Introduction
Cannabis is the most widely consumed illicit drug in the world today with an estimated 182.5 million users, which represents 3.8% of the global population. Cannabis is a complex mixture of several cannabinoids of which THC (Δ9-tetrahydrocannabinol) and cannabidiol (CBD) are the main active components. These components are present in variable amounts and proportions in each preparation. The activity of cannabis is likely influenced by terpenes and terpenoids, which vary in content and type [1]. Furthermore, the content of marijuana is not tightly regulated even in most legalized markets, which may lead to more intense concentrations of biologically active components as well as contamination with synthetic compounds or other illicit drugs.
The World Health Organization reports that marijuana use exceeds cocaine or opiates by an order of magnitude [2]. In North America, 15- to 64-year-olds abuse marijuana more than any other illicit substance with an estimated annual prevalence of 11.6% [2]. Despite its classification traditionally as an illicit substance in many nations, in recent years in the United States, 33 states and the District of Columbia have approved the clinical use of cannabis for various conditions and 10 states have legalized marijuana for recreational and medicinal purposes [3]. Medical use of marijuana focuses primarily upon its neurological and cognitive effects to include management of chronic pain and fibromyalgia, relief of spasticity in multiple sclerosis, and as an anti-emetic in the treatment of chemotherapy-induced nausea.
Until recent decades, the effects of cannabis on other organ systems beyond neurocognitive systems were not largely studied. However, a need for better understanding of cannabis effects upon the cardiovascular system has emerged with ever more importance, given the rapid increase and spread in cannabis use and that cardiovascular disease remains the leading cause of mortality worldwide, with estimated global mortality of 17.9 million deaths in 2016 and 630,000 deaths within the United States in 2015 [4]. A growing body of evidence has established that cannabis has potential adverse biological and clinical effects on the cardiovascular system. Cannabis consumption elicits numerous identified hormonal, adrenergic, vasospastic, and atherogenic effects upon the vasculature. Furthermore, medical research has demonstrated causal pathways for cannabis that cause arrhythmia, myocardial infarction (MI), cerebrovascular accident, myocarditis, peripheral ischemia, pulmonary vascular disease, and sudden cardiac death.
With the recent increased legalization and use of cannabis in the United States as well as worldwide, further research is needed to better understand the potential, frequency, and severity of cardiovascular harm caused by this drug and to develop public health educational programs about its adverse effects.
Biological Cardiovascular Effects of Cannabis
An important body of evidence has accumulated from basic science and observational studies regarding the biological and cardiovascular effects of cannabis on human physiology. Despite this, the efforts of researchers in understanding the biological effects of cannabis are challenging due to confusions that arise as a result of polysubstance use among cannabis subjects, which may or may not be fully disclosed to researchers, including tobacco, cocaine, alcohol, supplements, or illicit drugs or other substances. Cannabis effects depend upon the affinity of cannabinoids for CBD receptors 1 and 2 (CB1, CB2). These receptors are present, to varying degrees, in different body tissues and are responsible for the subsequent central and peripheral effects that we will further discuss in this section. CB1 receptors are expressed predominantly in the brain, cardiac muscle, liver, gastrointestinal tract, vascular endothelium, vascular smooth muscle cells, and kidney. CB2 receptors are predominantly expressed in immune cells and on endothelial cells. Adipocytes, platelets, and bronchial epithelium express both CB1 and CB2 receptors [5].
Marijuana use promulgates the formation of reactive oxygen species, decreases myocardial contractility, provokes a pro-inflammatory endothelial response, and promotes neointimal proliferation of vascular smooth muscle. It is, in part, because of these effects that marijuana use has been associated with adverse cardiovascular outcomes which include acute coronary syndromes, coronary artery dissection, coronary vasospasm, coronary thrombosis, arrhythmias, stroke, vasculitis, myocarditis, and cardiomyopathies [6].
Cannabis and Its Role in the Pathophysiology of Atherosclerosis
Cannabinoids affect atherogenesis via their effects on monocyte adhesion and cytokine expression. In atherogenesis, when vascular endothelium is injured, low-density lipoprotein cholesterol subsequently infiltrates the subendothelial layer. Concurrently, smooth muscle cells migrate to and infiltrate the intima of the vascular wall. Monocyte-derived macrophages accumulate oxidized low density lipoprotein resulting in the formation of foam cells, an early component of developing atherosclerotic plaque. Lipid uploading by macrophages is associated with the expression of inflammatory cytokines, which then activates type 1 T-helper cells (TH1). The TH1 cells then, in turn, stimulate the macrophages to continue to express inflammatory cytokines, which further contribute to the chronic atherosclerotic disease process [7].
In low doses, the main psychoactive component of marijuana, THC, decreases monocyte adhesion and infiltrates the vascular subendothelial layer via activation of CB2 receptors. Additionally, THC influences the macrophage’s cytokine release, decreasing interferon-ƴ release, which in turn downregulates the type 1 T-helper cell (TH1) immune response. [5] Conversely, CB1 expression has been identified in macrophages of advanced atheroma, and a higher number of CB1 receptors exist in coronary atheroma patients with unstable angina compared to those with stable angina [8]. As monocytes differentiate into macrophages, there is increased expression of CB1 receptors. The increased CB1 receptors correlate with increased reactive oxygen species production and endothelial cell injury, and additionally, CB1 receptor agonism results in increased lipid accumulation in macrophages [9]. There have been several studies investigating the effect of CB1 receptor blockade, which resulted in decreased inflammatory cytokine production, and inhibition of monocyte recruitment. [5, 8, 10, 11] In a mouse study, a decreased atherosclerotic lesion development with CB1 receptor antagonism was observed, which the authors theorized was in part related to cholesterol inhibition and in part related to anti-inflammatory effects [11].
Cannabinoids also influence vascular smooth muscle cell growth and proliferation, which contribute to atherosclerosis and stent restenosis. CB2 agonism decreases the production of TNF-α, an inflammatory cytokine that signals smooth muscle cells to proliferate and infiltrate the intima. Conversely, CB1 antagonism decreases platelet-derived growth factor production and agonism upregulates angiotensin 1 receptor leading to increased reactive oxygen species [5].
Although the relationship of CBD receptors to atherosclerosis is complex and multifactorial, general studies have shown contrasting effects of CB1 and CB2 receptors on the development of atherosclerosis, with CB1 agonism promoting atherosclerosis while CB2 agonism preventing it.
Physiological Cardiovascular Effects of Cannabis
Marijuana exhibits dose-dependent increases upon the heart rate, cardiac output, supine blood pressure, and postural hypotension [5, 12]. Heart rate can increase by 20–100%, with peak heart rate 10–30 minutes after inhaling marijuana smoke [13]. Smoking marijuana decreases time to maximum predicted heart rate with exertion and decreases the maximum exercise capacity of even healthy individuals without clinically significant coronary artery disease [5]. Increased activity of sympathetic nervous system, stimulation of beta-adrenergic receptors with increased plasma norepinephrine levels, inhibition of parasympathetic innervation of the heart, and reflex tachycardia due to vasodilation are all proposed mechanisms for tachycardia seen with cannabis use [14, 15].
Marijuana smoke exposure has been associated with the precipitation of angina in people with existing coronary artery disease. In one study, the exercise time of chronic stable angina patients decreased by an average of 48% after smoking one marijuana cigarette versus 23% after smoking a nicotine cigarette [12, 16, 17]. One proposed mechanism for the lower angina threshold is an increase in the levels of carboxyhemoglobin with decreased oxygen-carrying capacity of red blood cells. Additionally, catecholamine release increases heart rate and myocardial contractility, thereby resulting in oxygen demand [15]. These actions cause a net increase in myocardial oxygen demand with a decrease in oxygen supply [17].
In one study of 147 patients with cannabis associated myocardial infarction (with coronary imaging was available for 21 patients), 38% of patients had single-vessel coronary thrombosis; another 38% had normal results [18]. While some myocardial infarctions may be related to increased myocardial oxygen demand and decreased oxygen supply, other patients have a culprit lesion which is proposed to be due to disruption of vulnerable atherosclerotic plaque in response to hemodynamic effects associated with cannabis use [19].
In a retrospective study of nearly 2.5 million hospitalized patients with history of marijuana use, the burden of arrhythmia was evaluated and it occurred in about 2.7% of patients with atrial fibrillation being the most common, followed by ventricular tachycardia and atrial flutter [20]. Ventricular tachycardia with right bundle branch block pattern and left axis deviation without significant atherosclerotic disease has been described in the literature [21, 22] and it is hypothesized that it is triggered by activity in Purkinje fibers or reentry in a small region of the inferior left ventricle [22]. This form of ventricular tachycardia is responsive to verapamil therapy [22, 23].
In a case report of a 34-year-old male habitual marijuana user who developed ventricular tachycardia (VT), the VT was monomorphic with a right bundle branch block morphology and left axis deviation which responded to cardioversion [22]. He underwent coronary angiography and was found to have normal-appearing coronary arteries without stenosis, but had a marked reduction in coronary flow. After verapamil administration, he had normal coronary flow, and with repeat coronary angiography 3 days later, he again was found to have normal coronary flow. When initially undergoing electrophysiology testing, his VT was inducible, and after cessation of marijuana and treatment with verapamil, he no longer had inducible VT.
In addition to tachyarrhythmia, asystole has also been described in one case study [24], which showed that a 21-year-old male had recurrent episodes of presyncope and syncope while smoking marijuana. A Holter monitor demonstrated multiple symptomatic pauses, which corresponded to episodes where he was smoking marijuana. The proposed mechanism is thought to be due to a sudden increase in parasympathetic tone and parasympathetic activity, as demonstrated in mice [25]. CB1 receptor activation in the heart was found to have a triphasic response with initial vagally mediated fall in heart rate and blood pressure, then a brief non-sympathetically mediated pressor response, followed by a prolonged hypotensive effect due to decreased cardiac contractility and total peripheral resistance. Cannabinoids can elicit vasorelaxation, in part, by triggering the release of calcitonin gene-related peptide which induces vasorelaxation in isolated blood vessels [25].
The mechanisms of marijuana-induced myocardial infarction and ventricular arrhythmias are only partially understood, but these effects are thought to be due to the stimulation of the sympathetic nervous system and decrease in parasympathetic autonomic tone. This is demonstrated by slow or no flow in the coronary arteries, as TIMI grade coronary flow is a surrogate for blood flow in the microcirculation [22].
Sudden cardiac death or cardiomyopathy following cannabis use is rarer than myocardial infarction related to cannabis use; however, the exact incidence is difficult to determine as there may be underdiagnosis of marijuana as a causative agent for sudden death and myocardial infarction. For example, in the YOUNG MI registry, the adjusted hazard ratio for marijuana abuse was similar in effect size to cocaine for cardiovascular death, yet marijuana use may not be systematically tested for or reported as causal in MI or sudden death [6]. Bachs reviewed six cases of pathology review of likely acute cardiovascular cause of death and recent cannabis ingestion [15]. All subjects were young adults (17–43 years) whose sudden death appeared to be related solely to marijuana use. Toxicology studies revealed only presence of THC in the blood and urine, and all patients were healthy before sudden death.
There are a few case reports of stress cardiomyopathy due to cannabis use. One case report showed that a female with chronic cannabis use developed recurrent episodes of stress cardiomyopathy with reintroduction of cannabis [26]. The pathophysiology of stress cardiomyopathy in cannabis users is poorly defined, but it is thought to be associated with catecholamine surge. All studies investigating the role of cannabis in acute myocardial infarction and sudden death are observational which is hypothesis generating, but the infrequency of such reports prevents any certainty regarding the potential for direct effect of marijuana on left ventricle ejection fraction or sudden cardiac death.
There is likely a multifactorial etiology for some of the cardiovascular complications associated with cannabis use, and life style choices may play a significant role. The CARDIA study demonstrated that patients who use marijuana have a high caloric diet and were more likely to smoke tobacco and use other illicit drugs [27, 28].
Despite overall adverse cardiovascular physiologic and clinical effects of cannabis, paradoxically increasing reports of cannabis use among recreational and elite athletes have emerged. Although most competitive sports prohibit cannabis use during competition, no restriction may be required during training and some athletes report a perception of improved performance. However, as described above, cannabis would appear in sum to have deleterious effects on most athletic performance; thus, athletes’ perceived performance enhancement may simply result from anxiolysis, pain mitigation, or placebo effect rather than a real cardiovascular performance enhancement [29].
Pulmonary Vascular Biological Effects of Cannabis
No ample literature is available regarding the biological effects of cannabis on the pulmonary vascular system, but cannabis has known associations with lung disease, resultant pulmonary vasoconstriction, and pulmonary hypertension. This is a problem that is understudied and underappreciated. Regular marijuana smokers complain of more chronic bronchitis symptoms of chronic productive cough and wheezing [30], but there has been mixed data regarding chronic marijuana smoking and the risk of developing emphysema and reduced lung function compared to that of nicotine cigarette smoking [31–33]. A mouse study evaluating the effects of marijuana smoke on lung tissue found that the mice developed severe pulmonary hyper-responsiveness, inflammation, and emphysema [34]. These effects are related to elevated concentrations of four inflammatory cytokines, MCP-1, IFN-ƴ, TNF-α, and IL-12, which induce basophil and mast cell degranulation, induce nitric oxide synthase production, and enhance phagocytosis, IL-1 and PGE2 syntheses, and neutrophil accumulation. The activation of these cytokines leads to significant inflammation that eventually results in pulmonary tissue destruction [34].
The consequent severe lung disease results from parenchymal destruction as well as chronic pulmonary vascular disease including pulmonary hypertension.
Cerebrovascular Biological Effects of Cannabis
Cannabis-related cerebral infarction is an uncommon finding with less than 100 clinical cases reported in the literature. In a literature review examining 71 cannabis users with cerebral infarctions [18], a young (mean age 35.5 years) male predominance with a slight predilection for the posterior cerebral circulation was observed, with the majority being cerebellar and occipital infarctions. Most patients were regular users of marijuana and all had used marijuana within 24 hours of symptom onset. There is a temporal relationship between the use of cannabis and cannabis-associated cerebral infarct with studies demonstrating cerebral infarct or transient ischemic attacks (TIA) while actively smoking marijuana up to 30 minutes after cannabis inhalation [35]. There are several proposed mechanisms of cerebral infarcts and transient ischemic attacks after cannabis use, which include orthostatic hypotension with secondary impairment of autoregulation of cerebral blood flow or increased resistance in cerebral arteries, altered cerebral vasomotor function, supine hypertension and labile blood pressure, cardioembolism with atrial fibrillation or other arrhythmias, vasculopathy (toxic or with immune inflammatory), vasospasm, reversible cerebral vasoconstriction syndrome (RCVS) [36], and multifocal intracranial stenosis (MIS) [35]. Additionally, reduction in cerebral blood flow affects the cerebellum and causes cerebellar ischemia [37].
In a prospective cohort study of 48 patients admitted with acute ischemic stroke, of the patients who tested positive for cannabis (13 patients), there appeared to be a specific pattern of multifocal intracranial stenosis (MIS) in posterior cerebral arteries and superior cerebellar arteries appreciated on magnetic resonance angiography (MRA) and coronary angiography (CA), and upon follow-up, there was a partial or total reversibility of vasoconstriction within 3–6 months [38]. A study by Wolff et al. [35, 38] suggested reversible intracranial stenosis as a favored mechanism of action, but this contrasts with a subsequent literature review. Wolff et al. published a subsequent literature review of cannabis-associated acute cerebral infarct patients and a little more than half of those patients, 54% (n = 25), had abnormalities on cerebrovascular imaging [35].
Review of the literature highlights the difficulty in determining the mechanisms of stroke in cannabis users because in many of the cases reported, there was no adequate radiographic neurovascular evaluation during the acute phase of stroke and most patients did not have subsequent radiographic imaging upon follow-up. Furthermore, many of the patients may have reported or unreported polysubstance abuse [35, 39].
Peripheral Vascular Biological Effects of Cannabis
Numerous case reports have been published concerning cannabis or THC-associated arteritis, which may be one of the most frequent causes of peripheral arterial disease in adults under 50 years of age [40]. Cannabis use is associated with lower limb arteritis, which is mostly unilateral and has predominance in young males. Affected vessels often lack any evidence of conventional atherosclerotic disease. A literature review assessing 80 cannabis-associated arteritis patients [18] demonstrated that the average age of presentation was 28 years and 96% of these patients had involvement of their lower extremities. Most patients presented with painful distal necrosis of their limbs after several months of claudication, and vascular imaging revealed distal arterial occlusions in 97% of patients and their occlusions were described as consistent with thromboangiitis obliterans (TAO) [18]. It is not clear whether cannabis-associated arteritis might be a subtype of TAO or whether it is an entirely different entity, as there is differing opinion in the literature [18, 40].
When compared with other TAO patients, patients with cannabis-associated limb arteritis are younger, more often male, have more frequent unilateral involvement of the lower limbs at clinical presentation, and have fewer occurrences of thrombophlebitis and Raynaud’s phenomenon. In patients with cannabis arteritis, cannabis cessation was associated with arteritis remission, even during continued tobacco use. On the other hand, cannabis reintroduction after a period of cessation was associated with clinical arteritis recrudescence. Cannabis-associated arteritis has a poor prognosis with greater than 50% of patients requiring limb amputation without cannabis cessation [18].
Summary of Biological Effects of Cannabis (See Table 9.1)
Summary of the major cardiovascular and cerebrovascular adverse effects related to cannabis inhalation
Cardiovascular | Peripheral | Cerebrovascular |
|---|---|---|
Myocardial infarction Coronary slow flow or no-reflow Coronary vasospasm Coronary artery dissection Coronary thrombosis Cardiac arrhythmia Worsened angina Tachycardia Hypertension and hypotension Myocarditis | Arteritis Vasculitis Ischemic ulcer Digital necrosis Raynaud’s phenomenon | Reversible cerebral vasoconstriction syndrome Transient ischemic attacks Cerebral slow or no reflow Stroke |
Cardiac Adverse Clinical Outcomes Caused by Cannabis Use
Angina
Studies have investigated the effect of inhaled cannabis on patients with exertional angina who were not regular users of cannabis. In one study, 10 male subjects of age 41–53 years exercised without smoking and then in a double-blind fashion smoked cannabis containing 18–20 mg THC; then the time taken to develop angina was investigated and considered as the primary endpoint. All patients had greater than 75% angiographically proven coronary stenosis in at least one major coronary artery [17]. In another study, 10 males 43–55 years of age underwent exercise after smoking marijuana versus placebo cigarette to evaluate time to development of angina [16]. Marijuana-containing cigarettes decreased exercise time to angina compared to the control by 48% whereas the placebo cigarette decreased exercise time to angina also, but by just 8.6% versus baseline [16, 17]. The authors hypothesized that the anginal effect of THC is attributable in part to the increased myocardial oxygen demands caused by faster increases in heart rate within minutes of inhalation.
Myocardial Infarction
Previously, cannabis users and the medical community underappreciated the risk of significant public health burden resulting from development of myocardial ischemia. However, over the past several years, there is a growing body of evidence that demonstrates the occurrence of acute coronary syndromes in otherwise young, healthy users of marijuana. Typically, they are young male patients without significant cardiovascular comorbidity who present with chest pain, ST segment elevation on ECG, and positive troponin after using marijuana. In many of the case reports, toxicology screening was negative for cocaine, opiates, and amphetamines while positive for marijuana, which suggests that marijuana use itself can be responsible for acute myocardial infarction [41].
A case–control study of patients after myocardial infarction has estimated that the risk of myocardial infarction in cannabis users is 4.8 times greater than the baseline in the first hour after cannabis use and is likely due to its short duration of action. In the second hour after smoking, the risk decreased to 1.7 times [12].
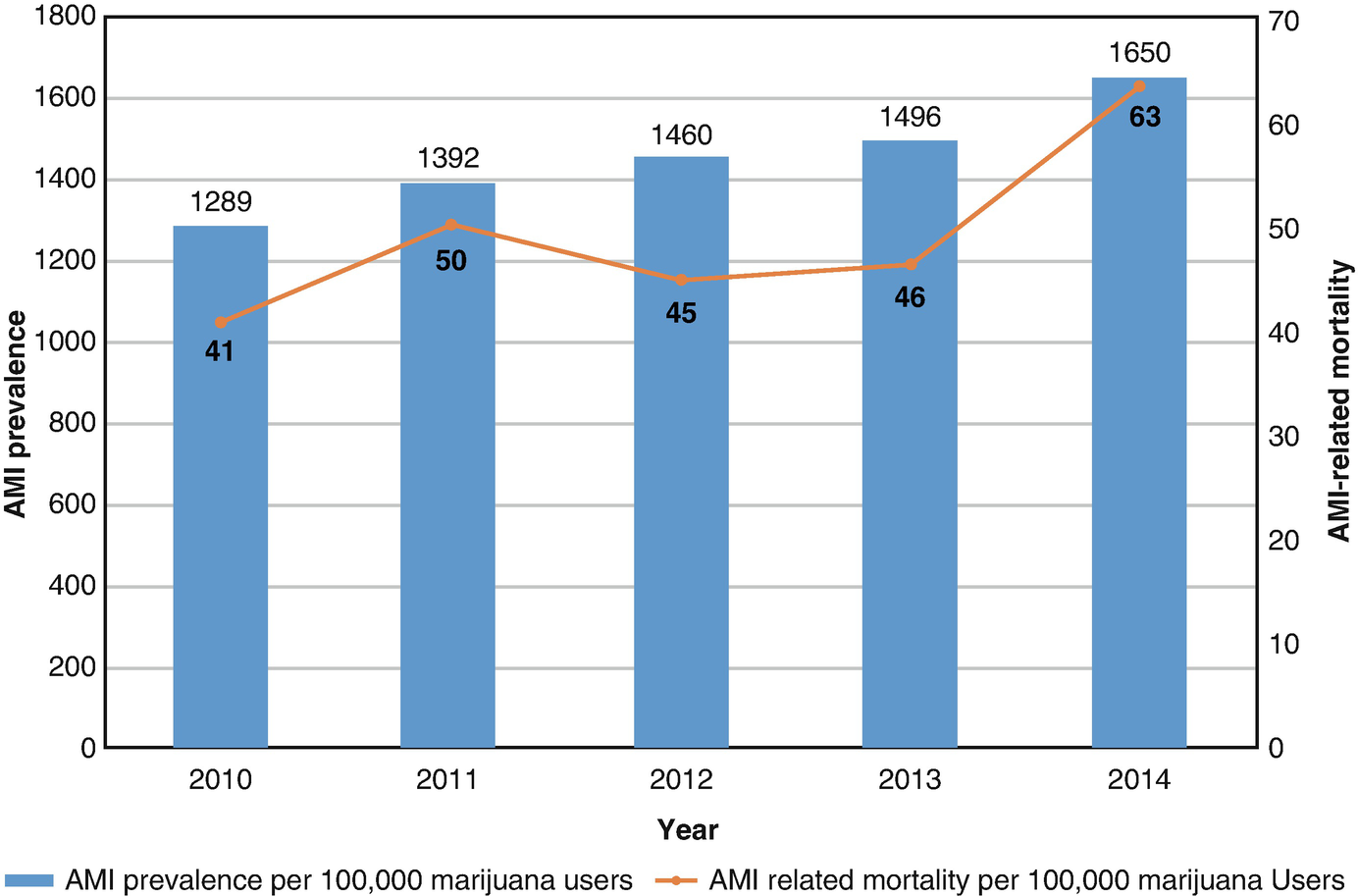
Trends of acute myocardial infarction prevalence and mortality per 100,000 marijuana users in the United States [42]

Prevalence trends of congestive heart failure, cardiogenic shock, dysrhythmias, and respiratory failure in acute myocardial infarction patients with marijuana use (11–70 years) [42].
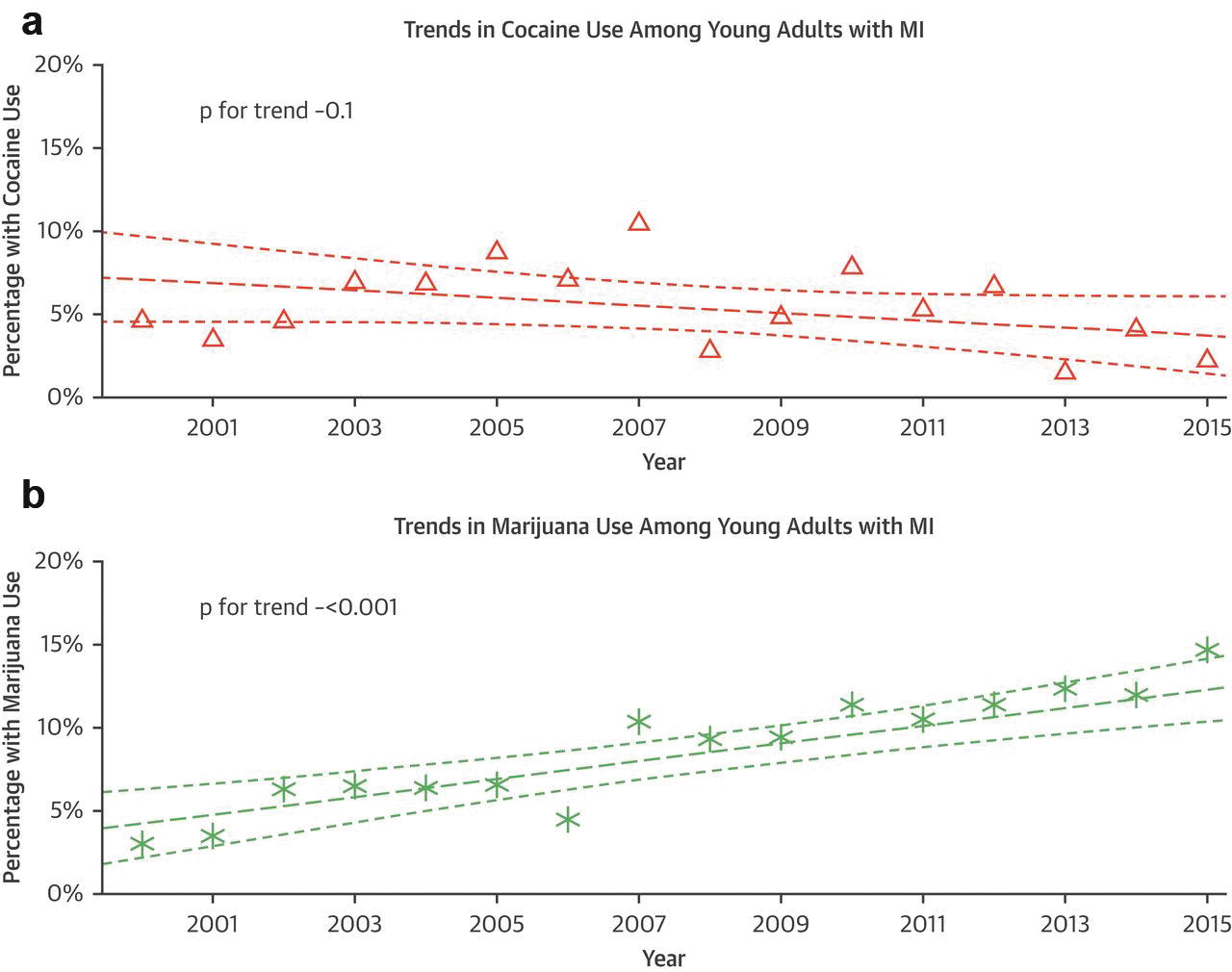
Trends in substance use over time [6]. Trends in (a) cocaine and (b) marijuana use over the course of the study period, 2000–2016. The thick dashed line represented a fitted regression line and the thinner dashed line are confidence intervals. MI myocardial infarction. Triangles represents the percentage of patients with MI for the particular year who used cocaine. Asterisks represent the percentage of patients with MI for the particular year who used marijuana

Adjusted cardiovascular mortality and all-cause death [6]. Forest plots are shown for adjusted model of all-cause and cardiovascular (CV) death. All-cause death was adjusted for age, sex, presence of diabetes, hypertension, peripheral vascular diseases, smoking, high-density lipoprotein cholesterol, triglycerides, revascularization, creatinine, medications are discharge, and length of stay. CV death was adjusted for age, presence of diabetes, hypertension, peripheral vascular diseases, smoking, high-density lipoprotein cholesterol, creatinine, medications at discharge, and length of stay. Adj, HR adjusted hazard ratio; CI confidence interval
Arrhythmia

Frequency of subtypes of arrhythmias per 100,000 hospitalized marijuana users [20]
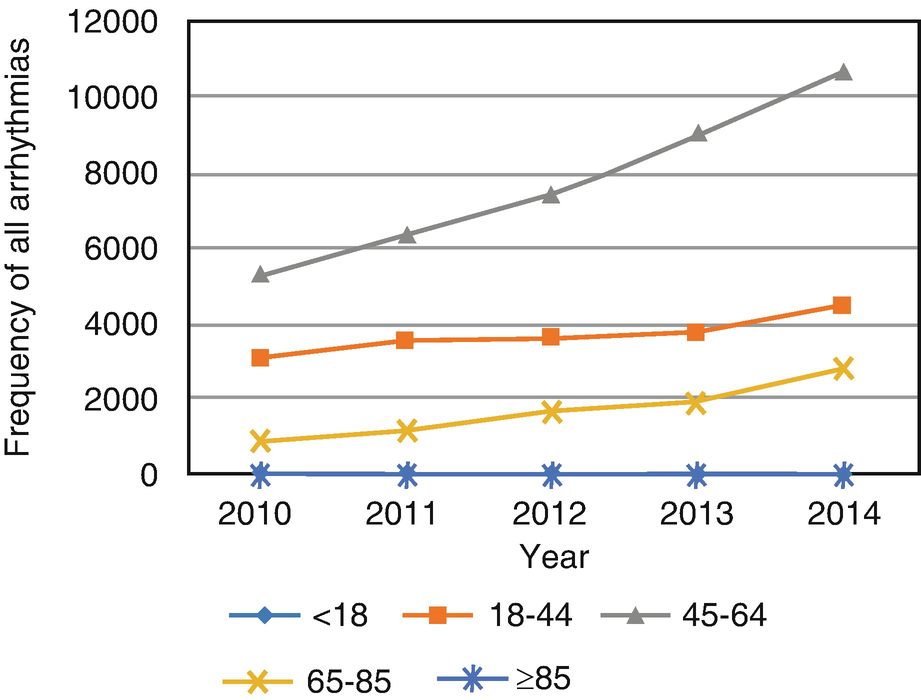
Frequency of all arrhythmias in hospitalized marijuana users by age [20]
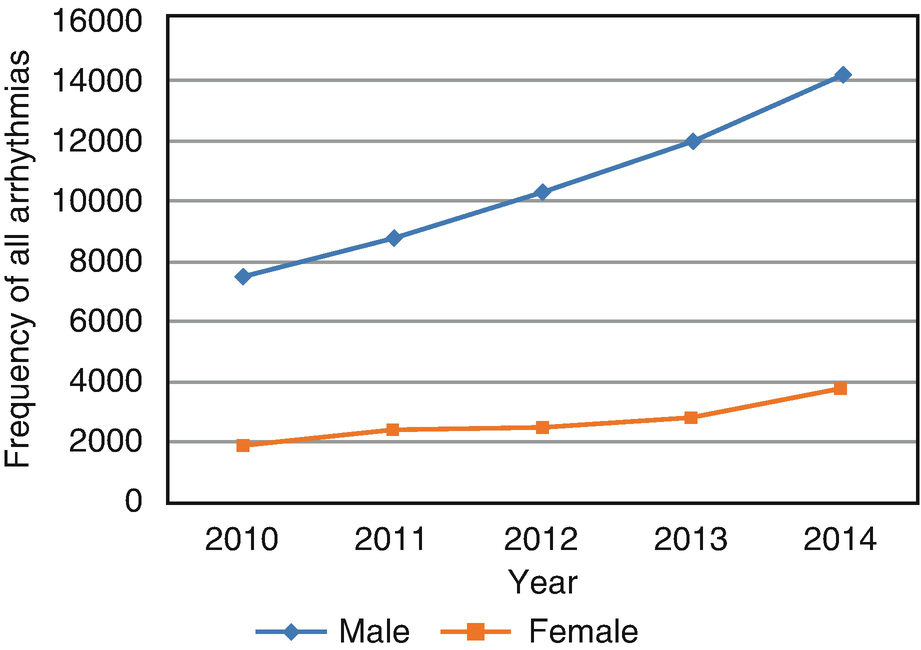
Frequency of all arrhythmias in hospitalized marijuana users by sex [20]
Sudden Cardiac Death
Marijuana has traditionally been regarded as a relatively safe recreational drug, though some case reports link its use with sudden death. One comprehensive review showed that there were at least 35 reports of cases of significant cardiovascular emergencies and at least 13 deaths from a cardiovascular mechanism and there was likely to have been an underestimate of the true incidence of its contribution to sudden cardiac death. The age of the 13 people who died ranged from 17 to 52 years (median 37 years, all males). In eight of the cases, there was some degree of significant coronary atherosclerosis: three with superimposed thrombus, two with dilated cardiomyopathy, and at least three suffering from an acute myocardial infarction [1]. Five of the cases had little or obvious pathology, whose age ranged from 17 to 42 years (mean 31 years, all male). In all of these cases, the authors believed that cannabis significantly contributed to their deaths, possibly due to arrhythmia [1].
Myocarditis
There are at least five reports of pericarditis and myocarditis shortly after marijuana use in the literature. One of the cases was due to accidental exposure in an 11-month-old child which ultimately resulted in death [44]. Other published cases reported recovery with cannabis cessation and medical management [45–47].
Marijuana content, potential, and contiminants vary significantly; thus safety and regulation prove difficult even in legalized markets. The pathogenesis of pericarditis/myocarditis after marijuana use is unclear. Reports have shown fungi (Aspergillus, Penicillium), bacteria, microbial toxins such as aflatoxins, heavy metals (aluminum), and pesticides to contaminate marijuana. It is possible that contaminants may be the explanation, but further research is necessary to better explain the pathophysiology [48].
Pulmonary Vascular Adverse Clinical Outcomes
The inhalation of marijuana has been associated with adverse pulmonary outcomes such as chronic bronchitis and obstructive lung disease [49]. Studies have shown a dose-response relationship between cannabis and FEV1/FVC ratios, and it has been shown to increase total lung capacitance. This suggests that significant respiratory changes on spirometry occur in cannabis smokers, even at a young age [50, 51]. The incidence of cannabis-associated pulmonary hypertension is underreported and understudied. Because marijuana has been shown to promote lung disease, pulmonary hypertension may be an underappreciated public health burden of the legalization of marijuana.
Cerebrovascular Outcomes

The incidence of stroke-related admissions was higher among cannabis users vs. non-users (0.33% vs. 0.26%, p < 0.001) in a study of discharge records from the National Inpatient Sample (NIS) from 2007 to 2014 [60]
Reversible cerebral vasoconstriction syndrome (RCVS) is a neurological syndrome that affects young adults and is characterized by acute, severe headaches with or without neurological symptoms, and segmental cerebral artery vasoconstriction that appears as “beading” on neurovascular imaging. It tends to resolve within 12 weeks from the initial syndrome [61]. The majority of cases of RCVS can be attributed to a secondary factor that increases vascular tone, which includes vasoactive substances such as marijuana [62]. In one large prospective series, marijuana was the most common vasoactive substance to trigger RCVS in 30% of the patients (67 patients in total) [63]. Marijuana was found to be the definite triggering factor for RCVS in several of the reported cases [64–66]. The prognosis for all comers with RCVS is typically benign, but some patients experience permanent neurological deficits or death.
One retrospective cohort study from Denver, Colorado, looked at the demographics, suspected etiology, and outcomes in patients admitted with RCVS triggered by vasoactive substances with an interest in those triggered by marijuana. Marijuana was the identifiable trigger in four of the six cases and the two remaining cases used marijuana in combination with other drugs. Among the patients who used marijuana, there were five subarachnoid hemorrhages, one with ischemic stroke, and one death. The patients with RCVS attributable to marijuana tended to be younger (26.5 vs. 50.5 years old) and were less likely to be female (33% vs. 76%), but these associations were not statistically significant [67]..
Peripheral Vascular Adverse Clinical Outcomes
Cannabis Arteritis

An exudative ulcerated lesion of the left hallux in a patient with cannabis arteritis [70]

Occlusion of the plantar arch of both feet in a patient with cannabis arteritis [70]
Public Health Implications and Conclusion
Many states have legalized the medicinal and recreational use of marijuana due to potential beneficial effects. Our current evidence base lacks adequate scientific studies to provide thorough risk-benefit considerations for most marijuana use. There is an emerging body of evidence that suggests that patients exposed to marijuana are at risk for myocardial infarction, cerebrovascular disease, myocarditis, peripheral vascular complications, arrhythmias, and sudden cardiac death, and this should raise concerns about its safety and long-term effects. More evidence-based research including prospective cohort study on the effect of marijuana on the cardiovascular system will be necessary as legislative momentum leads to continued approval of marijuana in healthcare settings and recreational use.
The authors report no financial conflicts of interest. The views expressed are those of the author and do not reflect any official policy of Fort Belvoir Community Hospital, Walter Reed National Military Medical Center, the Defense Health Agency, the Department of Defense, or the US government.