Musculoskeletal System
Examination
Begin examination as patient enters rooms, observing gait and posture. During examination, note ease of movement when patient walks, sits, rises, takes off garments, and responds to directions.
| Technique | Findings |
| Posture and General Guidelines | |
| Inspect skeleton and extremities, comparing sides | |
| Inspect anterior, posterior, lateral aspects of posture; ability to stand erect; body parts; extremities. | |
| EXPECTED: Bilateral symmetry of length, circumference, alignment, position and number of skinfolds; symmetric body parts; and aligned extremities. | |
| UNEXPECTED: Gross deformity, lordosis, kyphosis, scoliosis, bony enlargement. | |
| Inspect skin and subcutaneous tissues over muscles, cartilage, bones, joints | |
| UNEXPECTED: Discoloration, swelling, or masses. | |
| Inspect muscles and compare sides | |
| EXPECTED: Approximately symmetric bilateral muscle size. | |
| UNEXPECTED: Gross hypertrophy or atrophy, fasciculations, or spasms. | |
| Palpate all bones, joints, surrounding muscles (palpate inflamed joints last) | |
| EXPECTED: Firm. | |
| UNEXPECTED: Hard or doughy, spasticity. | |
| UNEXPECTED: Heat, tenderness, swelling, fluctuation of a joint, synovial thickening, crepitus, resistance to pressure, or discomfort to pressure on bones and joints. | |
| Test each major joint and related muscle groups for active and passive range of motion, and compare sides | |
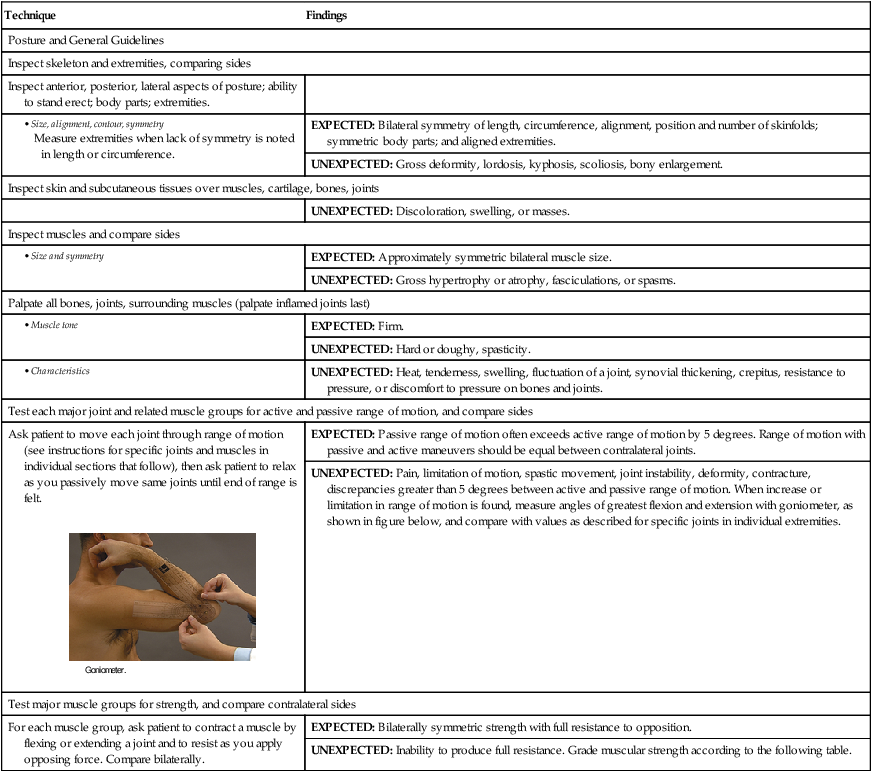
| Ask patient to move each joint through range of motion (see instructions for specific joints and muscles in individual sections that follow), then ask patient to relax as you passively move same joints until end of range is felt. | EXPECTED: Passive range of motion often exceeds active range of motion by 5 degrees. Range of motion with passive and active maneuvers should be equal between contralateral joints. |
| UNEXPECTED: Pain, limitation of motion, spastic movement, joint instability, deformity, contracture, discrepancies greater than 5 degrees between active and passive range of motion. When increase or limitation in range of motion is found, measure angles of greatest flexion and extension with goniometer, as shown in figure below, and compare with values as described for specific joints in individual extremities. | |
| Test major muscle groups for strength, and compare contralateral sides | |
| For each muscle group, ask patient to contract a muscle by flexing or extending a joint and to resist as you apply opposing force. Compare bilaterally. | EXPECTED: Bilaterally symmetric strength with full resistance to opposition. |
| UNEXPECTED: Inability to produce full resistance. Grade muscular strength according to the following table. | |
| Muscle Function Level | Grade |
| No evidence of contractility | 0 |
| Slight contractility, no movement | 1 |
| Full range of motion, gravity eliminated∗ | 2 |
| Full range of motion against gravity | 3 |
| Full range of motion against gravity, some resistance | 4 |
| Full range of motion against gravity, full resistance | 5 |
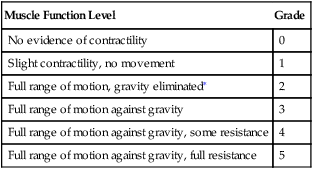
∗Passive movement.
(From Jacobson RD: Approach to the child with weakness and clumsiness, Pediatr Clin North Am 45[1]:145-168. 1998.)
| Technique | Findings |
| Hands and Wrists | |
| Inspect dorsum and palm of each hand | |
| EXPECTED: Palmar and phalangeal creases, palmar surfaces with central depression with prominent, rounded mound on thumb side (thenar eminence) and less prominent hypothenar eminence on little-finger side. | |
| EXPECTED: Fingers able to fully extend and align with forearm when in close approximation to each other. | |
| UNEXPECTED: Deviation of fingers to ulnar side or inability to fully extend fingers; swan neck or boutonnière deformities. | |
| EXPECTED: Lateral finger surfaces gradually tapered from proximal to distal aspects. | |
| UNEXPECTED: Spindle-shaped fingers, bony overgrowths at phalangeal joints. | |
| Palpate each joint in hand and wrist | |
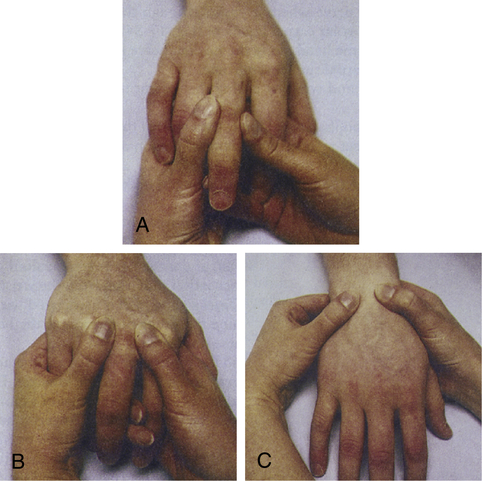
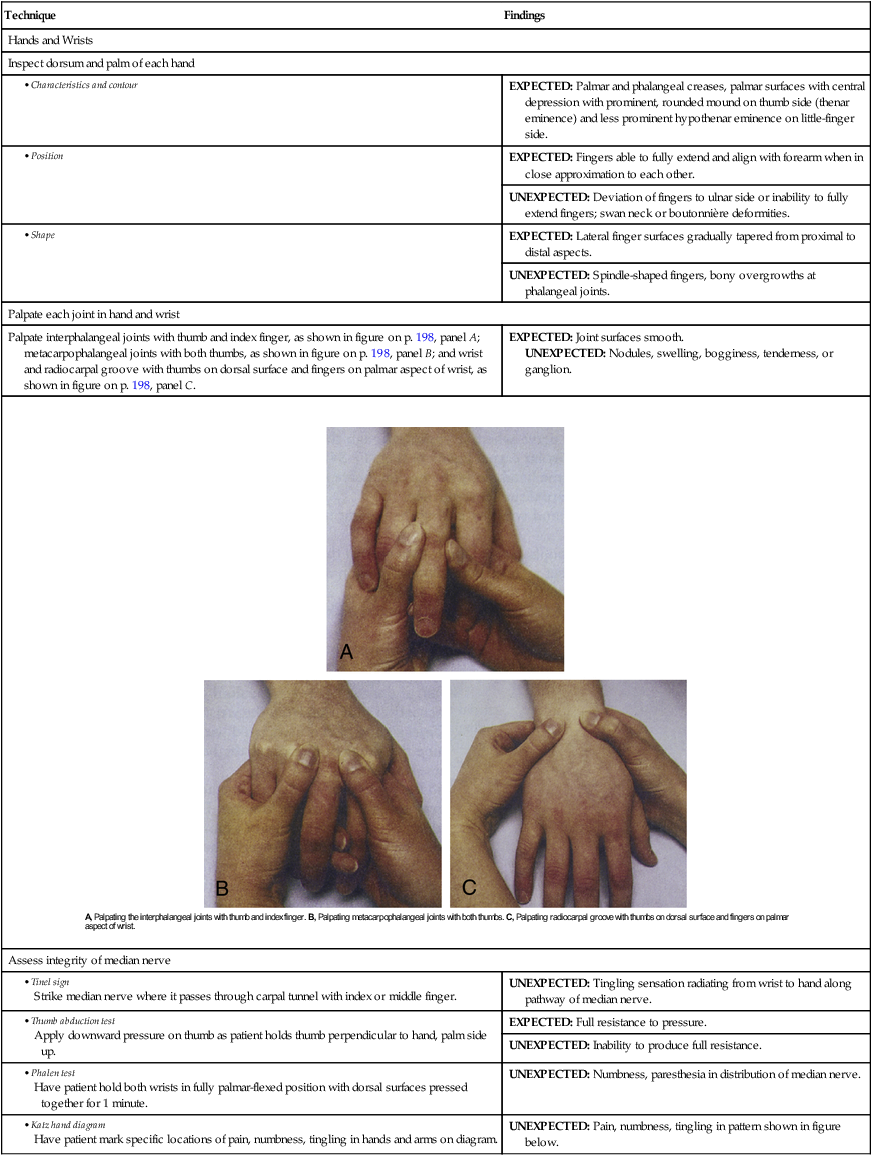
| Palpate interphalangeal joints with thumb and index finger, as shown in figure on p. 198, panel A; metacarpophalangeal joints with both thumbs, as shown in figure on p. 198, panel B; and wrist and radiocarpal groove with thumbs on dorsal surface and fingers on palmar aspect of wrist, as shown in figure on p. 198, panel C. | EXPECTED: Joint surfaces smooth. UNEXPECTED: Nodules, swelling, bogginess, tenderness, or ganglion. |
| Assess integrity of median nerve | |
| UNEXPECTED: Tingling sensation radiating from wrist to hand along pathway of median nerve. | |
| EXPECTED: Full resistance to pressure. | |
| UNEXPECTED: Inability to produce full resistance. | |
| UNEXPECTED: Numbness, paresthesia in distribution of median nerve. | |
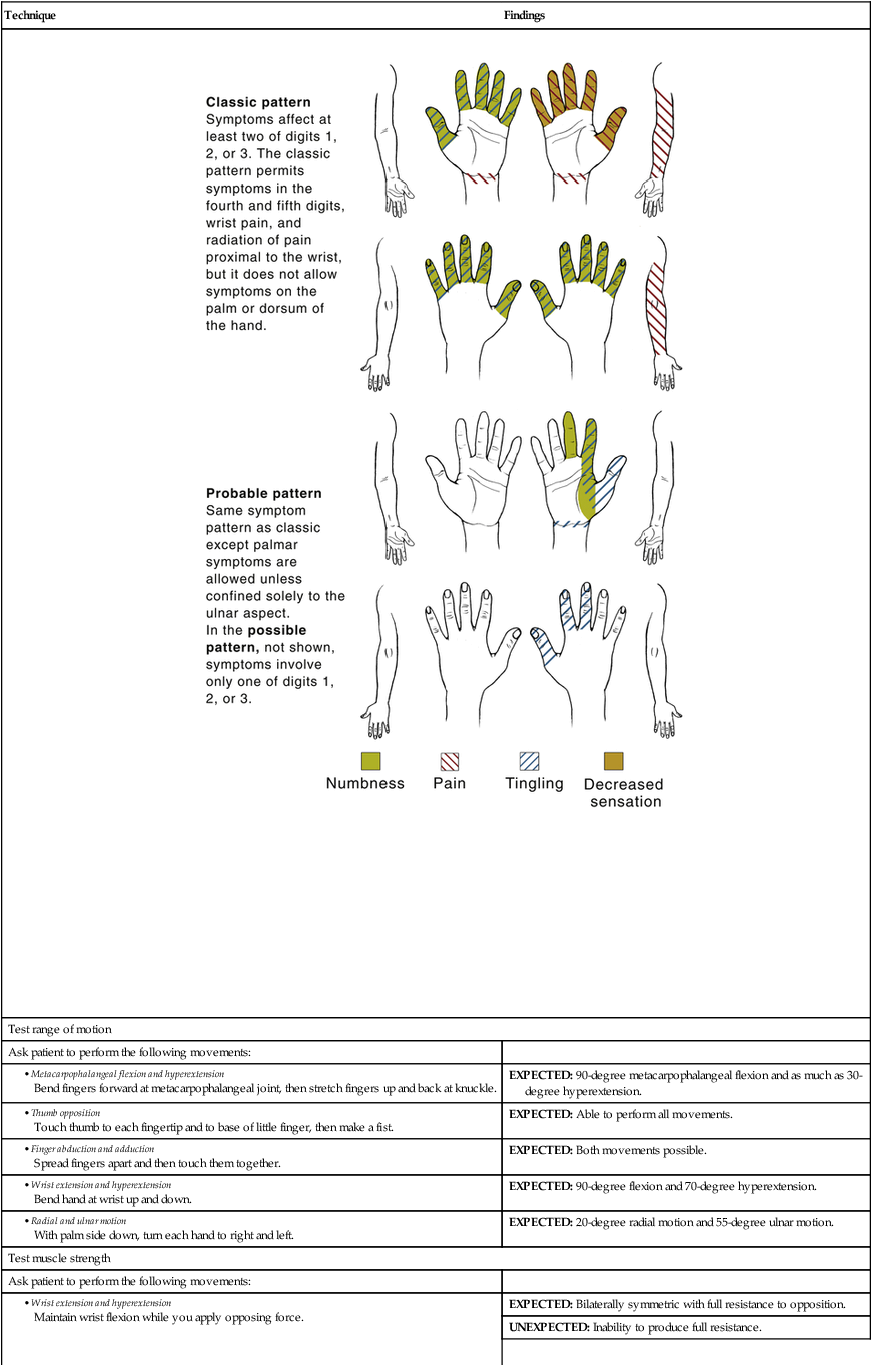
| UNEXPECTED: Pain, numbness, tingling in pattern shown in figure below. | |
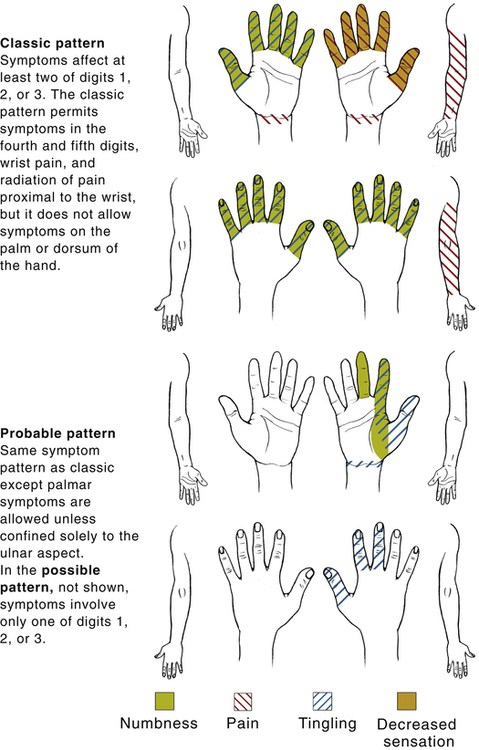 |
|
| Test range of motion | |
| Ask patient to perform the following movements: | |
| EXPECTED: 90-degree metacarpophalangeal flexion and as much as 30-degree hyperextension. | |
| EXPECTED: Able to perform all movements. | |
| EXPECTED: Both movements possible. | |
| EXPECTED: 90-degree flexion and 70-degree hyperextension. | |
| EXPECTED: 20-degree radial motion and 55-degree ulnar motion. | |
| Test muscle strength | |
| Ask patient to perform the following movements: | |
| EXPECTED: Bilaterally symmetric with full resistance to opposition. | |
| UNEXPECTED: Inability to produce full resistance. | |
| EXPECTED: Firm, sustained grip. | |
| UNEXPECTED: Weakness or pain. | |
| Elbows | |
| Inspect elbows in flexed and extended positions | |
| UNEXPECTED: Subcutaneous nodules along pressure points of extensor surface of ulna. | |
| EXPECTED: Usually 5 to 15 degrees laterally. | |
| UNEXPECTED: Lateral angle exceeding 15 degrees (cubitus valgus) or a medial carrying angle (cubitus varus). | |
| Palpate extensor surface of ulna, olecranon process, medial and lateral epicondyles of humerus, groove on each side of olecranon process | |
| Palpate with patient’s elbow flexed at 70 degrees. | UNEXPECTED: Boggy, soft, tenderness at lateral epicondyle or along grooves of olecranon process and epicondyles. |
| Test range of motion | |
| Ask patient to perform the following movements: | |
| EXPECTED: 160-degree flexion from full extension at 0 degrees. | |
| EXPECTED: 90-degree pronation and 90-degree supination. | |
| UNEXPECTED: Increased pain with pronation and supination of elbow. | |
| Test muscle strength | |
| Ask patient to maintain flexion and extension, as well as pronation and supination, while you apply opposing force. | EXPECTED: Bilaterally symmetric with full resistance to opposition. |
| UNEXPECTED: Inability to produce full resistance. | |
| Shoulders | |
| Inspect shoulders, shoulder girdle, clavicles and scapulae, area muscles | |
| EXPECTED: All shoulder structures symmetric in size and contour. | |
| UNEXPECTED: Asymmetry, hollows in rounding contour, or winged scapula. | |
| Palpate sternoclavicular and acromioclavicular joints, clavicle, scapulae, coracoid process, greater trochanter of humerus, biceps groove, area muscles | |
| Palpate the biceps groove by rotating the arm and forearm externally. Follow the biceps muscle and tendon along the anterior aspect of the humerus into the biceps groove. | EXPECTED: No tenderness or masses, bilateral symmetry. |
| Palpate the muscle insertion for the supraspinatus, infraspinatus, and teres minor near the greater tuberosity of the humerus by lifting the elbow posteriorly to extend the shoulder. | UNEXPECTED: Pain, tenderness, mass. |
| Test range of motion | |
| Ask patient to perform the following movements: | |
| EXPECTED: Symmetric rising. | |
| EXPECTED: 180-degree forward flexion. | |
| EXPECTED: 50-degree hyperextension. | |
| EXPECTED: 180-degree abduction. | |
| EXPECTED: 50-degree adduction. | |
| EXPECTED: 90-degree internal rotation. | |
| EXPECTED: 90-degree external rotation. | |
| Test shoulder girdle muscle strength | |
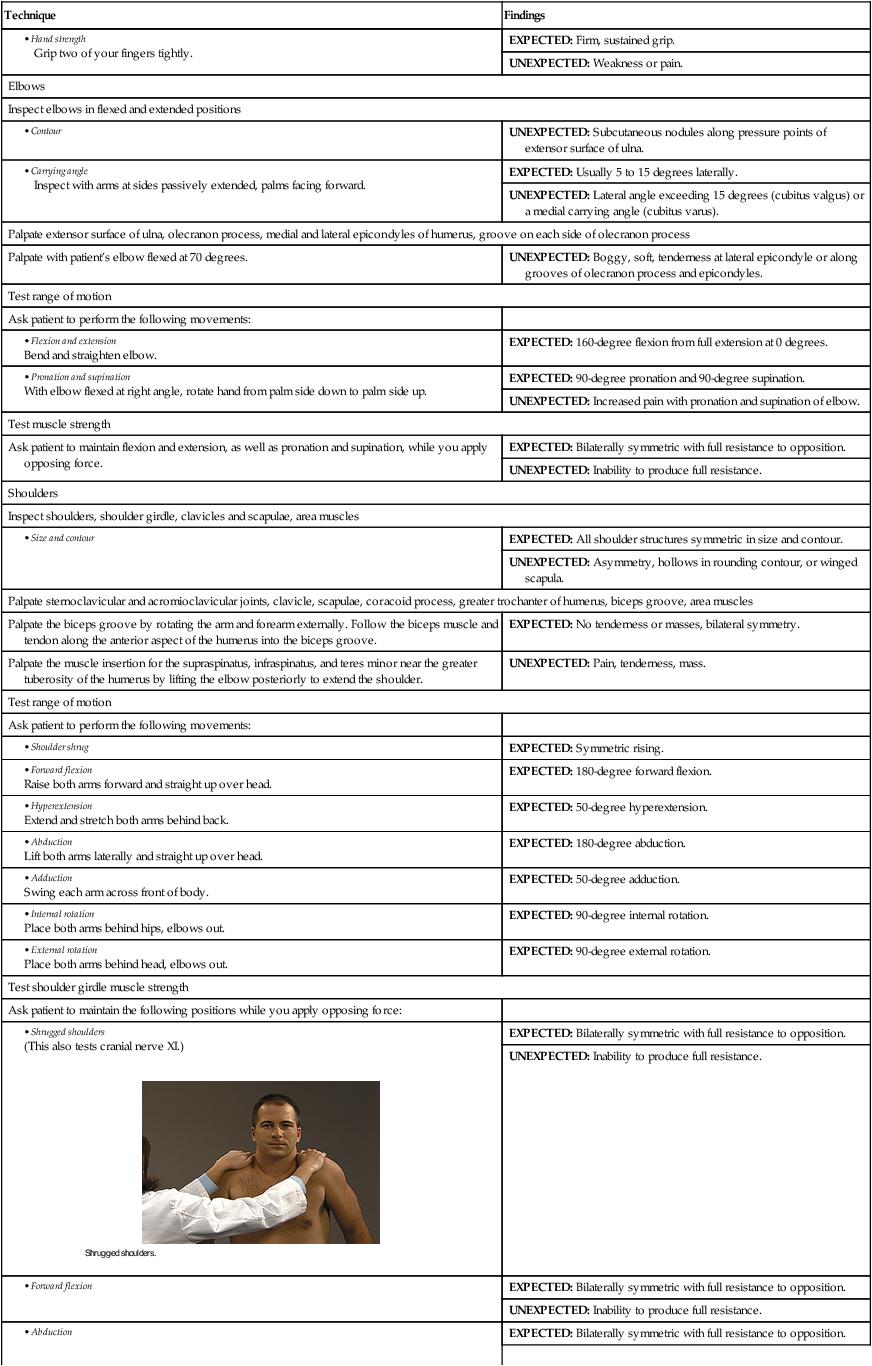
| Ask patient to maintain the following positions while you apply opposing force: | |
| EXPECTED: Bilaterally symmetric with full resistance to opposition. | |
| UNEXPECTED: Inability to produce full resistance. | |
| EXPECTED: Bilaterally symmetric with full resistance to opposition. | |
| UNEXPECTED: Inability to produce full resistance. | |
| EXPECTED: Bilaterally symmetric with full resistance to opposition. | |
| UNEXPECTED: Inability to produce full resistance. | |
| Assess rotator cuff muscles | |
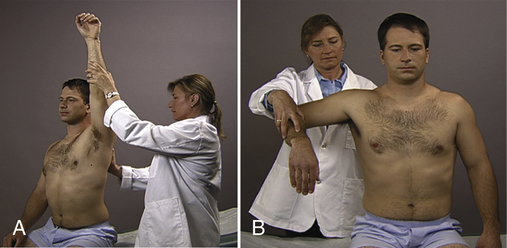
| Abduct the arm 90 degrees and flex the shoulders forward 30 degrees to test the supraspinatus muscle. Apply downward pressure on the distal humerus when the arm is rotated so that thumb points down or up. | UNEXPECTED: Pain and weakness with opposing force. |
| Flex the elbow 90 degrees and rotate the forearm medially against resistance to test the subscapularis muscle. | UNEXPECTED: Pain and weakness with opposing force. |
| With the arm at the side and elbow flexed 90 degrees, rotate the arm laterally against resistance to test the infraspinatus and teres minor muscles. | UNEXPECTED: Pain and weakness with opposing force. |
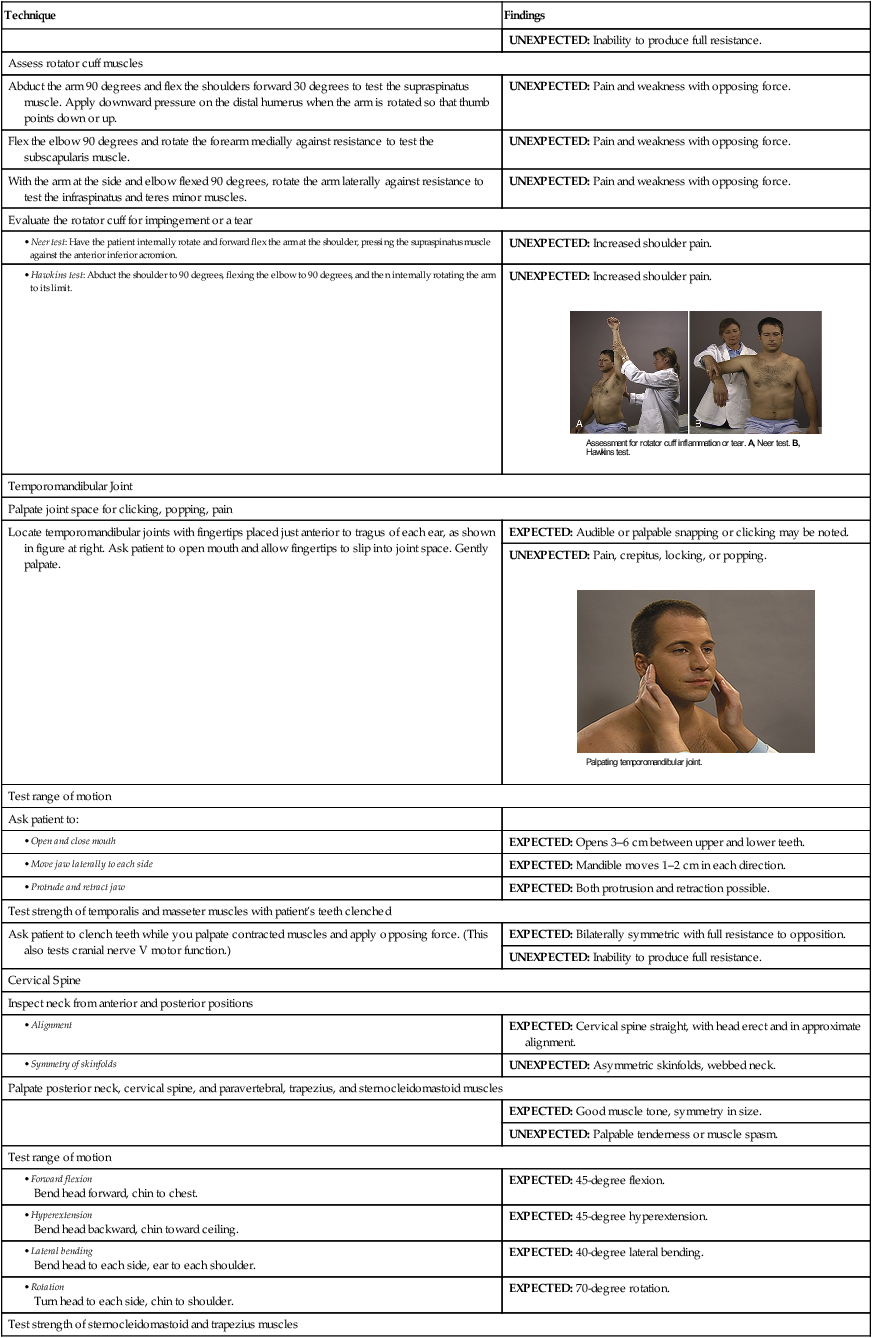
| Evaluate the rotator cuff for impingement or a tear | |
| UNEXPECTED: Increased shoulder pain. | |
| UNEXPECTED: Increased shoulder pain. | |
| Temporomandibular Joint | |
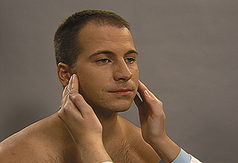
| Palpate joint space for clicking, popping, pain | |
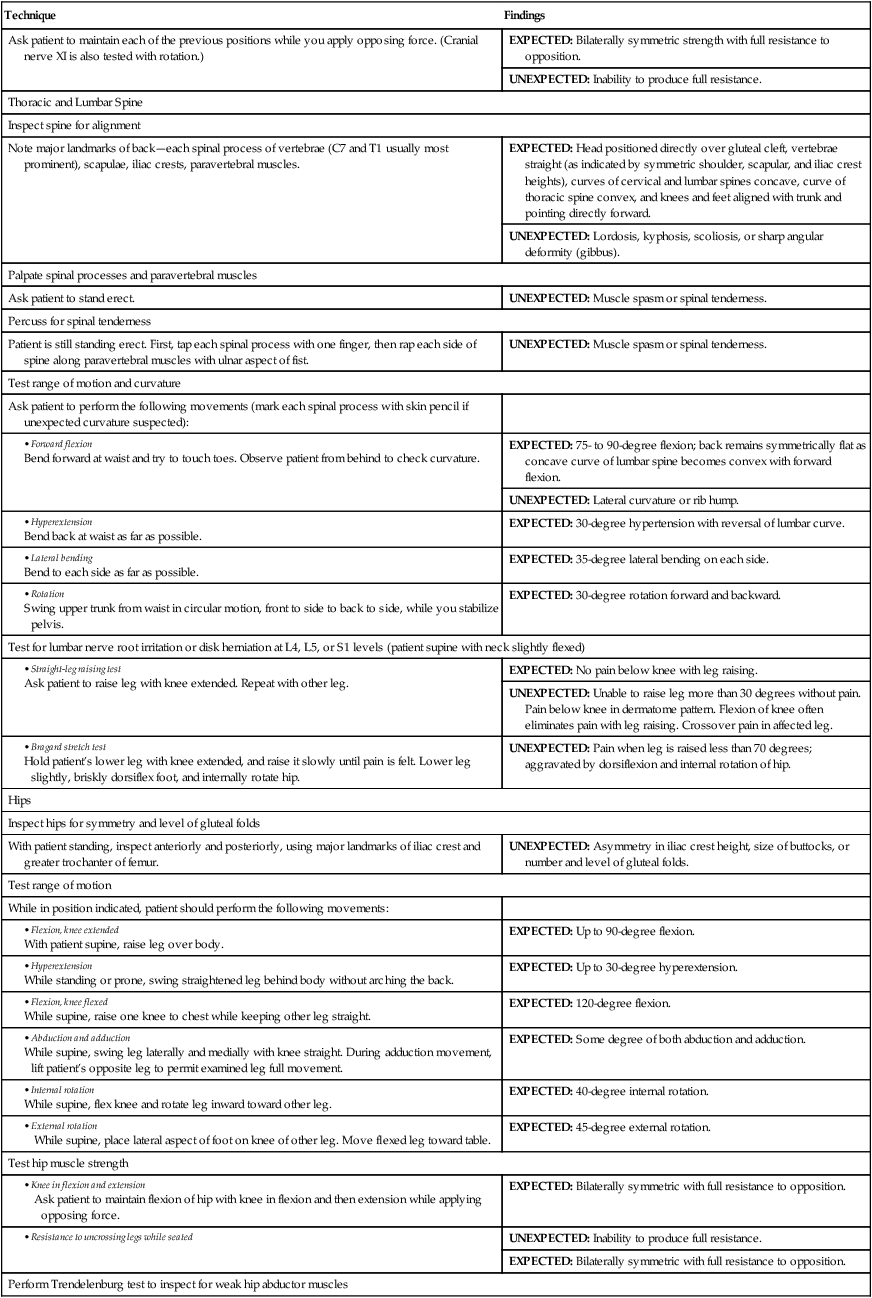
| Locate temporomandibular joints with fingertips placed just anterior to tragus of each ear, as shown in figure at right. Ask patient to open mouth and allow fingertips to slip into joint space. Gently palpate. | EXPECTED: Audible or palpable snapping or clicking may be noted. |
| UNEXPECTED: Pain, crepitus, locking, or popping. | |
| Test range of motion | |
| Ask patient to: | |
| EXPECTED: Opens 3–6 cm between upper and lower teeth. | |
| EXPECTED: Mandible moves 1–2 cm in each direction. | |
| EXPECTED: Both protrusion and retraction possible. | |
| Test strength of temporalis and masseter muscles with patient’s teeth clenched | |
| Ask patient to clench teeth while you palpate contracted muscles and apply opposing force. (This also tests cranial nerve V motor function.) | EXPECTED: Bilaterally symmetric with full resistance to opposition. |
| UNEXPECTED: Inability to produce full resistance. | |
| Cervical Spine | |
| Inspect neck from anterior and posterior positions | |
| EXPECTED: Cervical spine straight, with head erect and in approximate alignment. | |
| UNEXPECTED: Asymmetric skinfolds, webbed neck. | |
| Palpate posterior neck, cervical spine, and paravertebral, trapezius, and sternocleidomastoid muscles | |
| EXPECTED: Good muscle tone, symmetry in size. | |
| UNEXPECTED: Palpable tenderness or muscle spasm. | |
| Test range of motion | |
| EXPECTED: 45-degree flexion. | |
| EXPECTED: 45-degree hyperextension. | |
| EXPECTED: 40-degree lateral bending. | |
| EXPECTED: 70-degree rotation. | |
| Test strength of sternocleidomastoid and trapezius muscles | |
| Ask patient to maintain each of the previous positions while you apply opposing force. (Cranial nerve XI is also tested with rotation.) | EXPECTED: Bilaterally symmetric strength with full resistance to opposition. |
| UNEXPECTED: Inability to produce full resistance. | |
| Thoracic and Lumbar Spine | |
| Inspect spine for alignment | |
| Note major landmarks of back—each spinal process of vertebrae (C7 and T1 usually most prominent), scapulae, iliac crests, paravertebral muscles. | EXPECTED: Head positioned directly over gluteal cleft, vertebrae straight (as indicated by symmetric shoulder, scapular, and iliac crest heights), curves of cervical and lumbar spines concave, curve of thoracic spine convex, and knees and feet aligned with trunk and pointing directly forward. |
| UNEXPECTED: Lordosis, kyphosis, scoliosis, or sharp angular deformity (gibbus). | |
| Palpate spinal processes and paravertebral muscles | |
| Ask patient to stand erect. | UNEXPECTED: Muscle spasm or spinal tenderness. |
| Percuss for spinal tenderness | |
| Patient is still standing erect. First, tap each spinal process with one finger, then rap each side of spine along paravertebral muscles with ulnar aspect of fist. | UNEXPECTED: Muscle spasm or spinal tenderness. |
| Test range of motion and curvature | |
| Ask patient to perform the following movements (mark each spinal process with skin pencil if unexpected curvature suspected): | |
| EXPECTED: 75- to 90-degree flexion; back remains symmetrically flat as concave curve of lumbar spine becomes convex with forward flexion. | |
| UNEXPECTED: Lateral curvature or rib hump. | |
| EXPECTED: 30-degree hypertension with reversal of lumbar curve. | |
| EXPECTED: 35-degree lateral bending on each side. | |
| EXPECTED: 30-degree rotation forward and backward. | |
| Test for lumbar nerve root irritation or disk herniation at L4, L5, or S1 levels (patient supine with neck slightly flexed) | |
| EXPECTED: No pain below knee with leg raising. | |
| UNEXPECTED: Unable to raise leg more than 30 degrees without pain. Pain below knee in dermatome pattern. Flexion of knee often eliminates pain with leg raising. Crossover pain in affected leg. | |
| UNEXPECTED: Pain when leg is raised less than 70 degrees; aggravated by dorsiflexion and internal rotation of hip. | |
| Hips | |
| Inspect hips for symmetry and level of gluteal folds | |
| With patient standing, inspect anteriorly and posteriorly, using major landmarks of iliac crest and greater trochanter of femur. | UNEXPECTED: Asymmetry in iliac crest height, size of buttocks, or number and level of gluteal folds. |
| Test range of motion | |
| While in position indicated, patient should perform the following movements: | |
| EXPECTED: Up to 90-degree flexion. | |
| EXPECTED: Up to 30-degree hyperextension. | |
| EXPECTED: 120-degree flexion. | |
| EXPECTED: Some degree of both abduction and adduction. | |
| EXPECTED: 40-degree internal rotation. | |
| EXPECTED: 45-degree external rotation. | |
| Test hip muscle strength | |
| EXPECTED: Bilaterally symmetric with full resistance to opposition. | |
| UNEXPECTED: Inability to produce full resistance. | |
| EXPECTED: Bilaterally symmetric with full resistance to opposition. | |
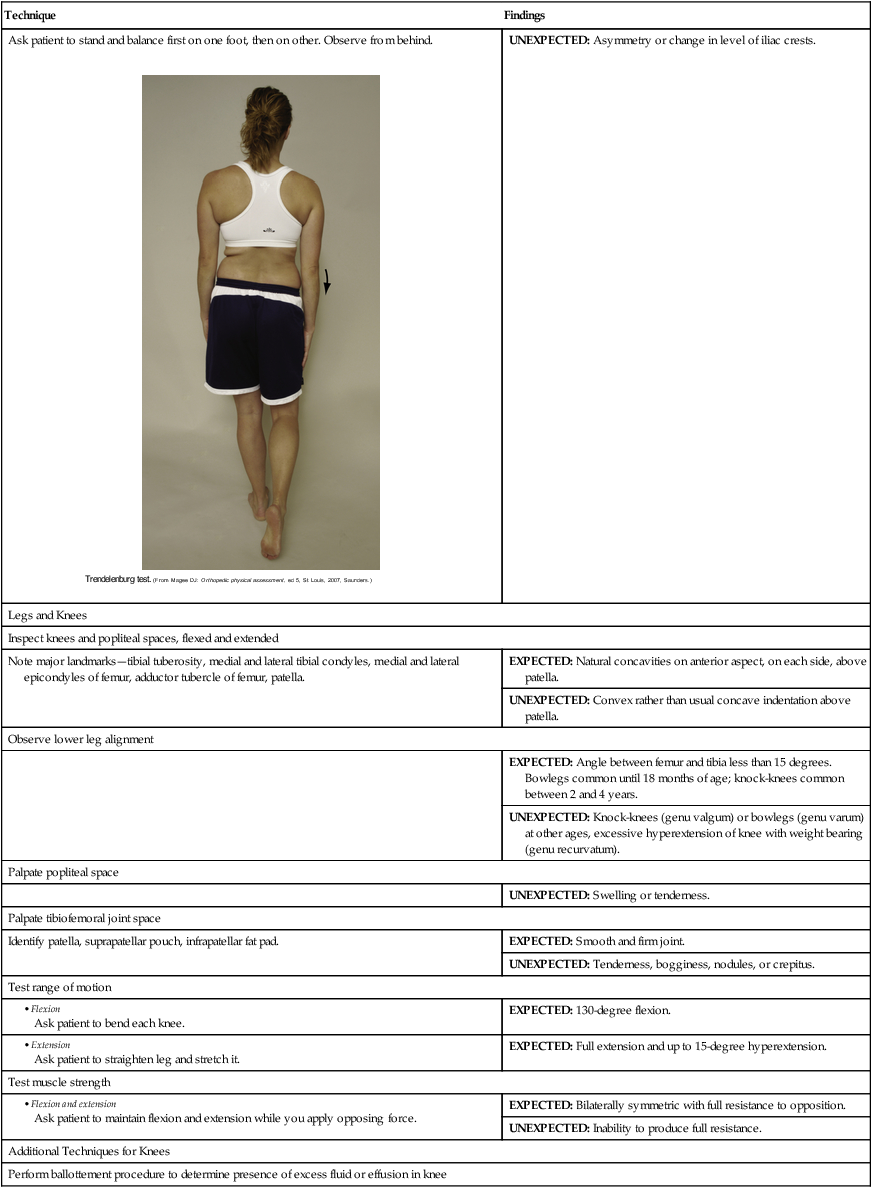
| Perform Trendelenburg test to inspect for weak hip abductor muscles | |
| Ask patient to stand and balance first on one foot, then on other. Observe from behind. | UNEXPECTED: Asymmetry or change in level of iliac crests. |
| Legs and Knees | |
| Inspect knees and popliteal spaces, flexed and extended | |
| Note major landmarks—tibial tuberosity, medial and lateral tibial condyles, medial and lateral epicondyles of femur, adductor tubercle of femur, patella. | EXPECTED: Natural concavities on anterior aspect, on each side, above patella. |
| UNEXPECTED: Convex rather than usual concave indentation above patella. | |
| Observe lower leg alignment | |
| EXPECTED: Angle between femur and tibia less than 15 degrees. Bowlegs common until 18 months of age; knock-knees common between 2 and 4 years. | |
| UNEXPECTED: Knock-knees (genu valgum) or bowlegs (genu varum) at other ages, excessive hyperextension of knee with weight bearing (genu recurvatum). | |
| Palpate popliteal space | |
| UNEXPECTED: Swelling or tenderness. | |
| Palpate tibiofemoral joint space | |
| Identify patella, suprapatellar pouch, infrapatellar fat pad. | EXPECTED: Smooth and firm joint. |
| UNEXPECTED: Tenderness, bogginess, nodules, or crepitus. | |
| Test range of motion | |
| EXPECTED: 130-degree flexion. | |
| EXPECTED: Full extension and up to 15-degree hyperextension. | |
| Test muscle strength | |
| EXPECTED: Bilaterally symmetric with full resistance to opposition. | |
| UNEXPECTED: Inability to produce full resistance. | |
| Additional Techniques for Knees | |
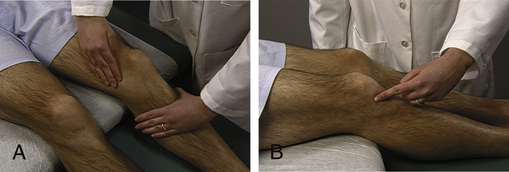
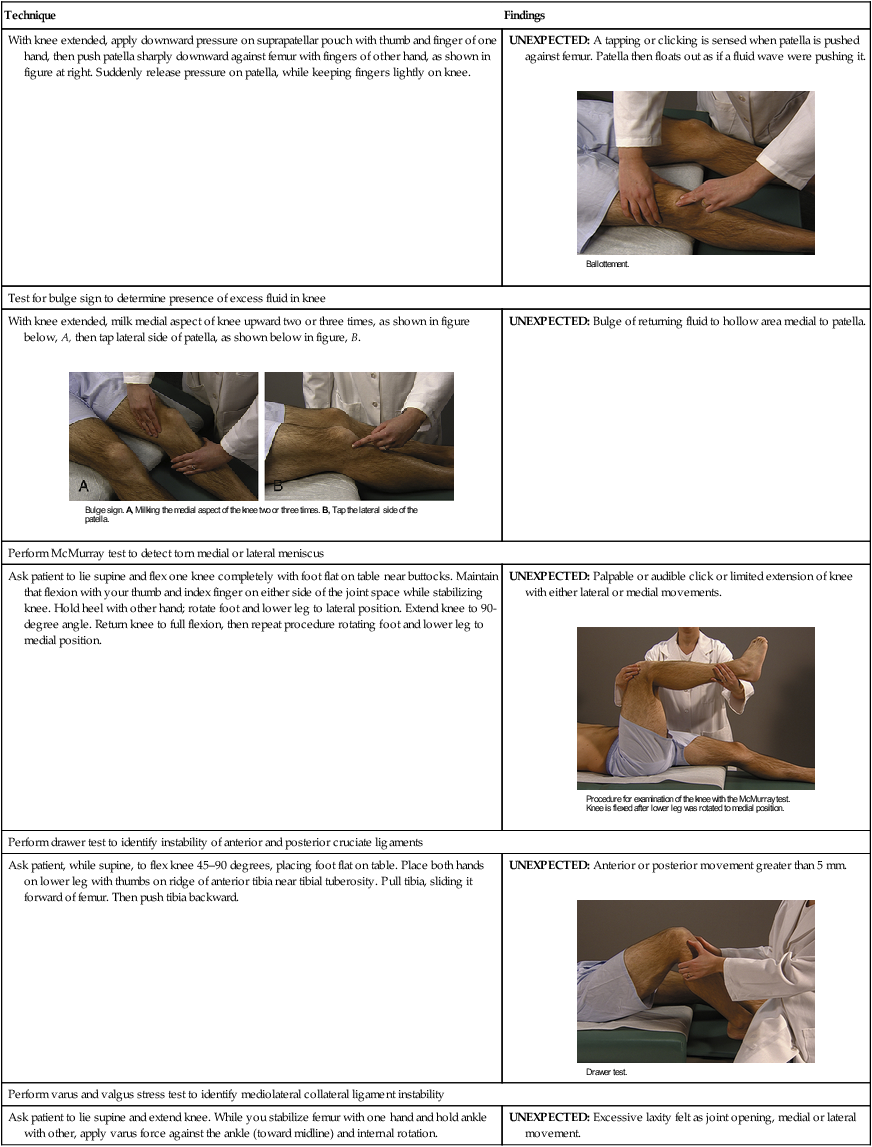
| Perform ballottement procedure to determine presence of excess fluid or effusion in knee | |
| With knee extended, apply downward pressure on suprapatellar pouch with thumb and finger of one hand, then push patella sharply downward against femur with fingers of other hand, as shown in figure at right. Suddenly release pressure on patella, while keeping fingers lightly on knee. | UNEXPECTED: A tapping or clicking is sensed when patella is pushed against femur. Patella then floats out as if a fluid wave were pushing it. |
| Test for bulge sign to determine presence of excess fluid in knee | |
| With knee extended, milk medial aspect of knee upward two or three times, as shown in figure below, A, then tap lateral side of patella, as shown below in figure, B. | UNEXPECTED: Bulge of returning fluid to hollow area medial to patella. |
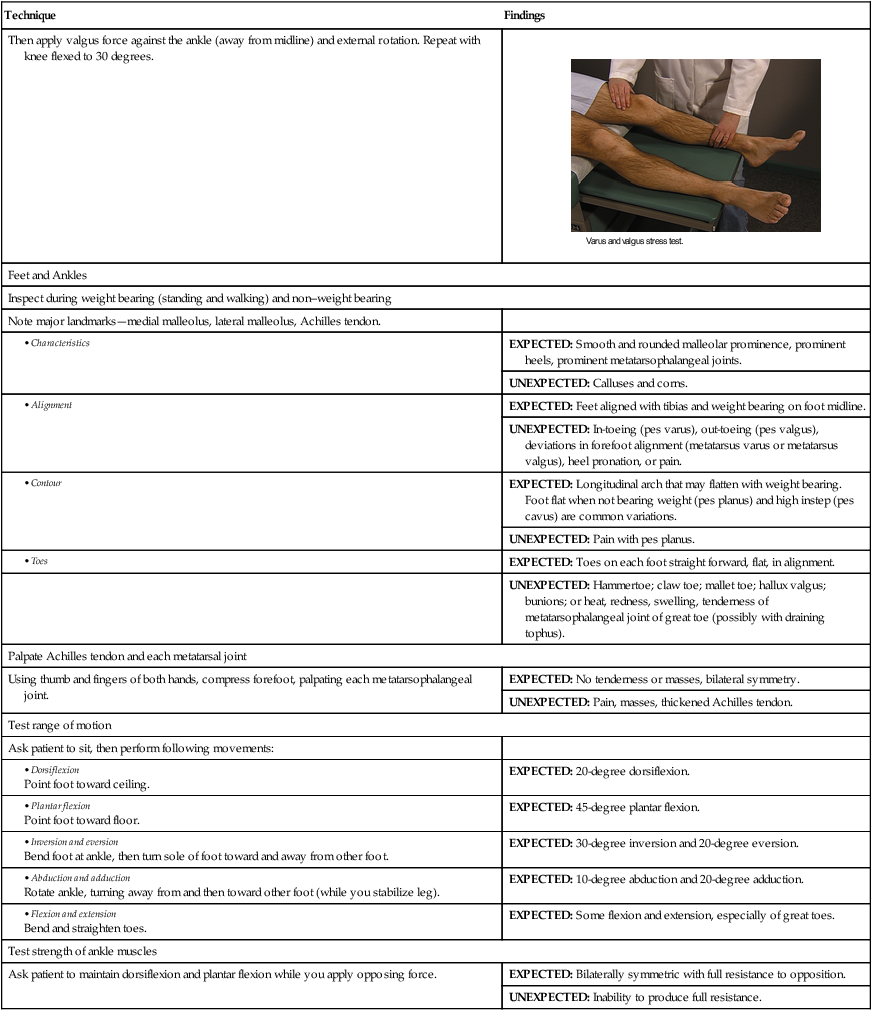
| Perform McMurray test to detect torn medial or lateral meniscus | |
| Ask patient to lie supine and flex one knee completely with foot flat on table near buttocks. Maintain that flexion with your thumb and index finger on either side of the joint space while stabilizing knee. Hold heel with other hand; rotate foot and lower leg to lateral position. Extend knee to 90-degree angle. Return knee to full flexion, then repeat procedure rotating foot and lower leg to medial position. | UNEXPECTED: Palpable or audible click or limited extension of knee with either lateral or medial movements. |
| Perform drawer test to identify instability of anterior and posterior cruciate ligaments | |
| Ask patient, while supine, to flex knee 45–90 degrees, placing foot flat on table. Place both hands on lower leg with thumbs on ridge of anterior tibia near tibial tuberosity. Pull tibia, sliding it forward of femur. Then push tibia backward. | UNEXPECTED: Anterior or posterior movement greater than 5 mm. |
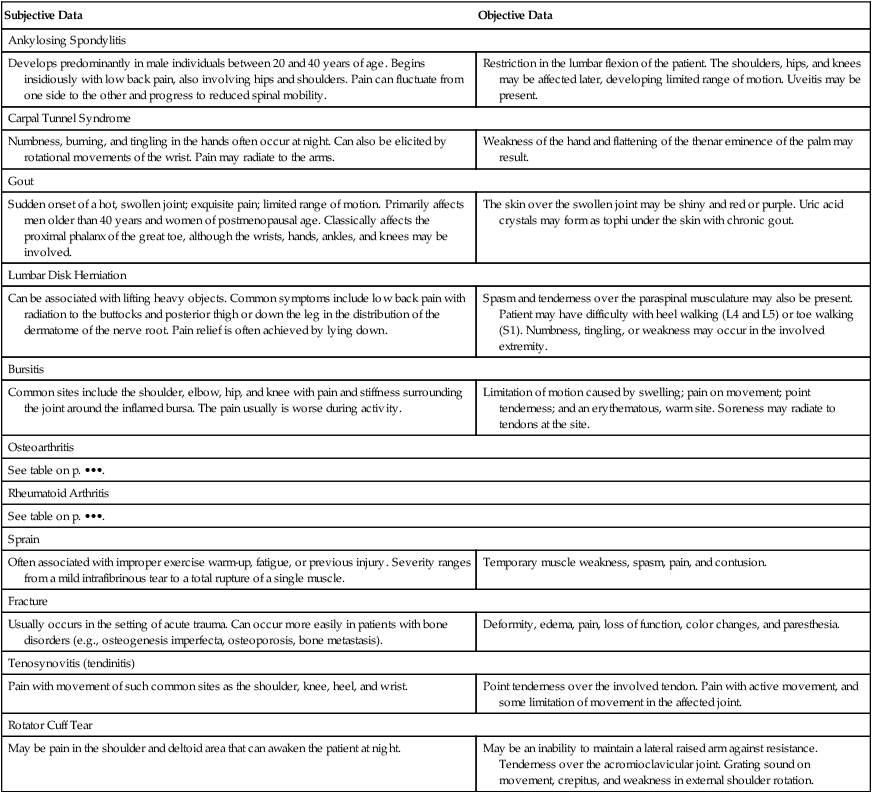
| Perform varus and valgus stress test to identify mediolateral collateral ligament instability | |
| Ask patient to lie supine and extend knee. While you stabilize femur with one hand and hold ankle with other, apply varus force against the ankle (toward midline) and internal rotation. | UNEXPECTED: Excessive laxity felt as joint opening, medial or lateral movement. |
| Then apply valgus force against the ankle (away from midline) and external rotation. Repeat with knee flexed to 30 degrees. | |
| Feet and Ankles | |
| Inspect during weight bearing (standing and walking) and non–weight bearing | |
| Note major landmarks—medial malleolus, lateral malleolus, Achilles tendon. | |
| EXPECTED: Smooth and rounded malleolar prominence, prominent heels, prominent metatarsophalangeal joints. | |
| UNEXPECTED: Calluses and corns. | |
| EXPECTED: Feet aligned with tibias and weight bearing on foot midline. | |
| UNEXPECTED: In-toeing (pes varus), out-toeing (pes valgus), deviations in forefoot alignment (metatarsus varus or metatarsus valgus), heel pronation, or pain. | |
| EXPECTED: Longitudinal arch that may flatten with weight bearing. Foot flat when not bearing weight (pes planus) and high instep (pes cavus) are common variations. | |
| UNEXPECTED: Pain with pes planus. | |
| EXPECTED: Toes on each foot straight forward, flat, in alignment. | |
| UNEXPECTED: Hammertoe; claw toe; mallet toe; hallux valgus; bunions; or heat, redness, swelling, tenderness of metatarsophalangeal joint of great toe (possibly with draining tophus). | |
| Palpate Achilles tendon and each metatarsal joint | |
| Using thumb and fingers of both hands, compress forefoot, palpating each metatarsophalangeal joint. | EXPECTED: No tenderness or masses, bilateral symmetry. |
| UNEXPECTED: Pain, masses, thickened Achilles tendon. | |
| Test range of motion | |
| Ask patient to sit, then perform following movements: | |
| EXPECTED: 20-degree dorsiflexion. | |
| EXPECTED: 45-degree plantar flexion. | |
| EXPECTED: 30-degree inversion and 20-degree eversion. | |
| EXPECTED: 10-degree abduction and 20-degree adduction. | |
| EXPECTED: Some flexion and extension, especially of great toes. | |
| Test strength of ankle muscles | |
| Ask patient to maintain dorsiflexion and plantar flexion while you apply opposing force. | EXPECTED: Bilaterally symmetric with full resistance to opposition. |
| UNEXPECTED: Inability to produce full resistance. | |
Aids To Differential Diagnosis
| Subjective Data | Objective Data |
| Ankylosing Spondylitis | |
| Develops predominantly in male individuals between 20 and 40 years of age. Begins insidiously with low back pain, also involving hips and shoulders. Pain can fluctuate from one side to the other and progress to reduced spinal mobility. | Restriction in the lumbar flexion of the patient. The shoulders, hips, and knees may be affected later, developing limited range of motion. Uveitis may be present. |
| Carpal Tunnel Syndrome | |
| Numbness, burning, and tingling in the hands often occur at night. Can also be elicited by rotational movements of the wrist. Pain may radiate to the arms. | Weakness of the hand and flattening of the thenar eminence of the palm may result. |
| Gout | |
| Sudden onset of a hot, swollen joint; exquisite pain; limited range of motion. Primarily affects men older than 40 years and women of postmenopausal age. Classically affects the proximal phalanx of the great toe, although the wrists, hands, ankles, and knees may be involved. | The skin over the swollen joint may be shiny and red or purple. Uric acid crystals may form as tophi under the skin with chronic gout. |
| Lumbar Disk Herniation | |
| Can be associated with lifting heavy objects. Common symptoms include low back pain with radiation to the buttocks and posterior thigh or down the leg in the distribution of the dermatome of the nerve root. Pain relief is often achieved by lying down. | Spasm and tenderness over the paraspinal musculature may also be present. Patient may have difficulty with heel walking (L4 and L5) or toe walking (S1). Numbness, tingling, or weakness may occur in the involved extremity. |
| Bursitis | |
| Common sites include the shoulder, elbow, hip, and knee with pain and stiffness surrounding the joint around the inflamed bursa. The pain usually is worse during activity. | Limitation of motion caused by swelling; pain on movement; point tenderness; and an erythematous, warm site. Soreness may radiate to tendons at the site. |
| Osteoarthritis | |
| See table on p. •••. | |
| Rheumatoid Arthritis | |
| See table on p. •••. | |
| Sprain | |
| Often associated with improper exercise warm-up, fatigue, or previous injury. Severity ranges from a mild intrafibrinous tear to a total rupture of a single muscle. | Temporary muscle weakness, spasm, pain, and contusion. |
| Fracture | |
| Usually occurs in the setting of acute trauma. Can occur more easily in patients with bone disorders (e.g., osteogenesis imperfecta, osteoporosis, bone metastasis). | Deformity, edema, pain, loss of function, color changes, and paresthesia. |
| Tenosynovitis (tendinitis) | |
| Pain with movement of such common sites as the shoulder, knee, heel, and wrist. | Point tenderness over the involved tendon. Pain with active movement, and some limitation of movement in the affected joint. |
| Rotator Cuff Tear | |
| May be pain in the shoulder and deltoid area that can awaken the patient at night. | May be an inability to maintain a lateral raised arm against resistance. Tenderness over the acromioclavicular joint. Grating sound on movement, crepitus, and weakness in external shoulder rotation. |
Differential Diagnosis of Arthritis
| Signs and Symptoms | Osteoarthritis | Rheumatoid Arthritis |
| Onset | Insidious | Gradual or sudden (24–48 hours) |
| Duration of stiffness | Few minutes, localized, but short “gelling” after prolonged rest | Often hours, most pronounced after rest |
| Pain | On motion, with prolonged activity, relieved by rest | Even at rest, may disturb sleep |
| Weakness | Usually localized and not severe | Often pronounced, out of proportion with muscle atrophy |
| Fatigue | Unusual | Often severe, with onset 4–5 hours after rising |
| Emotional depression and lability | Unusual | Common, coincides with fatigue and disease activity, often relieved if in remission |
| Tenderness over localized afflicted joint | Common | Almost always; most sensitive indicator of inflammation |
| Swelling | Effusion common, little synovial, reaction swelling rare | Fusiform soft tissue enlargement, effusion common, synovial proliferation and thickening |
| Heat, erythema | Unusual | Sometimes present |
| Crepitus, crackling | Coarse to medium on motion | Medium to fine |
| Joint enlargement | Mild with firm consistency | Moderate to severe |
Pediatric Variations
Examination
Musculoskeletal findings and motor development in infants, children, and adolescents change as they grow. (For a complete description of age-specific anticipated pediatric findings, see Chapter 21.)
Sports Participation Screening Examination for Children and Adolescents
• Observe posture and general muscle contour bilaterally.
• Ask patient to walk on tiptoes and heels.
• Observe patient hop on each foot.
• Ask patient to duck-walk four steps with knees completely bent.
• Inspect spine for curvature and lumbar extension, fingers touching toes with knees straight.
• Palpate shoulder and clavicle for dislocation.
• Check the following for range of motion—neck, shoulder, elbow, forearm, hands, fingers, hips.
Sample Documentation
Subjective
A 13-year-old girl referred by school nurse because of uneven shoulder and hip heights. Active in sports, good strength, no back pain or stiffness.
Objective
Spine straight without obvious deformities when erect, but mild right curvature of thoracic spine with forward flexion. No rib hump. Right shoulder and iliac crest slightly higher than left. Muscles and extremities symmetric; muscle strength appropriate and equal bilaterally; active range of motion without pain, locking, clicking, or limitation in all joints.