Abdomen
Examination
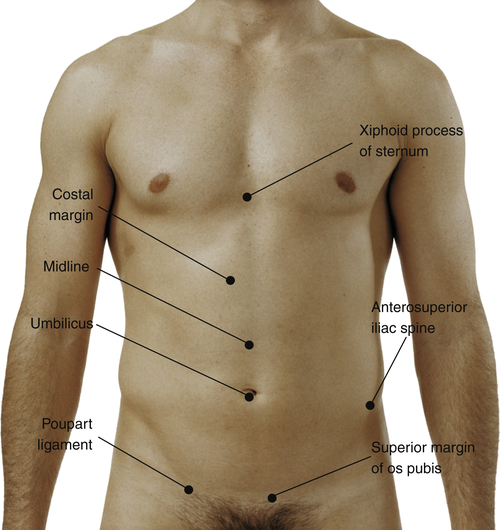
Have patient in the supine position to start the examination. Approach the patient from the right side.
| Technique | Findings |
| Inspect abdomen | |
| EXPECTED: Usual color variations, such as paleness or tanning lines. Fine venous network (venous return toward head above umbilicus, toward feet below umbilicus). | |
| UNEXPECTED: Generalized color changes, such as jaundice or cyanosis. Glistening, taut appearance. Bluish periumbilical discoloration, bruises, other localized discoloration. Striae, lesions or nodules, a pearl-like enlarged umbilical node, scars. | |
| EXPECTED: Flat, rounded, or scaphoid. Contralateral areas symmetric. Maximum height of convexity at umbilicus. Abdomen remains smooth and symmetric while patient holds breath. | |
| UNEXPECTED: Umbilicus displaced upward, downward, or laterally or is inflamed, swollen, or bulging. Any distention (symmetric or asymmetric), bulges, or masses while breathing comfortably or holding breath. | |
| EXPECTED: Smooth, even motion with respiration. Female patients mostly costal movement; male patients mostly abdominal. Pulsations often visible in upper midline in thin adults. | |
| UNEXPECTED: Limited motion with respiration in male adults. Rippling movement (peristalsis) or marked pulsations. | |
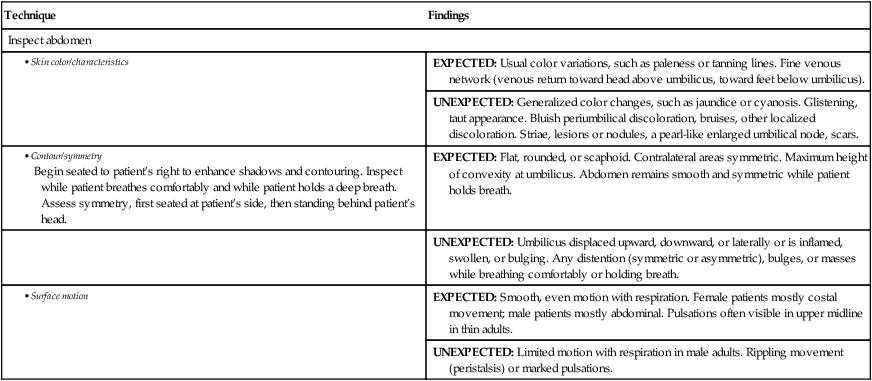
| Inspect abdominal muscles as patient raises head | |
| EXPECTED: No masses or protrusions. | |
| UNEXPECTED: Masses, protrusion of the umbilicus and other hernia signs, or separation of rectus abdominis. | |
| Auscultate with stethoscope diaphragm | |
| EXPECTED: 5-35 irregular clicks and gurgles per minute. Borborygmi, or increased sounds, may be because of hunger. | |
| UNEXPECTED: Increased sounds unrelated to hunger and high-pitched tinkling sounds may be caused by early intestinal obstruction; decreased or absent sounds after 5 min of listening may be associated with abdominal pain and rigidity. | |
| EXPECTED: Silent. | |
| UNEXPECTED: Friction rubs (high-pitched grating sound in association with respiration). | |
| Auscultate with stethoscope bell | |
| EXPECTED: No bruits (harsh or musical sound indicating blood flow turbulence), venous hum (soft, low-pitched, and continuous sound), or friction rubs. | |
| UNEXPECTED: Bruits in aortic, renal, iliac, or femoral arteries. | |
| EXPECTED: No venous hum. | |
| UNEXPECTED: Venous hum. | |
 |
|

Percussion Notes of the Abdomen
| Note | Description | Location |
| Tympany | Musical note of higher pitch than resonance | Over air-filled viscera |
| Hyperresonance | Pitch lies between tympany and resonance | Base of left lung |
| Resonance | Sustained note of moderate pitch | Over lung tissue and sometimes over abdomen |
| Dullness | Short, high-pitched note with little resonance | Over solid organs adjacent to air-filled structures |
| Technique | Findings |
| Percuss abdomen | |
| Note: Percussion can be done independently or concurrently with palpation. | |
| EXPECTED: Tympany predominant. Dullness over organs and solid masses. Dullness in suprapubic area from distended bladder. See table on p. 136 for percussion notes. | |
| UNEXPECTED: Dullness predominant. | |
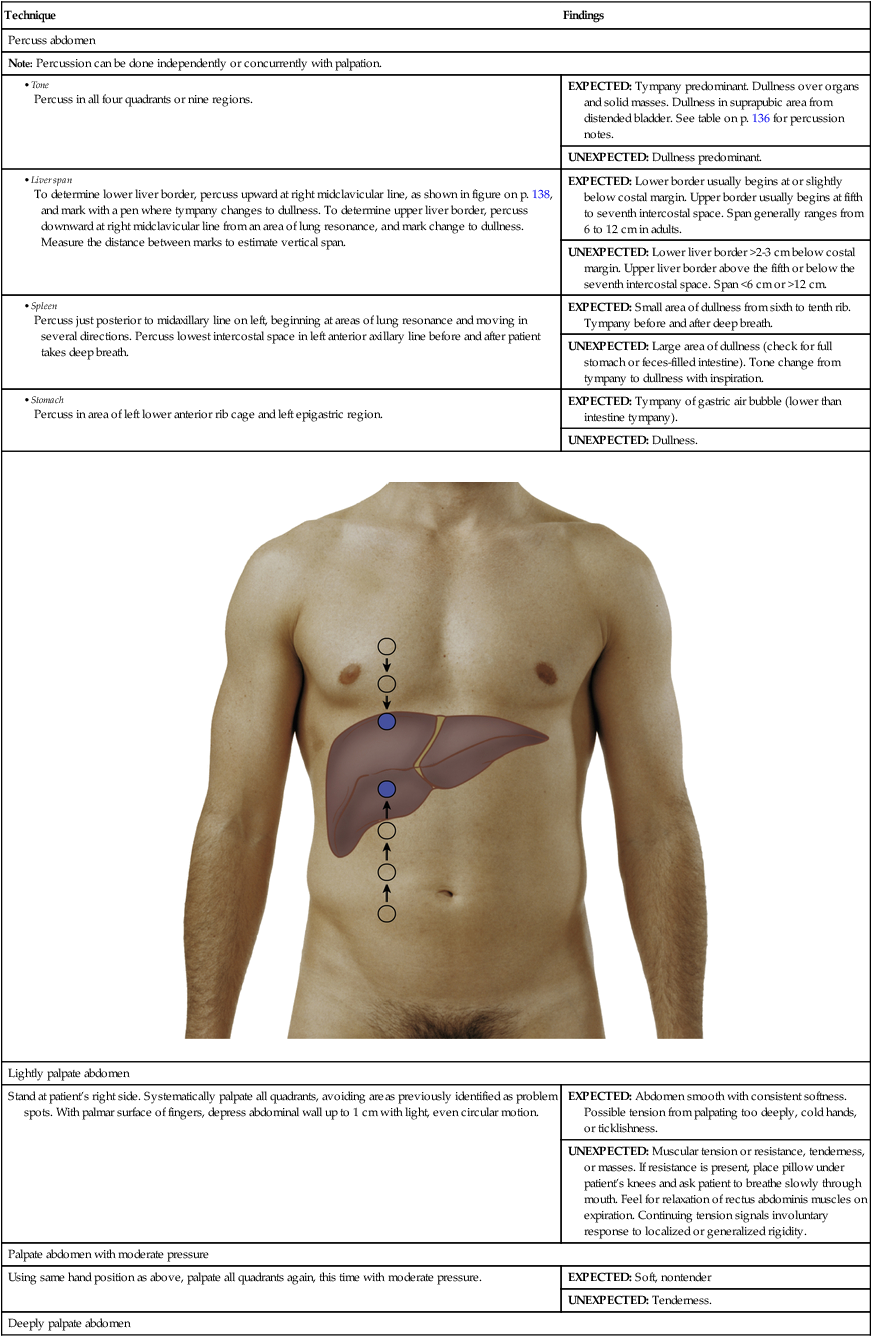
|
To determine lower liver border, percuss upward at right midclavicular line, as shown in figure on p. 138, and mark with a pen where tympany changes to dullness. To determine upper liver border, percuss downward at right midclavicular line from an area of lung resonance, and mark change to dullness. Measure the distance between marks to estimate vertical span. |
EXPECTED: Lower border usually begins at or slightly below costal margin. Upper border usually begins at fifth to seventh intercostal space. Span generally ranges from 6 to 12 cm in adults. |
| UNEXPECTED: Lower liver border >2-3 cm below costal margin. Upper liver border above the fifth or below the seventh intercostal space. Span <6 cm or >12 cm. | |
| EXPECTED: Small area of dullness from sixth to tenth rib. Tympany before and after deep breath. | |
| UNEXPECTED: Large area of dullness (check for full stomach or feces-filled intestine). Tone change from tympany to dullness with inspiration. | |
| EXPECTED: Tympany of gastric air bubble (lower than intestine tympany). | |
| UNEXPECTED: Dullness. | |
 |
|
| Lightly palpate abdomen | |
| Stand at patient’s right side. Systematically palpate all quadrants, avoiding areas previously identified as problem spots. With palmar surface of fingers, depress abdominal wall up to 1 cm with light, even circular motion. | EXPECTED: Abdomen smooth with consistent softness. Possible tension from palpating too deeply, cold hands, or ticklishness. |
| UNEXPECTED: Muscular tension or resistance, tenderness, or masses. If resistance is present, place pillow under patient’s knees and ask patient to breathe slowly through mouth. Feel for relaxation of rectus abdominis muscles on expiration. Continuing tension signals involuntary response to localized or generalized rigidity. | |
| Palpate abdomen with moderate pressure | |
| Using same hand position as above, palpate all quadrants again, this time with moderate pressure. | EXPECTED: Soft, nontender |
| UNEXPECTED: Tenderness. | |
| Deeply palpate abdomen | |
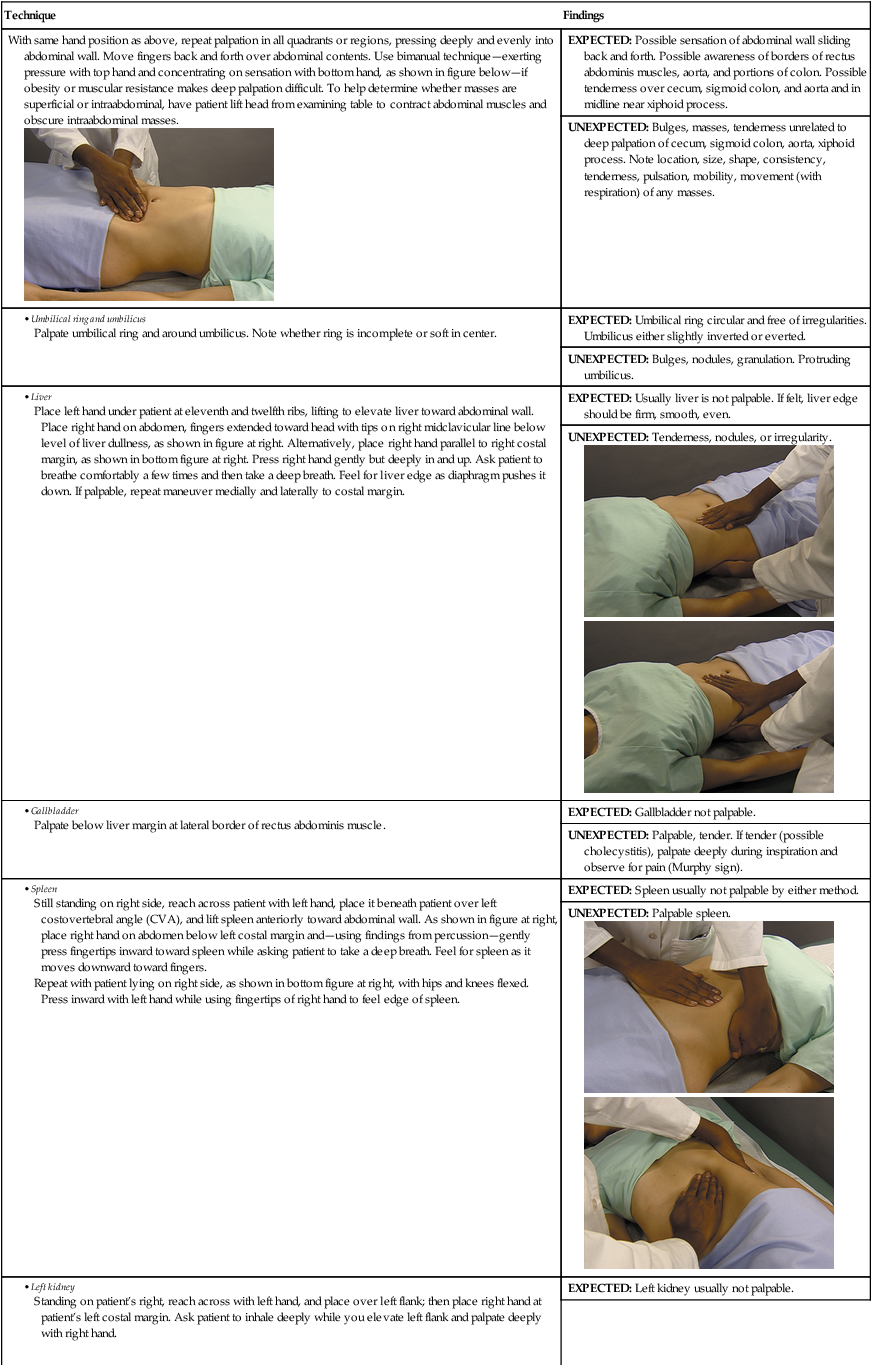
With same hand position as above, repeat palpation in all quadrants or regions, pressing deeply and evenly into abdominal wall. Move fingers back and forth over abdominal contents. Use bimanual technique—exerting pressure with top hand and concentrating on sensation with bottom hand, as shown in figure below—if obesity or muscular resistance makes deep palpation difficult. To help determine whether masses are superficial or intraabdominal, have patient lift head from examining table to contract abdominal muscles and obscure intraabdominal masses. |
EXPECTED: Possible sensation of abdominal wall sliding back and forth. Possible awareness of borders of rectus abdominis muscles, aorta, and portions of colon. Possible tenderness over cecum, sigmoid colon, and aorta and in midline near xiphoid process. |
| UNEXPECTED: Bulges, masses, tenderness unrelated to deep palpation of cecum, sigmoid colon, aorta, xiphoid process. Note location, size, shape, consistency, tenderness, pulsation, mobility, movement (with respiration) of any masses. | |
| EXPECTED: Umbilical ring circular and free of irregularities. Umbilicus either slightly inverted or everted. | |
| UNEXPECTED: Bulges, nodules, granulation. Protruding umbilicus. | |
|
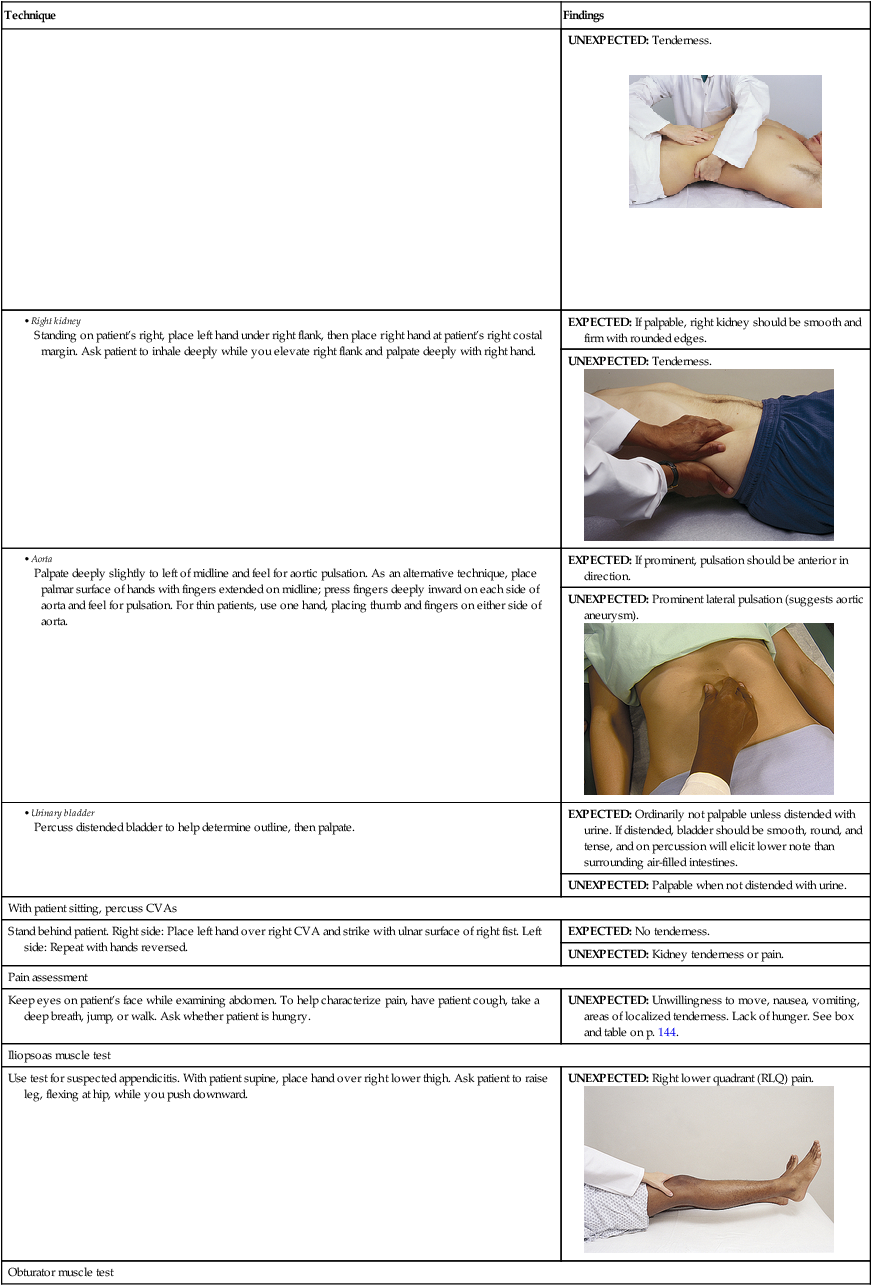
Place left hand under patient at eleventh and twelfth ribs, lifting to elevate liver toward abdominal wall. Place right hand on abdomen, fingers extended toward head with tips on right midclavicular line below level of liver dullness, as shown in figure at right. Alternatively, place right hand parallel to right costal margin, as shown in bottom figure at right. Press right hand gently but deeply in and up. Ask patient to breathe comfortably a few times and then take a deep breath. Feel for liver edge as diaphragm pushes it down. If palpable, repeat maneuver medially and laterally to costal margin. |
EXPECTED: Usually liver is not palpable. If felt, liver edge should be firm, smooth, even. |
UNEXPECTED: Tenderness, nodules, or irregularity.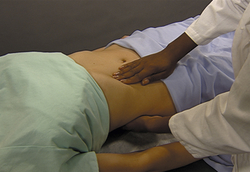  |
|
| EXPECTED: Gallbladder not palpable. | |
| UNEXPECTED: Palpable, tender. If tender (possible cholecystitis), palpate deeply during inspiration and observe for pain (Murphy sign). | |
|
Still standing on right side, reach across patient with left hand, place it beneath patient over left costovertebral angle (CVA), and lift spleen anteriorly toward abdominal wall. As shown in figure at right, place right hand on abdomen below left costal margin and—using findings from percussion—gently press fingertips inward toward spleen while asking patient to take a deep breath. Feel for spleen as it moves downward toward fingers. Repeat with patient lying on right side, as shown in bottom figure at right, with hips and knees flexed. Press inward with left hand while using fingertips of right hand to feel edge of spleen. |
EXPECTED: Spleen usually not palpable by either method. |
UNEXPECTED: Palpable spleen.  |
|
| EXPECTED: Left kidney usually not palpable. | |
UNEXPECTED: Tenderness.
 |
|
| EXPECTED: If palpable, right kidney should be smooth and firm with rounded edges. | |
UNEXPECTED: Tenderness. |
|
|
Palpate deeply slightly to left of midline and feel for aortic pulsation. As an alternative technique, place palmar surface of hands with fingers extended on midline; press fingers deeply inward on each side of aorta and feel for pulsation. For thin patients, use one hand, placing thumb and fingers on either side of aorta. |
EXPECTED: If prominent, pulsation should be anterior in direction. |
UNEXPECTED: Prominent lateral pulsation (suggests aortic aneurysm).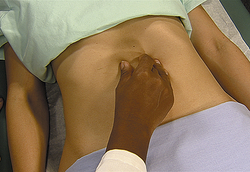 |
|
| EXPECTED: Ordinarily not palpable unless distended with urine. If distended, bladder should be smooth, round, and tense, and on percussion will elicit lower note than surrounding air-filled intestines. | |
| UNEXPECTED: Palpable when not distended with urine. | |
| With patient sitting, percuss CVAs | |
| Stand behind patient. Right side: Place left hand over right CVA and strike with ulnar surface of right fist. Left side: Repeat with hands reversed. | EXPECTED: No tenderness. |
| UNEXPECTED: Kidney tenderness or pain. | |
| Pain assessment | |
| Keep eyes on patient’s face while examining abdomen. To help characterize pain, have patient cough, take a deep breath, jump, or walk. Ask whether patient is hungry. | UNEXPECTED: Unwillingness to move, nausea, vomiting, areas of localized tenderness. Lack of hunger. See box and table on p. 144. |
| Iliopsoas muscle test | |
| Use test for suspected appendicitis. With patient supine, place hand over right lower thigh. Ask patient to raise leg, flexing at hip, while you push downward. | UNEXPECTED: Right lower quadrant (RLQ) pain. |
| Obturator muscle test | |
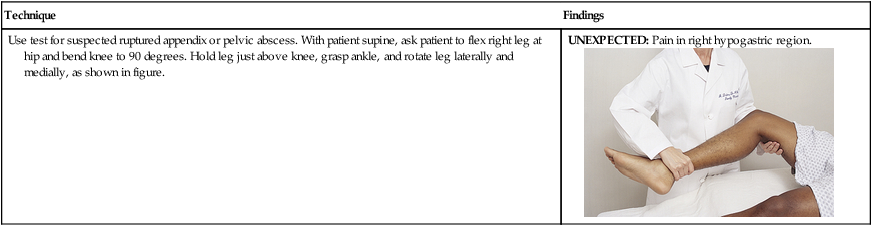
| Use test for suspected ruptured appendix or pelvic abscess. With patient supine, ask patient to flex right leg at hip and bend knee to 90 degrees. Hold leg just above knee, grasp ankle, and rotate leg laterally and medially, as shown in figure. | UNEXPECTED: Pain in right hypogastric region. |
(From Wilson and Giddens, 2009.)
Quality and Onset of Abdominal Pain
| Characteristic | Possible Related Condition |
| Burning | Peptic ulcer |
| Cramping | Biliary colic, gastroenteritis |
| Colic | Appendicitis with impacted feces; renal stone |
| Aching | Appendiceal irritation |
| Knife-like | Pancreatitis |
| Ripping, tearing | Aortic dissection |
| Gradual onset | Infection |
| Sudden onset | Duodenal ulcer, acute pancreatitis, obstruction, perforation |
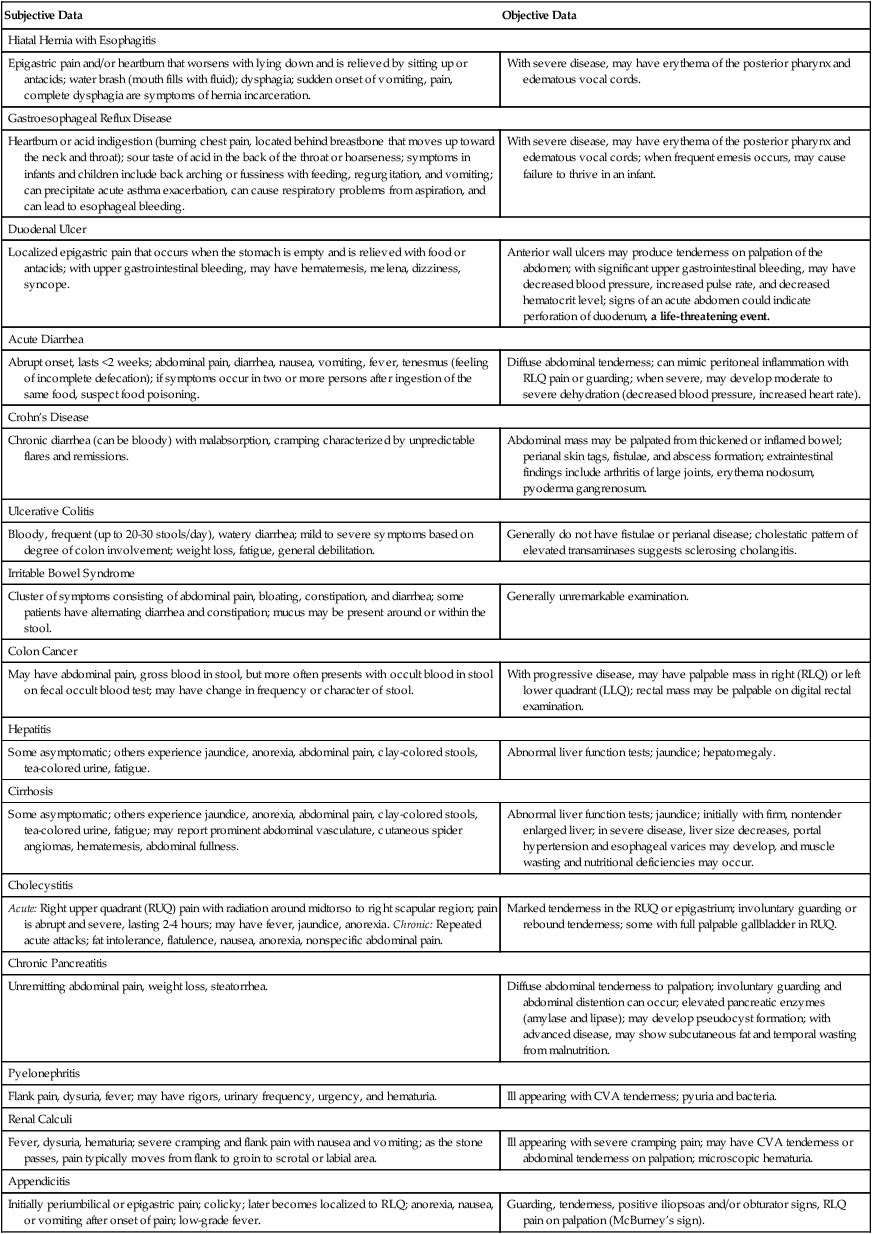
AIDS TO DIFFERENTIAL DIAGNOSIS
| Subjective Data | Objective Data |
| Hiatal Hernia with Esophagitis | |
| Epigastric pain and/or heartburn that worsens with lying down and is relieved by sitting up or antacids; water brash (mouth fills with fluid); dysphagia; sudden onset of vomiting, pain, complete dysphagia are symptoms of hernia incarceration. | With severe disease, may have erythema of the posterior pharynx and edematous vocal cords. |
| Gastroesophageal Reflux Disease | |
| Heartburn or acid indigestion (burning chest pain, located behind breastbone that moves up toward the neck and throat); sour taste of acid in the back of the throat or hoarseness; symptoms in infants and children include back arching or fussiness with feeding, regurgitation, and vomiting; can precipitate acute asthma exacerbation, can cause respiratory problems from aspiration, and can lead to esophageal bleeding. | With severe disease, may have erythema of the posterior pharynx and edematous vocal cords; when frequent emesis occurs, may cause failure to thrive in an infant. |
| Duodenal Ulcer | |
| Localized epigastric pain that occurs when the stomach is empty and is relieved with food or antacids; with upper gastrointestinal bleeding, may have hematemesis, melena, dizziness, syncope. | Anterior wall ulcers may produce tenderness on palpation of the abdomen; with significant upper gastrointestinal bleeding, may have decreased blood pressure, increased pulse rate, and decreased hematocrit level; signs of an acute abdomen could indicate perforation of duodenum, a life-threatening event. |
| Acute Diarrhea | |
| Abrupt onset, lasts <2 weeks; abdominal pain, diarrhea, nausea, vomiting, fever, tenesmus (feeling of incomplete defecation); if symptoms occur in two or more persons after ingestion of the same food, suspect food poisoning. | Diffuse abdominal tenderness; can mimic peritoneal inflammation with RLQ pain or guarding; when severe, may develop moderate to severe dehydration (decreased blood pressure, increased heart rate). |
| Crohn’s Disease | |
| Chronic diarrhea (can be bloody) with malabsorption, cramping characterized by unpredictable flares and remissions. | Abdominal mass may be palpated from thickened or inflamed bowel; perianal skin tags, fistulae, and abscess formation; extraintestinal findings include arthritis of large joints, erythema nodosum, pyoderma gangrenosum. |
| Ulcerative Colitis | |
| Bloody, frequent (up to 20-30 stools/day), watery diarrhea; mild to severe symptoms based on degree of colon involvement; weight loss, fatigue, general debilitation. | Generally do not have fistulae or perianal disease; cholestatic pattern of elevated transaminases suggests sclerosing cholangitis. |
| Irritable Bowel Syndrome | |
| Cluster of symptoms consisting of abdominal pain, bloating, constipation, and diarrhea; some patients have alternating diarrhea and constipation; mucus may be present around or within the stool. | Generally unremarkable examination. |
| Colon Cancer | |
| May have abdominal pain, gross blood in stool, but more often presents with occult blood in stool on fecal occult blood test; may have change in frequency or character of stool. | With progressive disease, may have palpable mass in right (RLQ) or left lower quadrant (LLQ); rectal mass may be palpable on digital rectal examination. |
| Hepatitis | |
| Some asymptomatic; others experience jaundice, anorexia, abdominal pain, clay-colored stools, tea-colored urine, fatigue. | Abnormal liver function tests; jaundice; hepatomegaly. |
| Cirrhosis | |
| Some asymptomatic; others experience jaundice, anorexia, abdominal pain, clay-colored stools, tea-colored urine, fatigue; may report prominent abdominal vasculature, cutaneous spider angiomas, hematemesis, abdominal fullness. | Abnormal liver function tests; jaundice; initially with firm, nontender enlarged liver; in severe disease, liver size decreases, portal hypertension and esophageal varices may develop, and muscle wasting and nutritional deficiencies may occur. |
| Cholecystitis | |
| Acute: Right upper quadrant (RUQ) pain with radiation around midtorso to right scapular region; pain is abrupt and severe, lasting 2-4 hours; may have fever, jaundice, anorexia. Chronic: Repeated acute attacks; fat intolerance, flatulence, nausea, anorexia, nonspecific abdominal pain. | Marked tenderness in the RUQ or epigastrium; involuntary guarding or rebound tenderness; some with full palpable gallbladder in RUQ. |
| Chronic Pancreatitis | |
| Unremitting abdominal pain, weight loss, steatorrhea. | Diffuse abdominal tenderness to palpation; involuntary guarding and abdominal distention can occur; elevated pancreatic enzymes (amylase and lipase); may develop pseudocyst formation; with advanced disease, may show subcutaneous fat and temporal wasting from malnutrition. |
| Pyelonephritis | |
| Flank pain, dysuria, fever; may have rigors, urinary frequency, urgency, and hematuria. | Ill appearing with CVA tenderness; pyuria and bacteria. |
| Renal Calculi | |
| Fever, dysuria, hematuria; severe cramping and flank pain with nausea and vomiting; as the stone passes, pain typically moves from flank to groin to scrotal or labial area. | Ill appearing with severe cramping pain; may have CVA tenderness or abdominal tenderness on palpation; microscopic hematuria. |
| Appendicitis | |
| Initially periumbilical or epigastric pain; colicky; later becomes localized to RLQ; anorexia, nausea, or vomiting after onset of pain; low-grade fever. | Guarding, tenderness, positive iliopsoas and/or obturator signs, RLQ pain on palpation (McBurney’s sign). |
Abdominal Signs Associated with Common Abnormal Conditions
| Sign | Description | Associated Conditions |
| Aaron | Pain or distress occurs in the area of patient’s heart or stomach on palpation of McBurney point | Appendicitis |
| Ballance | Fixed dullness to percussion in left flank and dullness in right flank that disappear on change of position | Peritoneal irritation |
| Blumberg | Rebound tenderness | Peritoneal irritation, appendicitis |
| Cullen | Ecchymosis around umbilicus | Hemoperitoneum, pancreatitis, ectopic pregnancy |
| Dance | Absence of bowel sounds in RLQ | Intussusception |
| Grey Turner | Ecchymosis of flanks | Hemoperitoneum, pancreatitis |
| Kehr | Abdominal pain radiating to left shoulder | Spleen rupture, renal calculi, ectopic pregnancy |
| Markle (heel jar) | Patient stands with straightened knees, then raises up on toes, relaxes, and allows heels to hit floor, thus jarring body; action will cause abdominal pain if positive | Peritoneal irritation, appendicitis |
| McBurney | Rebound tenderness and sharp pain when McBurney’s point is palpated (2艠3 the distance from the umbilicus to the anterior superior iliac spine) | Appendicitis |
| Murphy | Abrupt cessation of inspiration on palpation of gallbladder | Cholecystitis |
| Romberg-Howship | Pain down medial aspect of thigh to knees | Strangulated obturator hernia |
| Rovsing | RLQ pain intensified by left lower quadrant abdominal palpation | Peritoneal irritation, appendicitis |
Conditions That Produce Acute Abdominal Pain
| Condition | Usual Pain Characteristics | Possible Associated Findings |
| Appendicitis | Initially periumbilical or epigastric; colicky; later becomes localized to RLQ, often at McBurney’s point | Guarding, tenderness; positive iliopsoas and positive obturator tests, RLQ skin hyperesthesia; anorexia, nausea, or vomiting after onset of pain; low-grade fever; positive Aaron, Rovsing, Markle, and McBurney signs∗ |
| Peritonitis | Onset sudden or gradual; pain generalized or localized, dull or severe and unrelenting; guarding; pain on deep inspiration | Shallow respiration; positive Blumberg, Markle, and Ballance signs; reduced bowel sounds, nausea and vomiting; positive obturator and iliopsoas tests |
| Cholecystitis | Severe, unrelenting RUQ or epigastric pain; may be referred to right subscapular area | RUQ tenderness and rigidity, positive Murphy sign, palpable gallbladder, anorexia, vomiting, fever, possible jaundice |
| Pancreatitis | Dramatic, sudden, excruciating left upper quadrant (LUQ), epigastric, or umbilical pain; may be present in one or both flanks; may be referred to left shoulder | Epigastric tenderness, vomiting, fever, shock; positive Grey Turner sign; positive Cullen sign; both signs may occur 2-3 days after onset |
| Salpingitis | Lower quadrant, worse on left | Nausea, vomiting, fever, suprapubic tenderness, rigid abdomen, pain on pelvic examination |
| Pelvic inflammatory disease | Lower quadrant, increases with activity | Tender adnexa and cervix, cervical discharge, dyspareunia |
| Diverticulitis | Epigastric, radiating down left side of abdomen especially after eating; may be referred to back | Flatulence, borborygmi, diarrhea, dysuria, tenderness on palpation |
| Perforated gastric or duodenal ulcer | Abrupt RUQ; may be referred to shoulders | Abdominal free air and distention with increased resonance over liver; tenderness in epigastrium or RUQ; rigid abdominal wall, rebound tenderness |
| Intestinal obstruction | Abrupt, severe, spasmodic; referred to epigastrium, umbilicus | Distention, minimal rebound tenderness, vomiting, localized tenderness, visible peristalsis; bowel sounds absent (with paralytic obstruction) or hyperactive high-pitched (with mechanical obstruction) |
| Volvulus | Referred to hypogastrium and umbilicus | Distention, nausea, vomiting, guarding; sigmoid loop volvulus may be palpable |
| Leaking abdominal aneurysm | Steady throbbing midline over aneurysm; may penetrate to back, flank | Nausea, vomiting, abdominal mass, bruit |
| Biliary stones, colic | Episodic, severe, RUQ, or epigastrium lasting 15 min to several hours; may be referred to subscapular area, especially right | RUQ tenderness, soft abdominal wall, anorexia, vomiting, jaundice, subnormal temperature |
| Renal calculi | Intense; flank, extending to groin and genitals; may be episodic | Fever, hematuria; positive Kehr sign |
| Ectopic pregnancy | Lower quadrant; referred to shoulder; with rupture is agonizing | Hypogastric tenderness, symptoms of pregnancy, spotting, irregular menses, soft abdominal wall, mass on bimanual pelvic examination; ruptured: shock, rigid abdominal wall, distention; positive Kehr, Cullen signs |
| Ruptured ovarian cyst | Lower quadrant, steady, increases with cough or motion | Vomiting, low-grade fever, anorexia, tenderness on pelvic examination |
| Splenic rupture | Intense; LUQ, radiating to left shoulder; may worsen with foot of bed elevated | Shock, pallor, lowered temperature |
∗See table on pp. 148-149 for explanation of signs.
Conditions That Produce Chronic Abdominal Pain
| Condition | Usual Pain Characteristics | Possible Associated Findings |
| Irritable bowel syndrome | Hypogastric pain; crampy, variable, infrequent; associated with bowel function | Unremarkable physical examination; pain associated with gas, bloating, distention; relief with passage of flatus, feces |
| Lactose intolerance | Crampy pain after drinking milk or eating milk products | Associated diarrhea; unremarkable physical examination |
| Diverticular disease | Localized pain | Abdominal tenderness, fever |
| Constipation | Colicky or dull and steady pain that does not progress or worsen | Fecal mass palpable, stool in rectum |
| Uterine fibroids | Pain related to menses, intercourse | Palpable myoma(s) |
| Hernia | Localized pain that increases with exertion or lifting | Hernia on physical examination |
| Esophagitis/gastroesophageal reflux disease | Burning, gnawing pain in midepigastrium, worsens with recumbency | Unremarkable physical examination |
| Peptic ulcer | Burning or gnawing pain | May have epigastric tenderness on palpation |
| Gastritis | Constant burning pain in epigastrium | May be accompanied by nausea, vomiting, diarrhea, or fever; unremarkable physical examination |
Modified from Dains et al, 2011. Advanced Health Assessment & Clinical Diagnosis in Primary Care (Mosby) – Trade paperback (2011) by Joyce E Dains, Linda Ciofu Baumann, Pamela Scheibel.
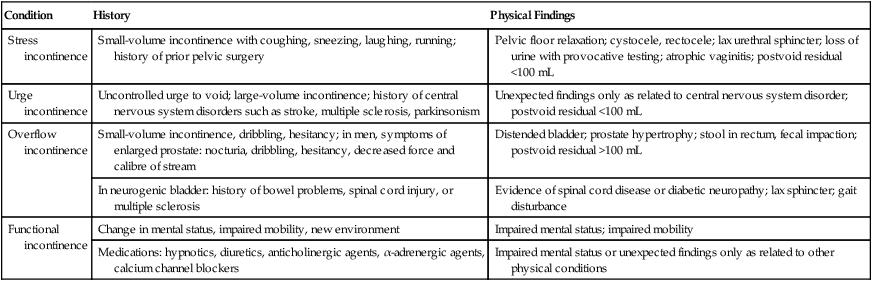
Differential Diagnosis of Urinary Incontinence
| Condition | History | Physical Findings |
| Stress incontinence | Small-volume incontinence with coughing, sneezing, laughing, running; history of prior pelvic surgery | Pelvic floor relaxation; cystocele, rectocele; lax urethral sphincter; loss of urine with provocative testing; atrophic vaginitis; postvoid residual <100 mL |
| Urge incontinence | Uncontrolled urge to void; large-volume incontinence; history of central nervous system disorders such as stroke, multiple sclerosis, parkinsonism | Unexpected findings only as related to central nervous system disorder; postvoid residual <100 mL |
| Overflow incontinence | Small-volume incontinence, dribbling, hesitancy; in men, symptoms of enlarged prostate: nocturia, dribbling, hesitancy, decreased force and calibre of stream | Distended bladder; prostate hypertrophy; stool in rectum, fecal impaction; postvoid residual >100 mL |
| In neurogenic bladder: history of bowel problems, spinal cord injury, or multiple sclerosis | Evidence of spinal cord disease or diabetic neuropathy; lax sphincter; gait disturbance | |
| Functional incontinence | Change in mental status, impaired mobility, new environment | Impaired mental status; impaired mobility |
| Medications: hypnotics, diuretics, anticholinergic agents, α-adrenergic agents, calcium channel blockers | Impaired mental status or unexpected findings only as related to other physical conditions |
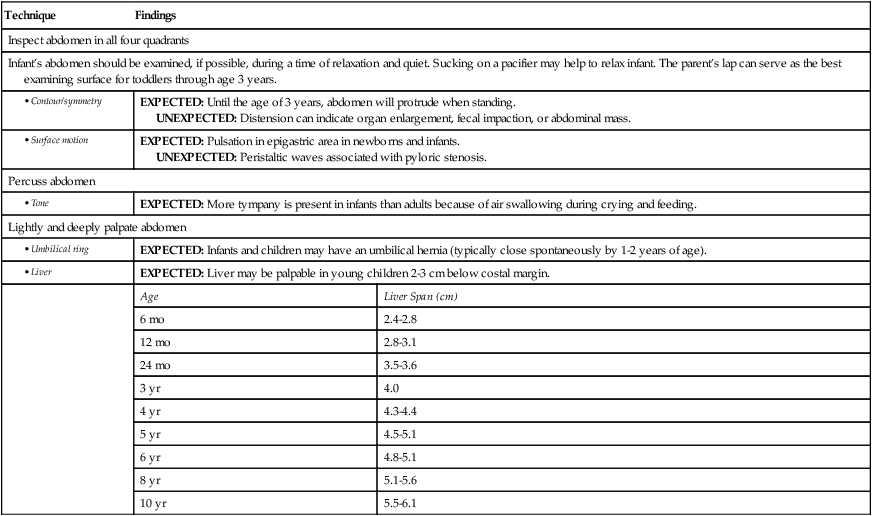
PEDIATRIC VARIATIONS
EXAMINATION
| Technique | Findings | |
| Inspect abdomen in all four quadrants | ||
| Infant’s abdomen should be examined, if possible, during a time of relaxation and quiet. Sucking on a pacifier may help to relax infant. The parent’s lap can serve as the best examining surface for toddlers through age 3 years. | ||
| EXPECTED: Until the age of 3 years, abdomen will protrude when standing. UNEXPECTED: Distension can indicate organ enlargement, fecal impaction, or abdominal mass. |
||
| EXPECTED: Pulsation in epigastric area in newborns and infants. UNEXPECTED: Peristaltic waves associated with pyloric stenosis. |
||
| Percuss abdomen | ||
| EXPECTED: More tympany is present in infants than adults because of air swallowing during crying and feeding. | ||
| Lightly and deeply palpate abdomen | ||
| EXPECTED: Infants and children may have an umbilical hernia (typically close spontaneously by 1-2 years of age). | ||
| EXPECTED: Liver may be palpable in young children 2-3 cm below costal margin. | ||
| Age | Liver Span (cm) | |
| 6 mo | 2.4-2.8 | |
| 12 mo | 2.8-3.1 | |
| 24 mo | 3.5-3.6 | |
| 3 yr | 4.0 | |
| 4 yr | 4.3-4.4 | |
| 5 yr | 4.5-5.1 | |
| 6 yr | 4.8-5.1 | |
| 8 yr | 5.1-5.6 | |
| 10 yr | 5.5-6.1 | |
Sample Documentation
Subjective
A 44-year-old woman describes a burning sensation in epigastric area and chest. Occurs after eating, especially with spicy foods. Lasts 1 to 2 hours and is worse when lying down. Sometimes causes bitter taste in mouth. Also feels bloated. Antacids do not relieve symptoms. Denies nausea/vomiting/diarrhea. No cough or shortness of breath.
Objective
Abdomen rounded and symmetric, with white striae adjacent to umbilicus in all quadrants. A well-healed, 5-cm, white surgical scar evident in RLQ. No areas of visible pulsations or peristalsis. Active bowel sounds audible. Percussion tones tympanic over epigastrium. Liver span 8 cm at right midclavicular line. On inspiration, liver edge firm, smooth, and nontender. No splenomegaly. Musculature soft and relaxed to light palpation. No masses or areas of tenderness to deep palpation. No CVA tenderness.