Chapter 9

Positive Physical Health: The Biology of Optimism
Health is a state of complete physical, mental, and social well-being
and not merely the absence of disease or infirmity.
—Preamble to the Constitution of the
World Health Organization, 1946
Turning Medicine on Its Head
I have been a psychotherapist for thirty-five years. I am not a very good one—I confess that I’m better at talking than at listening—but once in a while I have done pretty good work and helped my patient get rid of almost all of her sadness, almost all of her anxiety, and almost all of her anger. I thought that my work was done, and I would have a happy patient.
Did I get a happy patient? No. As I said in Chapter 3, I got an empty patient. That is because the skills of enjoying positive emotion, being engaged with the people you care about, having meaning in life, achieving your work goals, and maintaining good relationships are entirely different from the skills of not being depressed, not being anxious, and not being angry. These dysphorias get in the way of well-being, but they do not make well-being impossible; nor does the absence of sadness, anxiety, and anger remotely guarantee happiness. The takeaway lesson from positive psychology is that positive mental health is not just the absence of mental illness.
It is all too commonplace not to be mentally ill but to be stuck and languishing in life. Positive mental health is a presence: the presence of positive emotion, the presence of engagement, the presence of meaning, the presence of good relationships, and the presence of accomplishment. Being in a state of mental health is not merely being disorder free; rather it is the presence of flourishing.
This is directly contrary to the wisdom that Sigmund Freud handed down from Mount Sinai: that mental health is just the absence of mental illness. Freud was a follower of the philosopher Arthur Schopenhauer (1788–1860). Both believed that happiness was an illusion and the best we could ever hope for was to keep our misery and suffering to a minimum. Let there be no doubt about this: traditional psychotherapy is not designed to produce well-being, it is designed just to curtail misery—which is itself no small task.
Physical health has accepted the same “wisdom”: that physical health is merely the absence of physical illness. Disclaimers such as the World Health Organization’s (above), and the very name of the National Institutes of Health notwithstanding (misleading because more than 95 percent of its budget goes to curtail illness), a scientific discipline of health barely exists. It was with all of this in their minds that Robin Mockenhaupt and Paul Tarini, officials from the huge Robert Wood Johnson Foundation (RWJF), asked to come speak with me about positive psychology.
“We would like you to turn medicine on its head,” said Paul, director of the Pioneer branch. The Pioneer branch is just what it sounds like. Most of RWJF’s medical funding goes to gold bond ideas such as reducing obesity, so the Pioneer branch is the foundation’s way to balance its research portfolio by investing in innovative ideas well outside the mainstream of medical research—ideas that just might have a major payoff for health and health care in America.
“We’ve been following what you have done in mental health—to show that it is something real, something over and above the absence of mental illness—and we would like you to try the same thing for physical health,” he continued. “Are there positive properties—health assets—that constitute an actual state of physical health? Is there a state that increases longevity, which decreases morbidity, which results in a better prognosis when illness finally strikes, and which decreases lifetime health care costs? Is health a real thing, or is all that medicine needs to be after is the absence of illness?”
That was enough to set my heart pumping. I had been working on just one piece of this grand puzzle: discovering one psychological state—optimism—that predicts and might cause less physical illness, and a tantalizing panorama of findings has emerged. This started forty years before my chat with Paul and Robin.
Origins of Learned Helplessness Theory
I was part of a threesome—Steve Maier and Bruce Overmier were my partners—who discovered “learned helplessness” in the mid-1960s. We found that animals—dogs, rats, mice, and even cockroaches—later become passive and gave up in the face of adversity once they had first experienced noxious events that they could do nothing about. After that first experience with helplessness, thereafter they merely lay down in mildly painful shock and took it, just waiting it out, with no attempt to escape. Animals that first had exactly the same physical shock—but the shock was escapable—did not become helpless later on. They were immunized against learned helplessness.
Human animals do just what nonhuman animals do: in the paradigm human experiment, carried out by Donald Hiroto and replicated many times since, subjects are randomly divided into three groups. This is called the “triadic design.” One group (escapable) is exposed to a noxious but nondamaging event, such as loud noise. When they push a button in front of them, the noise stops, so that their own action escapes the noise. A second group (inescapable) is yoked to the first group. The subjects receive exactly the same noise, but it goes off and on regardless of what they do. The second group is helpless by definition, since the probability of the noise going off given that they make any response is identical to the probability of the noise going off given that they do not make that response. Operationally, learned helplessness is defined by the fact that nothing you do alters the event. Importantly the escapable and inescapable groups have exactly the same objective stressor. A third group (control) receives nothing at all. That is part one of the triadic experiment.
Go back over this paragraph, and be sure that you understand the triadic design, since the rest of this chapter will make little sense otherwise.
Part one induces learned helplessness, and part two displays the dramatic aftereffects. Part two takes place later and in a different place. Commonly in part two, all three groups encounter a “shuttle box.” The person puts his hand in one side of the box and the loud noise goes on. If he moves his hand a few inches to the other side, noise goes off. People from the escapable group and from the control group readily learn to move their hands to escape noise. The people from the inescapable group typically do not move. They just sit there taking the noise until it goes off by itself. In part one, they had learned that nothing they did mattered, and so in part two, expecting that nothing they do will matter, they do not try to escape.
I was aware of a legion of anecdotes about people taking sick and even dying when helpless, so I began to wonder if learned helplessness somehow could reach inside the body and undermine health and vitality themselves. I also wondered about the inverse: Paul Tarini’s question. Could the psychological state of mastery—the opposite of helplessness—somehow reach inside and strengthen the body?
Here is the rationale for the triadic design—three groups: escapable, inescapable, and normal control—that is the hallmark of all well-executed experiments on learned helplessness. The presence of a normal control group, which has no prior experience with the stressor, allows bidirectional inferences. Does helplessness damage the person, along with does mastery enhance the person? The answer to “Does helplessness damage?” (the “pathological” question) lies in the part two comparison of the people who received inescapable noise in part one to the normal control that got no noise at all in part one. If the inescapable group does worse than the normal control group in part two, helplessness has damaged the person.
The bipolar question is “Does mastery strengthen the person?” The answer to that question (the “positive psychology question”) lies in the part two comparison of the people who learned in part one to escape the noise to those in the normal control group. If they do better than the normal control group in part two, mastery has strengthened them. Notice that the poor performance of the helpless group relative to the mastery group is of less scientific interest than the comparison of both these groups to the control group—since the helpless group would do worse than the mastery group if helplessness weakens people, or if mastery strengthens people, or if both were true.
This is the insight underlying Paul Tarini’s question, an insight so obvious that it is easy to miss altogether. Psychology and medicine, following Freud and the medical model, view the world through the lens of pathology and look only at the toxic effects of malign events. Psychology and medicine get turned on their heads when we ask about the opposite of pathology: about the strengthening effects of benevolent events. Indeed, any endeavor—nutrition, the immune system, welfare, politics, education, or ethics—that is fixated on the remedial misses this insight and does just half the job: correcting deficits while failing to build strength.
Psychology of Illness
It was through learned helplessness that I got involved in the psychology of physical illness. Our best attempt to ask about physical health in the triadic design used rats and cancer. Madelon Visintainer and Joe Volpicelli—both my graduate students at the time—implanted a tumor that had a 50 percent lethality rate (LD 50) on the flanks of rats. We then randomly assigned the rats to one of the three psychological conditions: one session of sixty-four mildly painful escapable shocks (mastery), or one session of the identical shocks but inescapable shocks (helplessness), or no shock (the control group). That was part one.
In part two, we just waited to see which rats got cancer and died and which rats rejected the tumor. As expected, 50 percent of the control group, which had no experience with shock, died. Three-quarters of the rats in the inescapable group died, showing that helplessness weakened the body. One-quarter of the rats in the escapable group died, demonstrating that mastery strengthened the body.
I should mention that this experiment—published in Science in 1982—was the last time that I have been involved in an animal experiment, and I want to tell you why: on the ethical side, I am an animal lover—my life has continually been enriched by our dogs at home. So I found it very difficult to inflict suffering on animals for any purpose at all, even a humanitarian purpose. But the scientific argument is more telling for me: there are usually more direct ways of answering the questions that most interest me with human participants rather than animal subjects. All animal experiments that try to make inferences to humans must tangle with the problem of external validity.
This is a crucial, neglected, and really hairy issue. What attracted me to experimental psychology in the very first place was its rigor, what is called internal validity. Performing a controlled experiment is the gold standard of internal validity because it discovers what causes what. Does the fire cause the water to boil? Turn on the fire, and the water boils. Without the fire (the control group), the water does not boil. Do uncontrollable bad events spur tumor growth? Give one group of rats inescapable shock, give another group identical escapable shock, and compare them to a group that receives no shock. Rats that get inescapable shock grow the tumor at a greater rate; hence, inescapable shock causes tumor growth in rats. But what does this tell us about the causes of cancer in human beings, and about how being helpless influences cancer in people? This is the problem of external validity.
When laypeople complain about psychological experimentation with the gibe “white rats and college sophomores,” it is external validity that is the issue. Far from being a philistine complaint that psychologists have conveniently chosen to ignore, it is a profound one. Homo sapiens is different in so many ways from the white laboratory version of Rattus norvegicus. Inescapable shock is different in many ways from finding out that your child drowned in a boating accident. The tumor that we implanted on Rattus norvegicus is different in many ways from the naturally occurring tumors that afflict Homo sapiens. So even if the internal validity is perfect—rigorous experimental design, the control group exactly right, the numbers large enough to ensure randomization, and the statistics impeccable—we still cannot infer with confidence that this illuminates the effect uncontrollable bad events exert on the progression of illness in people.
If it is not worth doing, it is not worth doing well.
I have come to think that establishing external validity is an even more important but much more nettlesome scientific inference than establishing internal validity. Academic psychology requires entire courses on internal validity—“methodology” courses—of all serious psychology graduates. These courses are entirely about internal validity and almost never even touch on external validity, which is often passed off as mere ignorance about science on the part of laymen. Hundreds of professors of psychology make their living teaching about internal validity; no one makes a living teaching about external validity. Unfortunately, public doubts about the applicability of basic, rigorous science are often warranted, and this is because the rules of external validity are not clear.
The choice of experimental subjects, for example, has been overwhelmingly a matter of academic convenience as opposed to a matter of deliberation about what inferences would be warranted if the experiment works. White rats never would have been used in psychology if video games had been around in 1910. College sophomores never would have become the subjects of choice in psychology if the World Wide Web had been around in 1930. The bottom line for me, scientifically, is to avoid problems of external validity as much as possible by working with human beings on real-world mastery and real-world helplessness under repeatable conditions. There are, to be sure, instances in which I believe animal experimentation is justifiable, but they are limited to domains in which the problems of external validity are small, the ethical problems of doing the experiment with humans are insuperable, and the human benefits are large. I believe that all the issues that this book addresses can be better illuminated by research with humans, and I now turn back to these issues.
To my description of learned helplessness above, I have to add one important fact: when we gave inescapable noise to people or inescapable shock to animals, not all of them became helpless. With regularity, about one-third of people (and one-third of rats and one-third of dogs) never became helpless. With regularity, about one-tenth of people (and one-tenth of rats and one-tenth of dogs) were helpless to begin with, and they required no laboratory events to induce passivity. It was that observation that led to the field called learned optimism.
We wanted to find out who never became helpless, so we looked systematically at the way that the people whom we could not make helpless interpreted bad events. We found that people who believe that the causes of setbacks in their lives are temporary, changeable, and local do not become helpless readily in the laboratory. When assailed with inescapable noise in the laboratory or with rejection in love, they think, It’s going away quickly, I can do something about it, and it’s just this one situation. They bounce back quickly from setbacks, and they do not take a setback at work home. We call them optimists. Conversely, people who habitually think, It’s going to last forever, it’s going to undermine everything, and there’s nothing I can do about it, become helpless readily in the laboratory. They do not bounce back from defeat, and they take their marital problems into their jobs. We call them pessimists.
So we devised questionnaires to measure optimism as well as content analytic techniques for blindly rating the optimism of every “because” statement in speeches, newspaper quotes, and diaries for measuring people—presidents, sports heroes, and the dead—who won’t take questionnaires. We found that pessimists get depressed much more readily than optimists, that they underachieve in their jobs, in the classroom, and on the sports field, and their relationships are rockier.
Do pessimism and optimism, the great amplifiers of learned helplessness and mastery, respectively, influence illness? And by what mechanisms? How do other positive psychological variables, such as joy, zest, and cheer, influence illness? I will discuss this illness by illness, in the following order: cardiovascular disease, infectious illness, cancer, and all-cause mortality.
Cardiovascular Disease (CVD)
In the mid-1980s, 120 men from San Francisco had their first heart attacks, and they served as the untreated control group in the massive Multiple Risk Factor Intervention Trial (MR FIT) study. This study disappointed many psychologists and cardiologists by ultimately finding no effect on CVD by training to change these men’s personalities from type A (aggressive, time urgent, and hostile) to type B (easy-going). The 120 untreated controls, however, were of great interest to Gregory Buchanan, then a graduate student at Penn, and to me because so much was known about their first heart attacks: extent of damage to the heart, blood pressure, cholesterol, body mass, and lifestyle—all the traditional risk factors for cardiovascular disease. In addition, the men were all interviewed about their lives: family, job, and hobbies. We took every single “because” statement from each of their videotaped interviews and coded them for optimism and pessimism.
Within eight and a half years, half the men had died of a second heart attack, and we opened the sealed envelope. Could we predict who would have a second heart attack? None of the usual risk factors predicted death: not blood pressure, not cholesterol, not even how extensive the damage from the first heart attack. Only optimism, eight and a half years earlier, predicted a second heart attack: of the sixteen most pessimistic men, fifteen died. Of the sixteen most optimistic men, only five died.
This finding has been repeatedly confirmed in larger studies of cardiovascular disease, using varied measures of optimism.
Veterans Affairs Normative Aging Study
In 1986, 1,306 veterans took the Minnesota Multiphasic Personality Inventory (MMPI) and were tracked for ten years. During that time, 162 cases of cardiovascular disease occurred. The MMPI has an optimism-pessimism scale that reliably predicts mortality in other studies. Smoking, alcohol use, blood pressure, cholesterol, body mass, family history of CVD, and education were measured, as was anxiety, depression, and hostility, and all of these were controlled for statistically. Men with the most optimistic style (one standard deviation above average) had 25 percent less CVD than average, and men with the least optimism (one standard deviation below the mean) had 25 percent more CVD than average. This trend was strong and continuous, indicating that greater optimism protected the men, whereas less optimism weakened them.
European Prospective Investigation
More than 20,000 healthy British adults were followed from 1996 to 2002, during which 994 of them died, 365 of them from CVD. Many physical and psychological variables were measured at the outset of the study: smoking, social class, hostility, and neuroticism, for example. Sense of mastery was also measured by seven questions:
- I have little control over the things that happen to me.
- There is really no way I can solve some of the problems I have.
- There is little I can do to change many of the important things in my life.
- I often feel helpless in dealing with the problems of life.
- Sometimes I feel that I am being pushed around in life.
- What happens to me in the future mostly depends on me.
- I can do just about anything I really set my mind to do.
These questions capture the continuum from helplessness to mastery. Death from cardiovascular disease was strongly influenced by a sense of mastery, holding smoking, social class, and the other psychological variables constant. People high (one standard deviation above the mean) in mastery had 20 percent fewer CVD deaths than those with an average sense of mastery, and people high in a sense of helplessness (one standard deviation below the mean in a sense of mastery) had 20 percent more CVD deaths than average. This was also true of deaths due to all causes and—to a lesser extent but still significant statistically—of deaths from cancer.
Dutch Men and Women
Beginning in 1991, 999 sixty-five-to eighty-five-year-olds were followed for nine years in the Netherlands. In that time, 397 of them died. At the outset, researchers measured health, education, smoking, alcohol, history of cardiovascular disease, marriage, body mass, blood pressure, and cholesterol, along with optimism, which was measured by four items answered on a 1-to-3 scale of agreement:
- I still expect much from life.
- I do not look forward to what lies ahead for me in the years to come.
- I am still full of plans.
- I often feel that life is full of promises.
Pessimism was very strongly associated with mortality, particularly when holding all the other risk factors constant. Optimists had only 23 percent the rate of CVD deaths of the pessimists, and only 55 percent the overall death rate compared to the pessimists. Interestingly this protection was specific to optimism, a future-oriented cognition, and present-oriented mood items such as “Happy laughter often occurs” (this must read better in Dutch) and the items such as “Most of the time, I am in good spirits,” did not predict mortality.
In contrast, in the 1995 Nova Scotia Health Survey, a team of nurses rated the positive emotion (joy, happiness, excitement, enthusiasm, contentment) of 1,739 healthy adults. Over the next ten years, participants with high positive emotion experienced less heart disease, with 22 percent less heart disease for each point on a five-point scale of positive emotion. Optimism was not measured, so we cannot determine if positive emotion worked through optimism.
The influence of Dutch optimism was a continuous trend, with more optimism associated with fewer deaths along the entire dimension. These findings show that the effect is bipolar: high optimists die at a lower rate than average, and high pessimists die at a higher rate than average. Recall here the thrust of Paul Tarini’s question: Are there health assets that protect, and not just risk factors that weaken, the body? Optimism, in this study, strengthened people against cardiovascular disease when compared to the average person, just as pessimism weakened them compared to average.
Is depression the real culprit? Pessimism, in general, correlates pretty highly with depression, and depression, in many studies, also correlates with cardiovascular disease. So you might wonder if the lethal effect of pessimism works by increasing depression. The answer seems to be no, since optimism and pessimism exerted their effects even when depression was held constant statistically.
Women’s Health Initiative
In the largest study of the relationship between optimism and cardiovascular disease to date, 97,000 women, healthy at the outset of the study in 1994, were followed for eight years. As usual in careful epidemiological studies, age, race, education, religious attendance, health, body mass, alcohol, smoking, blood pressure, and cholesterol were recorded at the start. Epidemiological studies investigate patterns of health in large populations. Optimism was measured in yet another way by the well-validated Life Orientation Test (LOT), which poses ten statements such as: “In unclear times, I usually expect the best,” and “If something can go wrong for me, it will.” Importantly, depressive symptoms were also measured and their impact assessed separately. The optimists (the top quarter) had 30 percent fewer coronary deaths than the pessimists (bottom quarter). The trend of fewer deaths, both cardiac and deaths from all causes, held across the entire distribution of optimism, indicating again that optimism protected women and pessimism hurt them relative to the average. This was true holding constant all the other risk factors—including depressive symptoms.
Something Worth Living For
There is one trait similar to optimism that seems to protect against cardiovascular disease: ikigai. This Japanese concept means having something worth living for, and ikigai is intimately related to the meaning element of flourishing (M in PERMA) as well as to optimism. There are three prospective Japanese studies of ikigai, and all point to high levels of ikigai reducing the risk of death from cardiovascular disease, even when controlling for traditional risk factors and perceived stress. In one study, the mortality rate from CVD among men and women without ikigai was 160 percent higher than that of men and women with ikigai. In a second study, men with ikigai had only 86 percent of the risk of mortality from CVD compared to men without ikigai; this was also true of women, but less robustly so. And in a third study, men with high ikigai had only 28 percent of the risk for death from stroke relative to their low-ikigai counterparts, but there was no association with heart disease.
SUMMARY OF CARDIOVASCULAR DISEASE
All studies of optimism and CVD converge on the conclusion that optimism is strongly related to protection from cardiovascular disease. This holds even correcting for all the traditional risk factors such as obesity, smoking, excessive alcohol use, high cholesterol, and hypertension. It even holds correcting for depression, correcting for perceived stress, and correcting for momentary positive emotions. It holds over different ways of measuring optimism. Most important, the effect is bipolar, with high optimism protecting people compared to the average level of optimism and pessimism, and pessimism hurting people compared to the average.
Infectious Illness
How long do your colds last? For some people, colds last only seven days, but for many others, they last two or three weeks. Some people ward off colds, even when everyone else is in bed; others get a half dozen colds a year. Your reflexive demurrer is probably “This must be due to immune system differences,” but I need to caution you about rampant immunomythology. I wish that science had established that people with “stronger” immune systems ward off infectious illness better, but this is far from having been nailed down. Surprisingly, however, the influence of psychological states on susceptibility to colds has been nailed down better. The unraveling of the influence of emotion on infectious illness is one of the most elegant stories in all of psychology. The protagonist is a shy and soft-spoken professor of psychology at Carnegie Mellon University, Sheldon Cohen, one of those rare scientists whose research successfully bridges biology and psychology.
It is commonplace that happy people do not complain much: they report fewer symptoms of pain and illness, and they report better health generally. In contrast, sad people complain more about pain, and they report worse health. It is plausible that both actually have the same physical symptoms, but sadness and happiness change only how they perceive their bodily symptoms. Alternatively, this could merely reflect a bias in reporting symptoms, with sad people obsessed with negative symptoms, and happy people focused on what is going well. (Notice that this bias does not explain the optimism-CVD findings, since the outcome here is not the reporting of coronary symptoms but death itself.) So it is parsimonious to pass off the many observations that depressed people have more pain and more colds, and happy people less pain and fewer colds, as uninteresting artifacts of reporting. That is exactly where medical science stood until Sheldon Cohen came along.
Sheldon had the courage to actually infect volunteers with known doses of rhinovirus, the virus that brings you the common cold. I use the word courage because the harrowing story of his getting approval from Carnegie Mellon’s institutional review boards (IRB, explained below) to allow these studies remains untold. But as we shall see, we can be grateful that these studies passed ethical muster.
Ethics and Institutional Review Boards
My admiration of Sheldon’s courage and my gratitude that he was allowed to do the experiments I will shortly describe is based in a deep worry about the shackling of science in the United States today. Beginning in the 1970s, all scientists were required to submit their proposed research to an arm’s-length committee for ethical approval. The group is called an institutional review board, or IRB, and this demand for ethical review came in the wake of scandals in which patients and research subjects were not fully informed about the potentially dangerous procedures they were to undergo. IRBs help prevent universities from getting sued, and they speak well to the ethic of a fully open society. On the downside, IRBs are very costly; I would guess that Penn (just one of thousands of American research institutions) spends a lot more than $10 million per year running IRBs. Institutional review boards mire scientists in a mountain of red tape—my guess is that my laboratory spends five hundred hours per year filling out IRB forms.
The review boards started out to warn people fully about being in a scientific study that might subject them to serious harm, but they have now developed mission creep of the first magnitude: every time a scientist wants to even pilot an innocuous questionnaire on happiness, her first task is to provide hours’ worth of documentation to her institution’s IRB. As far as I know, IRBs have not—in forty years and at the cost of many billions of dollars—saved even a single life. But most important, they have a chilling effect on attempts to conduct potentially lifesaving science. Here’s an example of the most lifesaving study I know in the history of psychology—perhaps in the history of medicine—and this exposes just what is wrong with institutional review boards.
The worst epidemic of madness in recorded history began a few years after Christopher Columbus discovered the New World, and it continued with mounting ferocity until the early twentieth century. We have come to call this disorder general paresis. It begins with a weakness in the arms and legs, proceeds to symptoms of eccentricity followed by downright delusions of grandeur, then finally progresses to massive paralysis, stupor, and death. Its cause was unknown, but there was some suspicion that it was caused by syphilis. Reports of cases in which paretics were known to have had syphilis were clearly not sufficient, since these were contradicted by the many paretics who adamantly denied ever having syphilis and who showed no evidence of the sexually transmitted virus. Some 65 percent of paretics had a demonstrable history of syphilis, compared to only 10 percent of non-paretics. That evidence, of course, was merely suggestive: it did not demonstrate cause, since it did not show that 100 percent of paretics had prior histories of syphilis.
The overt symptoms of syphilis—the sores on the genitals—disappear in a few weeks, but the disease does not. Like measles, if you contract syphilis once, you can’t get it again. More bluntly, if someone who has already become syphilitic (a paretic) comes in contact with another syphilitic germ, he will not develop sores on his genitals.
There was one means, but a risky one, of finding out by way of an experiment if all paretics had previously had syphilis. If you injected paretics with the syphilis germ, one startling result would come about. The paretics would not contract the disease, since you cannot get syphilis twice. Betting on this outcome, the German neurologist Richard von Krafft-Ebing (1840–1902) performed this critical experiment. In 1897 he inoculated with material from syphilitic sores nine paretics, all of whom had denied ever having had syphilis. None developed sores, leading to the conclusion that they must have already been infected.
So successful was Krafft-Ebing’s work that the most common mental illness of the nineteenth century was soon eradicated with antisyphilitic medication and hundreds of thousands of lives were saved.
The moral of this story is that this experiment could not be carried out today. No institutional review board would approve it. But much worse, no scientist—not even the most courageous one—would even submit such a proposal to an IRB—no matter how many lives she believed would be saved.
Sheldon Cohen’s studies, like Krafft-Ebing’s, deserve the appellation courageous because they have the potential to save many lives. Cohen pioneered the causal influence of positive emotion on infectious illness within a bold experimental design. In all of Cohen’s studies, large numbers of healthy volunteers are first interviewed nightly for seven nights. They are well paid and fully informed of the risks. Yet many IRBs would not allow even this study to go forward because to them “well paid” equals “coercion.”
From these interviews and tests, the average mood—positive emotion and negative emotion—is rated. Positive emotion consists of the observer ratings “full of pep,” “energetic,” “happy,” “at ease,” “calm,” and “cheerful.” Negative emotion consists of “sad,” “depressed,” “unhappy,” “nervous,” “hostile,” and “resentful.” Notice that these are not ratings of the future-oriented traits of optimism and pessimism (for instance, “I expect many bad things to recur”), as in the medical literature concerning the association between mood and cardiovascular disease, but rather ratings of momentary emotional states. Possible confounds, or lurking extraneous factors, are also measured: age, sex, race, health, body mass, education, sleep, diet, exercise, antibody levels, and optimism.
Then all of the volunteers get rhinovirus squirted into their noses (shades of Krafft-Ebing) and are kept under observation and in quarantine for six days to let the cold develop. The cold is measured not only by self-report of symptoms (which could be biased by how much different individuals complain), but more directly by mucus production (the snotty tissues are weighed) and congestion (the amount of time it takes a dye injected into the nose to reach the back of the throat). The results are remarkable and conclusive:
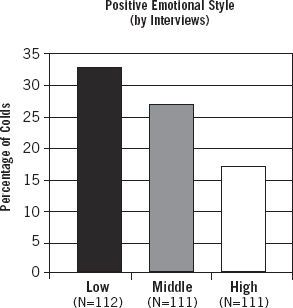
People with high positive emotion before the rhinovirus develop fewer colds than people with average positive emotion. And they, in turn, get fewer colds than people with low positive emotion. The effect is bidirectional, with high positive emotion strengthening volunteers compared to average, and low positive emotion weakening volunteers compared to average:
There is a smaller effect of negative emotion, with people low in negative emotion having fewer colds than the others. Importantly, positive emotion, not negative emotion, is clearly the driving force.
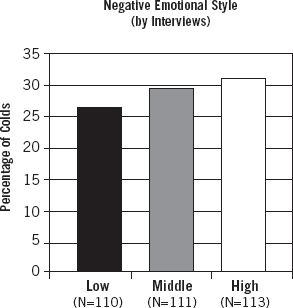
By what biological mechanism does positive emotion reduce colds? Since the volunteers are kept in quarantine and closely observed, differences in sleep, diet, cortisol, zinc, and exercise are ruled out. The key difference is interleukin-6, a protein that causes inflammation.
THE WAYS TO FLOURISH
The higher the positive emotion (PES), the lower the interleukin-6 (IL-6), and so the less the inflammation.
Sheldon replicated this study with flu virus as well as cold virus, with the same results: positive emotional style is the driving factor. In addition, he ruled out self-reported health, optimism, extraversion, depression, and self-esteem differences.
Cancer and All-Cause Mortality
Are positive states a panacea? In my very first speculations about helplessness and illness in the 1970s, I cautioned about the limits that psychological influences such as optimism might have on physical disease. In particular, I was concerned with the severity of illness, and I guessed that lethal and terminal illness could not be influenced by the psychological state of the victim. I wrote hyperbolically that “if a crane falls on you, optimism is not of much use.”
Barbara (“I Hate Hope”) Ehrenreich
I have been reminded of this in recent years by an Australian study showing that hope and optimism have no measurable effect on prolonging life in patients with inoperable cancer. Barbara Ehrenreich recently published Bright-Sided: How the Relentless Promotion of Positive Thinking Has Undermined America, in which she describes her personal experience with well-meaning health care workers telling her that her breast cancer could be relieved if only she were a more positive person. She then goes on to dismiss positive psychology. Ehrenreich is resentful of the happiness police insisting that she adopt a cheerful posture in order to conquer her breast cancer. There is no reason at all to believe that faking positive emotion in order to live longer will work, and I know of no one who advocates urging patients to fake well-being. In spite of this, Ehrenreich titled the British edition of her book Smile or Die.
I had a revealing exchange with Ehrenreich right after Smile or Die was published in England. I sent her a hot-off-the-press article about baseball players’ longevity: the intensity of smiling in the 1952 Baseball Register photos predicted how long players would live, with those showing a genuine (Duchenne) smile living seven years longer than those not smiling.
“I guess I’m doomed,” she quipped in her return email.
“As wrongheaded and evidence-ignoring as I believe your analysis is,” I responded, and here is the point that Ehrenreich misses, “cardiovascular disease, all-cause mortality, and quite possibly cancer are not a function of fake smiling but rather of PERMA, some configuration of positive emotion, plus meaning, plus positive relationships, plus positive accomplishment. You may be low on the first (as am I), but you have many of the others, I gather, and your book—as uncongenial as I find it—is surely a meaningful and positive accomplishment. So—ironically—taking on the positive as you do is itself a major positive (when “positive” is appropriately understood to be broader than enforced smiling) in your life.
“So you are not doomed.”
In her book, Ehrenreich failed to address the full range of the scientific literature, but her book triggered some glowing reviews, in which the reviewers took Ehrenreich’s conclusions at face value. The most egregious review came from Michael Shermer, founding editor of Skeptic magazine. “Ehrenreich systematically deconstructs—and then demolishes—what little science there is behind the positive psychology movement and the allegedly salubrious effects of positive thinking. Evidence is thin. Statistical significance levels are narrow. What few robust findings there are often prove to be either nonreplicable or contradicted by later research.” As the reader can see from this chapter, the evidence is robust, significance levels are high, and the findings replicate over and over.
So, Ehrenreich’s and Shermer’s rants aside, what is the actual state of the evidence about positivity and cancer? The most complete review, “Optimism and Physical Health: A Meta-Analytic Review,” was published in Annals of Behavioral Medicine in 2009. It meta-analyzes eighty-three separate studies of optimism and physical health. A “meta-analysis” averages over all the methodologically sound studies of a topic in the entire scientific literature. Conflicting findings are the rule for the effect of psychological well-being on survival per se and for almost every other finding in the social-science literature. (This is indeed how science progresses.)
To what extent, the authors ask, does optimism predict mortality from all causes, cardiovascular disease, immune function, and cancer? Eighteen of these eighty-three studies, involving a total of 2,858 patients, concern cancer. Taken together, they find that more optimistic people have better cancer outcomes, at a robust level of significance. The largest and most recent study involved 97,253 women from the Women’s Health Initiative study above, and measured the relationship of optimism and of “cynical hostility” to the prediction of cardiovascular disease, all-cause mortality, and cancer. Pessimism was a major predictor of CVD mortality, as mentioned above. Importantly, pessimism and cynical hostility were both significant predictors of cancer, particularly among African-American women, although the effect was smaller than for CVD.
Ehrenreich asked me for help preparing her book. We had two face-to-face meetings largely about the research literature on health. I then sent her an extensive bibliography and articles. Rather than present the full range of studies, however, Ehrenreich cherry-picks her way though some of the research, highlighting the minority of null evidence and failing to review the well-done studies that find that optimism significantly predicts better cardiovascular, all-cause mortality, and cancer outcomes. Cherry-picking is in the abstract one of the minor forms of intellectual dishonesty, but in matters of life and death, cherry-picking to dismiss the value of optimism and hope for women with cancer is, in my opinion, dangerous journalistic malpractice.
Of course, there are no experimental studies in which people are randomly assigned to “getting optimism” and “getting cancer,” so it is possible to doubt whether pessimism causes cancer and death. But these studies control for the other risk factors for cancer and still find that optimistic patients fare better. The evidence is sufficient to warrant a random-assignment, placebo-controlled experiment in which pessimistic women with cancer are randomly assigned to Penn Resiliency Training or to a health information control group, and followed for morbidity, mortality, quality of life, and health care expenditure.
So my overview of the cancer literature is that it leans quite heavily in the direction of pessimism as a risk factor for developing cancer. But because a noticeable minority of the cancer studies do not find significant effects (although not a single one shows that pessimism benefits cancer patients), I conclude that pessimism is a likely but a weaker risk factor for cancer than it is for cardiovascular disease and all-cause mortality.
Therefore, I would hazard from the entirety of the cancer literature that hope, optimism, and happiness may well have beneficial effects for cancer patients when the disease is not extremely severe. But caution is in order before dismissing positivity altogether even there. A letter in response to my crane-falling article on the limits of optimism began: “Dear Dr. Seligman: A crane fell on me, and I am alive today only because of my optimism.”
Studies that look at mortality from all causes are relevant to whether psychological well-being can actually help you if a crane falls on you. Yoichi Chida and Andrew Steptoe, psychologists from the University of London, recently published an exemplary comprehensive meta-analysis. Chida and Steptoe averaged seventy studies together, thirty-five of which began with healthy participants and thirty-five of which began with diseased participants.
Their meta-analysis finds that over all seventy studies, psychological well-being protects. The effect is quite strong if you are presently healthy. People who have high well-being are 18 percent less likely to die of any cause than those with low well-being. Among the studies that start out with sick people, those with high well-being show a smaller but significant effect, dying at the rate of 2 percent less than those with lower well-being. As for cause of death, a sense of well-being protects people against death from CVD, renal failure, and HIV, but not significantly for cancer.
Is Well-Being Causal, and How Might It Protect?
I conclude that optimism is robustly associated with cardiovascular health, and pessimism with cardiovascular risk. I conclude that positive mood is associated with protection from colds and flu, and negative mood with greater risk for colds and flu. I conclude that highly optimistic people may have a lower risk for developing cancer. I conclude that healthy people who have good psychological well-being are at less risk for death from all causes.
Why?
The first step in answering why is to ask if these are really causal relations or just correlations. This is a crucial scientific question, since some third variable, such as a loving mother or an excess of serotonin might be the real cause, with a loving mother or high serotonin causing both good health and psychological well-being. No observational study can eliminate all possible third variables, but most of the studies above eliminate the likely possibilities by statistically equating people for exercise, blood pressure, cholesterol, smoking, and a host of other plausible confounds.
The gold standard for eliminating all third variables is a random-assignment placebo-controlled experiment, and there exists only one in the optimism-health literature. Fifteen years ago, when Penn’s freshman class was admitted, I sent the entire class the Attributional Style Questionnaire, and everyone took it. (Students are very cooperative upon admission.) Gregory Buchanan and I then wrote the most pessimistic quarter of freshmen, at risk for depression on the basis of their very pessimistic explanatory style scores, and randomly invited them into one of two groups: an eight-week “stress management seminar” consisting of the Penn Resiliency Program (Learned Optimism), as discussed in the “Positive Education” and “Army Strong” chapters, or a no-intervention control group. We found that the seminar raised optimism markedly and lowered depression and anxiety over the next thirty months, as we’d predicted. We also assessed the students’ physical health over that period. Participants in the seminar group had better physical health than did the controls, with fewer self-reported symptoms of physical illness, fewer doctor visits overall, and fewer illness-related visits to the student health center. The seminar group was more likely to visit doctors for preventive checkups, and its members had healthier diets and exercise regimens.
This lone experiment suggests that it is the change in optimism itself that improved health, since random assignment to intervention versus control eliminates the unknown third variables. We do not know if this causal path is true of optimism in the cardiovascular disease literature, since no one has yet conducted a random-assignment study, teaching patients optimism to prevent heart attacks. One cheer, so far, for causality.
Why Optimists Are Less Vulnerable to Disease
How might optimism work to make people less vulnerable and pessimism to make people more vulnerable to cardiovascular disease? The possibilities divide into three large categories:
1. Optimists take action and have healthier lifestyles. Optimists believe that their actions matter, whereas pessimists believe they are helpless and nothing they do will matter. Optimists try, while pessimists lapse into passive helplessness. Optimists therefore act on medical advice readily, as George Vaillant found when the surgeon general’s report on smoking and health came out in 1964; it was the optimists who gave up smoking, not the pessimists. Optimists may take better care of themselves.
Even more generally, people with high life satisfaction (which correlates highly with optimism) are much more likely to diet, not to smoke, and to exercise regularly than people with lower life satisfaction. According to one study, happy people also sleep better than unhappy people.
Optimists not only follow medical advice readily, they also take action to avoid bad events, whereas pessimists are passive: optimists are more likely to seek safety in tornado shelters when there is a tornado warning than pessimists, who may believe the tornado is God’s will. The more bad events that befall you, the more illness.
2. Social support. The more friends and the more love in your life, the less illness. George Vaillant found that people who have one person whom they would be comfortable calling at three in the morning to tell their troubles were healthier. John Cacioppo found that lonely people are markedly less healthy than sociable people. In an experiment, participants read a script over the phone to strangers—reading in either a depressed voice or a cheerful voice. The strangers hang up on the pessimist sooner than on the optimist. Happy people have richer social networks than unhappy people, and social connectedness contributes to a lack of disability as we age. Misery may love company, but company does not love misery, and the ensuing loneliness of pessimists may be a path to illness.
3. Biological mechanisms. There are a variety of plausible biological paths. One is the immune system. Judy Rodin (whom I mentioned in the opening of the book), Leslie Kamen, Charles Dwyer, and I collaborated together in 1991 and took blood from elderly optimists and pessimists and tested the immune response. The blood of optimists had a feistier response to threat—more infection-fighting white blood cells called T lymphocytes produced—than the pessimists. We ruled out depression and health as confounds.
Another possibility is common genetics: optimistic and happy people might have genes that ward off cardiovascular disease or cancer.
Another potential biological path is a pathological circulatory response to repeated stress. Pessimists give up and suffer more stress, whereas optimists cope better with stress. Repeated episodes of stress, particularly when one is helpless, likely mobilize the stress hormone cortisol and other circulatory responses that induce or exacerbate damage to the walls of blood vessels and promote atherosclerosis. Sheldon Cohen, you will recall, found that sad people secrete more of the inflammatory substance interleukin-6, and that this results in more colds. Repeated episodes of stress and helplessness might set off a cascade of processes involving higher cortisol and lower levels of the neurotransmitters known as catecholamines, leading to long-lasting inflammation. Greater inflammation is implicated in atherosclerosis, and women who score low in feelings of mastery and high in depression have been shown to have worse calcification of the major artery, the trunk-like aorta. Helpless rats, in the triadic design, develop atherosclerosis at a faster rate than rats that demonstrate mastery.
Excessive production by the liver of fibrinogen, a substance used in clotting the blood, is another possible mechanism. More fibrinogen leads to more blood clots in the circulatory system by making the blood sludgy. People with high positive emotion show less of a fibrinogen response to stress than those with low positive emotion.
Heart rate variability (HRV), surprisingly, is another candidate for protection against cardiovascular disease. HRV is the short-term variation in beat-to-beat intervals, which is partly controlled by the parasympathetic (vagal) system of the central nervous system. This is the system that produces relaxation and relief. Accumulating evidence suggests that people with high heart rate variability are healthier, have less CVD, less depression, and better cognitive abilities.
The mechanisms proposed above have not been well tested. They are simply reasonable hypotheses, but each can be bidirectional, with optimism adding to protection compared to the average, and pessimism weakening people compared to the average. The gold standard for finding out if optimism is causal and how it works is the optimism intervention experiment. There is an obvious and expensive experiment very much worth doing: we take a large group of people vulnerable to CVD, randomly assign half to optimism training and half to a placebo, monitor their action, social, and biological variables, and see if optimism training is lifesaving. And this takes me back to the Robert Wood Johnson Foundation.
All of this—learned helplessness, optimism, CVD, and how to pin down the mechanism—raced through my mind when Paul Tarini visited me. “We want to invite you to send us two proposals,” Paul concluded after a long discussion, “one exploring the very concept of positive health, and the second proposing an optimism intervention to prevent CVD deaths.”
Positive Health
In due course, I submitted both proposals. The intervention proposal mobilized the Cardiology Department at Penn and we proposed the random-assignment Penn Resiliency Program intervention given to large numbers of people after their first heart attack. The other proposed exploring the concept of positive health, and it was this one that the foundation funded in the belief that a well-defined concept of positive health came first. The positive health group has now been at work for a year and a half, and it has four main thrusts:
- Defining positive health
- Reanalysis of existing longitudinal studies
- Cardiovascular health assets
- Exercise as a health asset
DEFINING POSITIVE HEALTH
Is health more than the absence of illness, and can it be defined by the presence of positive health assets? We don’t yet know what the health assets actually are, but we have strong clues about what some of them may be, such as optimism, exercise, love, and friendship. So we start with three entire classes of potential positive independent variables. First, subjective assets: optimism, hope, a sense of good health, zest, vitality, and life satisfaction, for example. Second, biological assets: the upper range of heart rate variability, the hormone oxytocin, low levels of fibrinogen and interleukin-6, and longer repetitive strands of DNA called telomeres, for example. Third, functional assets: excellent marriage, walking briskly up three flights of steps at age seventy without breathlessness, rich friendships, engaging pastimes, and a flourishing work life, for example.
The definition of positive health is empirical, and we are investigating the extent to which these three classes of assets actually improve the following health and illness targets:
- Does positive health extend life span?
- Does positive health lower morbidity?
- Is health care expenditure lower for people with positive health?
- Is there better mental health and less mental illness?
- Do people in positive health not only live longer but have more years in good health?
- Do people in positive health have a better prognosis when illness finally strikes?
So the definition of positive health is the group of subjective, biological, and functional assets that actually increase health and illness targets.
Longitudinal Analysis of Existing Data Sets
The definition of positive health will thus emerge empirically, and we have started by reanalyzing six large long-term studies of predictors of illness—studies that originally focused on risk factors, not on health assets. Under the leadership of Chris Peterson, the leading scholar of strengths, and Laura Kubzansky, a young Harvard professor who reanalyzes cardiovascular disease risk for its psychological underpinnings, we are asking if these studies, reanalyzed for assets, predict the health targets above. While the existing data sets concentrate on the negative, these six contain more than a few snippets of the positive, which until now have been largely ignored. So, for example, some of the tests ask about levels of happiness, exemplary blood pressure, and marital satisfaction. We will see what configuration of positive subjective, biological, and functional measures emerge as health assets.
Chris Peterson is hunting down character strengths as health assets. The ongoing Normative Aging Study, begun in 1999, includes two thousand men who were healthy at the outset and are assessed every three to five years for cardiovascular disease. They also undergo a battery of psychological tests each time. One of these is the Minnesota Multiphasic Personality Inventory-2, from which a “self-control” measure has been derived. Chris reports that, holding the usual risk factors constant (and even controlling for optimism), self-control is a major health asset: men with the highest self-control have a 56 percent reduced risk for CVD.
This is an example of how we are comparing health assets to risk factors. We can also make quantitative comparisons of the potency of health assets to risk factors; for example, we estimate that being in the upper quartile of optimism seems to have a beneficial effect on cardiovascular risk roughly equivalent to not smoking two packs of cigarettes daily. (But don’t hold me to the number two just yet.) Furthermore, does any specific configuration of these health assets optimally predict the targets? Such an optimal configuration of health assets, if it exists, defines empirically the latent variable of positive health with respect to any given disease. That configuration of health assets that is general across a range of diseases defines general positive health.
Once a single positive independent variable is convincingly shown to be a health asset, positive health suggests intervening to build this variable. So, for example, if the risk of cardiovascular death is lower with optimism, or exercise, or a harmonious marriage, or being in the upper quarter of heart rate variability, these become tempting (and inexpensive) targets of intervention. In addition to the practical value of discovering a lifesaving intervention in random-assignment, controlled designs, such intervention studies isolate cause. Positive health then seeks to quantify the cost-effectiveness of such positive interventions and to compare their cost-effectiveness to traditional interventions, such as lowering blood pressure, as well as to combine positive health interventions with traditional interventions and to investigate their joint cost-effectiveness.
Army Database: A National Treasure
Our collaboration with the army will, we expect, become the mother of all future longitudinal studies. Roughly 1.1 million soldiers are taking the Global Assessment Tool, measuring all the positive dimensions and health assets together with the usual risk factors over their entire careers. We expect to join their performance records and their lifetime medical records to the GAT. There are data sets in the army containing information on:
- Health care utilization
- Diagnoses of illness
- Medication
- Body mass index
- Blood pressure
- Cholesterol
- Accidents and mishaps
- Combat and noncombat injuries
- Physical shape
- DNA (needed to identify corpses)
- Job performance
So we can test in a very large sample the extent to which subjective, functional, and biological health assets (taken together and taken separately) predict the following:
- Specific illnesses
- Medication
- Health care utilization
- Mortality
This means that we will be able to answer definitively questions such as:
• Do emotionally fit soldiers suffer fewer infectious illnesses (as measured by antibiotic medication) and better prognosis (as measured by briefer courses of medication) when infection occurs, holding other health variables constant?
• Do soldiers satisfied with their marriage incur lower health care costs?
• Do soldiers who function well socially recover faster from childbirth, a broken leg, or heatstroke?
• Are there identifiable “superhealthy” soldiers (high in subjective, functional, and physical indicators) who need minimal health care, rarely get ill, and recover rapidly when they do?
• Are psychologically fit soldiers less likely to have accidents and to be wounded in combat?
• Are psychologically fit soldiers less likely to be evacuated for nonbattle injuries, disease, and psychological health issues during a deployment?
• Is the physical health of the leader contagious to the health of subordinates? And if so, is it in both directions (good and bad health contagion)?
• Do particular strengths as measured by the Signature Strengths test predict better health and lower costs?
• Does Penn Resilience Training save lives, both on the battlefield, and from naturally occurring illness?
We are under way, as I write, in reanalyzing the six promising data sets and marrying our Robert Wood Johnson efforts to the U.S. Army’s Comprehensive Soldier Fitness initiative. Stay tuned.
Cardiovascular Health Assets
I am just back from my fiftieth high school reunion. What amazed me was how healthy my classmates are. Fifty years ago, sixty-seven-year-old men were packing it in, sitting in rocking chairs on porches and waiting to die. Now they run marathons. I gave a brief speech about our expected mortality.
A healthy man at age sixty-seven today has a life expectancy of around twenty years. So, unlike our fathers and grandfathers, who were near the end of life at sixty-seven, we are just entering the last quarter of our lives. There are two things we can do to maximize the chances that we will attend our seventieth reunion. The first is to be future oriented: to be drawn into the future, as opposed to dwelling in the past. Work not just for your personal future but the future of your family, this school (the Albany Academies), your nation, and your dearest ideals.
Second, exercise!
This was my summary of the present state of the science of cardiovascular health as we conceive it. Is there a set of subjective, biological, and functional assets that will boost your resistance to cardiovascular disease beyond average? Is there a set of subjective, biological, and functional assets that will improve your prognosis beyond average if you should have a heart attack? This vital question is largely ignored in CVD research, which focuses on the toxic weaknesses that decrease resistance or undermine prognosis once a first heart attack occurs. The beneficial effect of optimism as a health asset on CVD is a good start, and the aim of our Cardiovascular Health Committee is to broaden our knowledge of health assets.
The committee, at work as I write, is headed by Dr. Darwin Labarthe, director of cardiovascular epidemiology at the U.S. Centers for Disease Control (CDC). This, I must mention, completes a circle in life for me. Darwin was my idol during my college years: he was president of the senior class at Princeton when I entered as a freshman in 1960, and he gave the unforgettable first speech—about honor and acting in the nation’s service—on my very first day. Darwin went on to found Wilson Lodge, the nonselective anticlub organization, which was the home and haven for many of the seriously intellectual and activist Princeton undergraduates. While I followed in his footsteps in the leadership of Wilson Lodge, I only admired him from afar as a student, and it has been a matter of immense personal gratification to work with him fifty years later in the service of human flourishing.
Exercise as a Health Asset
“Who should head the exercise committee?” I asked Ray Fowler.
Few of us are lucky enough to acquire mentors after age fifty. Ray became mine when I became president of the American Psychological Association in 1996. He had been president ten years before and had served as CEO (the real seat of power) ever since. In my first couple of months, as an innocent academic, I bumbled my way around the politics of psychotherapy, getting a bloody nose trying to convince the leading private practitioners to get behind evidence-based therapy. Pretty soon I was in “deep shit” with the practitioners.
I reported all this to Ray, and in his soft Alabama accent, he gave me the best political advice I ever heard. “These committee people have great sitting power. APA is a political minefield, and they have been mining it for two decades. You can’t begin to deal with them using transactional leadership—they are the grand masters of process. You shine at transformational leadership. Your job is to transform psychology. Use your creativity and come up with a new idea to lead APA.”
That, along with my five-year-old daughter telling me I should stop being a grouch and Atlantic Philanthropies, was the start of positive psychology. Since then, I have leaned on Ray repeatedly for advice.
Ray is a seventy-nine-year-old marathoner and a man of legendary willpower. Thirty years ago as a depressed, overweight couch potato, he decided he would transform himself and never having run before, he would run the Boston Marathon the following year. And he did. He is now about 120 pounds and all muscle. There is an annual ten-mile run at the APA convention every summer, and Ray always wins his division. (He says that the only reason he wins is that the competition in his age group is thinning out.) It is now called the Ray Fowler Race.
Ray was one of the visiting scholars who stayed with me at the Geelong Grammar School in Australia in January 2008. One extremely hot evening, he lectured to the faculty about physical exercise and cardiovascular disease, presenting the data that people who walk ten thousand steps every day markedly lower their risk for heart attack. We applauded politely at the end of the lecture, but in real tribute, we all went out and bought pedometers the next day. As Nietzsche tells us, good philosophy always says, “Change your life!”
In response to my question about who should head the exercise committee, Ray advised, “The leading person in exercise, Marty, bar none, is Steve Blair. Everything I know about exercise I learned from Steve. Try to get him to head the committee.”
I asked Steve, and he said yes. Like Ray, Steve is all muscle, but unlike Ray, who is shaped like a string bean, Steve is shaped like an eggplant: a five-foot-three-inch, 190-pound eggplant. Like Ray, Steve is a runner and a walker. If you looked at a silhouette of Steve, you would call him obese, and his work is at the center of the obesity-exercise controversy.
Fitness Versus Fatness
The United States has a great deal of obesity, enough so that many call it an epidemic, and huge resources are expended by the government and by private foundations, Robert Wood Johnson included, to curtail this epidemic. Obesity is undeniably a cause of diabetes, and on that ground alone, measures to make Americans less fat are warranted. Steve believes, however, that the real epidemic, the worst killer, is the epidemic of inactivity, and his argument is not lightweight. Here is the argument:
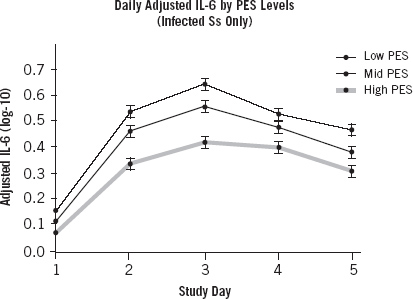
Poor physical fitness correlates strongly with all-cause mortality, and particularly with cardiovascular disease.

These data (and many others) show clearly that highly fit men and women over sixty have a lower death rate from cardiovascular disease and all causes than the moderately fit, who in turn have a lower death rate than the unfit. This may or may not be true of death from cancer. Lack of exercise and obesity go hand in hand. Fat people don’t move around much, whereas thin people are usually on the go.
So which of these two—obesity or inactivity—is the real killer?
There is a huge literature that shows that fat people die of cardiovascular disease more than thin people, and this literature is careful, adjusting for smoking, alcohol, blood pressure, cholesterol, and the like. Very little of it, unfortunately, adjusts for exercise. But Steve’s many studies do. Here is a representative one:
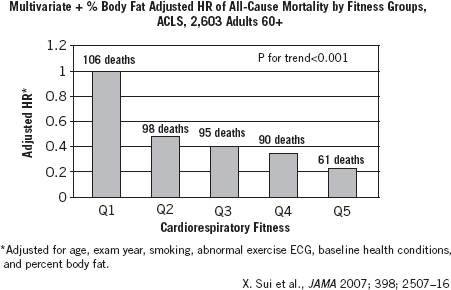
This is the all-cause rate of death for five categories of fitness, holding constant body fat, age, smoking, and the like. The better the fitness, the lower the death rate. This means that two individuals—one in the top fifth of fitness and the other in the bottom fifth of fitness—who weigh exactly the same, have very different risks of death. The fit, but fat, individual has almost half the risk of death of the unfit, fat individual.
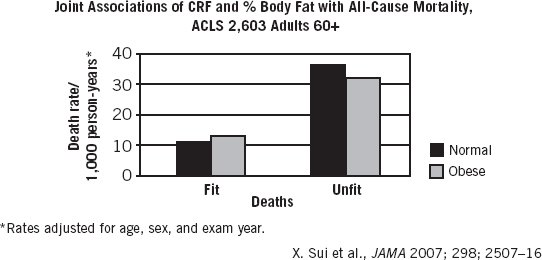
These data show the risk for death in normal-weight versus obese people who are fit or unfit. In the unfit groups, normal and obese people both have a high risk for death, and it does not seem to matter if you are fat or thin. In the fit groups, both fat and thin people have a much lower risk of death than their counterparts in the unfit groups, with fat but fit people at only slightly more risk than thin fit people. But what I now emphasize is that fat people who are fit have a low risk of death.
Steve concludes that a major part of the obesity epidemic is really a couch potato epidemic. Fatness contributes to mortality, but so does lack of exercise. There are not enough data to say which contributes more, but they are compelling enough to require that all future studies of obesity and death adjust carefully for exercise.
These are important conclusions for the average fat adult. Most dieting is a scam, a $59 billion scam last year in America. You can take off 5 percent of your weight in one month by following any diet on the best-seller list. The problem is that 80 percent to 95 percent of people will regain all that weight or more over the next three to five years, just like I did. Dieting can make you thinner, but it is usually only temporary. It does not make you healthier, however, because for most of us, dieting does not stick.
Exercise, in contrast, is not a scam. A much higher percentage of people who take up exercise stick with it and become permanently fit. Exercise is sticky and self-maintaining, dieting is usually not. Even though it lowers your risk for death, exercise will not make you much thinner, since the average vigorous exerciser loses fewer than five pounds of body weight.
Just as optimism is a subjective health asset for cardiovascular disease, it is clear that exercise is a functional health asset: people who exercise a moderate amount have increased health and low mortality, while couch potatoes have poor health and high mortality. The beneficial effects of exercise on health and illness are finally well accepted even within the most reductionist part of the medical community, a guild very resistant to any treatment that is not a pill or a cut. The surgeon general’s 2008 report enshrines the need for adults to do the equivalent of walking 10,000 steps per day. (The real danger point is fewer than 5,000 steps a day, and if this describes you, I want to emphasize that the findings that you are at undue risk for death are—there is no other word for it—compelling.) To take the equivalent of 10,000 steps a day can be done by swimming, running, dancing, weight lifting; even yoga and a host of other ways of moving vigorously.
What we need to discover now are new ways to get more people off the couch. I’m not waiting for new techniques, however. I found one that really works for me. The day after Ray’s talk, not only did I buy a pedometer, but I began—for the first time in my life—to walk. And walk. (I gave up swimming, having swum two-thirds of a mile a day for twenty years and failing to find any technique that kept me from being bored out of my skull.) I formed an Internet group of pedometrized walkers. Ray and Steve are in it, and also about a dozen other people from several walks of life, varying in age from seventeen to seventy-eight, from Down syndrome adults to chaired professors. We report to each other every night exactly how many steps we walked that day. The day feels like a failure under 10,000. When I find myself before bedtime at only 9,000 steps, I go out and walk around the block before reporting in. We reinforce one another for exceptional walking: Margaret Roberts just reported 27,692 steps, and I sent her a “Wow!” We give one another advice about exercise: my left ankle really hurt for two weeks, and my fellows told me, correctly, that my sneakers—with their new, expensive insoles—had become too tight. “Buy an airdesk [www.airdesks.com],” Caroline Adams Miller advised me. “That way you can play bridge online and walk on the treadmill at the same time.” We have become friends, bonded by this common interest. I believe such Internet groups are one new technique that will save lives.
I made a New Year’s resolution for 2009: to take 5 million steps, 13,700 per day on average. On December 30, 2009, I crossed the 5 million mark, and got “Wow!” and “What a role model!” from my Internet friends. So effective is this group for exercise that I am now trying this out for dieting. Having failed at dieting once every year for forty years, and knowing that I am among the 80 percent to 95 percent who regain all the weight we lose, I am at it again. I started 2010 at 215 pounds, and I also started reporting my daily caloric intake, as well as my number of steps, every night to my Internet friends. Yesterday I took in 1,703 calories and walked 11,351 steps. Today, February 19, 2010, for the first time in more than twenty years, I weigh less than 200 pounds.