Chapter 1
The New Patient
- History
- Principles of examination
- Systematic procedure for examination of the oro-facial tissues
- Special investigation
- Diagnosis
- Treatment planning
It is difficult to overstress the importance of a good history and thorough clinical examination for every patient. It is on this that the diagnosis is made and the treatment plan based. A full, clearly written record of the original consultation is essential to assess progress following treatment. This is particularly true if a colleague should be called to see the patient in the practitioner’s absence. The medico-legal importance of accurate records cannot be overemphasised.
In hospital and specialist practice this procedure can seldom be relaxed, but the student and the busy practitioner may find it irksome to maintain a high standard when faced with a series of apparently straightforward dental conditions. Nevertheless, sufficient time must be allowed for an unhurried consultation at the first visit. This will help to avoid errors of omission, and may contribute much to the success of treatment and to the interest of the practitioner. With experience, only important facts need be noted, the dental surgeon considering and setting aside the irrelevant points. This technique can be used with safety only after a long apprenticeship during which many histories and examinations have been methodically completed and all the information recorded. In this chapter a system for interviewing and examining patients, and recording findings, is briefly suggested.
History
At the first meeting it is important for the clinician to establish a rapport with the patient and to assess attitudes to the clinical situation. Behavioural issues must be addressed, attempting to put the patient at ease in what is for many a confrontational situation. The interview must be planned to facilitate the process, seating the patient comfortably, adjusting the chair as required to show care, as well as addressing them by the correct name and title. Even at this stage it should be possible to determine whether the patient is anxious or relaxed. The general details of age, sex, marital status, occupation and contact details, together with the names of their general medical and dental practitioner, should be available in the notes but can be checked. The history is then recorded under the headings shown in italics.
The patient will seldom tell their story well. Some will be verbose, others reticent, while the sequence is usually in inverse chronological order with the most recent events first. The art of the good history lies in avoiding leading questions, in eliciting all the essentials, in censoring verbosity and in arranging the facts in their true order, so that the written record is short and logical. Allowing the patient initially to give the history and subsequently writing notes in chronological order while rechecking and summarising the facts verbally, helps the clinician obtain a concise and accurate account of the patient’s symptoms.
Patient Referred By
The name and professional status of the person referring is noted. This facilitates a reply to the referral in the form of a letter.
Complains of (CO)
The patient’s chief complaint told in their own words. Opinions, professional and otherwise, repeated in an effort to help must be gently set aside and the patient encouraged to describe the symptoms they want cured, and not their views on the diagnosis.
History of Present Complaint (HPC)
This is an account in chronological order of the presenting complaint. When and how it first started, the suspected cause, any exacerbating factors and the character of the local lesion, such as pain, swelling and discharge. This includes remissions and the effects of any treatment received. General symptoms such as fever, malaise and nausea are also noted.
Previous Dental History (PDH)
This records how regularly the patient attends for dental care and the importance they attach to their teeth. Any past experience of oral surgery is included, especially where difficulty occurred in the administration of anaesthetics, the extraction of teeth and the control of bleeding.
Medical History (MH)
A summary in chronological order of the patient’s past illnesses. Details of prolonged illness or those requiring hospital admission are recorded. Current medication, which can give insight into the severity of any underlying conditions, and allergies of any kind, particularly drugs that might be prescribed and latex, must be noted. The more important medical conditions are discussed in Chapter 3.
The Family History (FH)
Occasionally this is of importance in oral surgery. Hereditary diseases such as the haemophilias and hypodontia together with autoimmune disease may be relevant in management of the patient.
The Social History (SH)
This includes a brief comment on the patient’s occupation and social habits, such as exercise, smoking and drinking. The home circumstances are important when surgery is to be performed – that is, whether the patient has far to travel, lives alone or has someone to look after them. These factors may influence the decision to treat as an in- or outpatient.
Principles of Examination
The basic principles of examination are the same in all fields of healthcare. It should be made according to a definite system, which in time becomes a ritual. In this way errors of omission are avoided.
From the moment the patient enters the surgery they should be carefully observed for signs of physical or of psychological disease which may show in the gait, the carriage, the general manner, or the relationship between parent and child. Too little time is often spent on visual inspection, both intra- and extraorally. Eyes first, then hands, should be the rule, not both together.
In palpation, all movements are purposeful and logical, and the touch firm but gentle. The tips of the fingers are used first to locate anatomical landmarks and then to determine the characteristics of the pathological condition. The patient’s co-operation is sought so that areas of tenderness may be recognised and the minimum discomfort caused. Wherever possible the normal side is examined simultaneously. Only by such comparison can minor degrees of asymmetry be detected. Swellings situated in the floor of the mouth or in the cheek are felt bimanually with one hand placed inside, and one outside, the mouth. Both positive and negative findings are written down as later one may wish to check that at the first visit no abnormality was found in certain structures.
Systematic Procedure for Examination of the Oro-Facial Tissues
Extraoral Examination
This commences with a general inspection and palpation of the face, including the mandible, maxillary and malar bones, noting the presence of any abnormality, such as asymmetry or paralysis of the facial muscles. The eyes, their movements and pupil reactions are observed together with any difficulty in breathing.
The Temporomandibular Joints
(See also Chapter 17)
With the surgeon standing behind the patient, the site of the condyles are identified by palpation while the patient opens and closes their mouth. The joints are examined for tenderness and clicking or crepitus on opening and closing. The range of opening and left and right lateral excursion are checked and abnormalities noted.
The Muscles of Mastication
The muscles of mastication are palpated for tenderness. From extraoral, principally this means masseter and temporalis muscles, although medial pterygoid insertion can be palpated at the lower border.
The Maxillary Sinuses
In disease these may give rise to swellings, redness and tenderness over the cheek and canine fossa, nasal discharge and fistulae into the mouth, often through a tooth socket.
The Lymph Nodes
The operator stands behind the patient, who flexes their head forward to relax the neck muscles. Enlarged submental and submandibular nodes can be felt with the fingertips by placing these below the lower border of the mandible and rolling the nodes outwards. The upper deep cervical group can be found by identifying the anterior border of the sternocleidomastoid muscles at the mastoid process and rolling the skin and subcutaneous tissues between fingers and thumb. Working down this muscle to the clavicle and then ascending the neck to palpate the trachea and hyoid regions, the nodes may be felt against other structures such as muscles and underlying bones. With practice, tenderness, consistency and degrees of mobility will be recognised.
The Lips
These are inspected for lesions such as fissuring at the angles of the mouth, or ulceration.
The Cranial Nerves
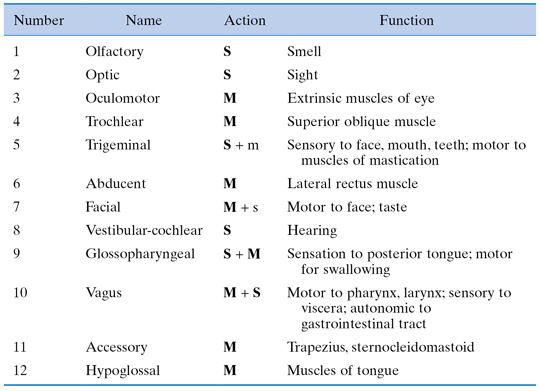
In some circumstances examination of all the cranial nerves is undertaken as part of the general examination. In particular this will be when neurological defects are noted and the possibility of intracranial lesions is suspected. The orofacial region encompasses the activity of the majority of the cranial nerves and a degree of familiarity with their action and testing is to be encouraged (Table 1.1). Facial trauma is often implicated in damage of the cranial nerves either intracranially or more peripherally, and even the most superficial dental examination will test branches of the 5th, 7th and 12th cranial nerve.
Table 1.1 Cranial nerves. The cranial nerves are listed with their area of activity in which testing must take place. The principal actions are indicated; S = sensory, M = motor (bold indicates main action of nerve, lower case indicates lesser action of nerve)
Intraoral Examination
Mirror Examination
An initial mirror examination of all the structures visible in the mouth, both soft tissues and hard, should be undertaken first to give a clear survey of the general state of the mouth.
The Mucous Membranes
The cheeks, lips, palate and floor of the mouth are examined for colour, texture and presence of swelling or ulceration. Comparison of both sides by palpation is essential to discover any abnormality.
The Tongue
Movements, both intrinsic and extrinsic, are tested, as limitation is an important clinical sign in inflammation and early neoplasia. The dorsum is best seen by protruding the tongue over dental gauze with which it can be grasped, drawn forward and, with the aid of a mouth mirror, examined over its length for fissures, ulcers, etc.
The Tonsils
These are seen by depressing the tongue with a spatula and asking the patient to say ‘Ah’.
The Pharynx
Again the tongue is depressed, the patient asked to say ‘Ah’. In good light, a small, warm mirror is passed over the dorsum of the tongue, past the uvula, and rotated to show the naso- and oropharynx. This can be demanding both for the surgeon and the patient, particularly those with a pronounced gag reflex.
The Salivary Glands
The examination of these is described in Chapter 16.
The Periodontal Tissues
The colour and texture of the gingivae are noted, and the standard of oral hygiene classified, including charting the presence of plaque and calculus. Recession, pocketing and hyperplasia of the gums are measured, and the mobility of the teeth assessed.
The Teeth
These are charted for caries and fillings with a mirror and probe. Loose teeth, crowns or fillings are noted.
Edentulous Ridges
These are examined for the form of the ridge, retained roots and soft tissue or bony abnormalities. Dentures worn should be inspected in situ before being removed to examine the underlying tissues
The Occlusion
This is best analysed by taking study models and mounting them on an anatomical articulator and is usual only for assessment of orthognathic cases. However, the occlusal function of natural teeth, bridges and dentures should be assessed at the same time as the teeth are charted.
Presenting Lesion
This is the examination of the lesion for which the patient has sought treatment. It may have been included in the general examination mentioned above, but frequently there is a swelling, ulcer, fistula or other disease that requires special attention, the details of which are best recorded under one heading easily referred to throughout treatment.
It is important in examining such pathological entities to determine their site, size, shape, colour, the character of their margins and whether they are single or multiple. Tenderness, discharge and lymphatic involvement are also important. Swellings should be palpated to determine whether they are mobile or fixed to the skin or to the underlying tissues. They may be either fluctuant or solid. Solid swellings may be very hard (like bone) or firm (like contracted muscle), soft (like relaxed muscle) or very soft (like fat). Induration is a firmness particularly associated with neoplastic lesions. Where a collection of fluid is suspected, fluctuation is elicited by placing two fingers of one hand on each side of the swelling and pressing centrally with a finger of the other hand. Where the lesion is fluid a thrill will be felt. This must be elicited in two directions at right angles, as muscle fluctuates in the longitudinal but not the transverse plane. All pulsatile swellings must be checked to establish whether the pulsation is true or transmitted from an underlying artery.
Special Investigation
The history taken and the examination of the patient having been completed, a differential or provisional diagnosis should be made. This should attempt to establish the disease process and relate it to the tissue involved. It is always useful to consider the main pathological categories (Table 1.2), rejecting those that do not fit the presenting situation. Similarly, the tissues in the area from which the lesion could arise should be identified. In this way a sensible argument may be sustained to support a definitive or differential diagnosis. Special investigations may be necessary to differentiate between these or to confirm a clinical finding. These are not indicated for every patient; indeed, their cost and the delay involved in completing them make it necessary to limit their use. Such investigations are an aid to diagnosis and may also be required for treatment planning. It is convenient to divide the more usual procedures into the four main categories shown in Box 1.1.
Box 1.1 Special Investigations Commonly Used in Oral Surgery
Local dental investigations
A Performed in the surgery
(1) Percussion of teeth for apical tenderness
(2) Vitality tests on teeth
(a) Thermal
(b) Electrical
(3) Radiography
(4) Diagnostic injections of local anaesthetic solutions in facial pain
(5) Study models for studying the occlusion
(6) Photography as a comparative record
B Requiring special facilities
(1) Bacteriological investigations, including sensitivity tests
(2) Aspiration of cystic cavities
(3) Biopsy of tissue
General investigations
A Performed in the surgery
(1) Temperature of body
(2) Pulse rate
(3) Blood pressure
(4) Respiration rate
(5) Cranial nerve testing (see Table 1.1)
B Requiring special facilities
(1) Urinalysis
Physical examination for colour, specific gravity
Chemical tests for sugar, acetone, albumen, chlorides, blood
Microscopic examination for cells, bacteria, blood
Bacteriological culture
(2) Blood investigations
Haemoglobin estimation
Red cell, white cell and platelet count
C-reactive protein (CRP)
Bleeding and clotting mechanisms
Grouping and cross-matching for transfusion
Blood chemistry and electrolytes – calcium, inorganic phosphorus, alkaline phosphatase, serum potassium, chloride, albumen, globulin, urea, glucose (see appendix)
Serology
(3) Radiographs, CT, MRI scans
(4) Electrocardiograph
(5) Tests for allergy
Table 1.2 The surgical sieve. The consideration of possible pathological processes and the tissues involved may be considered as a ‘surgical sieve’ into one of the holes of which the diagnosis may fit

The oral surgeon must be quite clear about how the necessary specimens are collected and, even more important, understand the clinical significance of the results. These have been dealt with extensively in other works and the methods of collection of certain specimens are described later in this text in the appropriate chapters.
Diagnosis
When the special investigations have been completed the surgeon should be able to make a final diagnosis and it is important that this be clearly stated in the notes. Diagnosis is not a matter of intuition but is a ‘computer’ exercise in which all the information is sorted and analysed. Sometimes it is impossible to reach a decision because of lack of information or knowledge, in which case the surgeon will need to consult textbooks or papers and may need to seek the opinion of a colleague.
Treatment Planning
Only when the diagnosis is established can a satisfactory treatment plan be made. This should be divided into preoperative, operative and postoperative care, each of which should be planned in a logical sequence, constantly bearing in mind that the ultimate aim is to cure the patient with the least risk and minimal inconvenience.
Further Reading
Douglas G, Nicol F, Robertson C (eds) (2009) Macleod’s Clinical Examination, 12th edn. Churchill Livingstone, Elsevier.
Meechan JG (2006) Minor Oral Surgery in Dental Practice. Quintessence, London.
Thomas J, Monaghan T (2007) Oxford Handbook of Clinical Examination and Practical Skills. Oxford University Press, Oxford.