What Your Doctor Might Find in Women
TO MEN, VISITING a urologist is a last resort. But for you, visiting an RE is no different from seeing your OB/GYN—it’s just another doctor giving you another pelvic exam. But what makes this visit (and subsequent ones) unique is that it determines whether or not you’ll be a mom. Think about the emotional void you feel if you’ve always envisioned yourself carrying your own child to term. Not knowing whether your child will share your biology can increase your anxiety until you have answers you trust.
What the Workup Was Like for Me
This may sound crazy, but I felt like a failure as a woman because of my inability to get pregnant. But I am working through it and doing all the right things now. Mark and I stopped occasional smoking, drinking, and all caffeine. So now when I get pregnant, I won’t have to quit anything!
—Natalie, 38, real estate investor
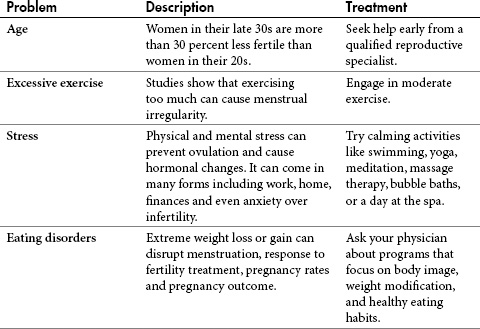
Sometimes simple changes to your environment or lifestyle can have a significant impact on your fertility. While you can’t turn back the clock (don’t we wish!), you certainly can modify your eating habits; exercise routine; need to smoke, drink, or do recreational drugs; or the way your body reacts when under stress (see chapter 5).
If everything goes well with your RE visit, your fertility workup will indicate you’re as fertile as a rabbit. But this is not the case for the majority of women who have difficulty conceiving. Most women visiting an RE will learn that their infertility is a result of one (or more) of five factors: ovarian, cervical, tubal, uterine, or peritoneal.
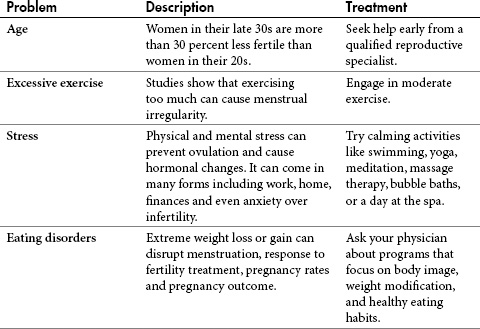
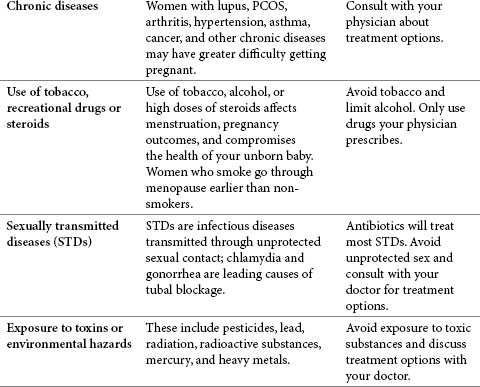
Table 4.1. Contributing factors to infertility in women
There are many reasons why you may have poor egg quality. The main culprit is age. Your fertility steadily declines starting in your mid-20s, and once you reach 30 the decline is more pronounced. This decline plummets further by 40. In fact, more than one-third of women who wait until their mid to late thirties will experience fertility problems. But all that is about to change now that you can review your workup results and address what’s keeping you from getting pregnant.
Doctors identify ovulatory dysfunction in 40 percent of infertile women. Warning signs include irregular, abbreviated, or absent menstrual cycles. Many women don’t think twice about missing a period every so often, but this is your body’s signal that you have an underlying problem. Without an evaluation, it could be serious. The list of possible causes includes eating disorders, extremes of weight loss or exercise, hyperinsulinemia, hyperandrogenism (elevated male hormone), hyperprolactinemia (elevated prolactin), obesity, pituitary tumor, and thyroid disease. If you’re not ovulating, you can expect your doctor to administer tests that measure your thyroid-stimulating hormone levels, your prolactin and estrogen levels, and insulin resistance.
Polycystic Ovarian Syndrome
Polycystic ovarian syndrome (PCOS) is a condition that affects a woman’s menstrual cycle, fertility, hormones, insulin production, heart, blood vessels, and appearance. It’s the most common hormonal problem in women of childbearing age. Insulin resistance is usually the primary cause of PCOS. With PCOS, women produce excess insulin, and this interferes with proper secretion of FSH and LH from the pituitary. This makes ovulation rare or nonexistent.

![]() How Widespread Is PCOS?
How Widespread Is PCOS?
Polycystic ovarian syndrome (Stein-Leventhal syndrome) affects 5 to 10 percent of women of childbearing age.
When a woman ovulates, her follicle releases a mature egg. If you have PCOS, your follicle development halts at an early stage, leaving you with ovarian buildup of small, benign, estrogen-releasing cysts. This buildup enlarges your ovaries and causes an increase in cells that secrete male hormones (androgens) like testosterone. These hormones stimulate the development of masculine features. This means that you might have irregular menstrual periods (or none at all), irregular insulin levels, acne, obesity, and excessive hair growth on your face, chest, or abdomen.
By now you’ll know if your doctor found any issues with your FSH, LH, prolactin, TSH (thyroid stimulating hormone), DHEAS (male hormone), and testosterone. If you have a history of obesity, an inverted FSH/LH ratio, or too much male hormone, he’ll test your glucose and insulin levels. This is usually done after fasting and again two hours after ingesting a 75 gram glucose load called a two-hour glucose tolerance test. If your glucose-to-insulin ratio is greater than 4.5, you’re in the normal range. If you have an abnormal glucose-to-insulin ratio, then you’re insulin resistant and may have PCOS.
It’s normal to have some degree of anxiety before any test. But rest assured this is one you’ll definitely need if indicated. Diagnosis and treatment of PCOS can help make your life better all around. To unravel any mysteries surrounding this test, table 4.2 outlines what your doctor is looking for.
Table 4.2. How to read your glucose-to-insulin ratio
If your RE suspects you have PCOS, he’ll give you a thorough evaluation based on your symptoms and your medical history. It will entail a physical examination, blood tests to measure your hormone levels, and an ultrasound to view your ovaries.
Treatment options include taking fertility drugs like clomiphene citrate and gonadotropins to stimulate ovulation (see chapter 7). If your doctor detects insulin resistance, he’ll probably prescribe metformin (brand name Glucophage™), which reduces insulin levels. Metformin alone will cause about 40 percent of women with PCOS to ovulate spontaneously.
Women with PCOS sometimes respond differently to fertility medications from non-PCOS patients. PCOS patients frequently respond either too well to fertility drugs or not well enough. In those that respond too well (i.e., mature too many eggs), there is a greater risk for multiple births and ovarian hyperstimulation syndrome (OHSS). To control your risk for multiple births, your RE might recommend IVF to control the number of embryos. To reduce risk of OHSS, PCOS patients often start on lower initial doses of fertility medications. Fortunately, once on metformin, PCOS patients often respond more like non-PCOS patients.
Another important aspect to treating PCOS in maintaining an insulin resistance is diet. A low-carbohydrate diet will help keep your insulin levels to a minimum. This diet consists of eating small animals (birds and fish), eggs, green vegetables, nuts, and berries. It’s sometimes referred to as the “paleo diet” because it mimics the diets humans would have eaten in Paleolithic times as hunter-gatherers. Large animals (beef) are consumed no more than once per week, and all processed foods, especially those with refined sugar or flour, are eliminated (if you’ve always needed a reason to get rid of your sweet tooth, now you have one). A good rule of thumb to avoid processed foods is to only eat food without labels. Obviously, this diet requires you to purchase, prepare, and eat only fresh food, so it may require some adjustment if you’re on a standard American diet.
Women with PCOS have a very good prognosis to a change in diet. In fact, most will achieve pregnancy within the first year. The statistics are overwhelmingly in your favor, but it’s important to note that one in five women will miscarry.
A less popular treatment option for PCOS is surgery. In rare cases a surgeon will reduce ovarian cysts by vaporizing a portion of your ovary (we know it sounds like something off the Starship Enterprise, but trust us—it’s real) to improve your hormonal imbalance and ovulation cycle, but results are often temporary. Ovarian cysts often reappear in women with PCOS because their ovaries constantly overproduce follicles compared with women with no history of this condition.
TIPS FOR KEEPING PCOS UNDER CONTROL
• Schedule regular OB/GYN checkups to monitor changes in your ovaries or uterine wall caused by irregular bleeding.
• Make sure that you have induced menstruation at least every three months to prevent endometrial cancer.
• Request blood tests to monitor your hormonal imbalance and confirm insulin resistance.
• Lose weight (if you need to) and eat a controlled carbohydrate diet to reduce insulin levels.
• Try moderate continuous exercise for 30 minutes daily to reduce insulin resistance.
• Birth control pills can reduce free levels of androgens in those not trying to conceive.
• Spironolactone and other medications may reduce facial hair. But do not take if you’re trying to get pregnant.
Talk to friends who have PCOS or get support from other women by visiting the Polycystic Ovarian Syndrome Association (see Resources on page 313).
Premature ovarian failure (POF) results in menopause in women younger than 40. POF causes your ovaries to stop releasing eggs and making estrogen, so you may experience symptoms of menopause, including the following:
• irregular menstrual periods
• shortening of menstrual periods
• absence of menstrual periods
• hot flashes
• mood swings
• vaginal dryness
There have been instances where women resume spontaneous ovulation, but this is rare.
POF has many causes, but a cause may not be determined in every case. Possible causes may include autoimmune disorders (when your body’s immune system attacks your ovary), genetic mutations or deletions, familial tendency, past pelvic infections, and previous ovarian surgery. Many cases are simply random events that prevented enough eggs from forming when you were a fetus (we call this bad luck). If you have relatives with POF, your chances of developing it are somewhat higher. Some women have abnormalities in genes that oversee ovarian function, a few make antibodies that prevent their ovaries from working, and a very small amount suffer from viral infections that have attacked their ovaries.
Treatments for POF include hormone replacement therapy, which gives your body the estrogen it’s missing along with progesterone. Your RE will likely recommend IVF with donor eggs as your best and probably only option for pregnancy. But if you’re determined to have a biological child and wish to give it a shot despite test results and your doctor’s advice, then by all means try.

![]() Egg Donation as an Option
Egg Donation as an Option
Egg donation increases your chance of pregnancy by 25 to 30 percent per attempt. This is because it’s the age of the egg that matters, not the age of the mother.
Resistant Ovarian Syndrome
If your ovaries have slowed down progressively but you ovulate occasionally, you may have resistant ovarian syndrome. This is a rare condition found in 20 percent of patients with POF. In this condition your ovaries fail to respond to your body’s natural FSH and LH. As a result, you will not respond to fertility drugs like gonadotropins. Under ultrasound evaluation your doctor will note that you have an absence of developing follicles.
Diminished Ovarian Reserve
Diminished Ovarian Reserve is a condition that occurs when you’re reaching the end of your egg supply. Elevated FSH levels indicate diminished ovarian reserve. With this condition you have used most of the egg producing follicles in your ovaries and are nearing the end of your supply. When you reach this point the eggs that remain are generally of lesser quality. This reduced quality facilitates decreased pregnancy rates seen with age as well as increased miscarriage rates and chromosomal abnormalities seen in pregnancies of older women. Women with diminished ovarian reserve do not respond well to fertility medications. This results in low egg production during fertility treatment cycles.
Hormonal Imbalances
Hormonal imbalances often lead to ovulation irregularities. If your prolactin level is too high or your thyroid level is too low, you may experience irregular ovulation. It’s important to test for these conditions because treatment is simple and often results in rapid resumption of ovulation.
Sperm relies on the hospitality of your cervical mucous to reach your eggs. Your partner’s sperm can’t reach your eggs if your cervical gland isn’t producing purposeful mucous. This slippery mucous provides an ideal environment so your partner’s sperm can pass through the cervical canal. Your mucous also nourishes and supports your partner’s semen while it swims toward your fallopian tubes. Here’s a list of cervical problems that can cause infertility.
• inadequate or inhospitable mucous
• immune system attacks sperm
• cervical narrowing, or “stenosis”
• cervical infections due to STDs
Your mucous changes throughout your menstrual cycle depending on the hormones your body is producing. During the first half of your cycle your body produces estrogen, which makes your mucous slippery like raw egg whites. After ovulation your body produces progesterone, which makes your mucous thick and sticky. Sperm cannot penetrate this type of mucous, as it would be like swimming in jelly. Besides facilitating your partner’s sperm, mucous may have a protective function that prevents bacteria from entering your uterine cavity.
Problems with cervical mucous usually don’t cause symptoms. If your cervical mucous contains antisperm antibodies, your immune system will mistake sperm as foreign invaders and destroy them. If your RE has determined that you’re ovulating but suspects cervical factor infertility, she might order a postcoital test (PCT). This test lets your doctor analyze your cervical mucous to see how well your partner’s sperm survives in it. The only way she can do this is if you arrive at her office two to eight hours after having intercourse. The PCT is rare these days because the most basic fertility treatment (Clomid/IUI) will place sperm beyond the cervix.
Cervical injuries or infections may cause scarring and narrowing of the cervix (cervical stenosis). Often cervical stenosis and scarring can obstruct menstrual blood from exiting and cause increased menstrual cramping and a higher incidence of endometriosis and infertility.
Another way you can acquire cervical stenosis is after surgical procedures like dilation and curettage (D&C); cervical conization (samples abnormal tissue from cervix); loop electrosurgical excision procedure (LEEP), which treats precancerous changes in the skin of the cervix; or cryosurgery. Your body repairs itself after surgery by developing scar tissue, and sometimes this scar tissue can lead to problems like cervical stenosis (an STD can cause this too).

![]() What Is a D&C?
What Is a D&C?
Dilation and curettage (D&C) is a procedure that involves surgical dilation of the cervix to allow access to the uterine cavity. A surgeon uses a metal device called a curette to scrape out the contents. Besides pregnancy termination, you may have a D&C to stop abnormal bleeding, diagnose causes of abnormal bleeding, remove uterine polyps, or remove tissue after a miscarriage.
Asherman’s syndrome, or scar formation inside the uterus, is a complication of elective abortion and D&C. Asherman’s syndrome is uncommon but is more likely if there was an infection after the procedure, if there was a follow-up procedure to remove leftover tissue, or when there were three or more terminations. Your doctor will remove the scar tissue with a hysteroscopy.
If your hormone levels are normal but you still have unexplained infertility, your RE will turn his focus to your fallopian tubes. Tubal blockage or dysfunction can often cause infertility by keeping sperm from reaching your egg or keeping your egg from passing into the uterus. Trauma, infection, and congenital deformities are all potential causes of blocked tubes.
As we discussed on page 33, your doctor will order an HSG. The procedure for an HSG is fairly simple. A radiologist carefully inserts a catheter into your uterus and injects a special dye into the catheter. While she watches a monitor that shows x-rays of your abdomen, the dye flows up into your tubes. (She’ll usually let you see too, if you ask). She’ll determine that you have an obstruction if the dye pools in one or both tubes. For best results you should take this test following your menstrual cycle once bleeding has stopped and before ovulation occurs. After your HSG your physician will review the films to confirm the findings.
If the HSG detects any blockages, you’ll need in vitro fertilization. If dilated fallopian tubes are present (a condition called hydrosalpinx), your physician may recommend a hysteroscopy (laparoscopy of the uterus) to remove them prior to in vitro fertilization. This involves viewing your internal organs through a fiber-thin flexible scope with a camera at the end that your doctor inserts through your navel (to eliminate scarring) and two small incisions, through which your doctor will insert fine tools to cut and remove the tube.
After this procedure you’ll be one step closer to your goal of parenthood. Several large studies indicate that the presence of a hydrosalpinx reduces IVF pregnancy rates by half. Once your specialist removes the damaged tube (using an outpatient surgical procedure called salpingectomy) these rates normalize. While physicians speculate that blockages occur from previous infections or endometriosis, the exact reason for your blockage will most likely remain unknown. The good news is that IVF is extremely effective in women who have had a salpingectomy.
I had an HSG. When Dr. Potter showed me the x-ray of my fallopian tubes, one tube appeared normal and the other looked like a whale. He reassured me that removing this tube was the fastest way to increase our chances of getting pregnant. He wasn’t kidding. The salpingectomy was quick, left almost no scars, and I was walking within an hour. Two months later I realized how important this surgery was.
Uterine abnormalities such as polyps, tumors, lesions, or congenital malformations (septated, partial, or absent uterus) can cause infertility. Once suspected, your doctor will order an HSG. She can use this not only to study your fallopian tubes but also to define the size and shape of your uterus. It will reveal any congenital defects of your uterine cavity such as bicornate uterus, T-shaped uterus, septate uterus, uterus didelphys, or acquired defects like fibroids, polyps, or scar tissue (see table 4.3).
While congenital abnormalities are rare, they do occur. And women who have them can feel singled out, isolated, and inherently different unless they seek guidance from an empathetic friend, physician, therapist, or support group. Remember that even in rare situations, there are always others who have walked the path that lies before you.
Even less common is Müllerian agenesis, or Mayer Rokitansky syndrome (also termed vaginal agenesis). It occurs in one out of 4,000 to 5,000 women. Table 4.3 describes what your RE will consult you on if he suspects this diagnosis or a related one.

Table 4.3. Congenital abnormalities of the uterus
Nearly all abnormalities can interfere with embryo implantation and may result in miscarriage. Uterine abnormalities occur in about 5 percent of infertile women. Severe cases might cause your RE to recommend using either a gestational or traditional surrogate. Luckily, severe congenital abnormalities are rare. More commonly seen are uterine fibroids. If your situation warrants further evaluation or removal, as in the case of uterine polyps or fibroid tumors, your doctor may order a hysteroscopy.
Uterine Fibroids
Fibroids are tumors that grow from muscle tissue in the uterus. They can be microscopic or can fill your uterine cavity (size of a cantaloupe), and they may weigh as much as 50 pounds. The largest reported fibroid weighed 140 pounds! Most are benign regardless of their size. Symptoms include the following:
• difficulty conceiving
• heavy menstrual bleeding
• urinary frequency
• fullness or pressure in lower abdomen
• backache
• constipation
No one knows what causes uterine fibroids, but there is a genetic aspect to them, as there are clusters among families and ethnic groups. Fibroids tend to grow in response to estrogen. Pregnancy is just one example of a time when their growth may increase due to the body’s peak in estrogen. Once you approach menopause and your estrogen levels decrease, your fibroids diminish and may disappear.
Nearly one-quarter of women of childbearing age develop uterine fibroids. Several small studies have found that athletes, smokers, and women who have delivered two or more babies vaginally are at a lower risk of developing fibroids opposed to those who have a family history and remain at a higher risk. Larger studies reveal that African American women are up to three times more likely to develop fibroids than are American women of European descent.
Typically your physician will find them during a routine pelvic exam. She may suspect fibroids if your uterus has lumps or irregularities. Fibroids usually do not require treatment; however, in severe cases treatment may be necessary. Your physician will evaluate your condition and make a recommendation based on one or more of the following: your level of discomfort and blood loss during menstrual periods, how rapidly your fibroids are growing, your age, your desire to bear children, and the position of the fibroids (since fibroids distort the uterine cavity and can contribute to infertility).
If you’re one of the individuals who require treatment, you have two surgical options. Assuming you want children, you’ll opt for a myomectomy. Using this procedure, your doctor will remove your fibroids, leaving your uterus intact. If you change your mind and decide to forgo having children, then you might opt for a hysterectomy. If your doctor performs this procedure, she’ll remove your entire uterus, making childbearing impossible.
While a hysterectomy is associated with less blood loss and years ago was the standard treatment for uterine fibroids, today it’s reserved for menopausal women who are past their childbearing years, women who wish to forgo childbearing, or those who have severe symptoms. Of the two treatments, a hysterectomy is the only procedure that guarantees fibroids will not reoccur. Ten years after a myomectomy there’s still a 25 percent chance of growing new fibroids that require a subsequent surgery. And both procedures warrant a four- to six-week recovery.
If the idea of surgery seems alarming, you do have viable alternatives. Lupron administered at very high doses will shrink or temporarily halt fibroid growth; however, this treatment has both positive and negative effects. Since prolonged use of Lupron (more than six consecutive months) can lead to irreversible loss of bone density (osteoporosis), your physician will generally prescribe it only for a limited period. Even if you sail through this time with little or no side effects, once your medication is discontinued, your fibroids are likely to resume growing.
A third technique that is receiving widespread interest is uterine artery embolization (UAE), or uterine fibroid embolization (UFE). A radiologist performs this procedure using imaging techniques to identify the exact location of your fibroid and the blood vessels around it. Once he finds your fibroid, he blocks the vessels that nurture it. Without blood, the fibroid starves and dissipates. Of all fibroid procedures, this is the least invasive (there’s no incision, only a needle prick in your thigh or groin). It typically requires a one-night hospital stay, and you can resume your normal activities within a week or two. This procedure (like all invasive procedures) is one to consider carefully only after discussing all your other options with your partner and doctor. Proceed with caution, because there is still no consensus on whether fertility is realistic after UFE.
Peritoneal-factor infertility occurs when your peritoneum (the thin lining of your abdominal cavity) becomes irritated through infection or with endometriosis, resulting in scarring and adhesions in your pelvis.
Endometriosis
Endometriosis is a progressive disease where the tissue lining your uterus (endometrium) implants and grows in your abdominal cavity. Once this occurs it usually attaches to the reproductive organs (ovaries and fallopian tubes), intestines, rectum, or bladder. Your endometrial tissue is the same tissue that normally sloughs off during your menstrual cycle. When you menstruate, the foreign tissue in your pelvis also bleeds (e.g., uterine lining sluffing off), causing irritation and inflammation that can lead to scar formation and distortion of your pelvic anatomy. This anatomical distortion can cause infertility. Strangely enough, severity of symptoms seen with endometriosis doesn’t correlate with severity or stage of the disease. Some women have little or no pain from severe endometriosis while others with mild disease experience immense discomfort before or during their period. Symptoms of endometriosis include
• extremely painful menstrual cramps (dysmenorrhea), especially if this condition develops after years of pain-free periods
• discomfort during intercourse (dyspareunia)
• pelvic, back, or side pains before or during periods
• rectal pain or painful bowel movements, diarrhea, constipation, or other intestinal upsets during menstruation
• frequent and painful urination during periods
• infertility
If your doctor diagnoses you with endometriosis, she’ll determine the severity of it based on a point system (staging), which takes into consideration the number and size of your growths and adhesions. While you undergo minor surgery, she’ll evaluate the location, diameter, depth, and density. Staging classifies growths and lesions into minimal, mild, moderate, and severe cases.
No one knows for sure why some women develop this condition and others don’t. One school of thought is that all women experience this type of backflow, but in most cases the immune system destroys this abnormal tissue before it settles and grows in the abdomen. Another, less adopted theory is that remnants of a woman’s own embryonic tissue that formed while she was in her mother’s womb may develop into endometriosis during adulthood or may transform into tissue of the uterine lining outside the uterus.

![]() How Common Is Endometriosis?
How Common Is Endometriosis?
Endometriosis is one of the most common gynecological diseases, affecting more than 5.5 million women in the United States and millions more worldwide.
While no cure exists, there are a number of treatment options for endometriosis. If you have any symptoms mentioned previously, your doctor will recommend a laparoscopy. Currently, this procedure is the only way to accurately diagnose endometriosis.
Though medications that interfere with ovulation such as oral contraceptives and progestins might provide some pain relief, recurrence rate following drug therapy remains high, and this type of treatment fails to resolve infertility. If your goal is to improve your pregnancy rate, resolve your infertility, and experience long-term pain relief, then you’ll want to opt for surgical treatment.
Other surgical options for severe pain include ovary removal (oophorectomy) or hysterectomy, but only women who wish to forgo childbearing should consider these major surgical procedures. Here are some nonsurgical tips for easing endometriosis pain.
• Rest on a comfortable sofa when experiencing pain.
• Take Advil or Motrin up to 440 mg every four hours.
• Take warm baths.
• Place a hot water bottle, hot pack, or a heating pad on your abdomen.
• Drink plenty of water and eat foods high in fiber to prevent constipation.
• Use techniques to help you relax, like yoga, deep breathing, and visualization.
• Stay informed of your condition, and discuss new treatments options with your physician.
• Talk to friends who have endometriosis or get support from other women by visiting the Endometriosis Association (see Resources on page 313).
Pelvic Adhesions
Another peritoneal condition that can result in infertility is pelvic adhesions. These are bands of fibrous scar tissue that can form in the abdomen and pelvis after surgery or an infection. Because adhesions connect organs and tissue that are normally independent, they can lead to a variety of complications, including pelvic pain, infertility, and bowel obstruction. For instance, if your ovaries are affected, instead of being somewhat mobile, they might adhere to the back of your uterus, to your uterine wall, or to the bowel.
How do you treat pelvic adhesions? If you’re not feeling pain, then your doctor will probably recommend not doing anything. For mild or moderate pain he might suggest medication, acupuncture, or medical hypnosis. But if your pain is severe, he’ll likely suggest surgery to separate your adhesions. This allows normal movement of affected organs and reduces symptoms caused by adhesions. Keep in mind that your risk of developing more adhesions increases with every surgery because this is part of your body’s healing process.

![]() What If Your Pelvic Exam Results in a Cancer Diagnosis?
What If Your Pelvic Exam Results in a Cancer Diagnosis?
This is a rare situation, but it does happen. Honestly, there are not many situations that require you to preserve your fertility, but cancer is definitely one of them. See chapter 12 to learn how to bank your fertility for future use.
WHAT QUESTIONS SHOULD YOU ASK?
Visiting an RE is not much different than seeing your gynecologist. But the most notable difference is that you have a lot riding on this appointment. From your workup your RE will tell you what factors are contributing to your infertility, and he’ll recommend a treatment plan for maximizing your chances of conception. In some cases you may be able to resolve your infertility with low-tech treatments like Clomid or IUI, or he may suggest IVF. In either case you and your partner will walk away knowing the truth instead of wasting years guessing what could be wrong. Be sure to ask your RE the following:
• What are my chances of conceiving a biological child?
• What needs to occur to make this a reality?
• What treatment, if any, do you recommend before fertility treatments can begin?
• Visiting an RE is no different than seeing your OB/GYN, but what makes this visit unique is that it determines whether or not you’ll be a mom.
• Simple changes to your environment or lifestyle can have a significant impact on your fertility. Try modifying your eating habits; exercise routine; need to smoke, drink, or do recreational drugs; or the way your body reacts under stress (see chapter 5).
• Most women visiting an RE will learn that their infertility is a result of one (or more) of five factors: ovarian, cervical, tubal, uterine, or peritoneal.
• Some infertility factors become harder to treat the longer they persist.