Afterword
When I was educated at Stanford I was not exposed to family practice, so it took me a number of years to discover it and recognize the benefits of the approach. Throughout my practice and in my personal life I encountered the need to advocate for the patient and the family. The system often makes unintended mistakes. We all know this, so it is necessary for doctors and family alike to be vigilant and intervene if necessary. No one knows the patient better than the family. The integration of the family into medical care is not a conflict but leads to enhanced care. Skilled physicians know this and are comfortable integrating the observations of family members into the care, whereas insecure physicians may find this threatening.
Good medical care involves thinking about the patient in the context of their life. Creative integration and experimentation with a variety of modalities—such as alternative therapies—will lead to the best outcomes. I often struggled to have this approach considered as part of care, as such “soft” and “unscientific” approaches are out of the experience of many conventional medical practitioners. I learned very early in training and practice, and in the care of Bonnie, that doctors need to be modest in what they believe about their contribution to cure.
I realize that my experiences in Ethiopia and Mexico were unusual and life altering—rare for medical students caught in the rigid structure of usual medical training. I was fortunate to have a medical school dean who was flexible enough to allow me the time to follow my passion. These experiences made me a better doctor and provided me with skills that most students never develop. More of this kind of flexibility in medical education is needed.
Now that I no longer see patients clinically, I remain engaged in medical issues and continue to teach research methodology to family practice residents, and clinical and research skills to midwifery students.
It was hard for me to stop seeing patients in my family practice—especially maternity care, my central area of passion, but in the end, I found that I was concerned about maintaining the quality of my practice. In my late sixties, I found the long sleepless nights increasingly difficult. It took me many days to recover from an all-nighter. My experience reflects the natural fraying at the edges that all older doctors experience—but I miss it.
Continuing as the listmaster of the Maternity Care Discussion Group (MCDG) helps keep me current. It is the only multidisciplinary maternity discussion group worldwide and a unique forum for obstetricians, family physicians, maternity nurses, midwives and doulas to share clinical experiences and solve problems—even political problems. Such a self-help discussion group is a model of non-territorial inter-professional cooperation. To join the list, contact me at mklein@mail.ubc.ca.
Maternity care is under stress around the world as medicalization of childbirth continues to accelerate, while society and professionals alike increasingly see childbirth as just an opportunity for things to go wrong. Fortunately, there are movements in the other direction. Women are driving this movement, insisting that the control of childbirth remain in the hands of the women having babies.
This is the current version of the earlier movement to “humanize” childbirth by getting partners into the delivery room and limiting unnecessary procedures. The movement toward normal physiological childbirth, though historically necessary, cannot easily go against current trends, but determined consumers are having an impact in some settings. Although midwives provide excellent one-to-one clinical care, they will also need to enter the political arena, with their natural allies, to maximize their impact on overall maternal health.
Increasing the midwifery resources to be able to care for appropriate low-risk women for birth in hospital and at home, and increasing the number of family doctors who include birth in their practice, will result in the need for fewer obstetricians. The obstetricians will then provide only the complex care needed for selected patients on referral from midwives and family doctors.
To rationalize maternity care, ministries of health and ministries of education will need to plan together how many of what type of provider will be required—and who will train them and where they will be trained. This is a tall order but becoming more possible as the system fails and women are finding it increasingly difficult to obtain the right care from their chosen provider. The pressure to plan for the future will become more and more clear, and serious discussions about how to care for pregnant women will have to take place at the highest governmental levels.
This evolving process also finds resonance among those who are paying the bills, including insurance companies, health authorities and even national health care schemes. The time may be right for a major change in how maternity care is provided, but it will take an enormous commitment from many players to realize what is best for childbearing women. If successful, the paradigm of childbirth as a disease may shift to a view of childbirth as a transformative, growth-promoting and joyous happening.
The earlier portion of my career and practice involved many areas, including public health and international health. So why did I focus so heavily on maternity care? For me, it was a natural evolution. My rather backward path from being a pediatrician/neonatologist to a family physician allowed me to see this area of care from several perspectives. My unique training and experience allowed me to operate at the interface of pediatrics, newborn intensive care, obstetrics, nursing, midwifery and family practice. Here, I felt I would make my greatest contribution in practice, training and research.
Maternity care, however, provides a window on the values of a society, just as, in a bizarre way, episiotomy provided a vehicle to traverse and understand a complex birth system. What do we feel is important as a society? How do we think about the future of society, the role of women, the value of children? Although I moved more and more from a general family practice to one focused mainly on birth, I nevertheless stayed committed to seeing birth in the context of society.
When birth is seen primarily as an expensive, unpredictable and dangerous event, birth and those who provide birth care will be sidelined. Hospitals and health authorities will download the care of pregnant women to large centralized hospitals where well-meaning strangers will do their best to care for women they do not know. This dystopic picture is well underway, while some attempts to slow or stop the trend are also happening. How this struggle will resolve remains to be seen.
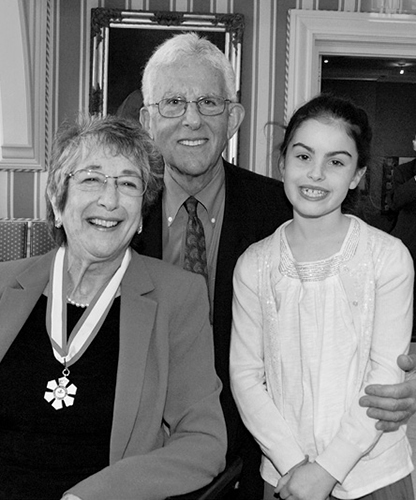
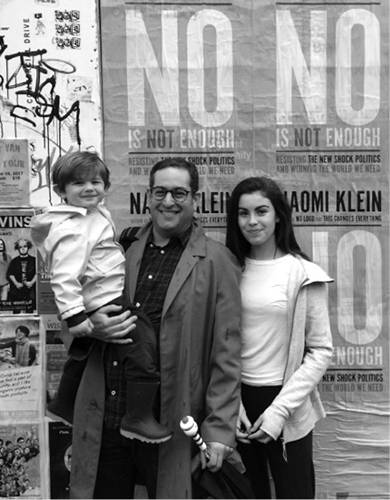
Although I still engage with maternity care at several levels, it is time to focus more on children and grandchildren and the outdoors, and worry more about the planet and the world that we are leaving for them.