5
IS SYMPTOM RELIEF A PATH TO BAD MEDICINE?
“A headache is not caused by a deficiency of aspirin.”
—William Mitchell, N.D., cofounder of Bastyr University
THE HISTORY OF CONVENTIONAL medicine illustrates quite clearly how a treatment that is in vogue at a particular time can later be viewed as completely irrational and counterproductive. Were the physicians of the late nineteenth century as convinced of the efficacy of the dominant treatments of the time (such as bloodletting and the use of toxic compounds, including mercury) as today’s physicians are about their treatments? Undoubtedly, and sadly, the answer is often yes. Certainly there are many safe and effective medical treatments, but I do believe there is a fundamental flaw in the use of most drugs: conventional drugs rarely have a curative effect. Instead they simply act as biochemical Band-Aids to make us feel better.
This focus on relieving symptoms often comes at a very high price. There are countless examples of drugs that take care of a primary symptom but have significant adverse consequences because they do not address the underlying cause. Some drugs create dependency; others interfere with normal physiology in a way that actually intensifies the very condition being treated; some produce side effects worse than the original symptoms.
CASE IN POINT: THE ALLOPATHIC APPROACH TO A HEADACHE
To illustrate the problem that arises when we focus on suppressing symptoms rather than on determining causes, let’s take a look at something very simple—a headache. Although a headache may be associated with a serious medical condition, most headaches are not serious. Headaches can be caused by a wide variety of factors, but the overwhelming majority are either tension or migraine headaches. A quick way to differentiate between the two is the nature of the pain. A tension headache is usually a steady, constant, dull pain that starts at the back of the head or in the forehead and spreads over the entire head, giving a sensation of pressure of a vise being applied to the skull. In contrast, migraine headaches are vascular headaches characterized by a throbbing or pounding sharp pain.
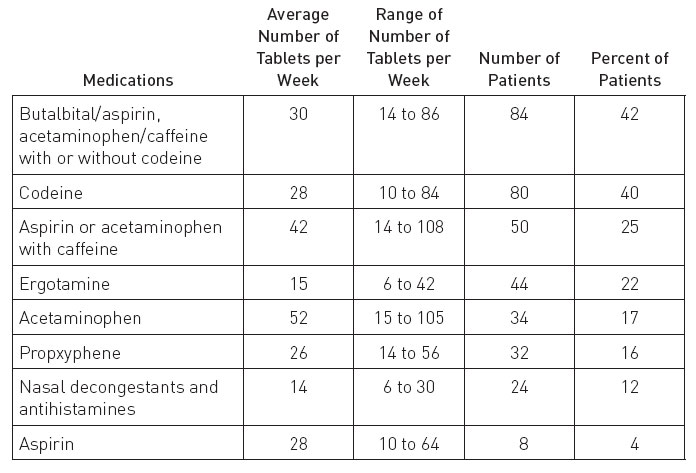
Modern drug treatment of the headache, whether a migraine or tension, is ultimately doomed because it fails to address the underlying cause, and as a result produces a significant risk of side effects. The goal of headache medications is not to identify and eliminate the precipitating factor, but simply to relieve the symptoms. Very interestingly, several clinical studies have estimated that in approximately 70 percent of patients with chronic daily headaches, the headaches are drug-induced. That is, their headaches are due to the medications they are taking to suppress the symptoms of a headache.1 In other words, the headache medications are giving these patients daily headaches; and if they quit taking the drugs, their headaches go away. In one study (summarized below) of 200 patients suffering from analgesic rebound headache, discontinuation of these symptomatic medications resulted in 52 percent improvement in the total headache index. There were specific improvements in general well-being and sleep patterns, and a reduction in irritability, depression, lethargy, and the frequency and severity of headaches.
Profile of 200 Patients with Chronic Daily Headaches1
WHAT CAUSES A TENSION HEADACHE?
If a tension headache is not caused by a deficiency of aspirin or acetaminophen, then what does cause it? Well, there is a reason why it is called a tension headache: it is usually caused by tightening in the muscles of the face, neck, or scalp as a result of stress or poor posture. The tightening of the muscles results in a pinching of a nerve or its blood supply, which in turn results in pain and pressure. Relaxation of the muscle usually brings immediate relief.
TREATING THE CAUSE OF TENSION HEADACHES
The primary therapy should address the factors that cause tension in the neck, face, or scalp muscles. Since the neck is an area of the body that often holds tension produced by psychological stress, it is especially important to learn techniques such as progressive relaxation. In addition, it is important to address any structural factor that may be causing tension headaches. In particular, chiropractic can be quite helpful when misalignment of the spine creates muscular tension in the neck. Several clinical studies provide significant scientific evidence that chiropractic can provide benefits for many patients with neck pain and headaches.2, 3, 4, 5 It is certainly worth a try. An alternative to chiropractic is getting a referral to a conventional physical therapist (PT) from your primary care doctor. Clinical studies have shown that conventional physical therapy consisting of education for posture at home and in the workplace, home exercise, massage, and stretching the cervical spine muscles can reduce the frequency and severity of tension headaches.
Relaxation Exercises Help Children with Chronic Headaches
Learning how to relax and diffuse tension goes a very long way in the treatment and prevention of tension headaches. Teaching people with chronic tension headaches how to relax, or using biofeedback therapies, has been shown, in clinical studies, to provide exceptional benefits without side effects. One of the more interesting studies considered the effectiveness of school-based relaxation training by nurses as a treatment for chronic tension headache in children (10–15 years old).6 These children’s headaches were, significantly reduced, compared with those of children in a no-treatment control group, after six weeks and at a six-month follow-up. At the time of the two evaluations, 69 percent and 73 percent of the students, respectively, trained in relaxation had achieved a clinically significant improvement (at least a 50 percent improvement) as compared with 8 percent and 27 percent of the children, respectively, in the no-treatment control group. The conclusion is that teaching kids with chronic tension headaches how to relax can be quite effective and is without side effects. What I really like about this therapy is that it sends kids a better message—rather than getting relief from a pill (drug), they learn how to control the headache themselves. This therapy was developed in Norway, and by now at least seven double-blind studies over a 20-year period support its effectiveness not only for tension headaches but also for migraines.7
WHAT CAUSES A MIGRAINE HEADACHE?
Considerable evidence supports an association between migraine headaches and instability of blood vessels. The mechanism of migraine can be described as a three-stage process: (1) initiation, (2) prodrome (time between initiation and appearance of headache), and (3) headache. Although a particular trigger may be associated with the onset of a specific attack, it appears that initiation depends on an accumulation of several triggers over time. Once a critical point of susceptibility (or threshold) is reached, a “cascade event” is initiated, setting in process a domino effect that ultimately produces a headache. Food allergies, histamine-releasing foods, alcohol (especially red wine), stress, hormonal changes (e.g., menstruation, ovulation, birth control pills), and changes in weather (especially changes in barometric pressure) are some common triggers of migraines.
TREATING THE CAUSE OF A MIGRAINE HEADACHE
The first step in treating a migraine headache is identifying the precipitating factor. Although food intolerance and allergy are most important, many other factors must be considered as either primary causes or contributors. In particular, it is important to assess the possible role of headache medications, especially in chronic headaches. Learning to deal with stress and learning how to relax are also critical. Just as in tension headaches, biofeedback and relaxation training can also be helpful. The effectiveness of biofeedback and relaxation training in reducing the frequency and severity of recurrent migraine headaches has been the subject of more than 35 clinical studies.8, 9 When the results of these studies were compared with those of studies using drug therapy, it was apparent that the nondrug approach was as effective as drugs, and without side effects. These results clearly demonstrate that the primary therapy for migraine headaches should be relaxation. (See Chapter 2 for a description of ways to create the relaxation response.)
My clinical experience indicates that food allergy or sensitivity plays a primary role in many migraine headaches. Many double-blind, placebo-controlled studies have demonstrated that the detection and removal of allergenic foods will eliminate or greatly reduce headache symptoms in the majority of patients, especially children. Food allergy or intolerance induces a migraine attack largely because platelets release compounds, such as serotonin and histamine, that lead to vascular instability. In addition, food additives and foods such as aged cheeses, beer, canned figs, chicken liver, chocolate, pickled fish, the pods of broad beans, red wine, and brewer’s yeast contain compounds (e.g., histamine and tyramine) that can set off migraines in sensitive individuals by causing blood vessels to expand.10, 11, 12, 13, 14
Identify Food Allergies
Many nutritionally oriented physicians perform blood tests to diagnose food allergies. However, in most cases such tests are not really necessary. For patients who have to pay for such tests out of pocket, these tests can be expensive. My experience is that it is best to try a simple elimination diet for seven to 10 days first, to see if your symptoms improve. Start by eliminating the most common allergens:
 Milk and all dairy products
Milk and all dairy products Wheat (including wheat flour products—e.g., bread, pastries, pasta)
Wheat (including wheat flour products—e.g., bread, pastries, pasta) Corn
Corn Citrus fruit (e.g., oranges, tangerines, lemons, and grapefruit)
Citrus fruit (e.g., oranges, tangerines, lemons, and grapefruit) Peanuts and peanut butter
Peanuts and peanut butter Eggs
Eggs Processed foods containing artificial food coloring
Processed foods containing artificial food coloring
As part of an elimination diet, I also recommend using RevitalX—a high-potency multinutrient powdered drink mix from Natural Factors. This product was specifically developed by Michael Lyon, M.D., to be an excellent source of important nutrients to support the gastrointestinal lining and aid detoxification. In an allergy elimination diet, RevitalX is taken twice per day as the primary source of sustenance. RevitalX is mixed with water or juice (fresh vegetable juice is preferred), or it can be blended as a fruit smoothie. Fresh or steamed vegetables and small amounts of fruit can be eaten when you are hungry, and one simple meal is prepared in the evening: steamed vegetables, lean chicken breast, and brown rice (cooked beans, split peas, or lentils along with brown rice can be used as a vegetarian alternative). A lightly sautéed stir-fry can also be prepared for this meal.
If your symptoms disappear within seven to 10 days, you’re on the right track. By slowly reintroducing the previously avoided foods back into the diet (for example, trying one “new” food every three days), and paying attention to which ones cause symptoms to return, you can identify the real culprit.
Will you be able to eat that food again? This depends on whether the allergy is cyclic or fixed. Cyclic allergies develop slowly and result from repeatedly eating a certain food. After the allergenic food has been avoided for a period of time (typically three to four months), it may be reintroduced. Usually the food won’t cause symptoms again unless you eat it too frequently or in large amounts. Cyclic allergies account for roughly 80 to 90 percent of food allergies. Fixed allergies occur whenever a food is eaten, no matter how much time has passed. If you have a fixed allergy, you will remain allergic to the food for life.
Several natural products have shown impressive results in the treatment of migraine headaches:
 Riboflavin. One of the theories used to explain a migraine headache is that it is caused by reduced energy production within the mitochondria, units of cells of blood vessels in the head. Therefore, because vitamin B2 (riboflavin) can potentially increase cellular energy production, it was thought that this vitamin might prevent migraine. In one double-blind study with riboflavin—400 milligrams (mg) daily—the proportion of patients who improved by at least 50 percent was 15 percent for a placebo and 59 percent for riboflavin.15 There were no side effects attributed to the riboflavin therapy. It is notable that riboflavin is as nearly as effective as drugs for migraines, but is much safer and relatively cheap.
Riboflavin. One of the theories used to explain a migraine headache is that it is caused by reduced energy production within the mitochondria, units of cells of blood vessels in the head. Therefore, because vitamin B2 (riboflavin) can potentially increase cellular energy production, it was thought that this vitamin might prevent migraine. In one double-blind study with riboflavin—400 milligrams (mg) daily—the proportion of patients who improved by at least 50 percent was 15 percent for a placebo and 59 percent for riboflavin.15 There were no side effects attributed to the riboflavin therapy. It is notable that riboflavin is as nearly as effective as drugs for migraines, but is much safer and relatively cheap. Magnesium. An insufficiency of magnesium may also play a significant role in many headaches. Several researchers have demonstrated substantial links between low magnesium levels and both migraine and tension headaches. A magnesium deficiency is known to set the stage for the events that can cause a migraine attack or a tension headache.16, 17 Low brain, tissue, and cellular concentrations of magnesium have been found in patients with migraines, indicating a need for supplementation, since a key function of magnesium is to maintain the tone of the blood vessels and prevent overexcitability of nerve cells. Magnesium supplementation can be quite effective in preventing migraine headaches.18, 19 The recommended dosage is 150 to 250 mg three times daily. Magnesium bound to citrate, malate, or aspartate is better absorbed and better tolerated than inorganic forms such as magnesium sulfate, hydroxide, or oxide, which tend to have a laxative effect. An increased intake of high-magnesium foods such as nuts, tofu, and green leafy vegetables also makes a lot of sense.
Magnesium. An insufficiency of magnesium may also play a significant role in many headaches. Several researchers have demonstrated substantial links between low magnesium levels and both migraine and tension headaches. A magnesium deficiency is known to set the stage for the events that can cause a migraine attack or a tension headache.16, 17 Low brain, tissue, and cellular concentrations of magnesium have been found in patients with migraines, indicating a need for supplementation, since a key function of magnesium is to maintain the tone of the blood vessels and prevent overexcitability of nerve cells. Magnesium supplementation can be quite effective in preventing migraine headaches.18, 19 The recommended dosage is 150 to 250 mg three times daily. Magnesium bound to citrate, malate, or aspartate is better absorbed and better tolerated than inorganic forms such as magnesium sulfate, hydroxide, or oxide, which tend to have a laxative effect. An increased intake of high-magnesium foods such as nuts, tofu, and green leafy vegetables also makes a lot of sense. Petadolex®. This standardized extract from the butterbur plant (Petasites hybridus) has been shown in several double-blind studies to produce excellent results as a treatment for migraine headaches, without side effects.20 In one study, 60 patients with headaches randomly received either 50 mg of Petadolex twice daily for 12 weeks, or a placebo.21 Petadolex reduced the frequency of attacks by 46 percent after four weeks, 60 percent after eight weeks, and 50 percent after 12 weeks of treatment. (The results for the placebo group were: 24 percent, 17 percent, and 10 percent, respectively.) Petadolex is generally well tolerated, but diarrhea has been reported in some individuals. If this side effect occurs, discontinue use. Its safety during pregnancy and lactation has not been determined. The typical adult dosage ranges from 50 to 100 mg twice daily with meals.
Petadolex®. This standardized extract from the butterbur plant (Petasites hybridus) has been shown in several double-blind studies to produce excellent results as a treatment for migraine headaches, without side effects.20 In one study, 60 patients with headaches randomly received either 50 mg of Petadolex twice daily for 12 weeks, or a placebo.21 Petadolex reduced the frequency of attacks by 46 percent after four weeks, 60 percent after eight weeks, and 50 percent after 12 weeks of treatment. (The results for the placebo group were: 24 percent, 17 percent, and 10 percent, respectively.) Petadolex is generally well tolerated, but diarrhea has been reported in some individuals. If this side effect occurs, discontinue use. Its safety during pregnancy and lactation has not been determined. The typical adult dosage ranges from 50 to 100 mg twice daily with meals.
THE INFECTION “EQUATION”
One of the most significant differences between a naturopathic physician and a conventional medical doctor becomes apparent when you take a look how each views and addresses an infection. Many doctors do not even consider the role of the immune system in the susceptibility to or treatment of an infection. They do not fully understand that the immune system, if functioning optimally, can adequately defend against virtually all infectious organisms except those that are particularly virulent.
Whether we develop an infection or not is a result of the strength of our defense mechanisms versus the virulence of the infective organism. An infection can be thought of, loosely, as like a mathematical equation, such as one plus two equals three. In an infection, what will determine the outcome is the interaction of the host’s immune system with the infecting organism. A naturopathic doctor tends to use treatments designed to enhance the immune system, whereas most conventional doctors tend to use antibiotics designed to kill the infecting organism, even if antibiotic therapy has been shown to be of limited (if any) value.
Conventional medicine has been obsessed with killing the infective organism rather than promoting defense against infection. This obsession really began with Louis Pasteur, the nineteenth-century physician and researcher who played a major role in the development of germ theory. This theory holds that different diseases are caused by different infectious organisms. Much of Pasteur’s life was dedicated to finding substances that would kill the infecting organisms. Pasteur and later figures who pioneered effective treatments for infectious diseases have given us a great deal for which we all should be thankful. However, there is more to the situation than the virility of the organism.
Another nineteenth-century French scientist, Claude Bernard, also made major contributions to medical understanding. But Bernard had a different view of health and disease. He believed that a person’s internal environment was more important in determining disease than any infective organism or pathogen. In other words, he believed that the internal terrain or the host’s susceptibility to infection was more important than the germ. Physicians, he believed, should focus more on making this internal terrain a very inhospitable place for disease.
Bernard’s theory led to some rather interesting studies. In fact, a firm advocate of germ theory would consider some of these studies absolutely crazy. One of the most interesting was conducted by a Russian scientist, Élie Metchnikoff, the discover of the white blood cells. He and his research associates consumed cultures containing millions of cholera bacteria. Yet none of them developed cholera. The reason: their immune systems were not compromised. Metchnikoff believed, like Bernard, that the correct way to deal with infectious disease was to focus on enhancing the body’s own defenses.
Late in their lives, Pasteur and Bernard engaged in scientific discussions on the virtues of the germ theory and Bernard’s perspective on the internal terrain. Supposedly, on his deathbed, Pasteur said: “Bernard was right. The pathogen is nothing. The terrain is everything.” Whether this is actually true or not, the point is that modern medicine has largely forgotten the importance of the “terrain.”
THE WIDESPREAD ABUSE OF ANTIBIOTICS
Despite my belief that the focus should be on promoting the body’s own defenses against infection, I want to make it very clear that antibiotics definitely have a place in modern medicine. In fact, I am extremely grateful that we have these wondrous agents available. When my daughter, Alexa, was 10 months old she developed a kidney infection from which she probably would not have recovered without antibiotics. There is little argument that when used appropriately antibiotics save lives. However, there is also little argument that antibiotics are grossly overused. The appropriate use of antibiotics makes good medical sense; what does not make sense is the reliance on antibiotics for such conditions as acne, recurrent bladder infections, chronic ear infections, chronic sinusitis, chronic bronchitis, and nonbacterial sore throats. Relying on antibiotics to treat these conditions does not make sense, because the antibiotics rarely provide real benefit.
Cold Remedies and Children
On October 19, 2007, a panel of the FDA voted 13 to 9 to recommend against the use of over-the-counter (OTC) cough and cold products for children under the age of six years. The panel has concluded that these popular medications offered no benefit and involved considerable risk. However, possibly yielding to the demands of drug manufacturers, the panel decided against making a similar recommendation for older children, even though earlier it had agreed there was no evidence that the products do any good for that age group, either.
The FDA is not bound by these conclusions, but it does usually follow the advice of its advisory panels. Officials of the FDA said they would review the complex recommendations and decide how to proceed. Because the products have been on the market so long, formal action could take years, the officials said. But the FDA plans to consult with the industry about possible voluntary action and whether to offer the public interim advice.
No one knows how many children have had adverse reactions to the medications, but the federal Centers for Disease Control and Prevention reported earlier in 2007 that at least 1,500 children younger than age two suffered complications in 2004 and 2005. A review prepared by the FDA for the October 2007 meeting described dozens of cases of convulsions, heart problems, trouble with breathing, neurological complications, and other reactions, including at least 123 deaths.
The hearing came a week after major manufacturers of the medications voluntarily withdrew 14 products designed for children younger than age two, including well-known brands such as Dimetapp Decongestant Plus Cough Infant Drops, Tylenol Concentrated Infants’ Drops Plus Cold, and Robitussin Infant Cough DM Drops.
The widespread abuse of antibiotics is becoming increasingly alarming for many reasons, including a near-epidemic of chronic candidiasis and the development of superbugs that are resistant to currently available antibiotics. According to many experts as well as the World Health Organization (WHO), we are coming dangerously close to a post-antibiotic era when many infectious diseases will once again become almost impossible to treat.
Since there is evidence that resistance to antibiotics is less of a problem when antibiotics are used sparingly, prescribing fewer antibiotics may be the only significant way to address the problem. According to several authorities as well as WHO, antibiotics must be restricted and inappropriate uses must be halted if the growing trend toward bacterial resistance to antibiotics is to be stopped or reversed.
ASTHMA—A CONSEQUENCE OF ANTIBIOTICS
The rate of asthma in children has doubled in the last 10 to 15 years. Why? In a combined analysis of seven studies involving more than 12,000 youngsters, researchers at the University of British Columbia found that those who had taken prescribed antibiotics before their first birthday were more than twice as likely as untreated kids to develop asthma. Among children who had multiple courses of antibiotics, the risk was even higher—it rose 16 percent for every course of the drugs taken before age one.22
Again, there is no question that antibiotics have their place in medicine—they definitely save lives. But here is my point: the majority of these kids may have developed asthma from antibiotics given to them for conditions (e.g., bronchitis, ear infections, and colds) against which antibiotics have not been shown to be effective.
There are a couple of explanations for this association between antibiotics and asthma. One is that antibiotics contribute to a state of “excess hygiene” leading to a reduced exposure to microbes, which in turn creates an oversensitive immune system mounting an over-the-top allergic reaction to pollen and dust mites, ultimately leading to asthma.
My feeling is that the underlying mechanism explaining a possible link between antibiotics and asthma is the negative effect of antibiotics on the normal flora in the gastrointestinal and respiratory passages, as I explained in the last chapter. Recent clinical studies have shown that taking probiotics (active cultures of beneficial bacteria such as Lactobacillus and Bifidobacteria species) lowers the risk of allergic diseases like asthma and eczema. These results definitely indicate that antibiotics actively raise the risk by wiping out these beneficial bacteria.
ANTIBIOTICS AND ACUTE BRONCHITIS
Over the past 20 years there have been several randomized controlled trials designed to assess the benefit of antibiotics in treating acute bronchitis. Despite sufficient data (now more than a dozen double-blind studies) showing no clinical benefit for antibiotics in acute bronchitis, these drugs are prescribed by 70 percent of doctors who encounter a patient presenting with acute bronchitis. This practice is also in direct conflict with the practice guidelines of the American College of Chest Physicians—the medical specialty that deals with bronchitis and other respiratory disorders.23 According to their most recent guidelines, “The widespread use of antibiotics for the treatment of acute bronchitis is not justified, and vigorous efforts to curtail their use should be encouraged.” Nonetheless, most doctors regularly prescribe an antibiotic for acute bronchitis even though it provides no benefit and does have significant risks. The risks include overgrowth of Candida albicans, disruption of normal gut microflora, and the possibility of developing antibiotic-resistant strains of bacteria.
Why do physicians prescribe antibiotics for acute bronchitis despite the scientific facts? This is a very good question. Apparently, in addition to wanting to offer some help, doctors have several misconceptions. For example, there are no data to support the use of antibiotics when a patient’s history is, “I’ve had a cough for a week, and now my phlegm has turned green.” Likewise, there are no data to support the use of antibiotics because of a fever in acute bronchitis, or in the hope of preventing a progression to pneumonia. Another reason why doctors prescribe antibiotics for acute bronchitis is that many patients believe only an antibiotic can cure it. This belief is perhaps best exemplified by the fact that 60 percent of eligible patients refused to enter one double-blind study because they felt that antibiotics were absolutely necessary.24 Given doctors’ and patients’ beliefs and expectations, it is little wonder that antibiotics continue to be prescribed for a condition whose course they will not alter and for which they are never warranted.
ANTIBIOTICS AND EAR INFECTIONS
The major reason for the use of antibiotics in childhood is the misguided belief that they are necessary to treat ear infections. A number of well-designed studies and detailed analyses have demonstrated that there were no significant differences in the clinical course of acute ear infections between children treated with antibiotics and children given a placebo.25, 26, 27 Interestingly, in some studies, children who did not receive antibiotics had fewer recurrences than children who received antibiotics. This result undoubtedly reflects the fact that antibiotics suppress the immune system and disturb the normal flora of the upper respiratory tract. Despite the data showing little, if any, benefit from antibiotics in treating ear infections, 98 percent of children with an ear infection in the United States are given an antibiotic.
FOOD ALLERGIES AND EAR INFECTIONS
The primary risk factors for ear infections include:
 Food allergies
Food allergies Exposure to secondhand smoke
Exposure to secondhand smoke Not being breast-fed
Not being breast-fed Day care
Day care Pacifiers
Pacifiers
All these factors can contribute to abnormal functioning of the eustachian tube, the underlying cause in virtually all cases of ear infections. The eustachian tube connects the middle ear to the back of the inner throat. It functions to regulate gas pressure in the middle ear, protects the middle ear from nose and throat secretions and bacteria, and clears fluids from the middle ear. Swallowing causes active opening of the eustachian tube due to the action of the surrounding muscles. Infants and small children are particularly susceptible to problems of the eustachian tube because at their age it is smaller in diameter and more horizontal.
Obstruction of the eustachian tube leads first to fluid buildup and then, if the bacteria present are pathogenic and the immune system is impaired, to bacterial infection. Obstruction results from collapse of the tube (due to weak tissues holding the tube in place, or to an abnormal opening mechanism, or to both), blockage with mucus in response to allergy or irritation, swelling of the mucous membrane, or infection.
The role of allergy as a major cause of chronic ear infections has been demonstrated in numerous studies, but for some reason it remains controversial in conventional medical circles.28, 29, 30, 31, 32 Studies have shown that 93 percent of children with ear infections have allergies: 16 percent to inhalants only, 14 percent to food only, and 70 percent to both. One way prolonged breast-feeding prevents ear infections may be by the avoidance of food allergies, particularly if the mother avoids sensitizing foods (i.e., those to which she is allergic) during pregnancy and lactation. In addition to breast-feeding, also of value is the exclusion or limited consumption of the foods to which children are most commonly allergic—wheat, egg, peanuts, corn, citrus, chocolate, and dairy products—particularly during the first nine months.
The allergic reaction causes blockage of the eustachian tube by two mechanisms: inflammatory swelling of the mucous membranes lining the tube, and inflammatory swelling of the nose, causing what is known as the Toynbee phenomenon (swallowing when both mouth and nose are closed, forcing air and secretions into the middle ear). In chronic ear infections, an allergy should always be considered as a possible cause, and any offending allergen should be identified and avoided. If that goal is achieved, the results are fabulous. For example, in one large study of children with chronic ear infections, after 12 months 92 percent improved when their allergies were identified and dealt with.31 In another study, the success rate was 78 percent.32 In contrast, the typical response with conventional medical treatment—antibiotics or surgical methods, including ear tubes and the removal of the tonsils and adenoids—is only about 50 percent.
WHAT’S A PARENT TO DO?
The point that I want to make here is that the best medicine is always prevention. Helping your child build a strong immune system is the primary goal. Breast-feeding for at least the first four months of life, avoiding food allergies and airborne irritants (such as cigarette smoke), and providing optimum nutrition are all very important in helping children develop greater resistance to infections. When illness does present itself, visiting a naturopathic physician for natural support should be the first step (please go to www.naturopathic.org to find an N.D. in your area).
In the treatment of acute ear infections, an eardrop preparation containing various herbal medicines was shown to be very effective in reducing pain and calming a crying child.33 In a double-blind trial with 171 children ages 5 to 18, eardrops containing a combination of extracts of marigold flowers (Calendula officinalis), St.-John’s-wort (Hypericum perforatum), and mullein flowers (Verbascum thapsus) in olive oil with the essential oil of garlic (Allium sativum) were given at a dose of five drops in the affected ear three times daily to the experimental group. This treatment was compared with the same dosage of an anesthetic eardrops containing amethocaine and phenazone. Other children were given either no antibiotic or amoxicillin. All the groups had a statistically significant improvement in ear pain over the course of three days, but the group getting the herbal eardrops without an antibiotic had the best response: a 95.9 percent reduction in their pain score. If the herbal eardrops were given with amoxicillin there was a 90.9 percent diminution of pain. The children given the anesthetic drops alone and with antibiotics had reductions of 84.7 percent and 77.8 percent, respectively. These data indicate that the topical treatment with herbal eardrops was the most effective.
ANOTHER EXAMPLE OF MORE HARM THAN GOOD
There are many effective alternatives to conventional drugs, but perhaps the best-known is the dietary supplement glucosamine sulfate in the treatment of osteoarthritis. Often, what is different about using such natural alternatives is that they truly promote the healing process rather than suppress symptoms. There is probably no better example than comparing the natural approach and the drug approach to osteoarthritis—the most common form of arthritis.
Osteoarthritis is characterized by a breakdown of cartilage. Cartilage has an important role in joint function. Its gel-like consistency provides protection to the ends of joints by acting as a shock absorber. Degeneration of the cartilage is the defining feature of osteoarthritis. This degeneration causes inflammation, pain, deformity, and limitation of motion in the joint.
Several studies have attempted to determine the natural course of osteoarthritis.34, 35 In other words, researchers have sought to determine what happens when people with osteoarthritis are given no treatment. One group of researchers studied the natural course of osteoarthritis of the hip over a 10-year period.35 At the beginning of the study, all subjects had X-rays suggestive of advanced osteoarthritis, yet the researchers reported marked clinical improvement over time. X-rays confirmed these improvements, including complete recovery in 14 of 31 subjects. These results, as well as others, raise the serious concern that medical intervention (i.e., drugs) may actually promote the progression of this disease.
KNEE SURGERY FOR OSTEOARTHRITIS IS NO BETTER THAN A PLACEBO
In a landmark study conducted by Baylor College of Medicine, a popular surgical treatment for osteoarthritis was shown to provide no real benefit.36 The procedure involves the use of an arthroscope, a pencil-thin viewing tube. With the arthroscope, worn, torn, or loose cartilage is cut away and removed (debridement); or the bad cartilage is simply washed away (lavaged). In the study, 180 patients with knee pain were randomized into three groups. One group received debridement; the second group underwent arthroscopic lavage; and the third group underwent simulated arthroscopic surgery—small incisions were made, but no instruments were inserted and no cartilage was removed.
During two years of follow-up, patients in all three groups reported moderate improvements in pain and ability to function. However, neither of the intervention groups reported less pain or better function than the placebo group. In fact, the placebo patients reported better outcomes than the debridement patients at certain points during follow-up. Throughout the two years, the patients were unaware of whether they had received real or placebo surgery.
In the United States, it is estimated that more than 650,000 arthroscopic debridement or lavage procedures are performed each year. At a cost of about $5,000 each, they represent roughly $3.25 billion. That is a lot of money, which could be put to better use than in a therapy that provides no real benefit to the patient.
DRUGS USED IN OSTEOARTHRITIS CAN PROMOTE JOINT DESTRUCTION
The primary drugs used in the treatment of osteoarthritis are the nonsteroidal anti-inflammatory drugs (NSAIDs). They include aspirin, ibuprofen, Aleve, Feldene, Voltarin, and the newer COX-2 inhibitor drugs such as Celebrex and Vioxx. These drugs are used extensively in the United States in the treatment of osteoarthritis, but research is indicating that they may be producing only short-term benefit and actually accelerating joint destruction and causing more problems down the road. These drugs are also associated with side effects, including gastrointestinal upset, headaches, and dizziness, and are therefore recommended for only short periods of time. In Chapter 1, I emphasized that although Celebrex and Vioxx came into prominence precisely to avoid the ulcers caused by anti-inflammatory drugs like aspirin and ibuprofen, after one year of use there was actually no difference between Celebrex and the older drugs ibuprofen and Voltaren with regard to the formation of ulcers. In light of the subsequent disclosures about Celebrex and Vioxx, and because it is estimated that more than 60,000 people may have died from side effects of these drugs, it seems that the drugs should never have been approved for use.
Vioxx Costs Merck Billions
When Merck Pharmaceuticals announced on September 20, 2004, that it was voluntarily withdrawing its arthritis medication Vioxx (which had been worth $2.5 billion a year) from the market because of the risk of heart attacks, it highlighted once again the failure of the FDA to adequately protect Americans from the greed and manipulation of the drug companies. It was not the loss of lives per se that was responsible for Merck’s withdrawing the drug and losing billions of dollars in revenues. Rather, it was probably a fear of the financial damages that a major class action law suit would inflict on Merck.
Merck’s executives were no doubt keenly aware of results of class action lawsuits involving the drug Baycol (cerivastatin), manufactured by the German drug company Bayer. This statin was shown to produce an often fatal destruction of muscle tissue (rhabdomyolysis) more than 20 times as frequently as other statin drugs. From the time Bayer became aware of the problem, one year elapsed before Baycol was removed from the market in August 2001; during that year there were 1,899 cases of rhabdomyolysis and at least 100 deaths. Bayer has paid $1.133 billion to settle 2,995 cases worldwide, and nearly 10,000 cases are still pending.
Can you imagine the deep concern the makers of Vioxx had when reports began to surface that COX-2 inhibitor drugs such as Vioxx and Celebrex might be linked to as many as 50,000 deaths in the United States alone? In the debacle over Baycol, Bayer paid on average $381,224 to each claimant. If family members of the victims of Vioxx received similar compensation, it would clearly bankrupt Merck, especially in light of the fact that Merck apparently was aware of the potential link between Vioxx and heart attacks. The removal of Vioxx from the market was mainly an attempt by Merck to reduce its liability. Even so, by March 2006, more than 10,000 cases and 190 class actions were filed against Merck, involving adverse cardiovascular events associated with Vioxx and the inadequacy of Merck’s warnings. In the first case to go all the way to trial, on August 19, 2005, a jury in Texas voted 10 to two to hold Merck liable for the death of Robert Ernst at age 59. The jury awarded his wife, Carol Ernst, $253.4 million in damages. But she will have a tough time getting that money, as Merck will appeal and fight this case and any other case it might lose. Merck has set aside nearly $1 billion to pay for legal expenses related to Vioxx.
One side effect of these NSAIDs that the drug companies won’t tell you about and your doctor doesn’t know about is that they can actually promote joint destruction and inhibit cartilage repair by inhibiting the formation of key compounds in cartilage, the glycosaminoglycans (GAGs).37 These compounds are responsible for maintaining the proper water content in the cartilage matrix, thereby helping cartilage remain gel-like and continue to absorb shock. Clinical studies have shown that NSAIDs are associated with acceleration of osteoarthritis and increased joint destruction.38, 39, 40, 41 Simply stated, aspirin and other NSAIDs appear to suppress the symptoms but accelerate the progression of osteoarthritis. They are designed to fight disease rather than promote health.
GLUCOSAMINE SULFATE IN THE TREATMENT OF OSTEOARTHRITIS
Glucosamine is a simple molecule that can be manufactured in the body. In joints, the main function of glucosamine is to stimulate the manufacture of glycosaminoglycans (GAGs), structural components of cartilage. Evidently, as some people age they lose the ability to manufacture sufficient levels of glucosamine. The result is that cartilage loses its capacity to act as a shock absorber. The inability to manufacture glucosamine has been suggested as the major factor leading to osteoarthritis—the most common form of arthritis, characterized by joint degeneration and loss of cartilage.
The most thoroughly researched form of glucosamine is glucosamine sulfate. This form has been the subject of more than 300 scientific investigations and at least 20 double-blind studies. Glucosamine sulfate has been used by millions of people worldwide, has no known toxicity in humans, and is registered as drug in the treatment of osteoarthritis in some 70 countries.42, 43, 44
The medicinal use of glucosamine sulfate in the treatment of osteoarthritis is consistent with the philosophy and practice of naturopathic medicine because of its action in facilitating the body’s natural healing process. The clinical benefits of glucosamine sulfate in the treatment of osteoarthritis are impressive. In comparative studies it has been shown to provide greater benefit than NSAIDs such as ibuprofen and piroxicam (Feldene). Although side effects are common (even expected) with these drugs, glucosamine sulfate does not cause side effects. One popular misconception that I have heard from both doctors and consumers is that glucosamine sulfate raises blood sugar levels. It is true that according to test-tube studies glucosamine can interfere with glucose metabolism. But, the concentrations used in these test-tube studies were 100 to 200 times higher than tissue levels that can be reached with oral supplementation. When researchers went back and reviewed clinical trials involving more than 3,000 subjects, they found that fasting blood sugar levels actually decreased slightly with use of glucosamine sulfate.44
In studies comparing glucosamine sulfate with ibuprofen, piroxicam (Feldene), or acetaminophen, results have shown glucosamine sulfate was more effective in relieving pain (though it does not have any direct analgesic effect) and was without significant side effects. In fact, subjects on glucosamine sulfate had fewer side effects than subjects in the placebo, and there were no dropouts in the glucosamine sulfate group. In contrast, many of the subjects taking NSAIDs had side effects and dropped out because these side effects are so severe.
In summary, whereas NSAIDs and acetaminophen offer only symptomatic relief in osteoarthritis and may actually promote the disease process, glucosamine sulfate appears to address one of the underlying factors that can cause osteoarthritis—reduced manufacture of the components of cartilage. Clinical studies have now confirmed that glucosamine sulfate can actually thicken cartilage, thereby restoring its shock-absorbing qualities. By getting at the root of the problem, glucosamine sulfate not only improves the symptoms, including pain, but also helps the body repair damaged joints. The treatment of osteoarthritis is just one instance in which a more natural approach produces better results and does so without side effects.
Case History: The Plumber’s Helper
Jack, a 56-year-old plumber, could barely walk into my office because his knee hurt so much. He told me that he had dragged himself in because he had read an article I had written on the value of glucosamine sulfate over NSAIDs in the treatment of osteoarthritis.
Jack had learned firsthand how destructive these drugs can be. About 10 years before, he started developing osteoarthritis in his left knee. His medical doctor first offered a prescription for ibuprofen (Motrin). When that didn’t work, the doctor prescribed more potent NSAIDs, including Voltaren and Feldene. In the 10 years he had taken these drugs, Jack’s arthritis got worse. Adding insult to injury, a severe ulcer developed in his stomach.
Two weeks before coming to me, Jack had been hospitalized because his ulcer was bleeding. Because his stomach was so bad, he had to stop taking Feldene. When he stopped, his knee hurt worse than ever. The acetaminophen (Tylenol) his doctor now prescribed was not working. Jack grew desperate and began looking into other options. That’s when he read my article about natural alternatives for dealing with osteoarthritis, but he was such a skeptic that he wanted to hear it directly from the horse’s mouth. He simply could not imagine that treating osteoarthritis could be as simple as I professed. I told him that it did not matter if he believed that glucosamine sulfate would work or not—I knew it would. Jack agreed to try.
When he returned six weeks later, he was ecstatic. He was doing deep knee bends and hopping up and down on his left leg to show me how good he felt. He said it was a miracle. He felt so good that the day before he had gone to his medical doctor’s office to show off his progress with glucosamine sulfate. His doctor said it was nothing more than a placebo response. Jack had replied, “Doc, if it was just a placebo, then why didn’t you prescribe it to me ten years ago instead of giving me all of those damn drugs?” I think Jack had a good point.
Jack came to see me in 1995, when glucosamine sulfate was just hitting the market. Most doctors at the time were not familiar with the science behind glucosamine sulfate. So, I sent Jack’s doctor a packet of information on glucosamine sulfate, including reports on several of the double-blind, placebo-controlled trials. A week later I received a very nice letter from the doctor. He thanked me and stated that he was unaware of all the double-blind studies supporting the efficacy of glucosamine sulfate. He was also surprised to learn that glucosamine sulfate is an approved medicine in more than 70 countries and has been used successfully by millions of people worldwide. My experience is that most conventional medical doctors appreciate learning about safe and effective tools that can help their patients.
FINAL COMMENTS
So, is relieving symptoms a path to bad medicine? My answer to this question is yes, but with some clarification. Relief of symptoms should be a major therapeutic goal, but it should not come at the price of doing more harm than good. Whether relief of symptoms is good or bad is determined by whether the treatment simply suppresses the symptoms or eliminates the underlying factors that are producing them. Symptoms are often whistle-blowers, alerting us to deeper issues. The whistle-blower is silenced, but this does not necessarily mean that the deeper issue has been taken care of. Think of a fire alarm: if you simply turn it off, the fire may burn out of control. Don’t underestimate the wisdom of your body or its ability to sense when something is not right. Symptoms often provide us with valuable information so that we can make changes that will lead to better health.