CHAPTER 5
Urticaria and Angio‐oedema
Rachael Morris‐Jones
Guy’s and St Thomas’ NHS Foundation Trust, London, UK
Introduction
Urticaria describes transient pruritic swellings of the skin, often referred to as wheals, hives, or nettle rash by the patient. Urticaria results from oedema in the superficial layers of the skin causing well‐demarcated erythematous lesions. It may be associated with allergic reactions, infections, or physical stimuli, but in most patients no cause can be found. Similar lesions may precede or be associated with vasculitis (urticarial vasculitis), pemphigoid, or dermatitis herpetiformis.
Angio‐oedema in contrast is usually painful rather than itchy and appears as a diffuse swelling that affects the deeper layers of the skin; it can occur rapidly and may involve the mucous membranes. Laryngeal oedema is the most serious complication and can be life‐threatening. Hereditary angio‐oedema is a rare form with recurrent severe episodes of subcutaneous oedema, swelling of the mucous membranes, and systemic symptoms.
Urticaria is a common skin disorder that affects 20% of the population at some point in their lives. Urticaria may occur as a single episode or be chronically recurrent. It is often self‐limiting and is controlled with antihistamine. The prognosis is varied depending on the underlying cause, but in chronic spontaneous urticaria (CSU) symptoms may persist for several years.
Pathophysiology
Urticaria results from histamine, bradykinin, and pro‐inflammatory mediators being released from basophils and mast cells in response to various trigger factors. The chemicals released by degranulation cause capillaries and venules to leak causing tissue oedema. Urticaria may be immunoglobulin E (IgE) mediated with cross‐linking of two adjacent IgE receptors, or complement‐mediated (causing direct degranulation of mast cells), or mast cells may be directly stimulated by an exogenous or unknown substance. In patients with chronic urticaria, histamine can be released spontaneously or in response to non‐specific stimuli and their vasculature is more sensitive to histamines.
Clinical history
Careful history‐taking is of great importance in diagnosing patients with urticaria and/or angio‐oedema because frequently there are no clinical signs for the medical practitioner to see. Ask about the onset, duration, and course of lesions, rashes, and swelling. Urticaria is very itchy and angio‐oedema usually painful. Patients with urticaria complain of itchy spots or rashes lasting minutes or hours (usually less than 24 hours) that resolve leaving no marks on the skin. Patients may complain of swelling (angio‐oedema) of their face, particularly eyelids, lips, and tongue, which may last hours or days.
If the skin eruption lasts for more than 24 hours, is painful and resolves with bruising then urticarial vasculitis (Figure 5.1) is more likely than ordinary urticaria (Figure 5.2).

Figure 5.1 Urticarial vasculitis with bruising.

Figure 5.2 Ordinary urticaria.
Patients may feel unwell before the onset of the rash or swelling and rarely in severe reactions anaphylaxis can occur. You should always ask about any associated respiratory distress. An attempt to identify possible triggers before the onset of symptoms is important. In particular, ask about any food eaten (nausea/vomiting), exercise, heat/cold, sun, medications/infusions, latex exposure, insect stings, animal contact, physical stimuli, infections, family history, and any known medical conditions (Figures 5.3 and 5.4).

Figure 5.3 Urticaria from contact with brown caterpillar moths.

Figure 5.4 Cold‐induced urticaria on the cheeks.
Classification of urticaria
Urticaria is traditionally classified as acute or chronic depending on whether symptoms last for less or more than six weeks. Another approach is to classify urticaria according to the underlying cause, but in 50% of cases no cause is identified (idiopathic). Urticaria can therefore broadly be divided into ordinary/idiopathic (acute/chronic), contact allergic, cholinergic, physical, or urticarial vasculitis. See Boxes 5.1 and 5.2.
Ordinary urticaria
This is the most common form of urticaria, characterised by intermittent fleeting wheals at any skin site, with or without angioedema (Figures 5.2 and 5.5). Lesions may be papular, annular (Figure 5.6) and even serpiginous. The urticarial lesions themselves last minutes to hours only and may recur over <6 weeks – acute urticaria, or attacks may become chronic (>6 weeks). In 50% of patients with ordinary urticaria no underlying cause is found. Possible triggers of acute urticaria include infections, vaccinations, medications, and food. Generally, the more persistent the attacks of urticaria, the less likely that an underlying cause is identified; this is termed chronic spontaneous urticaria.

Figure 5.5 Ordinary urticaria with dermatographism.

Figure 5.6 Annular urticaria.
Cholinergic urticaria
Patients are usually aged 10–30 years and typically experience urticaria following a warm shower/bath, or after exercise. Patients report erythema and burning pruritus followed by extensive urticaria. The lesions consist of pinhead‐sized wheals with a red flare around them. The underlying trigger is not fully understood, but deficiency in α1‐antitrypsin may predispose to urticaria in which sweat has been shown to play a role and where serum histamine levels are raised following exertion. Avoidance of heat usually helps reduce the frequency and severity of symptoms.
A rarer form of cholinergic urticaria can result from exposure to the cold. Patients report urticaria on exposed skin during cold weather, lip/tongue/hand swelling following the holding and ingestion of cold beverages and a more generalised reaction following swimming in an outdoor pool. Affected individuals should avoid swimming in cold water and ingestion of ice‐cold drinks as anaphylaxis and death have been reported.
Solar urticaria
Solar urticaria is a rare condition in which sunlight causes an acute urticarial eruption. Patients complain of stinging, burning, and itching at exposed skin sites within 30 minutes of ultraviolet or artificial light source exposure. Lesions resolve rapidly (minutes to hours) when light exposure ceases. Photosensitive drug eruptions can present in a similar manner; so, a detailed drug history is important. Differential diagnosis may include porphyria (lesions resolve with scarring) and polymorphic light eruption (lesions take days to weeks to resolve). The pathophysiology is poorly understood but is thought to be mediated by antigen production as serum transfer can induce similar symptoms in asymptomatic controls. Light‐testing confirms the diagnosis. Management can be challenging but avoidance of sunlight is helpful.
Pressure urticaria
Urticarial wheals occur at the site of pressure on the skin, characteristically around the waistband area (from clothing), shoulders (from carrying a backpack), soles of feet (from walking), hands (using tools or weight lifting), buttocks (from sitting), and genitals (sexual intercourse). The urticarial rash may occur immediately but a delay of up to six hours can occur (delayed pressure urticaria), and lesions resolve over several days. Symptoms are usually recurrent over many years. The cause is unknown and although histamine is thought to play a role, patients are less likely to respond to antihistamines than in other forms of urticaria. Eosinophils and interleukin are thought to play a role. Investigation can include pressure challenge testing. Patients may respond to dapsone or montelukast.
Angio‐oedema
Patients present with swelling plus or minus urticaria that develops over hours and resolves over days. Angio‐oedema causes well‐demarcated swelling of the subcutaneous tissues (Figure 5.7) and/or mucous membranes, from increased vascular permeability. A detailed drug history should be taken because allergy to medication (angiotensin‐converting enzyme inhibitors, non‐steroidal anti‐inflammatory drugs, bupropion, statins, or proton pump inhibitors) may be the cause. Laryngeal swelling is the most serious complication and should ideally be managed by emergency medicine specialists.
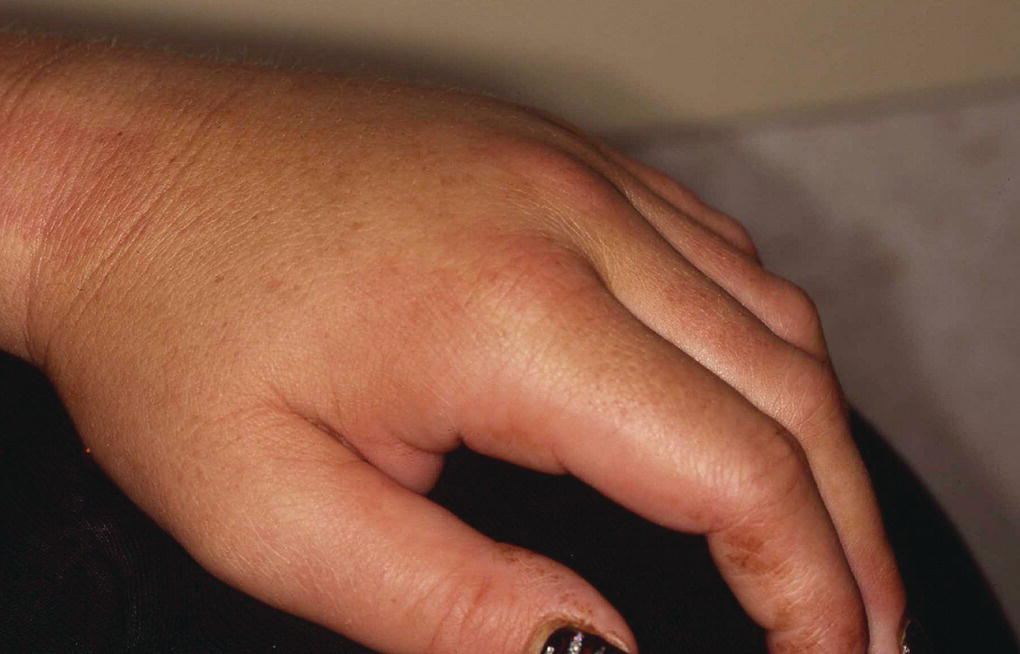
Figure 5.7 Angio‐oedema of the hand.
A hereditary form of angio‐oedema presents in young persons as recurrent severe attacks affecting the skin and mucous membranes. Tingling, tightness, and pain are the main symptoms associated with the oedema. Patients may suffer associated gastrointestinal symptoms and life‐threatening laryngeal oedema. Hereditary angio‐oedema is caused by a deficiency in C1 (esterase) inhibitor. Serum complement C4 levels are low following attacks. Danazol can be used to reduce the frequency and severity of attacks and fresh frozen plasma can be used before elective surgery.
General investigations
Apart from a detailed history and examination most patients need no further investigations. If food allergy is suspected, patients can be asked to keep a food diary, particularly if their urticaria is recurrent and episodic. An attempt to elicit dermatographism (exaggerated release of histamine causing wheal and flare) should be made by firmly stroking the skin with a hard object such as the end of a pen; this is usually positive in physical urticaria (Figure 5.8).

Figure 5.8 Dermatographism.
A skin biopsy can be useful if urticarial vasculitis is suspected; plain lidocaine should be used for the local anaesthetic (as adrenaline causes release of histamine from mast cells). Histology from urticaria may show dermal oedema and vasodilatation. In urticarial vasculitis, there is a cellular infiltrate of lymphocytes, polymorphs, and histiocytes.
In patients with more severe reactions to e.g. suspected foods then allergen‐specific IgE antibodies should be checked or skin prick testing (although not in patients with anaphylaxis) may help identify specific allergies. In addition, immediate type I hypersensitivity patch testing to identify contact urticaria can be undertaken in specialist centres.
If you suspect hereditary angio‐oedema, check the complement C3 level and C1 esterase which are usually low.
If heat or cold are the possible precipitants then exercising for 5 minutes or placing an ice‐cube on the skin for 20 minutes may be diagnostic. Physical urticaria can be elicited by firm pressure on the skin (dermographism/dermatographism). Solar urticaria can be assessed in specialist centres using a solar simulator.
General management
Patients often make their own observations concerning trigger factors, especially food, medication and insect stings, and know what they should try to avoid. Treatment of any underlying medical condition identified should help settle the urticaria. Oral antihistamines are the mainstay of treatment/prevention of urticaria and angio‐oedema. Patients can manage their own symptoms by purchasing antihistamines (cetirizine, loratadine, or chlorphenamine) over the counter.
In severe recalcitrant cases, physicians may need to prescribe high doses (two to four times the usual dose) of a single agent such as fexofenadine 180 mg (age 11 years and above, age 2–11 years 30 mg twice daily) or synergistic combinations of H1‐receptor blockers (as above plus desloratadine, levocetirizine, terfenadine, or hydroxyzine) plus H2 blockade (ranitidine or cimetidine) and leukotriene receptor antagonists (montelukast or zafirlukast) to control symptoms. Depending on the frequency of symptoms, antihistamines may be taken prophylactically daily or intermittently to treat symptoms.
During pregnancy chlorpheniramine, loratadine, or cetirizine are thought to be safe.
Oral corticosteroids may be indicated in very severe eruptions, particularly those associated with urticarial vasculitis or angioedema. However, in studies, oral prednisolone did not add any benefit to antihistamines in reducing the duration of the urticaria.
Patients known to be at risk of severe life‐threatening urticaria/angio‐oedema with respiratory distress may be asked to carry with them a pre‐assembled syringe and needle (EpiPen® or Anapen®) to inject adrenaline intramuscularly (300–500 μg). Management of the patient's airway is critical and once secured, oxygen and if necessary further intramuscular/intravenous adrenaline can then be administered by medical professionals.
Phase III clinical trials of 150 mg subcutaneous injection of omalizumab every 2–4 weeks for 9–12 months have shown encouraging results in patients whose urticaria is recalcitrant to the effects of H1‐blockers. For both CSU and chronic inducible urticaria (CindU) the drug appears to be effective. Omalizumab treatment led to complete remission in 83% of CSU and 70% of CindU) at about nine months, some patients symptoms stopped after the first dose and some patients were found to be in remission when the drug was stopped.
Further reading
- http://www.allergy‐clinic.co.uk/urticaria
- Kartal, S.P. and Kutlubay, Z. (2017). A Comprehensive Review of Urticaria and Angioedema. InTechOpen.
- Zuberbier, T., Grattan, C., and Maurer, M. (2010). Urticaria and Angioedema. Heidelberg: Springer.