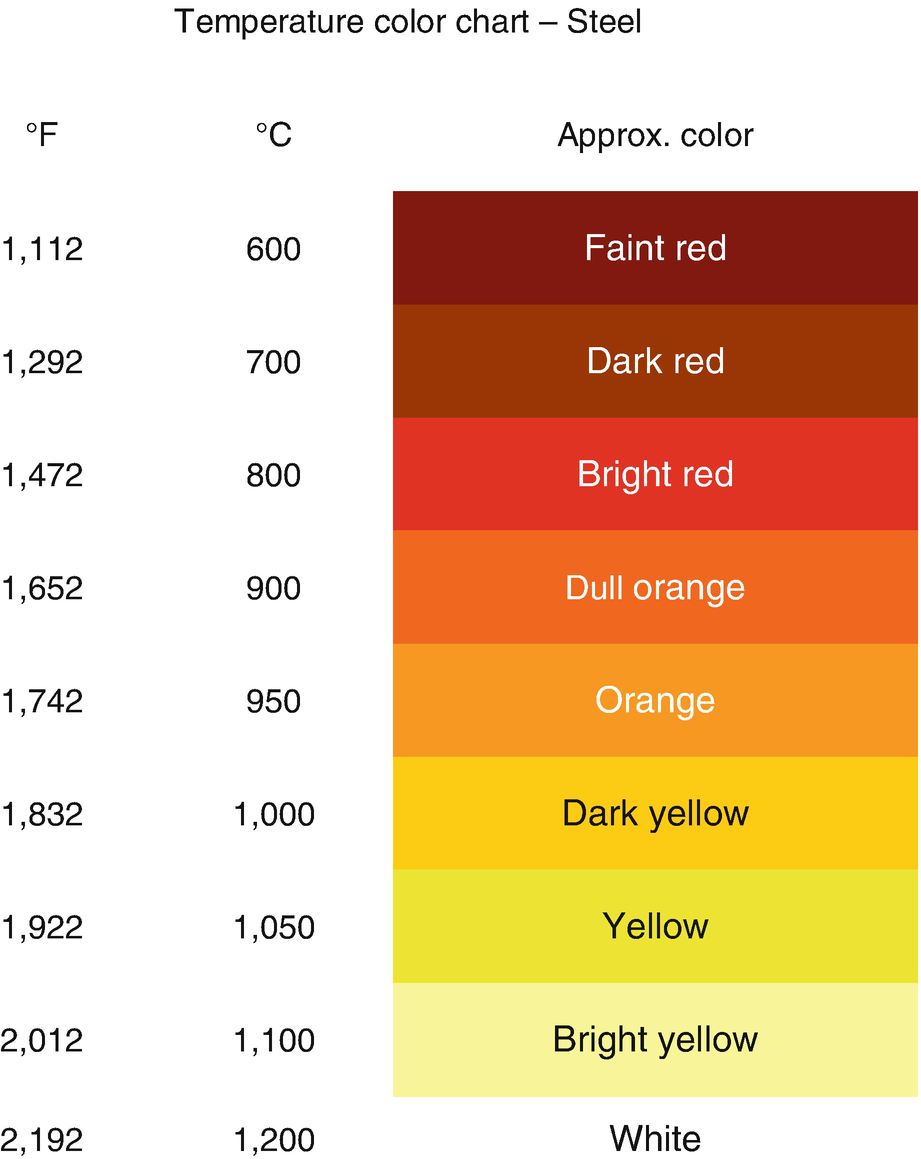
Nickel-chrome wire is widely used to manufacture the heating elements used in vape pens and e-cigarettes. It has a melting temperature of approximately 2,462°F (1,350°C) and a maximum operating temperature, when used as a heating element, of 1,652°F (900°C) [96]. For comparison purposes, steel has a melting temperature of approximately 2,500°F (1,370°C) [97]. In theory, regardless of the material, including ceramics and even titanium, any solid object will glow a similar color when heated to the respective temperature listed in Table 8.2.
THC and CBD
Delta 9-tetrahydrocannabinol or THC, the psychoactive component of the marijuana plant, is classified as a lipid and is therefore an organic chemical by definition. When extracted from the marijuana plant using a solvent such as butane (the resulting product is known as butane hash oil or BHO), ethanol (same as alcohol), or carbon dioxide (CO2), the resulting product can be a waxy substance or a thick oil [98, 99]. Further supporting the fact that THC is an organic chemical, it is comprised of 21 carbon atoms, 30 hydrogen atoms, and 2 oxygen atoms and can be denoted as C21H30O2 [100]. It should be further noted that cannabidiol (CBD) has the same chemical formula as THC because it is also comprised of 21 carbon atoms, 30 hydrogen atoms, and 2 oxygen atoms and can also be denoted as C21H30O2 [101]. Since THC and CBD have the same chemical formulas, namely, C21H30O2, they are known as isomers. This should not be surprising since both of these organic chemical compounds are extracted from the cannabis family of plants, namely, marijuana and hemp.
The previously mentioned solvent extraction process is also used to remove CBD from the hemp plant. The concern with this type of extraction process for both THC and CBD is the fact that the organic solvent used along with any residual insecticides, pesticides, and naturally occurring heavy metals can be concentrated in the resulting product. The heavy metals that can carry over to the resulting waxy or oil-like products is due to the fact that the cannabis plant is actually a “soil scrubber”; in fact, the cannabis plant is used in some areas in the world to clean up contaminated soil [102].
Cannabis plants also contain terpenes, which carry over with the THC and CBD extracts and give marijuana-based and hemp-based products their distinctive similar odors. Terpenes are also desirable additives because these compounds can either intensify or downplay the effects of both THC and CBD [103].
Vaping and Dabbing
There are two well-known methods to get THC quickly into the user’s bloodstream, namely, by either vaping or dabbing. A “dab” is the product resulting from the solvent extraction of the THC from the marijuana plant. The extracted product is highly concentrated and therefore has a much greater potency (80%+ THC). Vaping and dabbing both require the use of heat in the form of an electrically energized coil (for vaping) or a manually heated “nail” composed of either ceramic, titanium, quartz, or glass (for dabbing) [104]. Vaping devices use a battery to heat/energize a metal or ceramic coil. When dabbing, a nail is normally heated to a very high temperature with a commercially available propane torch or other similar heating device [99]. On a YouTube video discussing how to clean a vape pen, the color of the coil appears to be a yellow in color, indicating a temperature of approximately 1,922°F (1,050°C) [105]. Similarly, if dabbing, the glowing color of the nail indicates its approximate temperature.
As discussed previously, organic chemicals decompose into other compounds when they are exposed to an excessive amount of heat energy. Examples, previously discussed, were cooking oils heated to or above their “smoke point.” THC and CBD will both therefore similarly decompose at elevated temperatures since they are lipids too and will similarly decompose.
32–310°F (0–154°C) – This range is generally too low to vaporize any type of cannabis concentrate. This will result in zero clouds and thus no flavor.
315–450°F (157–232°C) – This is the range for your “low temp dabbing”. In this range terpene profiles efficiently vaporize without burning. You will experience the maximum flavor and taste exactly the way the extractor meant for the extract to taste.
450–600°F (232–315°C) – This is in range with a “medium temp dab” or a hybrid temperature. This range will deliver slightly lower flavor profiles while increasing cloud production.
600–900°F (315–482°C) – This is the “high temp dab” range. You will start seeing rapid combustion and thick clouds. You lose terpene flavors as they lose their molecular structure at such high heats.
900°F + (482°C+) – Anything above this temperature is generally frowned upon as certain carcinogens and toxins begin to release in vapor form. Hits will be cloudy, but extremely harsh with a distinct burnt taste.
It should be noted that at 900°F (482°C), this vendor clearly states that “certain carcinogens and toxins begin to release in a vapor form.” The vendor also states that at 600–900°F (315–482°C): “You will start seeing rapid combustion and thick clouds. You lose terpene flavors as they lose their molecular structure at such high heats.” Also note that the target temperature for vaping is within the range of the smoke point of most cooking oils, which makes sense because both vaping and dabbing rely on the inhalation of smoke to achieve the desired effect(s) by the user. It can be concluded that if cooking oils release harmful compounds at or above their smoke point, and, since THC and CBD are both considered lipids, they too would release similar biologically harmful compounds when heated to or above their respective smoke points.
1, Methacrolein (MC)
Methyl vinyl ketone
Hydroxyacetone
4,3-Methylfuran
5,2-Methylnaphthalene
1,3-Butadiene
Benzene
1-Methylcyclohexa-1
4-Diene
8, Benzene
The most concerning harmful chemical compounds identified were 1, methacrolein (MC), a noxious irritant and similar to acrolein; benzene, a known carcinogen; and 1,3-butadiene, another known carcinogen [108].
∗Note: The researchers should have also considered the impairment that occurs when dabbing THC. This is another factor that could make manual temperature regulation when dabbing very difficult. Drug-induced impairment could also affect how well the temperature control of a vape pen is managed by the user.The difficulty users find in controlling the nail temperature put users∗ at risk of exposing themselves to not only methacrolein but also benzene. Additionally, the heavy focus on terpenes as additives seen as of late in the cannabis industry is of great concern due to the oxidative liability (free-radical generation) of these compounds when heated.
Also, there is the distinct possibility of the generation of free radicals when dabbing and vaping THC or CBD, similar to what happens when overheating cooking oils, because both of these compounds have an O-H (oxygen-hydrogen) pair attached to its molecular structure, which can become a hydroxyl (O-H) radical or “free radical” upon decomposition. As discussed previously, free radicals are considered one of the causes of many diseases, such as atherosclerosis, cancer, and neurological disorders [109].
Terpene Hazards
The same researchers from the Portland State University Department of Chemistry listed the different terpenes that are associated with THC products and that are extracted from the marijuana plant or added to the product to augment the effects desired by user. They found that “myrcene was found to be the most abundant, followed by limonene, linalool, pinene, caryophyllene, and humulene; however, the plant can also contain up to 68 additional terpenic compounds in trace amounts.” Additionally, they stated that “some consumers increase the terpenoid content by dipping butane hash oil in a vial of terpenes prior to use (“terp dipping”)” [107].
- Myrcene [110]
- Hazard statements
Flammable liquid and vapor.
Causes skin irritation.
Causes serious eye irritation.
May cause respiratory irritation.
- Precautionary statements
Avoid breathing dust/fume/gas/mist/vapors/spray.
IF IN EYES: Rinse cautiously with water for several minutes. Remove contact lenses, if present and easy to do. Continue rinsing.
- Potential health effects
Inhalation may be harmful if inhaled. Causes respiratory tract irritation.
May be harmful if absorbed through skin. Causes skin irritation.
Causes eye irritation.
Ingestion may be harmful if swallowed.
- Limonene [111]
- Hazard statements
Flammable liquid and vapor.
May be harmful if swallowed.
Causes skin irritation.
May cause an allergic skin reaction.
Very toxic to aquatic life.
- Precautionary statements
Avoid release to the environment.
Wear protective gloves.
- Potential health effects
Inhalation may be harmful if inhaled. Causes respiratory tract irritation.
May be harmful if absorbed through skin. Causes skin irritation.
Causes eye irritation.
Ingestion may be harmful if swallowed.
- Linalool [112]
- Hazard statements
Combustible liquid.
May be harmful if swallowed.
Causes skin irritation.
Causes serious eye irritation.
May cause respiratory irritation.
- Precautionary statements
Avoid breathing dust/fume/gas/mist/vapors/spray.
IF IN EYES: Rinse cautiously with water for several minutes. Remove contact lenses, if present and easy to do. Continue rinsing.
- Potential health effects
Inhalation may be harmful if inhaled. Causes respiratory tract irritation.
May be harmful if absorbed through skin. Causes skin irritation.
Causes eye irritation.
Ingestion may be harmful if swallowed.
Conclusions
The “vaping crisis” has been reported on numerous times by all of the major media outlets (radio, Internet, newsprint, radio, and television). Vaping is causing lung illnesses and lung damage to such a degree that hospital treatment is usually required, and in several notable cases, death occurs. What is always reported as possible causes are the additives in the vape cartridges and/or residual pesticides, herbicides, and even dangerous heavy metals because of lax regulation, which allowed the vape cartridge black market to grow ever larger.
The THC, CBD, and nicotine vape cartridges can have additives, which include flavorings, propylene glycol, vegetable glycerine, and vitamin E acetate (all organic chemicals). These additives along with the pesticides and herbicides can decompose into dangerous chemical compounds when heated to high temperatures, which is not surprising given the known behavior of organic chemicals during decomposition. What is important to consider is the fact that the majority (approximately 76%±) of those injured were vaping THC [113, 114].
What is not being reported is the fact that THC and CBD can also decompose when heated excessively and form chemical compounds that can also cause serious health issues, including lung ailments. Further, the naturally occurring or added terpenes themselves are lung irritants. For some reason though, THC and CBD and the associated terpenes are not being considered as part of the problem. Another concern is related to the proper temperature regulation by the user and/or control circuitry of the vaping device; this key detail is also not being discussed either.
Using chemistry and science as a basis, one can conclude that this crisis may simply be related to the decomposition of organic chemicals when heated at or above their respective smoke point, namely, the temperature at which decomposition begins to occur. Further, the organic chemical compounds of concern should also include THC and CBD. Even if the THC or CBD are not heated to or above their respective smoke points, the naturally occurring or added terpenes are known lung irritants. Also, investigators should also determine whether or not there is a dabbing component tied to the vaping crisis because both activities produce similar harmful by-products and also involve terpene inhalation, and those who vape THC and/or CBD may also dab THC and/or CBD. Simply stated, the vaping crisis may also be related to dabbing. Further, the Center for Disease Control (CDC) may also want to update its new acronym, EVALI, which stands for “electronic cigarette (e-cigarette), or vaping, product use associated lung injury,” so that it includes dabbing.
Dr. Christine Miller, Dr. Kenneth Finn
The author declares no competing financial interest.