CHAPTER 14 Painful Periods
Painful Periods indicates menstrual pain that occurs before, during or after menstruation. The pain may occur in the lower abdomen or sacral region and sometimes extend to the legs. In severe cases, there may be nausea and vomiting or even fainting.
The Liver, Penetrating Vessel and Directing Vessel are responsible for the physiology of menstruation. For a normal period to occur, Blood must be abundant and move adequately. Proper movement of Blood relies on the free flow of Liver-Qi and of the Qi of the Penetrating Vessel.
As we have seen in Chapter 2 on physiology, four different phases may be identified in each menstrual cycle. During the pre-menstrual phase, Yang rises and Liver-Qi moves in preparation for moving Blood during the period. Thus, a proper movement of Liver-Qi and Liver-Blood is essential for a pain-free period. If Liver-Qi stagnates, it may cause pain, especially before the period, while if Liver-Blood stagnates, it causes pain during the period. Stagnation is therefore the most important pathological condition causing painful periods: even in deficiency conditions when the pain is mild, it is some element of stagnation that causes it.
The earliest mention of Painful Periods is probably in the Synopsis of Prescriptions of the Golden Cabinet which says: “If a woman has irregular periods with abdominal pain and fullness, and the periods are irregular, use Tu Gua Gen Powder”.1
Another passage in the same book appears to describe an episode of severe dysmenorrhoea from Cold:
When Cold invades the Lower Burner the menses may become scanty and painful with a dragging pain in the vagina and a feeling of cold in the abdomen … there is an acute pain on Qichong [ST-30] … there may be sudden vertigo and the woman may pass out … this is a gynaecological problem and is not due to an attack of evil spirits …2
Aetiology
Emotional strain
Emotional strain is a very important aetiological factor in painful periods. Anger, frustration, resentment, worry and guilt all may lead to Liver-Qi stagnation. In women, Liver-Qi stagnation causes Blood to stagnate in the Uterus leading to painful periods. In some cases, stagnant Liver-Qi may turn into Liver-Fire and this, in turn, may lead to Blood-Heat. Blood-Heat often combines with Damp-Heat in the Uterus.
External Cold and Dampness
Excessive exposure to Cold and Dampness, especially during the puberty years, may cause Cold to invade the Uterus. Cold contracts and causes stasis of Blood in the Uterus and therefore painful periods. In cold and damp countries where young girls dressed in shorts play school sports and games, this is a very common cause of painful periods. During puberty, the body is in a vulnerable state because it is undergoing profound changes, and it is therefore very likely to be affected by pathogenic factors. Invasion of Cold in the Uterus is the most common cause of painful periods in adolescent girls.
Women are also prone to invasion of Cold in the Uterus during and soon after the period when the Uterus and Blood are in a relatively weakened state. At this time, therefore, they should take particular care not to be exposed to cold and dampness. Fu Qing Zhu says:
The Liver pertains to Wood, it stores Blood and it hates wind and cold most of all. During menstruation the space between skin and muscles (cou li) is wide open, when this is invaded by wind and cold Liver-Qi stagnates and the passages of the menses become obstructed.3
Women with a pre-existing condition of Yang deficiency are obviously more prone to invasion of external Cold.
Overwork, chronic illness
Physical overwork or a chronic illness leads to deficiency of Qi and Blood, especially of Stomach and Spleen. Deficiency of Blood leads to malnourishment of the Penetrating and Directing Vessels so that the Blood has no force to move properly thus causing stagnation and pain.
Excessive sexual activity, childbirth
The Liver and Kidneys are weakened by excessive sexual activity (which affects women somewhat less than men), too many childbirths too close together, and sexual activity starting too early. A deficiency of Liver and Kidneys induces Emptiness of the Penetrating and Directing Vessels so that they cannot move Qi and Blood properly, thus causing painful periods.
Pathology
Thus, stagnation of Qi and/or Blood, which may arise by itself or be caused by Cold in the Uterus, is the most important factor in painful periods. Even deficiency types of painful periods, caused by Blood or Liver/Kidney deficiency, involve an element of stagnation as the deficient Blood fails to move properly.
The main patterns causing Painful Periods are therefore:
Stagnation of Qi and stasis of Blood are very common patterns occurring in Painful Periods. They very often accompany other patterns. For example, a deficiency of Qi and Blood may occur in combination with some stagnation of Qi and/or Blood. Similarly, Cold obstructing the Uterus obviously leads to stasis of Blood. In gynecology, stagnation of Qi and of Blood is always related to the Liver and the Penetrating Vessel.
A free-flowing Liver-Qi is essential to move Blood before and during the period; if Liver-Qi stagnates, Blood does not move properly and pain results. The Penetrating Vessel is also usually involved in painful periods from stagnation as it is the Sea of Blood and it flows through the Uterus: for this reason, stasis of Blood in the Uterus is often due to stagnation in this vessel. Of all the extraordinary vessels, the Penetrating Vessel is the most important one in the pathology of Painful Periods.
When the periods are painful from stagnation of Qi, the pain is accompanied by a pronounced feeling of distension of the abdomen, typically occurring especially before the periods. Other symptoms may include pre-menstrual tension, irritability, depression and a Wiry pulse. Many books list a Purple tongue as a sign of Qi stagnation: I tend to disagree as the tongue-body colour reflects more the state of Blood than Qi so that, if it is Purple, I relate that to Blood rather than Qi stagnation. In Qi stagnation, the tongue-body colour may be normal, except in severe and longstanding cases when it may be Red on the sides.
Stagnation of Liver-Qi is often secondary to or accompanied by Liver-Blood stasis (as discussed at length in Chapter 3 on pathology): when this is the case, the pulse may not be Wiry at all but Fine or Choppy (and perhaps slightly Wiry on one side) and the tongue may be Pale (from Blood deficiency).
When stasis of Blood is predominant, the pain is more intense, is stabbing in character and is typically relieved by the passing of dark clots. A dark menstrual blood with clots is an essential and sufficient symptom to diagnose stasis of Blood, i.e. by itself it validates a diagnosis of Blood stasis, even if there are no other indications. Another important sign is a Purple colour of the tongue body although, if the stasis of Blood is fairly recent and not too severe, the tongue may not show this sign. Another symptom of Blood stasis is that the period may be hesitant, i.e. it may start and stop.
Stagnation of Cold is a common cause of Painful Periods especially in young girls living in cold and damp countries. With stagnation of Cold, there is always stasis of Blood as Cold obstructs the Uterus and the vessels preventing a proper flow of blood. It is for this reason that with Cold, too, there are clots in the menstrual blood: however, if Cold is the cause, the menstrual blood is typically red and the clots are dark and rather small or stringy, whereas if stasis of Blood is the cause, the blood itself is dark and the clots are rather large. The pain from stagnation of Cold is very intense and cramping in character and typically alleviated by the application of heat.
Blood-Heat does not usually cause intense menstrual pain; often associated with Damp-Heat (for this reason these two pathogenic factors will be discussed together), it tends to make the periods heavy. Other symptoms include a feeling of heat, thirst, a Red tongue and a Rapid pulse. If Damp-Heat is present, there will also be a feeling of heaviness, an excessive vaginal discharge, a bearing-down sensation, a sticky-yellow coating on the tongue and a Slippery pulse.
Deficiency of Qi and Blood and Liver and Kidneys usually causes only mild menstrual pain. The latter pattern is seen more in older women. As mentioned before, even in Empty conditions there is some element of stagnation as deficient Qi and Blood fail to move Blood properly and this leads to some stagnation. In fact, Zhang Jing Yue in the Complete Works of Jing Yue (1624) says:
In women with painful periods, in many cases there is an intrinsic Deficiency and purely Excess types are few … when Qi and Blood are deficient Blood does not move … Qi is deficient and Blood stagnates.4
Diagnosis
Time of onset
Pain before and during the period is usually of the Full type, while pain after the period is of the Empty type.
Pressure
If the pain is made worse by pressure, it indicates Fullness, while if the patient gets relief from pressing the lower abdomen, it indicates Emptiness. Patients are not sure how to answer this question if it is not asked in a sensible way. Thus, instead of enquiring whether the “pain is better with pressure or not”, we should ask the patient whether she perhaps likes to hold her abdomen or whether she dislikes to be touched on the abdomen at that time. Women often find that a hot-water bottle on the abdomen relieves the pain, but sometimes they like the pressure rather than the heat of the bottle.
Heat-Cold
If the pain is relieved by the application of heat (such as a hot-water bottle), it indicates either a Cold condition or stasis of Blood from Cold. It should be kept in mind, however, that this sign is not always indicative of Cold, as other conditions, such as stagnation of Qi or Blood, may also be alleviated by the application of a hot-water bottle. Furthermore, a sensation of heat is often comforting in itself without really indicating that the pain is due to Cold. If the pain is aggravated by heat, it indicates Blood-Heat.
Cycle
If the cycle is long (i.e. the periods come consistently late) and the menstrual blood is dark and clotted, it indicates stasis of Blood. If the menstrual blood is red with small dark clots, it indicates Cold in the Uterus.
If the cycle is short, the period heavy and the blood bright red, it indicates Blood-Heat.
Treatment principles
From the point of view of Manifestation (Biao) the central pathology of Painful Periods is a disharmony of the Penetrating Vessel and Sea of Blood. Hence the main principle of treatment for the Manifestation is to regulate the Qi and Blood of the Penetrating Vessel. As discussed in Chapter 3 on pathology, the Penetrating Vessel is the Sea of Blood. It arises from the Uterus and is therefore always involved in Painful Periods. This vessel is particularly prone to stagnation of Qi and Blood in the abdomen and many of its points (especially KI-14 Siman) eliminate stagnation. The Qi of the Penetrating Vessel is prone to rebel upwards from the abdomen towards the chest giving rise to a feeling of oppression of the chest.
Since this vessel is also closely related to the Bright-Yang channels via the important point ST-30 Qichong, a stagnation in the Penetrating Vessel often causes Qi to rebel in the Bright Yang: this explains the nausea and vomiting experienced by some women suffering from painful periods. To treat stasis of Blood in the Penetrating Vessel, I often use the vessel’s opening points, i.e. SP-4 Gongsun on the right and P-6 Neiguan on the left together with other points on the vessel such as KI-14 Siman, KI-12 Dahe or KI-16 Huangshu.
Other points related to the Penetrating Vessel in treating painful periods are LIV-3 Taichong, ST-42 Chongyang and ST-30 Qichong. LIV-3 Taichong is the most important one to affect the Penetrating Vessel: by moving Liver-Qi, it regulates the Penetrating Vessel, subdues its rebellious Qi and invigorates Blood. The association between this point and the Penetrating Vessel is so close that sometimes the old classics call this vessel Taichong. In fact, the very first chapter of the Simple Questions, in describing the 7-year cycles of women, says: “At 14, the Heavenly Gui arrives [i.e. the menses], the Directing Vessel is open and the Taichong vessel is flourishing.”5 The ‘Taichong vessel’ is the Penetrating Vessel. ST-42 Chongyang also regulates Blood within the Penetrating Vessel and eliminates stasis due to the relationship between this vessel and the Bright Yang. ST-30 Qichong is one of the most important points on the Penetrating Vessel and strongly moves Qi and Blood in the abdomen. Its other name, Qijie, means ‘avenues of Qi’, referring to the channels and vessels of the abdomen which the Penetrating Vessel influences.
To treat the Root in Painful Periods, one must differentiate clearly between Heat, Cold, deficiency and excess. First identify the prevailing pattern, then treat it in order to treat the Root: this may involve moving Qi, invigorating Blood, expelling Cold, resolving Dampness, clearing Heat, tonifying Qi and Blood or strengthening Liver and Kidneys.
The most important differentiation is that between Full and Empty types of painful periods. Full types are much more common than Empty, and clinically are more important as they are characterized by more intense pain. Moreover, even in Empty types of painful periods there is an element of stasis of Blood as deficient Blood fails to move properly. For this reason, even for Empty types of painful periods, some Blood-moving herbs are added to the prescription used.
The treatment principle is often changed according to the time of the menstrual cycle. During the period one concentrates on treating the Manifestation, i.e. invigorate Blood and stop pain. At other points in the cycle one treats the Root, i.e. according to the main pattern. A deficiency, in particular, is best treated during the 2 weeks, or thereabouts, that follow the period.
Identification of patterns and treatment
Full conditions
Stagnation of Qi
Clinical manifestations
Lower abdominal pain during the period, or 1 to 2 days before the period, a pronounced feeling of distension of the abdomen and breasts, hesitant start to the period, menstrual blood dark without clots, pre-menstrual tension and irritability. Tongue: Normal coloured or slightly Red on the sides. If there is deficiency of Blood, the tongue may be Pale. Pulse: Wiry. The pulse may be Choppy if Liver-Blood deficiency predominates.
Acupuncture
LIV-3 Taichong, Ren-6 Qihai, G.B.-34 Yanglingquan, SP-8 Diji, ST-29 Guilai, SP-10 Xuehai, SP-6 Sanyinjiao, SP-4 Gongsun and P-6 Neiguan, SP-14 Fujie. Reducing or even method.
Herbal treatment
Women’s Treasure remedy
This remedy is a variation of the formula Xiao Yao San Free and Easy Wanderer Powder which pacifies the Liver, moves Qi, eliminates stagnation, nourishes Liver-Blood and tonifies Spleen-Qi. The formula has been adapted with the addition of herbs that move Qi and stop pain. The tongue presentation appropriate to this remedy is a normal-coloured body or slightly Pale on the sides; if the stagnation of Qi is severe, it could be slightly Red on the sides.
Stagnation of Qi
Lower abdominal pain during the period, or 1 to 2 days before the period, a pronounced feeling of distension of the abdomen and breasts, hesitant start to the period, menstrual blood dark without clots, pre-menstrual tension and irritability. Tongue: Normal coloured or slightly Red on the sides. If there is deficiency of Blood, the tongue may be Pale. Pulse: Wiry. The pulse may be Choppy if Liver-Blood deficiency predominates.
A 32-year-old woman had been suffering from painful periods for 2 years. The pain occurred during the period in the hypogastrium, lateral abdomen and sacrum. It was dull in character and associated with a bearing-down sensation. Her periods were regular and the menstrual blood was slightly dark with a few clots. She also suffered from pre-menstrual tension with a pronounced distension of breast and abdomen and irritability. She had been on the contraceptive pill for 10 years and the periods became painful when she stopped taking it. She had been given a progesterone pill but this had not helped the dysmenorrhoea at all. Apart from the menstrual problems, she also suffered from the so-called irritable bowel syndrome causing her a spastic pain in the abdomen and alternation of constipation and diarrhoea: she had had this problem for 10 years. On interrogation, it transpired that her vision was sometimes blurred, she was occasionally dizzy and experienced tingling of the limbs. Her tongue was slightly orangey on the sides, and her pulse was Fine on the right side and Fine but also slightly Wiry on the left.
Diagnosis
This is a very clear example of stagnation of Liver-Qi associated with (or caused by) Liver-Blood deficiency. The symptoms of Liver-Qi stagnation are very obvious: pre-menstrual tension with distension and irritability, painful periods, Wiry pulse on the left, abdominal pain with constipation and diarrhoea. The symptoms of Liver-Blood deficiency are also equally clear: the dull character of the menstrual pain, the blurred vision, the tingling and dizziness, the orangey colour of the sides of the tongue and the Fine pulse. I am inclined to think that, in this case, stagnation of Liver-Qi derived from Liver-Blood deficiency and this was, in turn, probably caused by the contraceptive pill.
Treatment principle
This patient was treated with acupuncture and herbal remedies. The acupuncture points used were selected from the following:
An example of a point combination in one treatment would be: LU-7 (on the right) and KI-6 (on the left), L.I.-4 on the left, LIV-3 on the right, Ren-4, ST-36 and SP-6 bilaterally; the last three points with reinforcing method, the others with even method.
The herbal remedies used were the Three Treasures’s Brighten the Eyes to nourish Liver-Blood and Freeing the Moon to pacify the Liver and eliminate stagnation. The latter remedy (a variation of Xiao Yao San Free and Easy Wanderer Powder) also nourishes Liver-Blood, and, in addition, pacifies Liver-Qi and tonifies Spleen-Qi. The patient took Brighten the Eyes for 2 weeks after the period and Freeing the Moon from then until the beginning of the next period.
This patient reacted exceedingly well to the treatment, improving even after the first session. After only three acupuncture sessions (over a period of 1 month) and use of the remedies, she reported experiencing no menstrual pain with her last period and no abdominal bowel pain, and feeling very much better in herself. Such a quick reaction is rather unusual as it normally takes at least 3 monthly cycles to affect a menstrual irregularity.
Stasis of Blood
Clinical manifestations
Intense, stabbing pain before or during the period, dark menstrual blood with large clots, mental restlessness, pain relieved after passing clots. Tongue: Purple. Pulse: Wiry.
Acupuncture
LIV-3 Taichong, Ren-6 Qihai, G.B.-34 Yanglingquan, SP-8 Diji, ST-29 Guilai, SP-10 Xuehai, SP-6 Sanyinjiao, SP-4 Gongsun and P-6 Neiguan, BL-17 Geshu, KI-14 Siman, ST-25 Tianshu. All with reducing or even method.
Explanation
Herbal treatment
c Prescription
d Prescription
e Prescription
Women’s Treasure remedy
This remedy is a variation of Ge Xia Zhu Yu Tang and it invigorates Blood in the Uterus and Lower Burner. The tongue presentation appropriate to this remedy is a Purple body.
Stasis of Blood
Intense, stabbing pain before or during the period, dark menstrual blood with large clots, mental restlessness, pain relieved after passing clots. Tongue: Purple. Pulse: Wiry.
LIV-3 Taichong, Ren-6 Qihai, G.B.-34 Yanglingquan, SP-8 Diji, ST-29 Guilai, SP-10 Xuehai, SP-6 Sanyinjiao, SP-4 Gongsun and P-6 Neiguan, BL-17 Geshu, KI-14 Siman, ST-25 Tianshu. All with reducing or even method.
A 29-year-old woman had been suffering from painful periods ever since the menarche. The pain occurred during the period and the menstrual blood was dark with some clots. The period started hesitantly and there was not much distension. The pain was alleviated by the application of a hot-water bottle.
She also suffered from thrush with itching of the vagina and a white, sticky discharge. She felt generally tired and her stools were loose. She had a lower backache, her memory was poor and she felt always cold. Her tongue was Pale and her pulse was Weak on the Liver and right Kidney positions and slightly Slow (68).
Diagnosis
My diagnosis was painful periods from mild stasis of Blood occurring against a background of Liver and Kidney deficiency (the tiredness, cold feeling, backache, poor memory and tongue and pulse all pointed to the latter). Besides this, she also suffered from Spleen deficiency (loose stools) and Dampness in the Lower Burner (vaginal itching and discharge).
Treatment principle
This case is given here as an example of adopting the wrong principle of treatment. As I came to the conclusion that the main aspect of the condition was a deficiency (of Liver, Kidneys and Spleen) with only a mild and secondary excess (stasis of Blood and Dampness in the Lower Burner), I adopted the principle of tonifying and warming the Kidneys and nourishing the Liver.
Explanation
The first eight herbs constitute a variation of You Gui Wan to tonify and warm the Kidneys and nourish the Liver.
After 10 packets of this decoction, she was no better at all. I therefore reassessed the diagnosis and principle of treatment and came to the conclusion that, although there was a pronounced deficiency, it would be better to eliminate pathogenic factors first. I did this by giving her first 10 packets of a decoction to resolve Dampness, and then 10 packets of a further decoction to invigorate Blood and eliminate stasis. The first decoction was a variation of Si Miao San Four Wonderful Powder:
Explanation
The first four herbs represent the Si Miao San.
She improved considerably after this decoction which was then followed by a variation of Ge Xia Zhu Yu Tang Eliminating Stasis below the Diaphragm Decoction to invigorate Blood and eliminate stasis:
This is a variation of Ge Xia Zhu Yu Tang with the addition of Bai Zhu to tonify the Spleen and Tu Si Zi to tonify the Kidneys and the removal of Mu Dan Pi Cortex Moutan, too cooling for her condition.
After 20 packets of this decoction, she was much better and her periods were painless. Even though neither of the above two formulae is tonifying, she had more energy. After 20 packets of this last decoction, the treatment principle reverted to the original one of tonifying Kidneys and Liver with You Gui Wan. This time, she felt well on it.
This case history is given to illustrate the importance of adopting a correct principle of treatment: even if the diagnosis is correct, adoption of the wrong principle of treatment will not yield results. This case also shows the importance, in mixed excess and deficiency conditions, of eliminating pathogenic factors before tonifying: this approach is particularly important when herbs are used, less so if only acupuncture is used.
Stagnation of Cold
Clinical manifestations
Lower abdominal pain before or after the period, pain central, pain relieved by the application of heat, menstrual blood rather scanty and bright red with small, dark clots, feeling cold, sore back. Tongue: Pale-Bluish or Bluish-Purple. Pulse: Deep and Choppy or Deep and Wiry.
Acupuncture
LU-7 Lieque (on the right) and KI-6 Zhaohai (on the left), Ren-4 Guanyuan, Ren-6 Qihai, ST-29 Guilai, KI-14 Siman, SP-8 Diji, SP-6 Sanyinjiao, ST-36 Zusanli, ST-28 Shuidao. Reducing method except on ST-36 which should be reinforced. Moxa must be used.
Explanation
Herbal treatment
Empty-Cold
a Prescription
This is a famous formula from the Synopsis of Prescriptions from the Golden Cabinet by Zhang Zhong Jing (AD 220), which is primarily for Cold obstructing the Uterus. The rationale behind it is as follows. When Cold obstructs the Uterus, it makes Blood stagnate. When Blood stagnates, new Blood has nowhere to go and it cannot be contained in the Uterus: this induces a deficiency of Blood. A longstanding Blood deficiency may give rise to some Empty-Heat signs, which may mistakenly be interpreted as Heat signs; but the Pale-Purple colour of the tongue clearly indicates that this is not so. In fact, the original text refers to a parched mouth and lips as the symptoms of Empty-Heat from Blood deficiency.10 When used for its proper pattern of longstanding internal Cold occurring against a background of deficiency and leading to stasis of Blood, this formula is very effective. An essential sign for its use is that the tongue-body colour be Pale or Bluish-Purple.
b Prescription
Compared with the previous formula, this is more warming and more tonifying. It is therefore suitable if there is a more pronounced Kidney-Yang deficiency, while the former is better if there is a Blood deficiency. The two formulae are similar in action. The main difference between them is that the former, Wen Jing Tang, which addresses the situation when the deficiency of Blood is a consequence of Cold obstructing the Uterus, is applicable for a deficiency of Blood and Yin with some symptoms of Empty-Heat such as a malar flush and a feeling of heat; the latter, Ai Fu Nuan Gong Wan, is used when a deficiency of Kidney-Yang and Blood leads to internal Cold.
c Prescription
This prescription is from Fu Qing Zhu’s Gynaecology. It is for long-term retention of Cold and Dampness in the Uterus leading to deficiency of Qi and Yang and painful periods. Fu Qing Zhu says:
Some women have pain below the umbilicus 3–5 days before the period, the pain is stabbing and the period is like black-bean juice … who would say that this is due to Cold and Dampness in the Lower Burner! … The Directing and Penetrating Vessels are in the Lower Burner, the Penetrating Vessel is the Sea of Blood and the Directing Vessel controls the Uterus and is the Blood Chamber … the menses spring from these two vessels, when these are obstructed by Cold and Dampness a struggle between these two causes pain; the pathogenic factors are victorious and the Upright Qi declines. Cold generates turbidity and, because of this, the menstrual blood looks like black-bean juice. The treatment must be aimed at resolving Dampness and expelling Cold [with warm herbs] to eliminate the pathogenic factors from the Directing and Penetrating Vessels.11
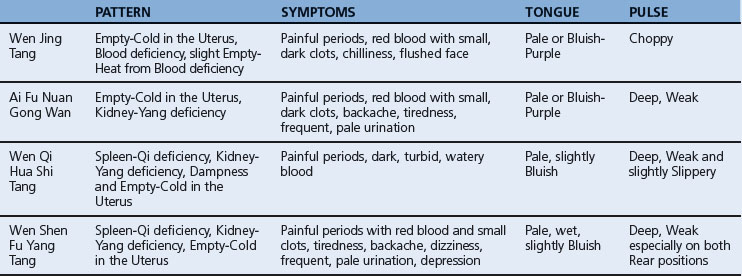
d Prescription
This formula is the most tonifying of the four for painful periods from Empty-Cold. The four formulae are compared and contrasted in Table 14.1.
Full-Cold
Prescription
Modifications
Lower abdominal pain before or after the period, pain central, pain relieved by the application of heat, menstrual blood rather scanty and bright red with small, dark clots, feeling cold, sore back. Tongue: Pale-Bluish or Bluish-Purple. Pulse: Deep and Choppy or Deep and Wiry.
LU-7 Lieque (on the right) and KI-6 Zhaohai (on the left), Ren-4 Guanyuan, Ren-6 Qihai, ST-29 Guilai, KI-14 Siman, SP-8 Diji, SP-6 Sanyinjiao, ST-36 Zusanli, ST-28 Shuidao. Reducing method except on ST-36 which should be reinforced. Moxa must be used.
A 42-year-old woman had been suffering from painful periods for 15 years. Her cycle was short, with a period coming every 21–25 days. She experienced severe pain during the period and the blood was red with small dark clots. She felt cold in general, but especially so during the period. She also suffered from backache and dizziness. Her tongue was Pale and slightly Swollen. Her pulse was very Slow (52), Choppy, Weak on the left Rear position and had no wave.
The painful periods themselves are due to Cold obstructing the Uterus. This is Cold of the Empty type as is clearly shown by the Weak and Choppy pulse. Besides this, there is an underlying deficiency of Kidney-Yang as shown by the Slow and Weak pulse on the left Rear position, Pale and Swollen tongue, dizziness, cold feeling and backache, and some deficiency of Qi and Blood as evidenced by the Choppy pulse.
The treatment principle adopted was to tonify and warm Kidney-Yang, scatter internal Cold, nourish Blood and stop pain. She was treated with both acupuncture and herbs.
The acupuncture points, used with even method to scatter Cold and reinforcing method to tonify the Kidneys and nourish Blood, were selected from the following:
The first 10 herbs constitute the root formula which scatters Cold, warms the Uterus, tonifies Qi and Blood and tonifies and warms Kidney-Yang.
This patient was treated with acupuncture every 2 weeks and took the above decoction, with slight variations, for 6 months. After this time, her cycle became regular and the menstrual pain was reduced by about 80%.
A 35-year-old woman had been suffering from painful periods from the age of 14 which were now getting worse. The pain was central in the lower abdomen and occurred mostly on the first day: severe and cramping, it was relieved by the application of a hot-water bottle. When she had the pain, she liked to curl up and she felt cold and turned pale. The menstrual cycle was 30 days long, the period lasted 5 days and the blood was dark with small clots.
Her complexion was pale, her tongue was slightly Pale with a white coating and her pulse was very slightly Tight on the left and Weak on both Rear positions.
This is a clear example of painful periods from Empty-Cold. The Cold is evident from the severe, cramping nature of the pain, its alleviation with heat, the cold feeling and pale complexion during the period, the small, dark clots and the Tight pulse. That the Cold is of a deficient nature is evident from the desire to curl up, from the Weak pulse on both Rear positions and from the fact that the pulse is only very slightly Tight on the left. Apart from the Empty-Cold, there is a deficiency of Kidney-Yang as shown by the Weak pulse on both Kidney positions.
As for the cause of this problem, as a schoolgirl in Yorkshire (a county in the North of England with a cold and damp climate) she played lots of sports and did cross-country running. This had obviously led to the invasion of external Cold in the Uterus; as explained in Chapter 4 on aetiology, the genital system in young girls is particularly vulnerable and prone to invasion of external Cold.
This patient was treated only with herbs as she lived quite a long way away. I selected a variation of Wen Jing Tang Warming the Menses Decoction, using the whole original decoction plus:
The results in this case exceeded every expectation as, after only seven packets of the above decoction, her next period was totally pain free and, at the time of writing (4 months later), her periods are still so. In subsequent decoctions, I added Du Zhong Cortex Eucommiae to tonify Kidney-Yang.
Damp-Heat
Clinical manifestations
Hypogastric pain before the period and sometimes on mid-cycle, burning sensation extending to the sacrum, feeling of heat, menstrual blood red with small clots, vaginal discharge, scanty, dark urine, thirst, mental restlessness. Tongue: Red, sticky-yellow tongue coating. Pulse: Slippery.
Acupuncture
SP-9 Yinlingquan, SP-6 Sanyinjiao, LU-7 Lieque on the right and KI-6 Zhaohai on the left, Ren-3 Zhongji, ST-28 Shuidao, BL-32 Ciliao, BL-22 Sanjiaoshu, Ren-9 Shuifen, L.I.-11 Quchi, SP-10 Xuehai, KI-2 Rangu, LIV-3 Taichong. Reducing or even method.
Herbal treatment
b Prescription
Women’s Treasure remedy
This remedy is a variation of the formula Qing Re Tiao Xue Tang Clearing Heat and Regulating Blood Decoction which clears Heat, cools Blood, resolves Dampness and stops pain. The tongue presentation appropriate to this remedy is a Red body with sticky-yellow coating.
Damp-Heat
Hypogastric pain before the period and sometimes on mid-cycle, burning sensation extending to the sacrum, feeling of heat, menstrual blood red with small clots, vaginal discharge, scanty, dark urine, thirst, mental restlessness. Tongue: Red, sticky-yellow tongue coating. Pulse: Slippery.
SP-9 Yinlingquan, SP-6 Sanyinjiao, LU-7 Lieque on the right and KI-6 Zhaohai on the left, Ren-3 Zhongji, ST-28 Shuidao, BL-32 Ciliao, BL-22 Sanjiaoshu, Ren-9 Shuifen, L.I.-11 Quchi, SP-10 Xuehai, KI-2 Rangu, LIV-3 Taichong. Reducing or even method.
Stagnant Liver-Qi turning into Fire
Clinical manifestations
Abdominal pain before or during the period, dark menstrual blood, heavy period, irritability, propensity to outbursts of anger, thirst, feeling of heat, dry stools. Tongue: Red with yellow coating, redder on the sides. Pulse: Rapid, Wiry. This is Liver-Fire deriving from long-term stagnation of Liver-Qi. It is treated not by draining Fire with bitter-cold herbs but by clearing Heat through eliminating stagnation.
Acupuncture
LIV-3 Taichong, LIV-2 Xingjian, LIV-14 Qimen, Ren-6 Qihai, Ren-4 Guanyuan, KI-14 Siman, SP-10 Xuehai, L.I.-11 Quchi, T.B.-6 Zhigou, G.B.-34 Yanglingquan. All with reducing or even method. No moxa.
Herbal treatment
a Prescription
Explanation
This formula is from Fu Qing Zhu’s Gynaecology. He explains that it is for abdominal pain before the period with dark, clotted blood, due to stagnant Liver-Qi turning into Fire. He says that to treat this, it is important to eliminate the stagnation; to clear Heat without eliminating the stagnation that creates it is like lopping off a branch (the Heat) but not the root (the stagnation).12
Unfortunately, Fu Qing Zhu does not explain the reason for the interesting inclusion of Bai Jie Zi in the formula: in fact, this herb expels Cold, warms the Lungs and resolves Cold-Phlegm from the Lungs. One possible explanation is that Bai Jie Zi is used to regulate Qi in the diaphragm, thus helping to pacify Liver-Qi; another, that this very pungent herb is coordinated with the bitter herbs, such as Huang Qin, according to the principle of using ‘the pungent taste to open the passages, and the bitter taste to make Qi descend’: this sounds good but it is a method that is actually used to resolve Dampness, not to pacify the Liver!
b Prescription
Explanation
This formula, already explained, is specific to clear Liver-Heat when it derives from stagnation of Liver-Qi. It is milder than the previous prescription and is therefore suitable when the symptoms of Heat are not pronounced and those of stagnation predominate.
Stagnant Liver-Qi turning into Fire
Abdominal pain before or during the period, dark menstrual blood, heavy period, irritability, propensity to outbursts of anger, thirst, feeling of heat, dry stools. Tongue: Red with yellow coating, redder on the sides. Pulse: Rapid, Wiry.
Empty conditions
Qi and Blood deficiency
Clinical manifestations
Dull hypogastric pain towards the end of or after the period, dragging sensation in the lower abdomen, pain relieved by pressure and massage, scanty bleeding, pale complexion, tiredness, slight dizziness, loose stools. Tongue: Pale. Pulse: Choppy.
Acupuncture
Ren-4 Guanyuan, Ren-6 Qihai, ST-36 Zusanli, SP-6 Sanyinjiao, SP-8 Diji, BL-20 Pishu, SP-10 Xuehai, BL-54 Zhibian, BL-32 Ciliao. All with reinforcing method except for SP-10, BL-54 and BL-32 which should be needled with even method. Moxa is applicable.
Herbal treatment
Women’s Treasure remedy
This remedy is a variation of the formula Ba Zhen Tang Eight Precious Decoction which nourishes Blood and tonifies Qi. The tongue presentation appropriate to this remedy is a Pale and Thin body.
Qi and Blood deficiency
Dull hypogastric pain towards the end of or after the period, dragging sensation in the lower abdomen, pain relieved by pressure and massage, scanty bleeding, pale complexion, tiredness, slight dizziness, loose stools. Tongue: Pale. Pulse: Choppy.
Ren-4 Guanyuan, Ren-6 Qihai, ST-36 Zusanli, SP-6 Sanyinjiao, SP-8 Diji, BL-20 Pishu, SP-10 Xuehai, BL-54 Zhibian, BL-32 Ciliao. All with reinforcing method except for SP-10, BL-54 and BL-32 which should be needled with even method. Moxa is applicable.
Yang and Blood deficiency
Clinical manifestations
Dull abdominal pain after the periods, scanty with pale blood, no clots, abdominal pain relieved by pressure and application of heat, dull headache, blurred vision, feeling cold, depression, dizziness. Tongue: Pale and Swollen. Pulse: Fine and Deep. This is due to a deficiency of Spleen-Yang and deficiency of Liver-Blood.
Acupuncture
BL-20 Pishu, Ren-12 Zhongwan, ST-36 Zusanli, SP-6 Sanyinjiao, Ren-4 Guanyuan, LIV-8 Ququan. LU-7 Lieque (on the right) and KI-6 Zhaohai (on the right), BL-54 Zhibian, BL-32 Ciliao. All with reinforcing method, except for BL-54 and BL-32 which should be needled with even method; moxa should be used.
Herbal treatment
a Prescription
Explanation
This is a variation of the formula Xiao Jian Zhong Tang Small Strengthening the Centre Decoction.
b Prescription
Women’s Treasure remedy
This remedy is a variation of the formula Dang Gui Jian Zhong Tang Angelica Strengthening the Centre Decoction which tonifies Kidney-Yang and nourishes Blood. The tongue presentation appropriate to this remedy is a Pale body.
Yang and Blood deficiency
Dull abdominal pain after the periods, scanty with pale blood, no clots, abdominal pain relieved by pressure and application of heat, dull headache, blurred vision, feeling cold, depression, dizziness. Tongue: Pale and Swollen. Pulse: Fine and Deep.
BL-20 Pishu, Ren-12 Zhongwan, ST-36 Zusanli, SP-6 Sanyinjiao, Ren-4 Guanyuan, LIV-8 Ququan. LU-7 Lieque (on the right) and KI-6 Zhaohai (on the right), BL-54 Zhibian, BL-32 Ciliao. All with reinforcing method, except for BL-54 and BL-32 which should be needled with even method; moxa should be used.
Kidney- and Liver-Yin deficiency
Clinical manifestations
Dull hypogastric pain towards the end of or after the period, sore back, dizziness, scanty bleeding, pain relieved by pressure and massage, tinnitus, blurred vision, exhaustion. Tongue: without coating; Red if there is Empty-Heat. Pulse: Floating-Empty.
Acupuncture
BL-23 Shenshu, BL-18 Ganshu, Ren-4 Guanyuan, SP-6 Sanyinjiao, KI-3 Taixi, ST-36 Zusanli, LU-7 Lieque (on the right) and KI-6 Zhaohai (on the left), BL-54 Zhibian, BL-32 Ciliao. Reinforcing method, except for BL-54 and BL-32 which should be needled with even method. A small amount of moxa may be used if the tongue is not too Red.
Herbal treatment
b Prescription
Explanation
This formula nourishes Blood as well as Yin and it is therefore used when there is deficiency of Blood as well as of Yin. It is a variation of Liu Wei Di Huang Tang Six-Ingredient Rehmannia Decoction.
Kidney- and Liver-Yin Deficiency
Dull hypogastric pain towards the end of or after the period, sore back, dizziness, scanty bleeding, pain relieved by pressure and massage, tinnitus, blurred vision, exhaustion. Tongue: without coating; Red if there is Empty-Heat. Pulse: Floating-Empty.
BL-23 Shenshu, BL-18 Ganshu, Ren-4 Guanyuan, SP-6 Sanyinjiao, KI-3 Taixi, ST-36 Zusanli, LU-7 Lieque (on the right) and KI-6 Zhaohai (on the left), BL-54 Zhibian, BL-32 Ciliao. Reinforcing method, except for BL-54 and BL-32 which should be needled with even method. A small amount of moxa may be used if the tongue is not too Red.
A 33-year-old woman had been suffering from painful periods for 10 years. The pain occurred during the period and the blood was bright red and rather scanty. She felt cold in general and colder during the period. She had had four miscarriages. She also suffered from backache, dizziness, tinnitus, poor memory, a dry mouth at night and night sweating. Her urination was frequent and occasionally it dribbled. She felt always very tired and her knees ached. Her tongue was of a normal colour but without spirit on the root. Her pulse was generally Weak and, on the left side, very Fine and Empty at the deep level.
This is a complicated condition characterized by a deficiency of both Kidney-Yin and Kidney-Yang. The symptoms of Kidney-Yin deficiency are: dizziness, tinnitus, dry mouth at night, night sweating, poor memory, tongue root without spirit and pulse Empty at the deep level. The symptoms of Kidney-Yang deficiency are: feeling cold, achy knees and frequent and dribbling urination. The miscarriages were due to the Kidney deficiency. Thus, this is a deficiency type of painful periods.
The treatment principle adopted was to nourish Kidney-Yin and warm and tonify Kidney-Yang. The emphasis was put on nourishing Kidney-Yin as when both Yin and Yang are deficient, it is important to nourish the substance first (Kidney-Yin) rather than the function (Kidney-Yang). The very Fine pulse which is also Empty at the deep level also indicates the importance of nourishing the Yin primarily. However, secondary tonification of Kidney-Yang should not be overlooked.
The first seven herbs constitute the Tiao Gan Tang which nourishes Liver and Kidneys.
This patient was treated with this decoction (with slight variations) for 6 months, producing a cure in the painful periods. After a further 6 months of treatment with the same decoction taken on alternate weeks, she conceived and delivered a healthy baby.
Ancient acupuncture prescriptions for Painful Periods14
Prognosis and prevention
Both acupuncture and Chinese herbs either singly or in combination give excellent results in painful periods and the overwhelming majority of cases can be cured. The Empty types are easier to treat than the Full types. Of the Full types, the one from Damp-Heat is the most difficult to treat while the one from stagnation of Qi and Blood is the easiest. Of course, in many patients there is a mixed condition of deficiency and excess, in which case one concentrates on treating the stagnation in the 2 weeks before the periods and the deficiency in the 2 weeks after. In some cases, it is better to eliminate pathogenic factors before tonifying: see case history above.
In any menstrual problem, it takes a minimum of three menstrual cycles to regulate Blood and the Directing and Penetrating Vessels. Three months is therefore the shortest possible time for the treatment to be successful.
If dysmenorrhoea is due to endometriosis (see below), the treatment will take considerably longer than for functional painful periods. Dr Su Xin Ming, my acupuncture teacher in Nanjing, used to say that acupuncture should give very good results in painful periods: if it does not, it probably means the woman has endometriosis.
Western view
Western medicine differentiates primary from secondary dysmenorrhoea.
Primary dysmenorrhoea starts during adolescence and is not associated with any organic disorder. From the Chinese point of view, this is often due to invasion of Cold in the Uterus when young girls are exposed to cold during puberty either because they often play outdoor games during cold and wet winters, or because they have been engaged in physical work (such as farming) outdoors.
Secondary dysmenorrhoea starts later in life and may be associated (although not necessarily) with organic diseases such as endometriosis, pelvic inflammatory disease or myomas.
Studies show that primary dysmenorrhoea is associated with uterine hypercontractility: during contractions, endometrial blood flow is reduced and there is a correlation between minimal blood flow and maximal colicky pain, favouring the idea that ischaemia due to hypercontractility causes primary dysmenorrhoea.16 This ties in well with the Chinese idea that stagnation of Qi and Blood is a factor in most types of dysmenorrhoea: indeed, one of the many actions of Blood-invigorating herbs is to improve circulation of blood and relieve ischaemia.
Endometriosis
In endometriosis, ectopic endometrium is implanted in adjacent pelvic organs such as ovaries, Fallopian tubes, pelvic ligaments, vagina, sigmoid colon, rectum, ureters or bladder. The most common symptom associated with endometriosis is pelvic pain which usually starts 1–2 days before the period and lasts throughout it. There may also be rectal pressure, pain on defaecation, lower backache radiating to the anterior thigh and dyspareunia (pain on intercourse). However, there is no direct correlation between the severity of the pain and the extent of endometriosis: in fact, some women with severe endometriosis may have no symptoms and, vice versa, women with very slight endometriosis may suffer severe pain.
The differential diagnosis of endometriosis is very difficult because many other diseases present with symptoms very similar to those of endometriosis: these include primary dysmenorrhoea, pelvic inflammatory disease, ovarian tumours, uterine myomas and gastrointestinal disorders such as irritable bowel syndrome.
The diagnosis of endometriosis is also fraught with difficulties and is affected by subjectivity. Although a laparoscopy may seem an objective and conclusive diagnostic technique, it suffers from inherent faults: the main one, that it relies entirely on the visual and very subjective assessment of the pelvis by the operator and consequently is prone to misinterpretation and subjectivity; often microscopic disease is not detected. Laparoscopy is also associated with significant morbidity.17 Endometriosis is on the increase and it has become the commonest cause of secondary dysmenorrhoea. It is also a major cause of infertility: 30–70% of women investigated for infertility are found to have endometriosis in varying degrees of severity. However, as it occurs in other cases, this association does not necessarily prove that there is a causal link between endometriosis and infertility, except in cases of gross disease of the pelvis.
Endometriosis may cause lack of ovulation, the luteinized unruptured follicle syndrome (i.e. the follicle responds to the luteinizing hormone surge but fails to rupture) and luteal phase deficiency: each of these conditions may cause infertility. The treatment for endometriosis in women over 40 is radical surgery, i.e. hysterectomy, bilateral salpingo-oophorectomy and resection of all residual disease. In women under 40, danazol is usually prescribed: this is a derivative of 17α ethinyl testosterone that acts on ovarian steroidogenesis and with an antigonadotropic effect. The side effects of danazol are largely androgenic and they include weight gain, reduction in breast size, mood changes, depression, acne, decreased libido, headaches, muscle cramps, hot flushes, oily skin, oedema, hirsutism, nausea and a deep voice. This last change is often permanent and irreversible when the medication is discontinued.
From a Chinese perspective, this disease falls under the category of ‘Painful Periods’ or ‘Abdominal Masses’. Endometriosis is discussed in detail in Chapter 65.
Myoma
Myomas do not usually cause pain. However, if there is torsion they may cause dysmenorrhoea. Dysmenorrhoea due to myomas may be helped even if they cannot be dissolved. Invigorating Blood and eliminating stasis will ease the dysmenorrhoea and in general make the abdomen feel more comfortable in spite of the myomas.
Very small myomas (up to about 2 cm in diameter) may be dissolved with acupuncture and Chinese herbs. If the diagnosis of myomas is definitely confirmed, then the formulae used should include strong herbs which ‘break’ Blood such as E Zhu Rhizoma Curcumae, Ze Lan Herba Lycopi and San Leng Rhizoma Sparganii.
A particularly good formula for myomas from stasis of Blood is Gui Zhi Fu Ling Tang Ramulus Cinnamomi-Poria Decoction which contains Gui Zhi Ramulus Cinnamomi, Fu Ling Poria, Tao Ren Semen Persicae, Chi Shao Radix Paeoniae rubra and Mu Dan Pi Cortex Moutan.
The treatment of myomas is discussed in detail in Chapter 67.
Clinical trials
Acupuncture
The effects of auricular acupressure and nitric oxide on menstrual symptoms for women with primary dysmenorrhoea
Objective
The aim of this study was to evaluate the effects of auricular acupressure on relieving menstrual symptoms and decreasing nitric oxide (NO) for women with primary dysmenorrhoea.
Methods
This was a randomized clinical trial comparing the effects of auricular acupressure by seed-pressure method and placebo adhesive patch. The trials took place at colleges in northern and central Taiwan. A total of 71 college women took part with a diagnosis of primary dysmenorrhoea confirmed by the presence of serum CA125 testing. Thirty-six women were randomly allocated to the acupressure group and 35 to the control group. The acupressure group received auricular acupressure by seed-pressure method on the Liver, Kidney and Endocrine points. The control group had a plain adhesive patch placed on the same points with no seed attached. The protocol included massaging each point 15 times, three times a day, for a total of 20 days. Outcomes measures were: a primary short-form Menstrual Distress Questionnaire (MDQ), and secondary NO blood samples. Assessments of both were performed at baseline and within the first 2 days of the next menstrual cycles (after completion of 20 days of acupressure).
Results
In the acupressure group, the overall menstrual symptoms and the two subscales, menstrual pain and negative affects, revealed that menstrual symptoms decreased significantly after auricular acupressure by the seed-pressure method (P < 0.05). NO level increased in the acupressure group, although this difference did not achieve statistical significance (P > 0.05).
The influence of ginger-partitioned moxibustion on serum nitric oxide (NO) and plasma endothelin-1 levels in patients with primary dysmenorrhoea due to Cold-Damp stagnation
Objective
To explore the mechanism of ginger-partitioned moxibustion in the treatment of cold-damp stagnation primary dysmenorrhoea (PD) patients.
Methods
A total of 209 PD outpatients with a diagnosis of cold-damp stagnation from three hospitals were randomized into two groups. The moxibustion group (n = 105) was treated with ginger-partitioned moxibustion, and the control group (n = 104) was given Yueyueshu Tang (Menstruation Calming Decoction). Ginger-partitioned moxibustion was applied to Ren-8 Shenque and Ren-4 Guanyuan from the start of the menstrual period onwards for the first course and 3 days before the start for the second and third course. At baseline and after the treatment, plasma endothelin-1 (ET-1) and serum nitric oxide (NO) levels were compared with those of women (n = 20) experiencing a normal menstrual period and were determined by radioimmunoassay and nitrate reductase methods.
Results
After treatment, of the 105 and 104 cases in the moxibustion and control groups, 58 and 32 were cured, 37 and 33 saw markedly effective results, 5 and 24 saw effective results, and 5 and 15 failed, with the effective rates being 95.24% and 85.58% respectively. The therapeutic effect of the moxibustion group was significantly better than that of control group (P < 0.05). At baseline, in comparison with the normal group, plasma ET-1 contents in both the moxibustion and control groups were significantly higher (P < 0.01), while serum NO contents in these two groups were markedly lower (P < 0.01). After the treatment, comparison of both the moxibustion and control groups showed that plasma ET-1 decreased significantly and serum NO levels increased considerably (P < 0.05, P < 0.01), and the therapeutic effect of the moxibustion group was markedly superior to that of the control group in lowering plasma ET-1 (P < 0.01).
The acupuncture treatment of dysmenorrhoea which is resistant to conventional medical treatment
Objective
To evaluate the effect of acupuncture on non-steroidal anti-inflammatory drug (NSAID)-resistant dysmenorrhoea-related pain.
Methods
Fifteen patients received 8 weekly acupuncture treatments at KI-3 Taixi, LIV-3 Taichong, SP-4 Gongsun, ST-36 Zusanli, ST-25 Tianshu, ST-29 Guilai, ST-30 Qichong, Ren-4 Guanyuan, Ren-6 Qihai, BL-62 Shenmai, HE-7 Shenmen, L.I.-4 Hegu, P-6 Neiguan and Zigong. The patients were allowed to continue taking painkillers. Pain was measured according to the visual analogue scale (VAS) and was measured at baseline (T1), mid-treatment (T2), end of the treatment (T3) and 3 months (T4) and 6 months (T5) after the end of the treatment.
Results
Pain levels and NSAID use were substantially reduced in 13 out of 15 patients (87%). The pain intensity was significantly reduced with respect to baseline (average VAS = 8.5), by 64%, 72%, 60% and 53% at T2, T3, T4 and T5 respectively. A greater reduction of pain was observed for primary as compared with secondary dysmenorrhoea. The average pain duration at baseline (2.6 days) was significantly reduced by 62%, 69%, 54% and 54% at T2, T3, T4 and T5 respectively. The average NSAID use was significantly reduced by 63%, 74%, 58% and 58% at T2, T3, T4 and T5 respectively, and ceased completely in 7 patients, who were still asymptomatic 6 months after the treatment.
A clinical observation of the treatment of primary dysmenorrhoea with acupuncture and massage
Objective
To observe the clinical therapeutic effect of acupuncture massage for primary dysmenorrhoea and the influence of acupuncture on prostaglandin F2α level in menstrual fluid.
Methods
Ninety women with primary dysmenorrhoea were assigned to an acupuncture group (n = 30), a massage group (n = 30) and a control group (n = 30) which was given Somiton tablet orally. The treatment course was three menstrual cycles. The pain-relieving effect was evaluated using a numerical rating scale (NRS) at baseline and after treatment and change of PGF2α content in menstrual fluid was tested.
Acupuncture at the Siguan (4 gates) points for the treatment of primary dysmenorrhoea
Objective
To observe the therapeutic effect of acupuncture, using the Qinglong Baiwei (Green Dragon Swaying its Tail) method at the Siguan points, on primary dysmenorrhoea (PD).
Methods
One-hundred and eighty women with PD were randomly divided into group A, group B and group C, with 60 cases in each group. Group A was treated by acupuncture at L.I.-4 Hegu and LIV-3 Taichong using the Qinglong Baiwei method; group B was treated by routine acupuncture with SP-6 Sanyinjiao and BL-32 Ciliao as the main points; and group C was treated by oral administration of Yueyueshu Tang (Menstruation Calming Decoction). After 3 months of treatment, the therapeutic effects were analysed, and changes of haemorrheologic indices and the prostaglandin level were observed.
Results
The cured rate and the total effective rates were 75% and 100% in group A, 60% and 95% in group B, and 25% and 90% in group C respectively, group A and B being significantly better than group C (P < 0.01). The analgesic effects within 30 minutes of treatment in both groups A and B were significantly better than that in group C (P < 0.01), and that in group A was significantly better than that in group B (P < 0.01).
Acupuncture in patients with dysmenorrhoea: a randomized study on clinical effectiveness and cost-effectiveness in usual care
Objective
To investigate the clinical effectiveness and cost-effectiveness of acupuncture in patients with dysmenorrhoea.
Methods
In this randomized controlled trial plus non-randomized cohort, 201 patients with dysmenorrhoea were randomized to receive acupuncture (15 sessions over 3 months) or to a control group (no acupuncture). A total of 649 women participated (mean age 36.1 ± 7.1 years) of whom 201 were randomized. Patients who declined randomization received acupuncture treatment. All subjects were allowed to receive usual medical care.
Results
After 3 months, the average pain intensity on a scale of 0–10 was lower in the acupuncture compared to the control group: 3.1 vs. 5.4 which was a significant difference (P < 0.001). The acupuncture group had better quality of life scores.
Conclusion
Additional acupuncture in patients with dysmenorrhoea was associated with improvements in pain and quality of life as compared to treatment with usual care alone. Although acupuncture treatment in addition to usual care incurs additional costs, the improvement to a patient’s quality of life can be considered as cost-effective.
An observation on retained seeds at auricular acupuncture points for the treatment of primary dysmenorrhoea
Objective
To observe the therapeutic effect and prognosis of using ear seeds for primary dysmenorrhoea.
Methods
One-hundred and fourteen women were randomly divided into an ear seed group (n = 60) and a Western medication group (n = 54). The ear seed group was treated at the points: Shenmen, Uterus, Endocrine, Subcortex, Sympathetic and Kidney using Vaccaria seeds which were retained with an adhesive plaster. The Western medication group was treated orally with Indomeixin enteric tablets. (Enteric tablets use a special coating which prevents release and absorption of the active ingredients until the tablets reach the intestines.) The therapeutic effects were assessed after treatment of three menstrual cycles.
A randomized controlled study on the analgesic effect of superficial needling plus electrostimulation of SP-6 Sanyinjiao for primary dysmenorrhoea
Objective
To evaluate the analgesic and therapeutic effects of superficial acupuncture followed by electrostimulation (ESA) of SP-6 Sanyinjiao for treating primary dysmenorrhoea (PD).
Methods
One-hundred and seventy-one patients were randomly divided into ESA (n = 57), superficial acupuncture (SA; n = 57) and medication (n = 57) groups. Patients in the SA group were needled bilaterally at SP-6 Sanyinjiao and patients in the ESA group were needled at SP-6 Sanyinjiao bilaterally before electric stimulation of 60 Hz (2–3 V) was applied for 30 minutes. Patients in the medication group took Brufen sustained-release capsules 0.3 mg, b.i.d., for 3 days, then again 3 days before the start of menstruation for 5 days. The cumulative score of clinical symptoms was evaluated before and after the treatment.
Results
Comparison among the three groups showed that there was a significant difference from baseline scores to post-treatment scores in both the ESA and SA groups and these were significantly larger than that of the medication group (P < 0.001). In the ESA group, during the first menstrual cycle, the number of patients who saw complete relief from their symptoms after 30 minutes of stimulation was significantly more than those of the SA group (P < 0.05). Results of intention-to-treat (ITT) analysis showed that out of the ESA, SA and medication groups, the cured cases were 40, 38 and 10, the markedly effective were 9, 10 and 27, the effective were 5, 4 and 7, and the failed were 3, 5 and 13 respectively with the total effective rates being 94.74%, 91.23% and 77.19% respectively. The effective rates of ESA and SA groups were significantly higher than that of medication group (P < 0.01), and the results of per-protocol analysis were similar to those of ITT analysis.
Ascertaining the efficacy of acupuncture for the treatment of primary dysmenorrhoea
Objective
The aim of this study was to evaluate the effect of acupuncture in the treatment of primary dysmenorrhoea (PD).
Methods
This clinical prospective, placebo-controlled trial included 57 women with primary dysmenorrhoea. Of these, 30 were treated with real acupuncture at the points Du-20 Baihui, bilateral L.I-4 Hegu, Ren-3 Zhongji, Ren-4 Guanyuan, Ren-6 Qihai, bilateral G.B-34 Yanglingquan, bilateral BL-23 Shenshu, bilateral SP-6 Sanyinjao and auricular acupuncture at Shenmen; 27 women were treated with placebo acupuncture. Acupuncture treatments were considered successful if PD did not occur any more, medication for PD became unnecessary or if PD symptoms did not occur for 2 years after the acupuncture treatment.
Herbal treatment
The therapeutic effects of Chiljeh Yangbuh Wan on primary dysmenorrhoea: a randomized, double blind, placebo-controlled study
Objective
This clinical study was conducted to investigate the efficacy and safety of Chiljeh Yangbuh Wan (CYW), a herbal medicine native to Korea, in treating primary dysmenorrhoea.
Methods
One-hundred patients with primary dysmenorrhoea who visited Kyung Hee University Korean Oriental Medicine Hospital between 19 July 2004 and 27 August 2004 were recruited. Secondary or drug-related dysmenorrhoea was screened out through interviews and examination. The patients were randomized to receive either CYW or a placebo formula for one menstrual period in a double-blind model. Visual analogue scale (VAS), Verbal rating scale (VRS), and multidimensional verbal rating scale (MVRS) were used to evaluate the severity of the dysmenorrhoea. A total of 71 patients who passed the screening test was divided into either the placebo or CYW group. These two groups were further split into smaller subsets (indication, non-indication, and unspecified group) according to Korean Oriental medical diagnosis.
Results
In the non-indication group, the placebo and CYW group did not show significant difference in VAS, VRS and MVRS scores at baseline (first VAS, first VRS, first MVRS), or after medication (second VAS, second VRS, second MVRS). In the indication group, the placebo and CYW group showed significant difference in change in VAS and MVRS scores. No evidence of toxicity could be found, and no serious adverse reactions to CYW were reported.
The clinical efficacy of Kampo medicine (Japanese traditional herbal medicine) in the treatment of primary dysmenorrhoea
Methods
A retrospective evaluation of Kampo treatment in 176 subjects with dysmenorrhoea during the previous 12 years was performed. In order to minimize the subjective discretion of the severity of symptoms, classification of the severity level of abdominal pain during menstruation was applied by considering the requirement for non-steroidal anti-inflammatory drugs (NSAIDs) and disturbance of daily activities. Severity levels at baseline and after Kampo treatment were defined in 108 patients. The following severity levels were used: no abdominal pain (level 0), abdominal pain with no requirement of NSAIDs (level 1), abdominal pain with no daily activity disturbances with use of NSAIDs (level 2), and painful menstruation which required absenteeism even with use of NSAIDs (level 3).
A traditional Chinese herbal medicine used to treat dysmenorrhoea among Taiwanese women
Objective
The purposes of this study were two-fold: first, to ascertain the relative effectiveness of the Chinese herbal formula Si Wu Tang Four Substances Decoction (SWT) for dysmenorrhoea, and second, to compare two different timings for consumption of SWT in terms of menstrual pain.
Methods
A total of 49 participants was alternately assigned into two study groups. The experimental group was administered 15 g of SWT daily for 7 consecutive days, following the cessation of menstrual bleeding, for two consecutive menstrual cycles. The comparison group was provided with a similar intervention as soon as menstrual bleeding was noted. The degree of menstrual pain was recorded daily using a visual analogue scale and the duration of pain was also recorded during menstrual bleeding for five consecutive menstrual cycles.
Results
The results indicated that the decrease in menstrual pain levels and the duration of pain between the experimental group and the comparison group was not significant. However, the decrease in menstrual pain and the duration of pain over the five menstrual cycles within the experimental group (from 2.07 to 1.42; 2.71 to 1.21; P < 0.05) and within the comparison group (from 1.94 to 1.23; 2.66 to 1.68; P < 0.05) were significant (P < 0.05).
Chinese herbal medicine for primary dysmenorrhoea
Objective
To determine the efficacy and safety of Chinese herbal medicine for primary dysmenorrhoea when compared with placebo, no treatment and other treatment.
Search strategy
Selection criteria
Any randomised controlled trials involving Chinese herbal medicine versus placebo, no treatment, conventional therapy, heat compression, another type of Chinese herbal medicine, acupuncture or massage were assessed. Exclusion criteria were identifiable pelvic pathology and dysmenorrhoea resulting from the use of an intra-uterine contraceptive device.
Data collection and analysis
Quality assessment, data extraction and data translation were performed independently by two review authors. Attempts were made to contact study authors for additional information and data.
Results
Thirty-nine randomized controlled trials (RCTs) involving a total of 3475 women were included in the review. A number of the trials were of small sample size and poor methodological quality. Results for Chinese herbal medicine compared to placebo were unclear in three RCTs. Chinese herbal medicine resulted in significant improvements in pain relief in 14 RCTs, improvement in overall symptoms in six RCTs and use of additional medication in two RCTs when compared to use of pharmaceutical drugs. Self-designed Chinese herbal formulae resulted in significant improvements in pain relief in 18 RCTs, in overall symptoms in 14 RCTs and use of additional medication in five RCTs after up to 3 months of follow-up when compared to commonly used Chinese herbal health products. Chinese herbal medicine also resulted in better pain relief than acupuncture in two RCTs and heat compression in one RCT.
The effect of Tong Jing Ning Dysmenorrhoea pill on primary dysmenorrhoea
Methods
One-hundred and twenty primary dysmenorrhoea patients were treated with TJN and 40 patients were treated with aspirin as controls. The levels of serum oestrogen (E2) and progestin (P) content in the luteal metaphase and anaphase (MI/AI) as well as endothelin (ET) and calcitonin gene related peptide (CGRP) in the metaphase and menstrual stage before and after treatment were determined.
Results
The therapeutic effect, and the curative markedly effective rate and improvement rate of the main accompanying symptoms of severe and moderate primary dysmenorrhoea patients in the treated group were superior to those in the control group (P < 0.01). The level of E2 and ET were significantly decreased, and the content of P and CGRP respectively were significantly increased in the treated group after treatment (P < 0.01).
A novel anti-dysmenorrhoea therapy with cyclic administration of 2 Japanese-Chinese herbal medicines
Objective
To evaluate the effect of two Japanese–Chinese herbal medicines on the treatment of dysmenorrhoea.
Methods
Seventeen patients were administered Shakuyakukanzoto (SK) (Shao Yao Gan Cao Tang Peony and Licorice Decoction) and Tokishakuyakusan (TS) (Dang Gui Shao Yao San Angelica Paeonia Powder) alternately within the menstrual cycle (SK/TS cyclic therapy).
Results
All of the 17 patients suffering from dysmenorrhoea (including recurrent endometriotic and adenomyotic patients following treatment with gonadotropin-releasing hormone agonists or Danazol) obtained complete relief within 3 months when treated with the SK/TS cyclic therapy. Nine of 12 patients treated with the SK/TS cyclic therapy ovulated as determined by biphasic changes in basal body temperature patterns. All the three secondary amenorrhoea patients with moderate levels of serum oestradiol, but not the three secondary amenorrhoea patients with little serum oestradiol, ovulated during the SK/TS cyclic therapy. One of the treated patients, who had a history of 10 repetitive spontaneous abortions, carried the eleventh pregnancy to term resulting in a healthy newborn.
He Ren 1981 A New Explanation of the Synopsis of Prescriptions from the Golden Cabinet (Jin Gui Yao Lue Xin Jie![]() ), Zhejiang Science Publishing House, p. 188. The Synopsis of Prescriptions from the Golden Cabinet was written by Zhang Zhong Jing c. AD 200..
), Zhejiang Science Publishing House, p. 188. The Synopsis of Prescriptions from the Golden Cabinet was written by Zhang Zhong Jing c. AD 200..
Fu Qing Zhu 1973 Fu Qing Zhu’s Gynaecology (Fu Qing Zhu Nu Ke![]() ), Shanghai People’s Publishing House, Shanghai, p.19. First published in 1827. Fu Qing Zhu was born in 1607 and died in 1684..
), Shanghai People’s Publishing House, Shanghai, p.19. First published in 1827. Fu Qing Zhu was born in 1607 and died in 1684..
Zhang Jing Yue 1986 The Complete Works of Jing Yue (Jing Yue Quan Shu![]() ), Shanghai Science and Technology Press, Shanghai, p. 641. First published in 1624..
), Shanghai Science and Technology Press, Shanghai, p. 641. First published in 1624..
1979 The Yellow Emperor’s Classic of Internal Medicine – Simple Questions (Huang Di Nei Jing Su Wen![]() ), People’s Health Publishing House, Beijing, p. 4. First published c. 100 BC..
), People’s Health Publishing House, Beijing, p. 4. First published c. 100 BC..
Shandong College of Traditional Chinese Medicine 1980 An Explanation of the ABC of Acupuncture (Zhen Jiu Jia Yi Jing Jiao Shi![]() ), People’s Health Publishing House, Beijing, p. 1476. The ABC of Acupuncture was written by Huang Fu Mi c. AD 259..
), People’s Health Publishing House, Beijing, p. 1476. The ABC of Acupuncture was written by Huang Fu Mi c. AD 259..
Hu Xi Ming 1990 Great Treatise of Secret Formulae in Chinese Medicine (Zhong Guo Zhong Yi Mi Fang Da Quan![]() ), Culture Publishing House, Shanghai, Vol. 2, p. 203..
), Culture Publishing House, Shanghai, Vol. 2, p. 203..
Zhou Cui Zhen 1996 Titbits from Dr Cai Xiao Sun Experience in Treating Difficult Gynaecological Diseases, Journal of Traditional Chinese Medicine (Zhong Yi Za Zhi![]() ) 37(2): 80..
) 37(2): 80..
An Explanation of the ABC of Acupuncture, p. 1476..
A New Explanation of the Synopsis of Prescriptions from the Golden Cabinet, p. 188..
Fu Qing Zhu’s Gynaecology, pp 22–23..
Great Treatise of Secret Formulae in Chinese Medicine, p. 204..
Wang Xue Tai 1995 Great Treatise of Chinese Acupuncture (Zhong Guo Zhen Jiu Da Quan ![]() ), Henan Science and Technology Publishing House, p. 452..
), Henan Science and Technology Publishing House, p. 452..
Chen You Bang 1990 Chinese Acupuncture Therapy (Zhong Guo Zhen Jiu Zhi Liao Xue![]() ), China Scientific Publishing House, Beijing, p. 884..
), China Scientific Publishing House, Beijing, p. 884..
Ann McPherson 1993, Women’s Problems in General Practice, Oxford University Press, Oxford, p. 185..