Head-to-Toe Examination
Adult
Components of the Examination
There is no one correct way to order the parts of the physical examination. You are encouraged to consider and then to adapt and edit the following suggested approach for the unique needs of the particular patient and the relevant demands of the moment.
General Inspection
Start examination the moment the patient is within your view. As you first observe the patient, for example, in the waiting room, take note of the following characteristics:
• Signs of distress or disease

• Relationship with others in room
• Degree of interest in what is happening in room
• Manner with which you are met
• Moistness of palm when you shake hands
• Eyes—luster and expression of emotion
• Speech pattern, disorders, foreign language
• Difficulty hearing, assistive devices
• Vision problems, assistive devices
Patient Seated, Wearing Gown
Stand in front of patient seated on examining table.

Head and Face
• Inspect skin characteristics.
• Inspect symmetry and external characteristics of eyes and ears.
• Inspect configuration of skull.
• Inspect and palpate scalp and hair for texture, distribution, and quantity of hair.
• Palpate temporomandibular joint while patient opens and closes mouth.
• Palpate sinus regions; if tender, transilluminate them (may be helpful, but sensitivity and specificity are uncertain when considered separate from other findings).
• Inspect ability to clench teeth, squeeze eyes tightly shut, wrinkle forehead, smile, stick out tongue, and puff out cheeks (CN V, VII).
• Test sensation using light touch on forehead, cheeks, chin (CN V).
Eyes
• Inspect eyelids, eyelashes, palpebral folds.
• Determine alignment of eyebrows.
Mouth and Pharynx
• Inspect lips, buccal mucosa, gums, hard and soft palates, floor of mouth for color and surface characteristics.
• Inspect oropharynx: note anteroposterior pillars, uvula, tonsils, posterior pharynx, mouth odor.
• Inspect teeth for color, number, surface characteristics.
• Inspect tongue for color, characteristics, symmetry, movement (CN XII).
• Test gag reflex and “ah” reflex (CN IX, X).
• Assess sense of taste test when clinically indicated (CN VII, IX).
Neck
• Inspect for symmetry and smoothness of neck and thyroid.
• Inspect for jugular venous distention (also when patient is supine).
• Perform active and passive range of motion; test resistance against examiner’s hand.
• Test strength of shoulder shrug (CN IX).
• Palpate carotid pulses. Be sure to palpate one side at a time (also when patient is supine).
• Palpate lymph nodes—preauricular and postauricular, occipital, tonsillar, submental, submandibular, superficial cervical chain, posterior cervical, deep cervical, supraclavicular.
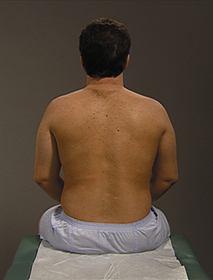
Patient Seated, Back Exposed
Stand behind patient seated on examining table. Have male patients pull gown down to the waist so entire chest and back are exposed. Have females expose back; keep breasts covered.
Lungs
• Inspect respiration—excursion, depth, rhythm, pattern.
• Palpate for expansion and tactile fremitus.
• Palpate scapular and subscapular nodes.
• Percuss posterior chest and lateral walls systematically for resonance.
• Percuss for diaphragmatic excursion.
• Auscultate systematically for breath sounds. Note characteristics and adventitious sounds.
Patient Seated, Chest Exposed
Move around to front of patient. Have female patients lower gown to expose anterior chest.

Anterior Chest, Lungs, Heart
• Inspect skin, musculoskeletal development, symmetry.
• Inspect respirations—patient posture, respiratory effort.
• Inspect for pulsations or heaving.
• Palpate chest wall for stability, crepitation, tenderness.
• Palpate precordium for thrills, heaves, pulsations, and location of apical impulse.
• Palpate for tactile fremitus.
• Percuss systematically for resonance.
• Auscultate systematically for breath sounds.
• Auscultate systematically for heart sounds—aortic, pulmonic, second pulmonic, tricuspid, and mitral areas.
Female Breasts
• Inspect in these positions—patient’s arms hanging loosely at the sides, extended over head or flexed behind the neck, pushing hands on hips, hands pushed together in front of chest, patient leaning forward.
• Perform chest wall sweep and bimanual digital palpation.
• Palpate axillary, supraclavicular, and infraclavicular lymph nodes (if not already performed).
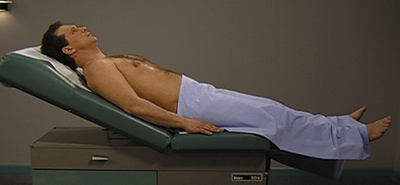
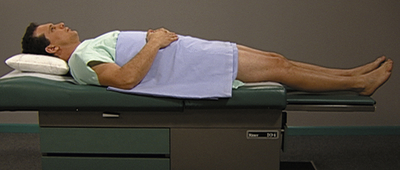
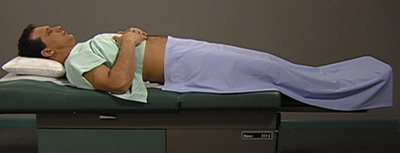
Patient Supine, Abdomen Exposed
Have patient remain supine. Cover chest with patient’s gown. Arrange draping to expose abdomen from pubis to epigastrium.
Abdomen
• Inspect skin characteristics, contour, pulsations, movement.
• Auscultate all quadrants for bowel sounds.
• Auscultate aorta and renal, iliac, and femoral arteries for bruits or venous hums.
• Percuss all quadrants for tone.
• Percuss liver borders and estimate span.
• Percuss left midaxillary line for splenic dullness.
• Lightly palpate all quadrants.
Patient Sitting, Lap Draped
Assist patient to a sitting position. Have patient wear gown with a drape across lap.

Neurologic
• Test sensory function—dull and sharp sensation of forehead, cheeks, chin, lower arms, hands, lower legs, feet.
• Test position sense and vibratory sensation of wrists, ankles.
• Test two-point discrimination of palms, thighs, back.
• Test stereognosis, graphesthesia.
• Test fine motor function, coordination, and position sense of upper extremities, asking patient to do the following:
• Touch nose with alternating index fingers.
• Rapidly alternate touching fingers to thumb.
• Rapidly move index finger between own nose and examiner’s finger.
• Test fine motor function, coordination, and position sense of lower extremities, asking patient to do following:
• Test deep tendon reflexes and compare bilaterally—biceps, triceps, brachioradial, patellar, Achilles.
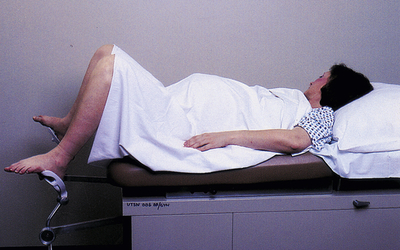
Female Patient, Lithotomy Position
Assist female patient into lithotomy position and drape appropriately. Examiner is seated.
Internal Genitalia
• Perform speculum examination:
• Perform bimanual palpation to assess for characteristics of vagina, cervix, uterus, adnexa (examiner standing).
• Perform rectovaginal examination to assess rectovaginal septum, broad ligaments.