Chapter 20 NURSING ASSESSMENT: visual and auditory systems
1. Outline the structures and functions of the visual and auditory systems.
2. Outline the physiological processes involved in normal vision and hearing.
3. Identify the significant subjective and objective assessment data related to the visual and auditory systems that should be obtained from the patient.
4. Discuss the appropriate techniques used in the physical assessment of the visual and auditory systems.
5. Differentiate normal from common abnormal findings of a physical assessment of the visual and auditory systems.
6. Outline age-related changes in the visual and auditory systems, and differences in assessment findings.
7. Explain the purpose, significance of results and nursing responsibilities related to diagnostic studies of the visual and auditory systems.
Structures and functions of the visual system
The visual system consists of the internal and external structures of the eyeball, the refractive media and the visual pathway. The internal structures are the iris, lens, ciliary body, choroid and retina. The external structures are the eyebrows, eyelids, eyelashes, lacrimal system, conjunctiva, cornea, sclera and extraocular muscles. The entire visual system is important for visual function. Light reflected from an object in the field of vision passes through the transparent structures of the eye and, in doing so, is refracted (bent) so that a clear image can fall on the retina. From the retina, the visual stimuli travel through the visual pathway to the occipital cortex, where they are perceived as an image.
STRUCTURES AND FUNCTIONS OF VISION
Eyeball
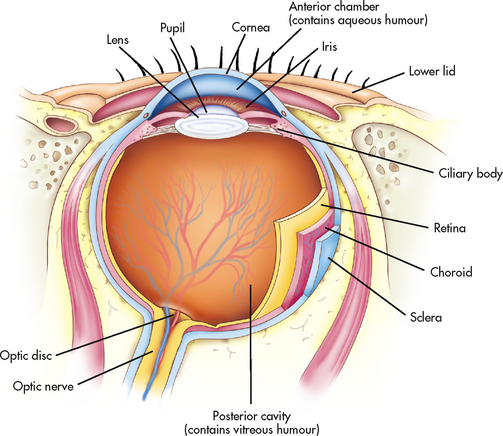
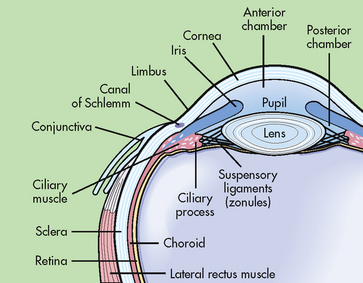
The eyeball, or globe, is composed of three layers (see Fig 20-1). The tough outer layer is composed of the sclera and the transparent cornea. The middle layer consists of the uveal tract (iris, choroid and ciliary body) and the innermost layer is the retina. The anterior chamber lies between the iris and the posterior surface of the cornea, whereas the posterior chamber lies between the anterior surface of the lens and the posterior surface of the iris. These chambers are filled with aqueous humour, which is secreted by the ciliary body (see Fig 20-2). The anatomical space between the posterior lens surface and the retina is filled with vitreous humour.
Refractive media
For light to reach the retina, it must pass through a number of structures: the cornea, aqueous humour, lens and vitreous humour. Each structure has a different density and plays a role in helping the focused image to fall on the retina. All of these structures must remain clear for light to reach the retina and stimulate the photoreceptor cells. The transparent cornea is the first structure through which light passes. It is responsible for the majority of light refraction that is necessary for clear vision.1
Aqueous humour, a clear watery fluid, fills the anterior and posterior chambers of the anterior cavity of the eye. Aqueous humour is produced by the ciliary process and passes through the pupil from the posterior chamber into the anterior chamber (see Fig 20-2). It drains through the trabecular meshwork located in the angle formed by the cornea and iris and into the canal of Schlemm. This circular canal conveys fluid into scleral veins, which enter the circulation of the body. The aqueous humour bathes and nourishes the lens and the endothelium of the cornea. Excess production or decreased outflow can elevate intraocular pressure above the normal 10–21 mmHg, a condition termed glaucoma.
The lens is a biconvex structure located behind the iris and supported in place by small fibres called zonules. The primary function of the lens is to bend light rays, allowing the rays to fall onto the retina. The lens shape is modified by the action of the ciliary zonules as part of accommodation, a process that allows the patient to focus on near objects, such as in reading. Anything altering the clarity of the lens affects light transmission.
Vitreous humour is located in the posterior cavity, which is the large area behind the lens and in front of the retina (see Fig 20-1). Light passing through the vitreous humour may be blocked by any non-transparent substance within the vitreous humour. The effect on vision varies, depending on the amount, type and location of the substance blocking the light. For example, in the case of haemorrhage into the vitreous humour, little light will reach the retina and vision will be severely compromised. However, cellular debris that accumulates from normal cell metabolism will cause only a relatively small shadow on the retina (‘floater’). The vitreous humour becomes more liquid with ageing.1
Refractive errors
Refraction is the ability of the eye to bend light rays so that they fall on the retina. In the normal eye, parallel light rays are focused through the lens into a sharp image on the retina. This condition is termed emmetropia and means that light is focused exactly on the retina, not in front of it or behind it. When the light does not focus properly, it is called a refractive error.
The individual with myopia can see near objects clearly (nearsightedness) but objects in the distance are blurred. This condition occurs when an image is focused in front of the retina, either because the eye is too long or because there is excessive refracting power (see Fig 20-3, A). A concave lens is used to correct the light refraction so that objects seen in the distance are focused clearly on the retina (see Fig 20-3, B).

Figure 20-3 Refraction disorders. Abnormal and corrected refraction observed in myopia (A and B) and hyperopia (C and D). FP, focal point.
The individual with hyperopia can see distant objects clearly (farsightedness) but close objects are blurred. This condition occurs when an image is focused behind the retina, either because the eye is too short or because there is inadequate refracting power (see Fig 20-3, C). A convex lens is used to correct the refraction (see Fig 20-3, D).
Astigmatism is caused by unevenness in the corneal or lenticular curvature, causing horizontal and vertical rays to be focused at two different points on the retina, which results in visual distortion. It can be myopic or hyperopic in nature in relation to where the image falls.
Presbyopia is a form of hyperopia, or farsightedness, that occurs as a normal process of ageing, usually at about 40 years of age. As the lens ages and becomes less elastic, it loses refractive power, and the eye can no longer accommodate for near vision. As with hyperopia, convex lenses are used to correct the light refraction so that the presbyopic individual can see clearly to read and accomplish other near-vision tasks.
Visual pathways
Once the image travels through the refractive media, it is focused on the retina, inverted and reversed left to right (see Fig 20-4). For example, if the visualised object is in the upper part of the left temporal visual field, it will be focused in the lower part of the nasal retina, upside down and as a mirror image. From the retina, the impulses travel through the optic nerve to the optic chiasm, where the nasal fibres of each eye cross over to the other side. Fibres from the left field of both eyes form the left optic tract and travel to the left occipital cortex. The fibres from the right field of both eyes form the right optic tract and travel to the right occipital cortex. This arrangement of the nerve fibres in the visual pathways allows determination of the anatomical location of abnormalities in those nerve fibres by interpretation of the specific visual field defect (see Fig 20-4).
EXTERNAL STRUCTURES AND FUNCTIONS
Eyebrows, eyelids and eyelashes
The eyebrows, eyelids and eyelashes serve an important role in protecting the eye by providing a physical barrier to dust and foreign particles. The eye is further protected by the surrounding bony orbit and by fat pads located below and behind the globe, or eyeball.
The upper and lower eyelids join at the medial and lateral canthi. The upper eyelid blinks spontaneously approximately 15 times a minute. Blinking distributes tears over the anterior surface of the eyeball and helps control the amount of light entering the visual pathway.
The eyelids open and close through the action of muscles innervated by cranial nerve (CN) VII, which is the facial nerve. Muscular action also helps hold the eyelids against the eyeball. Sebaceous glands, located in the eyelids, help form the lipid layer of the tear film.
Conjunctiva
The conjunctiva is a transparent mucous membrane that covers the inner surfaces of the eyelids (the palpebral conjunctiva) and also extends over the sclera (bulbar conjunctiva), forming a ‘pocket’ under each eyelid. This structure takes on the pink colour of the underlying tissue. The bulbar conjunctiva terminates at the corneal–scleral limbus and contains tiny blood vessels, which are most visible in the periphery. Glands in the conjunctiva secrete mucus and tears.
Sclera
The sclera is composed of collagen fibres meshed together to form an opaque structure commonly referred to as the white of the eye. It makes up the posterior five-sixths of the external eye and encircles the globe to join the cornea at the limbus. The sclera forms a tough shell that helps protect the intraocular structures.
Cornea
The transparent and avascular cornea makes up the anterior one-sixth of the globe and allows light to enter the eye (see Fig 20-1). The curved cornea refracts (bends) incoming light rays to help focus them on the retina. It is innervated by the trigeminal nerve (CN V).
The cornea consists of five layers: the epithelium, Bowman’s layer, the stroma, Descemet’s membrane and the endothelium. The epithelium consists of a layer of cells that helps protect the eye by serving as a barrier to fluid loss and to the entry of pathogens. The stroma consists of collagen fibrils separated by the ground substance, which has a unique ability to hold water. The stroma is relatively free of water so as to maintain transparency.
The avascular cornea obtains oxygen primarily through absorption from the tear film layer that bathes the epithelium. A small amount of oxygen is obtained from the aqueous humour through the endothelial layer, which is also responsible for transporting other nutrients into the corneal tissues.
Lacrimal apparatus
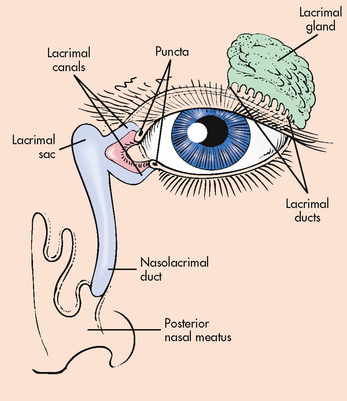
The lacrimal system consists of the lacrimal gland and ducts, lacrimal canals and puncta, lacrimal sac and nasolacrimal duct. In addition to the lacrimal gland, other glands provide secretions to make up the mucous, aqueous and lipid layers of the tear film that covers the anterior surface of the globe. The tear film moistens the eye and provides oxygen to the cornea. Lid and globe movements are both involved in spreading tears over the anterior surface of the eye. The tears are drained from the eye through the upper and lower puncta, then through the lacrimal sac and finally through the nasolacrimal duct into the nose (see Fig 20-5).
Extraocular muscles
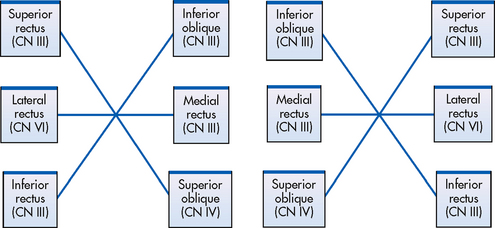
Each eye is moved by three pairs of extraocular muscles: the superior and inferior rectus muscles, the medial and lateral rectus muscles, and the superior and inferior oblique muscles (see Fig 20-6). Neuromuscular coordination produces simultaneous movement of the eyes in the same direction (conjugate movement).
INTERNAL STRUCTURES AND FUNCTIONS
Iris
The iris provides the colour of the eye. This structure has a small round opening in its centre, the pupil, which allows light to enter the eye. The pupil constricts via action of the iris sphincter muscle (innervated by CN III) and dilates via action of the iris dilator muscle (innervated by CN V) to control the amount of light that enters the eye. The constrictor muscle of the iris is stimulated by light falling on the retina and by accommodation. The autonomic nervous system also affects pupil size. Sympathetic stimulation results in contraction of the radial muscle and dilation of the pupil. Parasympathetic stimulation results in contraction of the circular muscle and constriction of the pupil.
Crystalline lens
The crystalline lens is a biconvex, avascular, transparent structure located behind the iris. It is supported by the anterior and posterior ciliary zonules. The lens is composed of thick gelatinous material enclosed in a clear capsule. The primary function of the lens is to bend light rays so that they fall onto the retina. Accommodation occurs when the eye focuses on a near object and is facilitated by contraction of the ciliary body, which changes the shape of the lens.
Ciliary body
The ciliary body consists of: the ciliary muscles, which surround the lens and lie parallel to the sclera; the ciliary zonules, which attach to the lens capsule; and the ciliary processes, which constitute the terminal portion of the ciliary body. The ciliary processes lie behind the peripheral part of the iris and secrete aqueous humour.
Choroid
The choroid is a highly vascular structure that serves to nourish the ciliary body, the iris and the outer portion of the retina. It lies inside and parallel to the sclera and extends from the area where the optic nerve enters the eye to the ciliary body (see Fig 20-1).
Retina
The retina is the innermost layer of the eye that extends and forms the optic nerve. Neurons make up the major portion of the retina. Therefore, retinal cells are unable to regenerate if destroyed. The retina lines the inside of the eyeball, extending from the area of the optic nerve to the ciliary body (see Fig 20-1). It is responsible for converting images into a form the brain can understand and process as vision. The retina is composed of two types of photoreceptor cells: rods and cones. Rods are stimulated in dim or darkened environments, and cones are receptive to colours in bright environments. The centre of the retina is the fovea centralis, a pinpoint depression composed only of densely packed cones. This area of the retina provides the sharpest visual acuity.2 Surrounding the fovea is the macula, an area less than 1 mm2, which has a high concentration of cones and is relatively free of blood vessels. Nourishment to the macula comes from two sources: the choroid and the underlying pigment epithelium, which is the deepest layer of the retina.
With the exception of the macula, the retina is nourished by retinal arterioles and veins. This blood supply enters the eye through the optic disc, which is located nasally from the macula. The optic disc is the area where the optic nerve (CN II) exits the eyeball. Within the disc is the physiological cup, a depression that can be visualised through the pupil with an ophthalmoscope. The retinal veins and arteries can also be visualised in this way and can provide information about the vascular system in general.
Gerontological considerations: effects of ageing on the visual system
Every structure of the visual system is subject to changes as the individual ages. Even though many of these changes are relatively benign, others may result in severely compromised visual acuity in the older adult. The psychosocial impact of poor vision or blindness can be highly significant. Age-related changes in the visual system and differences in assessment findings are presented in Table 20-1.
Assessment of the visual system
Assessment of the visual system may be as simple as determining a patient’s visual acuity or as complex as collecting complete subjective and objective data pertinent to the visual system. To do an appropriate ophthalmic evaluation, the nurse must determine which parts of the data collection are important for each patient. In order to do this appropriately the nurse needs to ask patients about any general problems they are having, including the signs and symptoms, and observe the outside of the eyelids and eyeball—is there swelling (oedema), redness (erythema), cuts, bruising (lacerations or lesions)? Assessment also includes asking patients about any specific problems with vision (e.g. double vision, blurred eyesight, flashes of light, small moving objects in the vision [floaters] or fuzzy lights around objects [haloes]).
SUBJECTIVE DATA
Important health information
Past health history
Information about the patient’s past health history should include both ocular and non-ocular history. The nurse should ask the patient specifically about systemic diseases, such as diabetes, hypertension, cancer, rheumatoid arthritis, syphilis and other sexually transmitted infections, acquired immunodeficiency syndrome, muscular dystrophy, myasthenia gravis, multiple sclerosis, inflammatory bowel disease and hypothyroidism or hyperthyroidism, because many of these diseases have ocular manifestations. It is particularly important to determine whether the patient has any history of cardiac or pulmonary disease because β-adrenergic blockers are often used to treat glaucoma but these medications can slow heart rate, decrease blood pressure and exacerbate asthma or chronic obstructive pulmonary disease.3
A history of tests for visual acuity should be obtained, including the date of the last examination and any change in glasses or contact lenses. The nurse should specifically ask about a history of strabismus, amblyopia, cataracts, retinal detachment, refractive surgery or glaucoma. Any trauma to the eye, its treatment and sequelae should be noted.
The patient’s non-ocular history can be significant in assessing or treating the ophthalmic condition. Specifically, the nurse should ask the patient about previous surgeries or treatments related to the head, as well as about previous trauma to the head.
Medications
If the patient takes medication, the nurse should obtain a complete list, including over-the-counter medicines, eye drops and herbal or natural supplements or substances. Many patients do not think that over-the-counter drugs, eye drops and herbal agents are real medication and may not mention their use unless specifically questioned. However, many of these drugs have ocular effects. For example, many cold preparations contain a form of adrenaline that can dilate the pupils. The nurse should also note the use of any antihistamines or decongestants because these drugs can cause ocular dryness. The nurse should ask specifically whether the patient uses any prescription drugs such as corticosteroids, thyroid medications or agents such as oral hypoglycaemics and insulin to lower blood glucose levels. Corticosteroid preparations can contribute to the development of glaucoma or cataracts. It is especially important to determine whether the patient is taking any β-adrenergic blockers because these can be potentiated by the β-blockers used to treat glaucoma.
Each drug the patient uses should correspond with a disease or disorder described in the patient’s history. If a medication cannot be correlated with a disease or disorder, the patient needs to explain why the drug is used. Finally, the nurse should determine whether the patient has allergies to medications or other substances, as these may lead to conditions such as itching eyes, blurring of vision or watery eyes.
Surgery or other treatments
Previous surgical procedures related to the eye or brain should be noted. Brain surgery and the subsequent swelling can cause pressure on the optic nerve or tract, resulting in visual alterations. Any laser procedures to the eye should also be documented. The effect of any eye surgery or laser treatment on visual acuity is important information to obtain.
Functional health patterns
The ophthalmic patient may seek healthcare for a specific problem or for regular ophthalmic care. When the patient needs routine ophthalmic care, the nurse should focus the assessment of functional patterns on issues related to health promotion. When the patient has a recognised problem, the nurse should direct the assessment to identify those issues related to the patient’s specific problem.
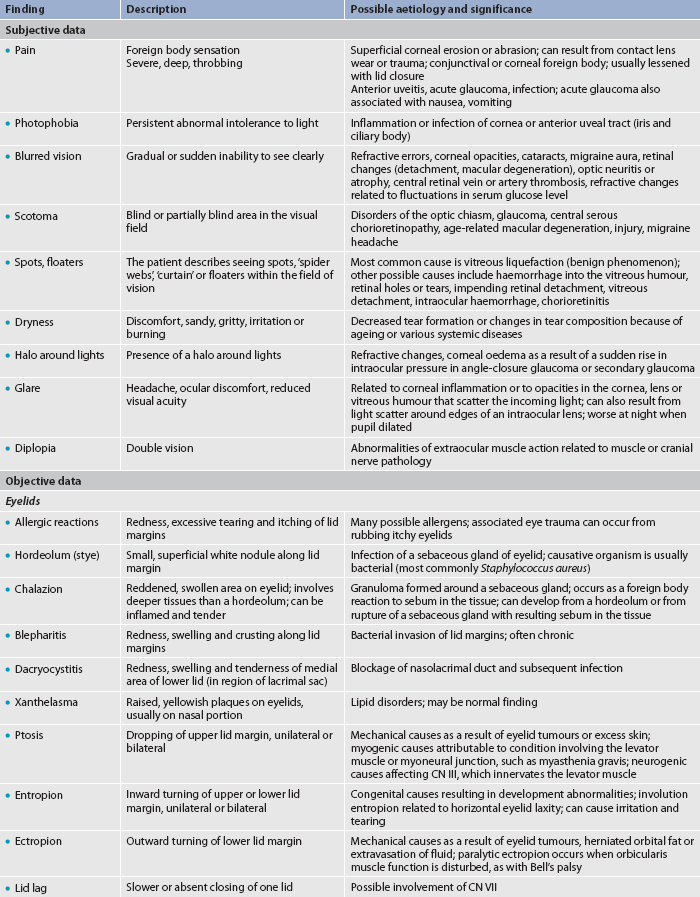
Ocular problems do not always affect the patient’s visual acuity. For example, patients with blepharitis or diabetic retinopathy may not have any visual deficit. The nurse should be aware that many conditions may cause vision loss. The focus of the functional health pattern assessment depends on the presence or absence of vision loss and whether the loss is permanent or temporary. Table 20-2 lists suggested health history questions to obtain data relating to the functional health patterns.

Health perception–health management pattern
A patient’s age is pertinent in considering cataracts, macular problems, glaucoma and other ophthalmic conditions. Men are more likely than women to have colour blindness.4 Indigenous Australians are more susceptible to trachoma, diabetes and its related complications,5 and older individuals are at higher risk of damage to the optic nerve from glaucoma.6
The ophthalmic patient in a clinic setting is often seeking routine eye care or a change in the prescription of eyewear. However, there can be some underlying concern that the patient may not mention or even recognise. The nurse should ask the patient, ‘Why are you here today?’
The patient’s visual health can affect activities at home or at work. It is important to know how the patient perceives the current health problem. As outlined in Table 20-2, the nurse can guide the patient in defining the current problem and how it affects the patient’s normal activities. The nurse should also assess the patient’s ability to accomplish all necessary self-care, especially any eye care related to the patient’s ophthalmic problem.
The patient’s ocular healthcare activities should also be assessed. The patient may not recognise the importance of eye safety practices, such as wearing protective eyewear during potentially hazardous activities or avoiding noxious fumes and other eye irritants. The nurse should question the patient about use of sunglasses in bright light, as prolonged exposure to ultraviolet light can affect the retina. Night driving habits and any problems encountered should be noted. Today, millions of people wear contact lenses but many do not care for them properly.7 The type of contact lenses used and the patient’s wearing and care habits may provide information for teaching.
Information about allergies should be obtained. As stated above, allergies often cause eye symptoms, such as itching, burning, watering, drainage and blurred vision.
Many chronic diseases and hereditary systemic diseases (e.g. sickle cell anaemia) can significantly affect ocular health. For example, vascular conditions such as hypertension are recognised as important predisposing factors to diseases such as glaucoma. In addition, many refractive errors and other eye problems are hereditary. For these reasons, the nurse should obtain a careful family history of both ocular and non-ocular diseases. Specifically, the nurse should ask whether the patient has a family history of diseases such as atherosclerosis, diabetes mellitus, thyroid disease, hypertension, arthritis or cancer. The nurse should also determine whether the patient has a family history of ocular problems such as cataracts, tumours, glaucoma, refractive errors (especially myopia and hyperopia) or retinal degenerative conditions (e.g. macular degeneration, retinal detachment, retinitis pigmentosa).
Nutritional–metabolic pattern
The patient’s intake of antioxidants (vitamins C and E) and trace minerals can be important to ocular health. Some patients with age-related macular degeneration may benefit from supplements of these vitamins and trace minerals.8
Elimination pattern
Straining to defecate (Valsalva manoeuvre) can raise the intraocular pressure. Although there is some evidence that elevation of the intraocular pressure through normal activities is not detrimental to the surgical incision made during eye surgery, many surgeons do not want the patient to strain. The nurse should assess the patient’s usual pattern of elimination and determine whether there is the potential for constipation in the patient who has had ophthalmic surgical procedures.
Activity–exercise pattern
A patient’s usual level of activity or exercise may be affected by reduced vision, by symptoms accompanying an ocular problem or by activity restrictions following a surgical procedure. For example, a patient with hyphaema (intraocular bleeding) may be on bed rest or have severely restricted activity. The diabetic patient with lower limb prostheses will have additional ambulation difficulties if diabetic retinopathy with vision loss is present.
The nurse should inquire about leisure activities during which the patient may incur an ocular injury. For example, gardening, woodworking and other craft activities can result in corneal or conjunctival foreign bodies or even penetrating injuries to the globe. Injuries to the globe or bony orbit can also occur after blows to the head or eye during sports activities such as squash, football, boxing and tennis. Cross-country skiers and bush walkers may develop corneal fungal ulcers after an abrasion caused by low-hanging tree limbs. Other leisure activities, such as embroidery, fly tying or bird watching, may have high-level visual demands and produce eye strain.
Sleep–rest pattern
In the otherwise healthy person, lack of sleep may cause ocular irritation, especially in the patient who wears contact lenses. Normal sleep patterns may be disrupted in the patient with painful eye problems such as corneal abrasions. The patient with alkali burns of the eye requires continuous irrigation of the ocular surface until the pH of the conjunctival sac returns to normal levels.9 Normal sleep will be disrupted during this time.
Cognitive–perceptual pattern
The entire assessment of the ophthalmic patient focuses on the sense of sight but it is important not to overlook other cognitive or perceptual problems. For example, the functional ability of a patient with a visual deficit will be further compromised if the patient also has hearing problems. Patients who cannot see to read may have increased difficulty in following postoperative instructions if they also have trouble hearing or remembering verbal instructions. Patients who do not understand or read English may require written or verbal instructions and information in their native language.
Eye pain is always an important symptom to assess. Corneal abrasions, iritis and acute glaucoma manifest with pain and are serious eye problems. Infections and foreign bodies can cause less severe eye discomfort but are also potentially serious. If eye pain is present, the patient should be questioned about treatment and response.
Self-perception–self-concept pattern
The loss of independence that can follow a partial or complete loss of vision, even if the condition is temporary, can have devastating effects on the patient’s self-concept. The nurse should carefully evaluate the potential effect of vision loss on the patient’s self-image. For instance, disabling glare from a cataract may prevent night-time driving or even limit daytime driving, resulting in a diminished self-image. In today’s highly mobile society, loss of ability to drive can represent a significant loss of independence and self-esteem. Also, patients with severe ptosis or other disfiguring ophthalmic conditions may be embarrassed by their appearance and suffer from a poor self-image.
Role–relationship pattern
The patient’s ability to maintain the necessary or desired roles and responsibilities in the home, work and social environments can be negatively affected by ocular problems. For example, macular degeneration may decrease the patient’s visual acuity to a level that is inadequate to function at work. Many occupations place workers in conditions in which eye injury may occur. For example, factory workers may be at risk of flying metal debris. Information should be obtained about eye safety practices, such as the use of goggles or safety glasses. Workers can also be exposed to eye strain in the office from display screens, poor lighting and glare.
The patient with diabetes mellitus may not be able to see well enough to self-administer insulin. This patient may resent the dependence on a family member who takes over this function. Also, patients with exophthalmos (marked protrusion of eyeballs) may be embarrassed by their appearance and avoid usual social activities. The nurse should sensitively inquire whether the patient’s preferred roles and responsibilities have been affected by the ocular problem.
Sexuality–reproductive pattern
The inactivity that may be associated with low vision, blindness and certain eye problems and surgeries can negatively affect a patient’s sexuality. The patient with severe vision loss may develop such a poor self-image that the ability to be sexually intimate is lost. The nurse can assure the patient that low vision or blindness does not affect a person’s ability to be sexually expressive. For many sexually expressive acts, touch is more important than vision.
If a patient with low vision or blindness has a young family, assistance with child-rearing tasks may be necessary. The nurse should determine the need for and availability of help in this situation.
Coping–stress tolerance pattern
The patient with temporary or permanent visual problems will experience emotional stress. The nurse should assess the patient’s coping level, coping mechanisms and availability of social and personal support systems. The patient with permanent visual loss experiences the usual stages of grief after the loss. The nurse should assess the potential need for psychosocial counselling and eventual vocational rehabilitation.
Value–belief pattern
The nurse must be sensitive to the individual values and spiritual beliefs of each patient because patients often make decisions regarding ophthalmic care based on their values and beliefs. It can be difficult to understand why a patient refuses treatment that has potential benefit or wants treatment that may have limited potential benefit. The nurse should assess the patient’s value–belief pattern that serves as the basis for making those decisions.
OBJECTIVE DATA
Physical examination
Physical examination of the visual system includes inspecting the ocular structures and determining the status of their respective functions. Physiological functional assessment includes determining the patient’s visual acuity and ability to judge closeness and distance, assessing extraocular muscle function, evaluating the visual fields, observing pupil function and measuring the intraocular pressure. Assessment of ocular structures should include examining the ocular adnexa, external eye and internal structures. Some structures, such as the retina and blood vessels, must be visualised with the aid of ophthalmic observation equipment, such as the ophthalmoscope.
Assessment of the visual system may include all of the following components or it may be as brief as measuring the patient’s visual acuity. The nurse should assess what is appropriate and necessary for each patient. All of the following assessments are within the nurse’s scope of practice but some require special training. Normal physical assessment of the visual system is outlined in Box 20-1. Age-related visual changes and differences in assessment findings are listed in Table 20-1. Assessment techniques related to vision are summarised in Table 20-3 and common assessment abnormalities are listed in Table 20-4.
Initial observation
The initial observation of the patient can provide information that will help the nurse to focus the assessment. When first encountering the patient, the nurse may observe that the patient is dressed in clothing with unusual colour combinations. This may indicate a colour-vision deficit. The nurse may also note an unusual head position. The patient with diplopia may hold the head in a skewed position in an attempt to see a single image. The patient with a corneal abrasion or photophobia will cover the eyes with the hands to try to block out room light. The nurse can make a crude estimate of depth perception by extending a hand for the patient to shake.
During the initial observation, the nurse needs to ensure good lighting and, if necessary, use magnification. The nurse should also observe the overall facial and ophthalmic appearance of the patient. The eyes should be symmetrical and normally placed on the face. The globes should not have a bulging or sunken appearance. If the client has a red eye, a history of a foreign body in the eye or a sensation of grittiness in the eye, the upper eyelid may need to be everted for further examination. Eversion of the eyelid should never be done if there is any suggestion of a penetrating eye injury. The anterior chamber of the eye should be examined for the presence of blood (hyphaema). The nurse should check the size of both pupils (they should normally be round, regular and of equal size). Normally both pupils should constrict when light is shone onto the eye.
Assessing functional status
Visual acuity
The nurse should always record the patient’s visual acuity for medical and legal reasons. The patient’s visual acuity must be documented before the patient receives any care. This is usually achieved by using the Snellen chart. The Snellen chart consists of rows of capital letters, the letters of each row becoming smaller down the chart. The letter at the top is of a size that can be read by a person with normal vision at a distance of 6 m.
The patient sits or stands 6 m from the Snellen chart with the usual correction (glasses or contact lenses) left in place unless they are used solely for reading. The nurse asks the patient to cover the left eye with a card and read the smallest line that the patient can read comfortably. If the patient reads that line with two or fewer errors, the nurse instructs the patient to read the next lower line. When recording the results of eye testing, the first number is always the testing distance (6 m) and the last number (denominator) is the smallest line that the client can read from the chart (the lines are numbered). If the client has a problem with one eye, the better eye is tested first. The nurse records the visual acuity using the ophthalmic abbreviations for right eye (oculus dexter [OD]), left eye (oculus sinister [OS]) and each eye (oculus uterque [OU]). For example, for the patient who reads to the 9 m line with the right eye, the nurse records the acuity as 6/9 OD. A visual acuity of 6/9 means that from 6 m away, the patient can read the same letters that the person with normal vision can read from 9 m away. The nurse then asks the patient to cover the other eye with the card and the process is repeated. Legal blindness is defined as the best-corrected vision in the better eye of 6/60 or less.9
If the patient cannot read letters (e.g. is illiterate), an eye chart with pictures or numbers can be used, such as an E chart. An E chart consists of rows containing the capital letter ‘E’, which faces a variety of directions and is sized differently depending on the row in which it is placed. The examiner asks the patient to show with the fingertips (of the hand that is not covering the eye being tested) which way the legs of the E are pointing. An alternative chart for children has rows depicting different animals whose sizes vary according to the line in which they are placed. The child is asked to identify the various animals in the same way as an adult is asked to read the letters on the Snellen chart.
To evaluate visual acuity when the patient is unable to see the 6/60 letter, the nurse should reduce the patient’s distance to 3 m, 2 m then 1 m from the Snellen chart. If the patient’s visual acuity is less than 6/9 then a pinhole (PH) should be used. This enables light rays to reach the retina. If the patient has an uncorrected refractive error (this may occur, for example, if the patient has been wearing the same pair of glasses for many years without correction), then their sight may be improved. If the patient is unable to read the 6/60 letter from the reduced distance, the nurse can hold up a number of fingers 0.9–1.5 m in front of the patient and ask the patient to count them. If the patient is unable to count the fingers, the nurse holds up a different number of fingers at successively closer distances up to 30 cm and again asks the patient to count them. The nurse then tests the opposite eye in the same manner and records the acuity of each eye. If the patient can count the number of fingers at 0.6 m the nurse records the acuity as FC or CF (finger counting or counts fingers) at 0.6 m. If the patient cannot count fingers, the nurse asks the patient to indicate if moving the hand is seen in front of the face. This level of visual acuity is HM (hand motion). LP (light projection) is the term for a patient’s visual acuity if only light can be seen.
If the patient has a complaint of visual problems with near vision, and for all patients 40 years of age or older, the nurse tests the near visual acuity. The patient is instructed to hold a Jaeger card 35 cm from the eyes. The nurse covers the patient’s left eye with the occluder, asks the patient to read paragraphs with successively smaller lines of print from the card, and records the visual acuity that corresponds to the smallest line of print that the patient can read comfortably. The procedure is repeated while covering the right eye. A near acuity of Jaeger1 (J1) indicates that the patient can read 4-point type at 35 cm and is considered normal. A near acuity of J10 indicates that the smallest print the patient can read at 35 cm is 14-point type and is moderately impaired. Normal newspaper print is 8-point type.
If the nurse must assess visual acuity without access to an eye chart, an accurate assessment is still possible. Examples of other stimuli acceptable for use include newsprint or the label on a container. The examiner records the acuity as ‘reads newspaper headline at … cm’.
Extraocular muscle functions
Extraocular muscle function can be tested by observing the movement of the eyes in six specific directions. This can be done by holding a light or other object 15 cm in front of the patient’s face. While moving the object in several directions the nurse asks the patient to follow it with their eyes, without moving their head.
Pupil function
Pupil function is determined by inspecting the pupils and their reactions to light. The pupils should be equal in size and round and should react briskly to light. In a small percentage of the population, the pupils are unequal in size (anisocoria). The pupils should react to light both directly (the pupil constricts when a light shines into the same eye) and consensually (the pupil constricts when a light shines into the opposite eye). The nurse should also check the accommodative response by having the patient fixate on an object 60–90 cm away and then bringing the object closer to the patient until the patient is fixating on the object at 15–20 cm away. The pupils should constrict when the patient tries to focus on the near object.
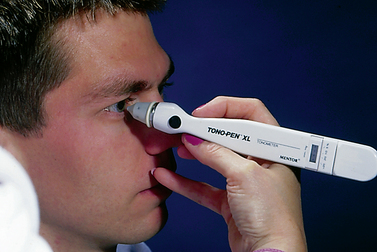
Intraocular pressure
Intraocular pressure can be measured by a variety of methods, including the Tono-pen (see Fig 20-7). The Tono-pen is simple to use and very accurate. The surface of the anaesthetised cornea is touched lightly several times with the covered end of the probe. The instrument records several readings and provides a mean measurement on a digital light-emitting diode (LED) screen located on the front surface. Normal intraocular pressure ranges from 10 to 21 mmHg.
Assessing structures
The structures that constitute the visual system are assessed primarily by inspection. The visual system is unique because the nurse can directly inspect not only the external structures but also many of the internal structures. The iris, lens, vitreous humour, retina and optic nerve can all be visualised directly through the clear cornea and pupil opening.
This direct inspection requires the examiner to use special observation equipment, such as the slit lamp microscope and the ophthalmoscope. This equipment permits examination of the conjunctiva, sclera, cornea, anterior chamber, iris, lens, vitreous humour and retina under magnification. With the slit lamp microscope, a narrow beam or slit of light is directed onto the eye to illuminate a small section brightly. The patient’s chin is positioned in a chin rest to stabilise the head. The ophthalmoscope is a hand-held instrument with a light source and magnifying lenses that is held close to the patient’s eye to visualise the posterior part of the eye. No pain or discomfort is associated with these examinations. As with other skills, using this equipment requires some special training and practice. However, special equipment provides the means for a thorough ophthalmic assessment that gives the nurse information not only about the ocular structures themselves but also about the patient’s systemic condition.
Eyebrows, eyelashes and eyelids
All structures should be present and symmetrical, and without deformities, redness or swelling. Eyelashes extend outwards from the lid margins. The eyelids are positioned symmetrically with the upper and lower eyelids approximately at the corneal–scleral limbus and the lid margins against the globe. In normal closing, the upper and lower eyelid margins just touch. The lacrimal puncta should be open and positioned properly against the globe, with no swelling or redness around the lower puncta, indicating lacrimal sac inflammation. If the sac is inflamed, pressure over the lacrimal sac may cause purulent material to ooze from the puncta. The nurse may need to look inside the upper eyelids for anything stuck to them (subtarsal foreign bodies and non-penetrating bodies) and for trachoma follicles or scarring.10,11
Conjunctiva and sclera
The nurse can easily examine the conjunctiva and sclera at the same time. To examine the palpebral conjunctiva, the nurse places a forefinger over the cheekbone and gently pulls down. This manoeuvre exposes the palpebral conjunctiva of the lower lid to assess colour (normally pale pink), texture (normally smooth) and the presence of lesions or foreign bodies. The bulbar conjunctiva covering the sclera is normally clear, with fine blood vessels visible. These blood vessels are more common in the periphery.
The sclera is normally white in Caucasian and Indigenous Australians, but it may take on a yellowish hue in older individuals because of lipid deposition. A pale blue cast caused by scleral thinning can also be normal in older adults and infants (who have naturally thinner scleras). The blue cast is actually the vascular choroid showing through. A slight yellow cast may be found in some dark-pigmented populations, such as Polynesians and Indigenous Australians. If the sclera is red, the fact must be recorded and the doctor needs to be notified.
Cornea
The cornea should be clear, transparent and shiny. The nurse can use either a hand-held torch, oblique light or slit lamp microscope to inspect the anterior chamber. The iris should appear flat and not bulging towards the cornea. The area between the cornea and the iris should be clear with no blood or purulent material visible in the anterior chamber. (If there is a defect, the light will be broken up and uneven.) Blood and purulent material have viscosities greater than that of aqueous humour and they will settle to the lower portion of the chamber, if present. It is also important to ask the patient whether they experience dryness of their eyes, as this can cause irritation and corneal damage if untreated. Dryness can be a side effect of tricyclic antidepressants, β-blockers and steroids, so it is important to assess in older people who are on such medications.
Iris
Both irides should be of similar colour and shape. However, a colour difference between the irides occurs normally in a small portion of the population. The iris should be inspected with the upper lid raised. Any area of missing iris will be evident because the absence of the coloured iris tissue leaves what appears to be a dark, abnormally shaped ‘pupil’. Round or notched areas of missing iris tissue are often the result of cataract or glaucoma surgery. The nurse should determine the cause of these areas and document the findings.
Retina and optic nerve
To assess these structures, the nurse uses an ophthalmoscope to magnify the ocular structures and bring them into crisp focus. Blood vessels in the vascular choroid are visible through the retinal tissues, as is the optic disc (where the optic nerve enters the back of the eye). The ability to view arteries, veins and the optic nerve directly in this manner is unique.
When using the ophthalmoscope, the nurse directs the beam of light obliquely into the patient’s pupil. The red reflex should be visible. This reflex results from the light reflecting off the pink colour of the retina. Any dense areas in the lens, such as a cataract, will decrease the red reflex. The reflex is followed inwards until the fundus, or back of the eye, comes into view. Both arterioles and veins can be seen. Arterioles are smaller, thinner and lighter red and reflect light better than veins. The nurse should examine the areas where arterioles and veins cross for nicking or narrowing. These changes are associated with diabetes mellitus and hypertension.
The nurse should then follow a blood vessel towards the optic nerve and examine the optic nerve and disc for size, colour and abnormalities. The disc is creamy yellow with distinct margins. A slight blurring of the nasal margin is common. A central depression in the disc, called the physiological cup, may be seen. This area is the exit site for the optic nerve. The cup should be less than half the diameter of the disc. The nurse should document the presence of any unusual rings or crescents surrounding the disc.
Normally, no haemorrhages or exudates are present in the fundus (retinal background). Careful inspection of the fundus can reveal the presence of retinal holes, tears, detachments or lesions. Small haemorrhages can be associated with diabetes mellitus or hypertension and can appear in various shapes, such as dots or flames. Finally, the nurse examines the macula for shape and appearance. This area of high reflectivity is devoid of any blood vessels.
The nurse can obtain important information about the vascular system and the central nervous system (CNS) through direct visualisation with an ophthalmoscope. Skilled use of this instrument requires practice.
Special assessment techniques
Colour vision
Testing the patient’s ability to distinguish colours can be an important part of the overall assessment because some occupations may require accurate colour discrimination. The Ishihara colour test determines the patient’s ability to distinguish a pattern of colour in a series of colour plates. Older adults have a loss of colour discrimination at the blue end of the colour spectrum and loss of sensitivity throughout the entire spectrum.
Stereopsis
Stereoscopic vision allows the patient to see objects in three dimensions (see Table 20-3). Any event that causes a patient to have monocular vision (e.g. enucleation, patching) results in the loss of stereoscopic vision. When stereopsis is not present, the individual’s ability to judge distances is impaired. Accurately judging the height of steps is also affected.12 This disability can have serious consequences if the patient trips over a step when walking or follows too closely behind another vehicle when driving.
Diagnostic studies of the visual system
Diagnostic studies provide important information for the nurse in monitoring the patient’s condition and planning appropriate interventions. These studies are considered objective data. Table 20-5 presents the most common basic diagnostic studies of the visual system.
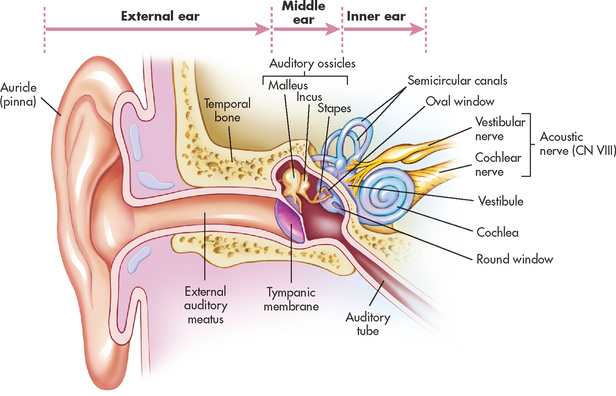
Structures and functions of the auditory system
The auditory system is composed of the peripheral auditory system and the central auditory system. The peripheral auditory system includes the structures of the ear itself—the external, middle and inner ear (see Fig 20-8)—and is concerned with the reception and perception of sound. The inner ear functions in hearing and balance. The central auditory system (the brain and its pathways) integrates and assigns meaning to what is heard.
EXTERNAL EAR
The external ear consists of the auricle, or pinna, and the external auditory canal. The auricle is composed of cartilage and connective tissue covered with epithelium, which also lines the external auditory canal (see Fig 20-8). The external auditory canal is a slightly S-shaped tube about 2.5 cm in length in the adult. The skin that lines the canal contains fine hairs and sebaceous (oil) and ceruminous (wax) glands. The oil and wax lubricate the ear canal, keep it free from debris and kill bacteria.13 Hair is present in the outer half of the canal. The inner half of the ear canal is highly sensitive. The function of the external ear and canal is to collect and transmit sound waves to the tympanic membrane (eardrum). This shiny, translucent, pearl-grey membrane is composed of skin, connective tissue and mucous membrane. It serves as a partition between the external auditory canal and the middle ear.
MIDDLE EAR
Mucous membrane lines the middle ear and is continuous from the nasal pharynx via the eustachian tube. The middle ear cavity is an air space located in the temporal bone. It contains three tiny bones: malleus, incus and stapes (called the ossicular chain). Vibrations of the tympanic membrane cause the ossicles to move and transmit sound waves to the oval window. This oval window vibration causes the fluid in the inner ear to move and stimulates the receptors of hearing. The round window, which is covered with mucous membrane, also opens into the inner ear and allows for dissipation of the fluid disturbances (round window reflex). The superior part of the middle ear is called the epitympanum, or the attic, and also communicates with air cells within the mastoid bone. The air cells are lined with the same mucous membrane as the middle ear.
The middle ear cavity is filled with air. Equalisation of atmospheric air pressure is accomplished by the eustachian tube opening during yawning or swallowing. Blockage of the tube can occur with allergies, nasopharyngeal infections and enlarged adenoids. The facial nerve (CN VII) traverses above the oval window of the middle ear. The thin, bony covering of the facial nerve can become damaged by chronic ear infection, skull fracture or trauma during ear surgery. Problems may result related to voluntary facial movements, eyelid closure and taste discrimination.
The external and middle portions of the ear function to conduct and amplify sound waves from the environment. This portion of sound conduction is termed air conduction. Problems in these two parts of the ear may cause conductive hearing loss, resulting in an alteration in the patient’s perception or sensitivity to sounds.
INNER EAR
The middle ear interfaces with the inner ear where the stapes meets the oval window. The inner ear is composed of the bony labyrinth and the membranous labyrinth and contains the functional organs for hearing and balance.
The receptor organ for hearing is the cochlea, a coiled structure. It contains the organ of Corti, whose tiny hair cells respond to stimulation of selected portions of the basilar membrane according to pitch. This mechanical stimulus is converted into an electrochemical impulse and then transmitted by the acoustic portion of the vestibulocochlear nerve (CN VIII) to the brain to be processed and interpreted as sound.
Three semicircular canals and two sacs, the utricle and saccule, make up the organ of balance. These structures make up the membranous labyrinth, which is housed in the bony labyrinth. The membranous labyrinth is filled with endolymphatic fluid and the bony labyrinth is filled with perilymphatic fluid. The perilymphatic fluid cushions these two sensitive organs and communicates with the brain and the subarachnoid spaces of the brain. The nervous stimuli are communicated by the vestibular portion of CN VIII. Debris or excessive pressure within the lymphatic fluid can cause disorders including vertigo.
Gerontological considerations: effects of ageing on the auditory system
Age-related changes of the auditory system can result in impaired hearing. Presbycusis, or hearing loss due to ageing, can result from ageing or insults from a variety of sources. Noise exposure, vascular or systemic diseases, poor or inadequate nutrition, ototoxic drugs and pollution during the life span can damage the delicate hair cells of the organ of Corti or atrophy lymph-producing cells. Sound transmission is diminished by calcification of the ossicles. Dry cerumen in the external canal can also interfere with the transmission of sound.
Tinnitus, or ringing in the ears, may accompany the hearing loss that results from the ageing process. Hearing loss, especially in the older adult, can have serious implications for quality of life, including progressive physical and psychosocial dysfunction.14 As the average life span increases, the number of people with hearing loss will also increase. Early identification of problems will ensure a more active and healthy patient population in their seventh and eighth decades.
Age-related changes in the auditory system and differences in assessment findings are presented in Table 20-6.
Pathology of the inner ear or along the nerve pathway from the inner ear to the brain can result in sensorineural hearing loss. This may result in an alteration of the patient’s perception or sensitivity to high-pitched tones. These may be experienced as a decrease in intensity, muffling of the intensity (increased sensitivity to loud sounds) or decrease in the ability to understand spoken words (distortion). Problems within the central auditory system from the cochlear nuclei to the cortex cause central hearing loss. This type of hearing loss causes difficulty in understanding the meaning of the words heard. (Types of hearing loss are discussed in Ch 21.)
Transmission of sound
Sound waves are conducted by air and picked up by the auricles and auditory canal. The tympanic membrane is struck by the sound waves, which cause it to vibrate. The central area of the tympanic membrane is connected to the malleus, which also starts to vibrate, transmitting the vibration to the incus and then the stapes. As the stapes moves back and forth, it pushes the membrane of the oval window in and out. Movement of the oval window produces waves in the perilymph. Once sound has been transmitted to the liquid medium of the inner ear, the vibration is picked up by the tiny sensory hair cells of the cochlea, which initiate nerve impulses. These impulses are carried by nerve fibres to the main branch of the acoustic portion of CN VIII and then to the brain.
Assessment of the auditory system
Assessment of the auditory system includes assessment of the vestibular (balance) system because the auditory and vestibular systems are so closely related. It is often difficult to separate symptoms from the two systems. The nurse must help the patient to describe symptoms and problems in order to differentiate the source of the problems. Health history questions to ask a patient with an auditory problem are listed in Table 20-7.
Problems with balance may present as nystagmus or vertigo. Nystagmus is abnormal eye movements that may be observed by others as twitching of the eyeball or described by the patient as a blurring of vision with head or eye movement. Vertigo is a sense that the person or objects around the person are moving or spinning and is usually stimulated by movement of the head. Dizziness is a sensation of being off-balance that occurs when standing or walking. It does not occur when lying down. Initially the nurse should try to categorise symptoms related to dizziness and vertigo and separate them from symptoms related to hearing loss or tinnitus. The symptoms can be combined later in the assessment to help make the diagnosis and plan for the patient.
SUBJECTIVE DATA
Important health information
Past health history
Many problems related to the ear are sequelae of childhood illnesses or result from problems of adjacent organs. Consequently, a careful assessment of past health problems is important. In many Indigenous communities in Australia there are high rates of otitis media, ranging from recurrent episodes to chronic otitis media, with the associated complications of hearing problems (and disruptive behaviours in school), and mastoiditis and cholesteroma. As a result of these possible complications, assessment for middle ear disease and hearing impairment should be a routine part of the primary care of children in rural and remote Australia.
The patient should be questioned about previous problems regarding the ears, especially problems experienced during childhood. The frequency of acute middle ear infections (otitis media), surgical procedures (e.g. myringotomy), perforations of the eardrum, drainage, complications and a history of mumps, measles or scarlet fever should be recorded. Congenital hearing loss can result from infectious diseases (rubella, influenza or syphilis), teratogenic medications or hypoxia in the first trimester of pregnancy. Since a safe and effective rubella vaccine was developed in 1969, reported cases of deafness due to rubella have dropped to 1%.15
Symptoms such as dizziness, tinnitus and hearing loss are recorded in the patient’s words. It may be difficult for the patient to describe the dizziness. However, it is important that patients describe the dizziness in detail using their own words. This careful description could help differentiate the cause.
Medications
Information about present or past medications that are ototoxic (cause damage to CN VIII) and can produce hearing loss, tinnitus and vertigo should be obtained. Aminoglycosides, other antibiotics, salicylates, antimalarial agents, chemotherapeutic drugs, diuretics and non-steroidal anti-inflammatory drugs are groups of drugs that are potentially ototoxic.16 Careful monitoring is essential. Many drugs produce hearing loss that may be reversible if treatment is stopped. Assessing the amount and frequency of aspirin use is also important because tinnitus can result from high aspirin intake.
Surgery or other treatments
Information regarding previous hospitalisations for ear surgery, as well as for tonsillectomy and adenoidectomy, should be obtained. A history of a head injury should also be documented because a head injury may result in hearing loss. Use of and satisfaction with a hearing aid should be documented. Problems with impacted cerumen should also be noted.
Functional health patterns
Hearing and balance problems can affect all aspects of a person’s life. To assess the impact of hearing loss, health history questions can be asked based on a functional health pattern approach (see Table 20-7).
Health perception–health management pattern
The nurse should note the onset of hearing loss, whether sudden or gradual. It should be recorded who noted the onset, whether it be the patient, family or significant others. Gradual hearing losses are most often noted by those who communicate with the patient. Sudden losses and those exacerbated by some other condition are most often reported by the patient.
Information about allergies is important because they can cause the eustachian tube to become oedematous and prevent aeration of the middle ear. Information regarding family members with hearing loss and type of hearing loss is important. Some congenital hearing loss is hereditary. The age of onset of presbycusis also follows a familial pattern.
The patient should be questioned about personal practices used to preserve hearing. The use of protective ear covers or earplugs is good practice for persons in high-noise environments. If the patient is a swimmer, the frequency and duration of swimming and use of ear protection should be documented. It is also important to note the type of water (pool, river or ocean) in which the swimming takes place.
Nutritional–metabolic pattern
Both alcohol and sodium affect the amount of endolymph in the inner ear system. Patients with Ménière’s disease generally notice some improvement in their symptoms with alcohol restriction and a low-sodium diet. Improvements and exacerbations associated with food intake should be noted. The patient should also be questioned about any ear pain or discomfort associated with chewing or swallowing that might decrease nutritional intake. This situation is often associated with a problem in the middle ear.
Assessment of clenching or grinding of the teeth helps differentiate problems of the ear from referred pain of the temporomandibular joint. The nurse should ask about dental problems and dentures. There is a higher incidence of hearing loss in individuals who wear dentures.17
Elimination pattern
Elimination patterns and their association with ear problems are mainly of interest in patients with a perilymph fistula or who are immediately postoperative. If the patient experiences frequent constipation or straining with bowel or bladder elimination, this may interfere with healing of a perilymph fistula or its repair. The post-stapedectomy patient especially needs to prevent the increased intracranial (and consequent inner ear) pressure associated with straining during bowel movements. Stool softeners may be ordered postoperatively for patients who report chronic problems with constipation.
Activity–exercise pattern
Activity–exercise review is most important when assessing the patient with vestibular problems. The patient should be questioned specifically about activities that relieve or exacerbate symptoms of dizziness or cause nausea or vomiting. If dizziness is a problem, the patient should be questioned about the onset, duration, frequency and precipitating factors of this symptom. Patients with chronic vertigo syndrome (benign paroxysmal positional vertigo [BPPV]) will note that the symptoms improve throughout the day as adjustment to the visual and positional input from the environment occurs. In contrast, patients with Ménière’s syndrome demonstrate increasing inability to compensate for environmental input as the day progresses. Symptoms are experienced particularly in the evening. The nurse and the patient should identify a list of activities and exercises that affect dizziness and vertigo. The patient may use habituation exercises to help control the symptoms. Habituation exercises involve frequent repetition of an activity that causes the symptoms until the body adjusts and the activity is no longer a problem.
Sleep–rest pattern
The patient with chronic tinnitus should be questioned about sleep problems. Tinnitus can disturb sleep and activities conducted in a quiet environment. If a sleep problem is associated with tinnitus, the patient should be asked whether any masking devices or techniques are used or have been tried to drown out the tinnitus. The nurse should also assess for snoring because it can be caused by swelling or hypertrophy of tissue in the nasopharynx. This excessive tissue can impair the functioning of the eustachian tube and cause the sensation of ear fullness or pain.
Cognitive–perceptual pattern
Pain is associated with some ear problems, particularly those involving the middle ear. If pain is present, the patient should be asked to describe the pain and the treatments used for relief. The effect on the pain level when the ear is moved should also be noted.
Hearing loss is associated with many middle and inner ear problems. The nurse or family may report the patient’s decreased hearing or the patient may express concern about perceived hearing loss. If decreased hearing is noted, the patient and family should be questioned about the duration, severity and circumstances associated with the decreased hearing.
Self-perception–self-concept pattern
Patients should be asked to describe how the ear problem has affected their personal life and feelings about themselves. Hearing loss and chronic vertigo are particularly distressing for patients. Hearing loss can result in embarrassing social situations that cause the patient to have a diminished self-concept and may lead to social isolation. The nurse should sensitively question the patient about the occurrence of such situations.
Patients with chronic vertigo may at times be accused of alcohol intoxication. The patient should be asked whether this has happened and, if so, how the situation was handled.
Role–relationship pattern
The patient should be questioned about the effect the ear problem has had on family life, work responsibilities and social relationships. Hearing loss can result in strained family relations and misunderstandings. Failure to acknowledge hearing loss and failure to seek treatment can further hinder family relationships.
The patient should be questioned regarding employment or contact with environments that have excessive noise levels, such as working with jet engines and machinery, and having contact with the firing of firearms and electronically amplified music. The use of ear protection or preventative devices worn in noisy environments is important to document.
Many jobs rely on the ability to hear accurately and respond appropriately. If a hearing loss is present, the nurse should gather detailed information of the effect that this has on the patient’s job. The patient should be assisted to evaluate the job situation realistically.
Hearing loss often leaves the patient feeling isolated from valued social relationships. The nurse should gather information about social activities such as playing cards, going to the movies and attending church from before and since the hearing loss occurred. Comparison of the frequency and enjoyment of the events can indicate whether a problem is present.
The unpredictability of vertigo attacks can have devastating effects on all aspects of a patient’s life, as ordinary activities such as driving, child care, housework, climbing stairs and cooking all have an element of danger. The patient should be asked to describe the effect of the vertigo on their many roles and responsibilities. Compensatory practices to avoid the development of dangerous situations should also be noted.
Sexuality–reproductive pattern
The nurse should determine whether hearing loss or deafness has interfered with the establishment or maintenance of a satisfactory sex life for the patient. Although intimacy does not depend on the ability to hear, it could interfere with establishing a relationship that could develop into a sexual relationship, or with maintaining a current relationship.
Coping–stress tolerance pattern
The patient should be asked to report their usual coping style, tolerance for stress, stress-reducing behaviours and available support. This information enables the nurse to determine whether the patient’s resources are adequate to meet the demands imposed by the ear problem. If the nurse concludes that the patient seems unable to manage the situation, outside intervention may be required. Denial is a common response to a hearing problem and should be assessed.
Value–belief pattern
The patient should be questioned about any conflicts related to values or beliefs that are produced by the problem or treatment. Every effort should be made to resolve the problem so that the patient does not experience additional stress. The nurse should ask whether the patient uses alternative (home) remedies, such as hot oil in the ear.
OBJECTIVE DATA
Physical examination
The nurse can collect valuable objective data regarding the patient’s ability to hear during the health history interview. Clues such as posturing of the head and the appropriateness of responses should be noted. Does the patient ask to have certain words repeated? Does the patient intently watch the nurse but miss comments when not looking at the nurse? Such observations are significant and should be recorded. This is also important because the patient is often unaware of hearing loss or does not admit to changes in hearing until moderate losses have occurred.
A normal assessment of the ear is listed in Box 20-2. Age-related changes of the auditory system and differences in assessment findings are listed in Table 20-6.
External ear
The external ear is inspected and palpated before examination of the external canal and tympanum. The auricle, preauricular area and mastoid area are observed for symmetry of both ears, colour of skin, nodules, swelling, redness and lesions. The auricle and mastoid areas are then palpated for tenderness and nodules. Grasping the auricle may elicit pain, especially if inflammation of the external ear or canal is present.
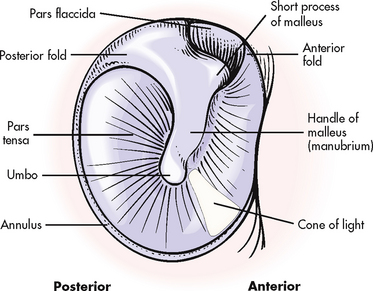
External auditory canal and tympanum
Before inserting an otoscope, the nurse should inspect the canal opening for patency, palpate the tragus and move the ear about to check for discomfort. After inspecting the canal opening for patency, an otoscopic examination can be performed. Key factors in proper use of the otoscope are adequate illumination, absence or clearing of cerumen and a tight seal of the speculum in the ear canal.18 A speculum slightly smaller than the size of the ear canal is selected. The otoscope should be held in such a way as to enable secure bracing against the patient’s head in order to avoid injuring the ear if, for instance, the patient makes a sudden movement (see Fig 20-9). The otoscope should be inserted slowly and never forced. Without causing discomfort, the auricle should be moved to align the cartilaginous part of the ear canal with the bony portion. The walls of the canal can then be inspected for sores, scratches, injuries, cerumen, pus or objects (flies, beads, old tissue). The canal is observed for size and shape, and the colour, amount and type of cerumen. If a large amount of cerumen is present, the tympanum may not be visible. The tympanum is observed for colour, landmarks, contour and intactness (see Fig 20-10).
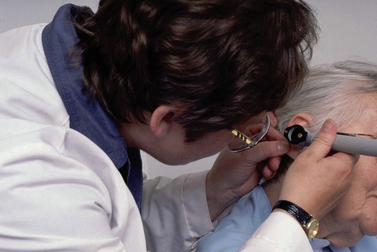
Figure 20-9 Otoscopic examination of the adult ear. The auricle is pulled up and back. The hand holding the otoscope is braced against the face for stabilisation.
Source: Wellcome PhotoLibrary, Wellcome Images.
The tympanic membrane (eardrum) separates the external ear from the middle ear. It is pearl-grey, white or pink, shiny and translucent. The anteroinferior quadrant is situated obliquely in the ear canal and is furthest from the examiner. The major landmarks are formed by the short process of the malleus superiorly, the handle, or manubrium, and the umbo, the most depressed point of the concave tympanum. From the innermost part of the tympanum a light reflex or cone of light is formed with the point directed towards the umbo. The circumference of the tympanum is thickened into a dense, whitish, fibrous ring or annulus, except in the superior area. The tympanum within the annulus is taut and is called the pars tensa. Above the short process of the malleus is the pars flaccida, the flaccid part of the tympanum. The malleolar folds are anterior and posterior to the short process of the malleus. The middle and inner ear cannot be examined with the otoscope because of the tympanic membrane. Table 20-8 summarises common assessment abnormalities of the auditory system.
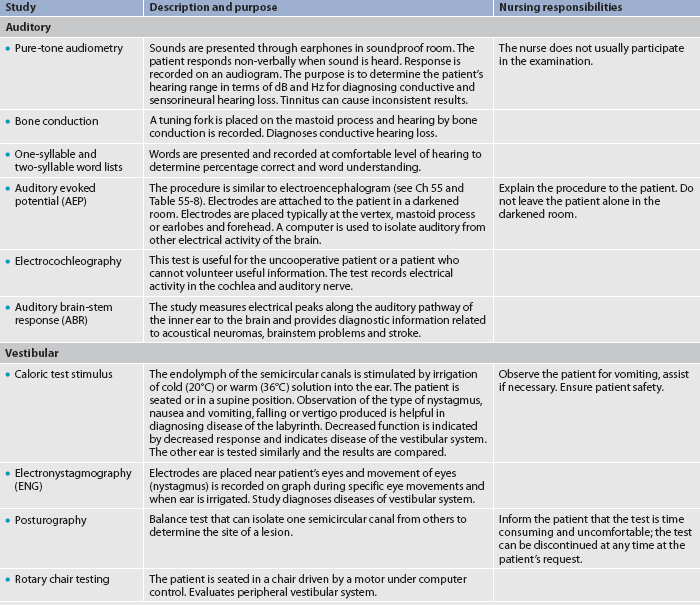
Diagnostic studies of the auditory system
Table 20-9 describes diagnostic studies commonly used to assess the auditory system.
TESTS FOR HEARING ACUITY
Tests involving the whispered and spoken voice can provide gross screening information about the patient’s ability to hear. Audiometric testing provides more detailed information that can be used for diagnosis and treatment.
In the whispered test the examiner stands 60 cm to the side of the patient and, after exhaling, speaks using a low whisper. If the patient does not respond correctly, the examiner moves forward to 30 cm and uses the same low whisper. Spoken voice, increasing in loudness, is similarly used. The patient is asked to repeat numbers or words or answer questions. Each ear is tested. The ear not being tested is masked with the patient occluding the ear or with the examiner moving a finger rapidly, close to the ear canal.
Tuning-fork tests
Tuning-fork tests aid in differentiating between conductive and sensorineural hearing loss. Tuning forks of 256 Hz, 512 Hz (sometimes called middle C tuning fork) and 1024 Hz are generally used for this examination. Both skill and experience are required to ensure accurate results. If a hearing problem is suspected, further evaluation by pure-tone audiometry is essential. The most common tuning fork tests are the Rinne test (to assess for damage to the auditory nerve that carries sound in the inner ear, i.e. sensorineural hearing loss) and Weber’s test (to assess any loss of sound travelling through the ear, i.e. conduction hearing loss). Normally, Weber’s test is performed before the Rinne test.
For Weber’s test, the nurse activates the tuning fork (by striking the fork lightly against the hand) and places it on the midline of the patient’s skull, forehead or teeth. The patient is asked to indicate where the sound is heard best. In normal auditory function the patient perceives a midline tone (i.e. they hear the sound equally in both ears). If the patient has a conductive hearing loss in one ear, sound is heard louder (lateralises) in that ear. If a sensorineural loss is present, sound is louder (lateralises) in the unaffected ear.
For the Rinne test the base of an activated tuning fork is held first against the mastoid bone (the bone behind the ear) and then in front of the ear canal (10–25 cm). The nurse starts counting in seconds and asks the patient to advise when the sound stops (the nurse needs to remember how many seconds it took). The patient reports whether the sound is louder behind the ear (on the mastoid bone) or next to the ear canal. When the sound is no longer perceived behind the ear, the fork is moved next to the ear canal until the patient indicates that the sound is no longer heard. As soon as the patient says the sound has stopped, the nurse moves the fork to the other ear (without touching the ear and starting counting in seconds again). The nurse records the times in seconds against the bone and against the ear opening. The patient should hear the air conduction tone (against the ear opening) for twice as long as when behind the ear. Thus, the Rinne test is positive when the patient reports that sound by air conduction (AC) is heard longer than by bone conduction (BC). This can indicate normal hearing or a sensorineural loss. If the patient hears the tuning fork better by bone conduction, the Rinne test is negative and indicates that a conductive hearing loss is present.
Results of tuning-fork tests are subjective. The patient with inconsistent test results or questionable results should be referred for more objective audiometric evaluation.
Audiometry
Audiometry is beneficial as a screening test for hearing acuity and as a diagnostic test for determining the degree and type of hearing loss. The audiometer produces pure tones at varying intensities to which the patient can respond. Sound is characterised by the number of vibrations or cycles that occur each second. The hertz (Hz) is the unit of measurement used to classify the frequency of a tone; the higher the frequency, the higher the pitch. Hearing loss can affect certain sound frequencies. The specific pattern produced on the audiogram by these losses can assist in the diagnosis of the type of hearing loss. The intensity or strength of a sound wave is expressed in terms of decibels (dB), ranging from 0 to 140 dB. The intensity of a sound required to make any frequency barely audible to the average normal ear is 0 dB. Threshold refers to the signal level at which pure tones are detected (pure-tone thresholds) or the signal level at which the patient correctly hears 50% of the signals (speech detection thresholds).
Normal speech is approximately 40–65 dB; a soft whisper is 20 dB. Normally, a child and a young adult can hear frequencies from about 16 to 20,000 Hz, but hearing is most sensitive between 500 and 4000 Hz. This range is similar to the frequency range of speech. A 40–45 dB loss at these frequencies causes moderate difficulty in hearing normal speech. A hearing aid may be helpful because it amplifies sound. Patients with a loss primarily in the higher frequencies, such as 4000–8000 Hz, have difficulty distinguishing the high-pitched consonants. Words such as cat, hat and fat may not be perceived accurately because the important information conveyed by the consonant is not heard. A hearing aid makes sound information louder but not clearer and so may not be helpful to patients who have problems with discrimination of sounds or sound information, because the consonants are still not heard enough to make speech understandable.
Screening audiometry
Screening audiometry is the testing of large numbers of people with a fast, simple test to detect possible hearing problems. A pass–fail criterion is used to screen people who will or will not be given additional diagnostic testing. People who fail the screening should be referred for threshold audiometry. In screening audiometry, the audiometer is usually set at a hearing level of 10–20 dB. Patients wear earphones as the tester sweeps across the available signal frequencies. They are directed to raise their hand when a sound is heard. Responses to air-conducted tones are checked at each frequency setting.
Pure-tone audiometry
A pure-tone audiometer produces pure tones at variable frequencies and intensities. Threshold audiometry generally determines thresholds for seven frequencies from 250 to 8000 Hz. The intensity is plotted against the frequency on an audiogram. In a quiet setting a tone loud enough to be clearly heard by the patient is presented. The threshold level for frequency is then determined. A person with a threshold at 25 dB or higher will demonstrate problems in everyday communication. A 26 dB hearing loss is used as a guideline for further action, but a hearing aid or surgery is rarely recommended for a hearing loss of less than 25–30 dB.19
SPECIALISED TESTS
The more specialised tests of the auditory system are most often performed in an outpatient setting by an audiologist. An audiologist can perform many additional tests with the advent of audiometers and computers that record electrical activity from the middle ear, inner ear and brain (see Table 20-9). The most common test performed by the audiologist is pure-tone audiometry. The audiologist can also test bone conduction to aid in differentiating sensorineural from conductive hearing losses.20 The nursing responsibilities include: (1) explaining the examination in general terms; (2) informing the patient if there are any dietary restrictions, such as caffeine or other stimulants; and (3) advising the patient if sedation will be used.
More sophisticated tests are available to determine the origin of certain hearing losses. These include evoked potential studies (also called auditory brainstem response) and electrocochleography. Computed tomography (CT) and magnetic resonance imaging (MRI) scans are used to diagnose the site of a lesion, such as a tumour of the auditory nerve.
TESTS FOR VESTIBULAR FUNCTION
Nystagmus, an abnormal involuntary repetitive movement of the eyes, can be caused by disturbances in the endolymph fluid. The movement of the endolymph fluid stimulates receptor cells and causes nystagmus. Lesions in the CNS (e.g. multiple sclerosis) and drug toxicity can also cause nystagmus. In the test for nystagmus, the patient looks straight ahead and then follows the examiner’s finger to an extreme lateral gaze. Quick jerking movements along the way, except on extreme lateral gaze, are considered abnormal.
Caloric testing and electronystagmography are specific tests used to evaluate the function of the vestibular system (see Table 20-9). For the caloric test, the patient’s ear canal is irrigated with cold or warm water, which causes disturbances in the endolymph. The patient’s reaction is observed for nystagmus. This observation may be made subjectively by the examiner or objectively with electronystagmography, using electrodes placed around the patient’s eyes. A normal individual will have nystagmus when water is instilled in the ear, with cold water producing nystagmus on the opposite side of instillation. Peripheral or brain lesions are suspected in the patient with no nystagmus elicited by caloric testing. Drugs that may alter the test results include alcohol, CNS depressants and barbiturates. The patient’s use of these substances should be known before testing.
Platform posturography and rotational chair tests (see Table 20-9) isolate one semicircular canal from the other to determine the site of a lesion causing vestibular disturbance. They can also provide data concerning the degree of disability caused by the disorder. These tests are time consuming and in those patients with vestibular disturbance can cause distress and discomfort, particularly nausea and vomiting. The patient will require pre-test instructions regarding intake of substances that can affect test results. In addition, the patient should be reassured that the test can be discontinued if stimulation to the vestibular system cannot be tolerated.
1. In a patient who has a haemorrhage in the posterior chamber of the eye, the nurse knows that blood is accumulating:
2. Increased intraocular pressure may occur as a result of:
3. The nurse should specifically question patients using eye drops to treat glaucoma about:
4. The nurse should always assess the patient with an ophthalmic problem for:
5. During assessment of hearing the nurse would expect to find:
7. Before injecting fluorescein for angiography, the nurse should:
1 Smith SC. Basic ocular anatomy. Insight. 2008;33:19.
2 Thibodeau G, Patton K. Structure and function of the body, 13th edn. St Louis: Mosby, 2008.
3 Saunders nursing drug handbook, 2009. St Louis: Saunders, 2009.
4 Reichel E. Hereditary cone dysfunction syndromes. In Albert DM, Jakobiec FA, eds.: Principles and practice of ophthalmology: clinical practice, 2nd edn., Philadelphia: Saunders, 1999.
5 Taylor H. Eye health in Aboriginal and Torres Strait Islander communities: better vision for all. Canberra: Commonwealth of Australia, 1997.
6 Jarvis C. Physical examination and health assessment, 4th edn. Philadelphia: Saunders, 2004.
7 Mannish MJ, Zadnik K, Carol-Ghanem C, Kara-José N. Contact lenses in ophthalmic practice. New York: Springer, 2004.
8 Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta-carotene, and zinc for age-related macular degeneration and vision loss. Arch Ophthalmol. 2001;119:1417.
9 Riordan-Eva P. Eye. In Tierney L, McPhee S, Papakadis M, eds.: Current medical diagnosis and treatment, 44th edn., New York: McGraw-Hill, 2005.
10 Council of Remote Area Nurses of Australia (CRANA). National clinical procedures manual for remote and rural practice. Alice Springs: CRANA, 2001.
11 Queensland Health and The Royal Flying Doctor Service. The primary clinical care manual, 4th edn. Brisbane: Queensland Health, 2005.
12 Vale A, Buckley J, Elliott D. Gait alterations negotiating a raised surface induced by monocular blur. Optom Vis Sci. 2008;85:1128.
13 Lum CL, Jeyanthi S, Prepageran N, et al. Antibacterial and antifungal properties of human cerumen. J Laryngol Otol. 2008;11:1.
14 Seidel HM, Ball JW, Dains JE, Benedict GW. Mosby’s guide to physical examination, 6th edn. St Louis: Mosby, 2006.
15 Brookhauser PE. Diseases of the cochlea and labyrinth. In: Wetmore RF, Muntz HR, McGill TS, eds. Pediatric otolaryngology: principles and practice pathways. New York: Thieme, 2000.
16 Mosby’s drug consult. 17th edn. St Louis: Mosby; 2007.
17 Peeters J, Naert I, Carette E, et al. A potential link between oral status and hearing impairment: preliminary observations. J Oral Rehabil. 2004;31:306–310.
18 Holcomb SS, ed. New guidelines improve treatment of otitis media. Nurse Practitioner. 2004;29:6–13.
19 DeChicchis AR, Bess FH. Hearing aids and assistive listening devices. In Bailey BJ, Calhoun KH, Derkay CS, et al, eds.: Head and neck surgery—otolaryngology, 4th edn., Philadelphia: Lippincott-Raven, 2006.
20 Chernecky C, Berger B. Laboratory tests and diagnostic procedures, 5th edn. Philadelphia: Elsevier Saunders, 2007.