6
The Neuroscience of ADHD
Whatever your view is on the cause of ADHD, we know that behavior is a result of the brain – even if we view it as a consequence of environmental input. Therefore it is understandable that differences in the brain between people with ADHD and controls have been investigated.
Early studies looking at the brain used post-mortem samples in which those who died with a particular disorder were compared with those who died without the disorder. Fortunately, in the last two decades, neuroimaging, in which the brain can be visualized, has become commonplace. As one would imagine, many studies of the brain have been conducted in children and adults with ADHD. With the rise in new technologies, such as functional magnetic resonance imaging (fMRI) within neuroimaging, it is possible to assess the functional activation and size of the brain in ADHD. However, we have to be careful that we do not get too seduced by these new technologies and over-extend what they can tell us.
Before we continue with the main purpose of this chapter, we have to address two fundamental areas before we can place ADHD in neuroanatomical context: (1) basic neuroanatomy – the regions and subregions of the brain; and (2) the methods for measuring differences in the brain between groups of patients and non-patients.
The Brain: A Brief Guide to Development and Neuroanatomy
The brain goes through many changes in utero and throughout life, most notably in early childhood and adolescence. The changes that occur in the brain during development can have serious ramifications for its internal functioning and ultimately its behavioral output. No matter what your perspective is, whether you consider the environment as a cause of ADHD or you have a Freudian view, it all ultimately comes down to the brain. For example, if ADHD is due to an over-restrictive and less tolerant society, it is the brain of the individual that is unable to adapt to that world, and given that the majority of the population do not have ADHD (although they might have another disorder), those with ADHD are different. Such a perspective is often dismissed as reductionistic and therefore meaningless in the social context. Critics will state that behavior is more than neural output. And of course they are correct: output is the end-point of the processing of inputs, and thereby the cultural and social context has an impact on the brain and in turn neural output changes the environment, which provides further input, and the process goes on and on. Whichever route you take, or whatever philosophy you adhere to, it will come back to the processes of the brain. I think I have given you my point of view!
The continual development of the brain, which includes growth and death of brain cells at key periods, means that neural structures are more vulnerable to toxicological/environmental insult – a problem more acute in males than females [281]. What many people find surprising is that the brain undergoes many changes up to about the age of 25 years [649–650]. As the brain develops, the use of drugs like methylphenidate has given cause for concern since it may influence neural development in a permanent way [334]. Many see ADHD as a delay in brain maturation; however, there may not always be a delay, as we now see the continuation of ADHD into adulthood. Recent studies support persistent neurological changes in ADHD [651]. However, the neurodevelopment of individuals with ADHD is currently an area that needs further evaluation as to which individual symptoms can be mapped to neural changes.
Regions of the Brain
During early brain development, the cells of the brain become differentiated and specialized. Cellular differentiation permits the architecture of the brain to be discerned. Some features can be seen clearly, such as the cerebellum – the cauliflower-like structure at the lower back of the brain. Others require scientific techniques to visualize them post mortem or via neuroimaging. The brain can be looked at from three orientations. There is a convention to describe what a particular orientation is or where sets of cells are situated. These terms prefix an area and provide a reference point to its location (e.g. lateral hypothalamus: an area towards the outer edge of the hypothalamus). If you see the words lateral, caudal, rostal, dorsal, ventral, and medial, these just refer to specific locations.
The level at which we look at the brain can be either large structures (e.g. cortex) or smaller components (e.g. single cells). The different regions of the brain have been associated with different behaviors. However, ascribing a particular function to one region is not simple because all the areas communicate with each other. One must not think of the regions of the brain working on one particular behavior alone; the regions communicate with each other in order to control behavioral processes. Despite this caveat, we often hear of brain regions that control a specific behavior.
A second caveat is linked to the issue of etiology. An example that best illustrates this point is the study conducted on London taxi drivers who have to pass “the Knowledge,” which is a test of spatial knowledge. The Knowledge is a test of a taxi driver’s ability to navigate routes around London. Professor Chris Frith and colleagues gave taxi drivers a positron emission tomography (PET) scan and found they had increased activation of the right hippocampus [652]. This study demonstrated an increased use of taxi drivers’ hippocampi but did not tell us if this was a result of being a taxi driver or if increased hippocampus is a prerequisite for becoming a taxi driver. A later study indicated that hippocampal volume was correlated with the amount of time spent as a taxi driver; thus taxi drivers’ brains may have changed as a result of the job they did [653]. In ADHD we have a similar chicken-and-egg conundrum: are the differences seen the cause of ADHD symptoms or a result of the symptoms’ impact on individuals? A final point to note is that something that one might think is the straightforward identification of brain regions is not always unanimously agreed upon. Different names are used by different authors, and some have different opinions about which regions can be included in a macrostructure comprising of numerous smaller regions.
The telencephalon part of the forebrain is made up of the two cerebral hemispheres containing the cortex, the limbic system, the basal ganglia, and the cerebellum – regions extensively studied in ADHD.
The cortex
The convoluted area of the brain is the cortex, which is the most recent addition to the brain in evolutionary terms. The brain is a bilateral organ with two cerebral hemispheres clearly visible. This bilateral aspect doesn’t mean that the hemispheres of the brain are complete mirror images of each other, but they are close. A fissure (large cortical fold) separates the two hemispheres. This has given rise to the concept of a right brain and a left brain with specialized functions, e.g. a language-dominant left hemisphere. Between the hemispheres are small connections called the cerebral commisures; the corpus callosum is the most obvious to the naked eye.
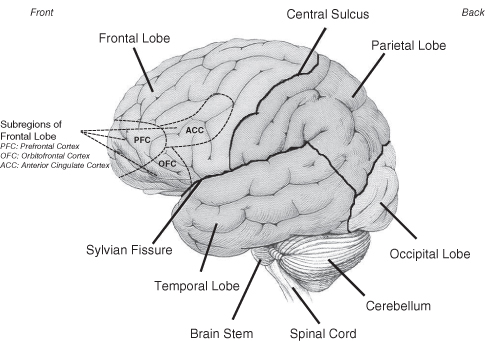
The lateral and central fissures divide the brain into four lobes: the frontal, occipital, temporal, and parietal lobes (see Figure 6.1). These areas are associated with various behavioral functions: the occipital lobe is the area of visual perception; the temporal lobe is the focus of many theories of memory; and the parietal lobe is associated with visuomotor guidance (see [654] for review). The frontal lobes are considered to be the area that makes us unique as humans. It is the frontal lobe, and its numerous connections, that is a region of interest in ADHD.
Figure 6.1 The cortical regions of the brain
The limbic system
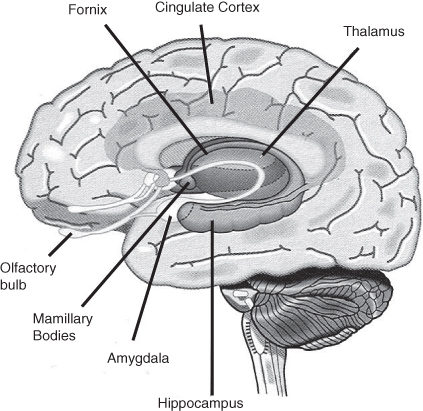
The limbic system is a network of cells that are thought to be involved in emotions and learning. The limbic system comprises the hippocampus, amygdala, cingulate cortex, fornix, septum, and mamillary bodies (see Figure 6.2). The hippocampus and the amygdala have been extensively studied in animals and humans (see [655]).
Figure 6.2 The limbic system
The basal ganglia
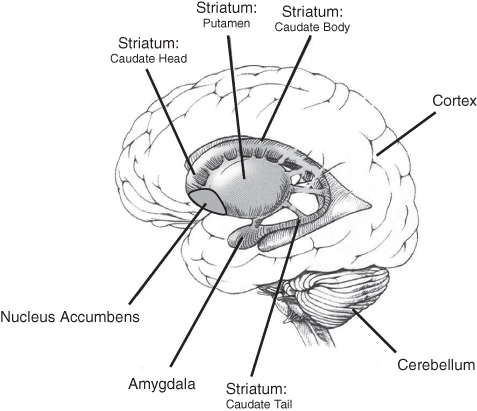
The basal ganglia comprise the striatum, the globus pallidus, and the substantia nigra; and in some classifications they also contain the amygdala (see Figure 6.3). The striatum is further subdivided into caudate and putamen. The globus pallidus has an internal and external part. The substantia nigra divides into two areas called the pars compacta and pars reticulata. The basal ganglia are extremely important in motor control and implicated in the pathology of ADHD and its subsequent treatment.
Figure 6.3 The regions of the basal ganglia
The cerebellum
This area of the brain sits at the back under the occipital lobe. It is the cauliflower-like structure that can be seen in MRI scans. The cerebellum is involved in motor control, but also in cognitive functions such as attention.
A Brief Account of Imaging the Brain
Imaging the brain without opening the skull is similar to taking X-rays of bones to determine a fracture. Neuroimaging requires a multidisciplinary team to conduct successful scans; medical staff, statisticians, physicists, and engineers are all needed. However, no amount of technology can make up for a poorly designed study.
Presently there are five main imaging techniques that are used. These five can fall into two camps: magnetic imaging and nuclear imaging. Many studies in ADHD use the magnetic imaging technique as it avoids the use of the radioactive substances that are required in nuclear imaging.
Within the domain of magnetic imaging are three different variations: (1) MRI – Magnetic Resonance Imaging; (2) fMRI – functional Magnetic Resonance Imaging; and (3) MRS – Magnetic Resonance Spectroscopy. All three methods can tell us something different about the brain.
Magnetic resonance is a non-invasive procedure that involves the patient being placed in a narrow cylinder. The MRI image is a visual reconstruction of the different concentrations of water molecules in cells; the shades of grey seen in MRI scans represent the different concentrations. How the scanner does all this is complicated. MRI permits a structural analysis of the brain: the location, shape, and size of subregions.
Structural MRI scans have been used in studies of ADHD to determine the size of different brain regions. Although the differences that have been found are small, they are statistically significant. Of course what that then means in terms of clinical significance is another question.
Functional MRI is similar in method to that of structural MRI. However, fMRI further utilizes the fact that busy parts of the brain have increased oxygen containing hemoglobin in the red blood cells. By using this feature, the scanner can detect the differences in oxygen content, and thus activity of the brain. The images have regions of activity colored in, with highly active regions of the brain being colured in the red–yellow spectrum (these are often referred to as hot spots). Such images allow scientists to determine which part of the brain is being used for a particular task.
MRS looks at particular individual chemicals that can be differentiated by the scanner. However, only a few chemicals can be detected using this technique, and this limits its utility. It works in a similar manner to MRI, but is selective in detecting particular cell nuclei. Very few studies have been done using this technique, and this is most likely due to the fact that dopamine, the main chemical studied in ADHD, cannot be pinpointed and measured directly. Studies that have used the technique have focused on other chemicals, e.g. glutamate [656]. But a common trend has been an association with the fronto-striatal circuits (see below) [105].
Many imaging studies have been conducted in ADHD, but the choice of the task that is being performed is even more important than the scanning technology; as is often stated “junk in, junk out” (see [657] for review). One has to careful not to be seduced by the colorful images and the facts they show. Imaging studies have come under a lot of criticism recently [106] and one should be cautious in overestimating their importance. Adolph and colleagues [658] have also criticized the time of measuring a phenomenon typically used by developmental researchers, and suggest it may be inadequate to accurately depict the pattern of developmental changes. Thus it would appear we have inaccurate knowledge about normal development, let alone the atypical development seen in ADHD.
Nuclear imaging requires the administration of a radioactive tracer that will be detected by the scanner. Owing to the inherent danger of radiation, nuclear imaging techniques are seldom used in children. Positron emission tomography (PET) and single photon emission computed tomography (SPECT) use low doses of radiation which are relatively safe, but it is inadvisable to use these in certain populations. PET and SPECT are valuable tools in understanding neural activity. They are able to detect specific molecules in the brain – i.e. those that are specified by the chemical to which the radioactive isotope is attached. For example, a drug such as methylphenidate can be made radioactive with an [11C] radioisotope, thus [11C]- methylphenidate (if you see a prefix such as [11C] or [3H] or [123I] prior to a chemical name, this usually means it has been made radioactive). The radioactivity can be then visualized and measured by the scanner (e.g. [659]). A range of chemicals can be traced in small concentrations; thus these techniques are open to measuring specific neurotransmitter systems. The radioactive information can be assembled into a visual image of the brain with “hot spots” of activity. Such techniques have been used in understanding the dopamine system with a great deal of success, but of course they are limited somewhat in childhood ADHD.
The Brain in ADHD
The rise of ADHD, as we have seen in chapter 2, evolved from the use of minimal brain damage and minimal brain dysfunction as terms that were once used. In the days when such terms were used, there was no such thing as neuroimaging and therefore brain damage could not be assessed but rather was inferred from behavior. More recent studies have not necessarily looked for brain damage, but instead looked for differences – sometimes very small and subtle differences. In ADHD research, numerous studies have taken full advantage of modern imaging techniques. Some have looked at structural changes; others have looked at the brain’s activity during specific tasks; whilst still others have mapped the effects of dopamine and methylphenidate.
Structural Changes
Assessments of general brain volume have found reductions in ADHD patients (e.g. [660]). Recent meta-analyses found that there was a statistically significant reduction in both males and females with ADHD [661–662], an effect which was not confounded by medication effects, according to Krain and Castellanos [663]. The effects of medication may well be minimal when looking at global scores. However, when specific regions of the brain are looked at, e.g. the right anterior cingulate cortex [664], medication appears to have an effect.
These studies indicate that the brain in ADHD is on the whole a little smaller than age- and sex-matched controls. A number of studies have looked more closely at specific brain regions and brain composition in ADHD. These studies have examined both structural and sometimes functional correlates, e.g. behavioral inhibition tasks [665]. Such studies are somewhat more informative than those concerned with global changes in brain volume; after all, there is a great deal of variability in brain size across individuals, and what, for example, a 3.4 percent reduction [661] translates to clinically is uncertain.
Gray and White Matter
A number of studies have assessed the neural composition of those with ADHD in greater detail. These studies looked at the gray and white matter volume in those with ADHD. Gray matter refers to the neurons’ cell body, dendrites, and unmyelinated axons as well as glial cells and capillaries (see Figure 7.1). White matter, in contrast, describes the physical appearance of myelinated axons. Both gray and white matter change over the lifespan (see [663]). It is therefore important to have proper age-matched controls when looking at comparison with ADHD. The studies to date indicate that there is a reduction in both gray and white matter in ADHD, especially in the prefrontal cortex [666–670]. In contrast Sowell et al. [671] found increases in white and gray matter in other cortical regions. A meta-analysis of studies indicated that increases occurred in four studies but without a regional differentiation [672].
The regions that did stand out in ADHD were right putamen/globus pallidus – subcortical regions with a decrease in gray matter [672]. An area that has been highlighted as having a marked reduction of white matter is the corpus callosum (e.g. [673]). What is the significance of all of this work? The reason it is interesting is that these areas are all connected, most notably by dopamine, and therefore deficits in white and gray matter may be indicative of a hypofunctional dopamine system [672].
The Frontal Lobes
Moving on to specific regions of the brain, numerous imaging studies have looked at cortical and subcortical structures. The neuropsychological literature points to a dysfunction in the cortex, and most notably the frontal lobe (see chapter 4). The cortex of those with ADHD has been shown to be abnormal, with reductions in cortical volume and folds within the cortex [674–675]. The frontal lobe was seen to be the only significantly different area to be reduced in ADHD when there was an average cerebral reduction of 8.3 percent [669]. The frontal lobes can be divided into further subregions, and when doing so one area stands out as reduced in ADHD: the prefrontal cortex (PFC), especially on the right side of the brain (see [663]). However, others more recently have found reduction in prefrontal cortical regions on the left side of the brain [676]. Another region, the anterior cingulate cortex, is also of interest in ADHD, and has been shown to have an approximately 22 percent reduction in volume among adults [677]. Regional changes that are seen in children are also seen in adults, which some have argued is evidence in support of the claim that ADHD is a valid disorder (e.g. [678]).
The idea that in ADHD there is a delay in brain maturation has received comment [174, 679], whereas others see it as a distinct deviation from typical neural architecture [680]. Shaw et al. [681–682] observed that cortical maturation followed the same pattern in ADHD and controls but was delayed in ADHD.
The Basal Ganglia
Moving deeper into the brain and intimately connected to the frontal lobes are the structures that make up the basal ganglia. These areas have received considerable attention. The reason for this is partly based on the psychopharmacology in which methylphenidate is thought to act. The basal ganglia have been argued to be smaller in ADHD [683]. Looking at the striatum and the subregion called the caudate, numerous studies have found conflicting evidence for changes in ADHD [663], although the most recent meta-analysis identified the caudate as a region of interest [684]. A study by Silk et al. [685] found that the development that is normally seen in the caudate between the ages of 8 and 18 years was delayed in those with ADHD. However, a study looking at youths with a history of ADHD suggests that right caudate was larger in the ADHD sample compared with the controls [686]. Clearly such youths will have had a mixed history of medication/interventions, but as far as the caudate goes, an imaging study found no difference between those who were treatment-naïve and those who had had medication [664].
Whereas the caudate is more frequently associated with cognitive functioning, the putamen is associated with the physical motor symptoms of ADHD. Again the data are conflicting, making conclusions hard to draw [663]. More recent studies have not cleared the picture up, with one study showing a difference in the anterior putamen [683] and another showing a similar pattern of development to controls [685]. Dividing the caudate up further into head and body revealed small differences between ADHD and control groups when overall there was no difference in volume [687]. In adults who had not received medication for more than one month it was also shown that DA activity was reduced in the caudate and associated with inattention [688]. However, there may still be residual medication effects even after one month.
The Cerebellum
The cerebellum, like the putamen, is associated with movement, but it is also associated with cognitive functioning [663, 689]. MRI studies indicate that a smaller volume of tissue in this are is associated with ADHD [690–691] and linked to the DRD4 7R genotype [692]. This latter study demonstrates how the gap between gene and disorder is been bridged by looking at intermediate neuropathological differences. The cerebellum can also be broken down into subcomponents, and the cerebellar vermis is particularly associated with ADHD [693] and is normalized by treatment [694].
Other areas of the brain have been found to be different in those with ADHD, such as the hippocampus and amygdala [695–696]. How these areas, and more besides, can be integrated into a neurological account of ADHD remains to be seen. Most authors of imaging studies conclude that there are problems in multiple circuits, but most notably the fronto-striatal circuit.
Functional Significance
The structural studies are all well and good (or not!), but what do they tell us? They tell us that a region is bigger or smaller in ADHD. That is it! What this means clinically or functionally is an academic pursuit. Structural studies are good at identifying areas and quantifying them, but our functional understanding of the brain in disorders such as ADHD needs to be assessed; then again, it needs to be assessed in normal populations as well!
An understanding of how structural changes are converted into functional significance has been attempted. Numerous studies have linked the above regions with symptoms’ severity and test scores on rating scales and neuropsychological tests [663].
Functional Imaging of ADHD
The previous studies demonstrated structural changes, which could be correlated with measures of ADHD. With the introduction of functional imaging technologies, the activity, and not just the structure, of the brain could be investigated. It is a case of looking at what you do with your brain and not the size of it!
Early studies using SPECT and PET technology found mixed results across ages (see [697]). This is in part due to differences in methodology [104]. The effect of treatment has been questioned in a number of studies since the effects of methylphenidate have different outcomes depending on the dosage regime used (acute or chronic) [104].
Using fMRI, the anterior cingulate cortex (ACC) has been demonstrated by many to be dysfunctional in ADHD, especially when using tasks such as the Go/No-go [105, 698].
In the striatum, lower levels of activity were seen in ADHD [679, 699–701]. However, in the lateral frontal cortices, reliable and stable differences have not been found [105]. All these effects seen in functional imaging studies are interesting, but they are also limited to the tasks that have been used to activate the regions of the brain, and also task parameters that when modified can change neural activity [699].
The compartmentalization of regions of the brain in such studies may give rise to the notion that there is a brain region that serves a particular function. The truth is more complex, and most authors argue that there is a deficit in the fronto-striatal neurocircuitry in ADHD (e.g. [702]). Many researchers have taken the idea of behavioral inhibition and looked for differences in neural processing in normal controls and those with ADHD. Such studies typically find reduced activation in such tasks as the Go/No-go task [703] and the SSRT [704]. The argument about the contributory role of working memory in behavioral inhibition could be resolved to some extent by imaging studies in which “response [behavioral] inhibition and working memory impairments in ADHD may stem from a common pathologic process rather than being distinct deficits” [403] (p. 1395].
On the whole, the low numbers of individuals used in imaging studies make it difficult to generalize findings. A sample of 10–20 people is hardly representative of 5 percent of the pediatric population. A serious criticism of imaging studies, which can join the permanent one about diagnostic accuracy, is that they often have medication as a confounding variable. Drugs such as methylphenidate can have long-lasting effects on the structure and function of the brain [705]. Numerous animal studies have shown neural changes in response to medications such as antipsychotics and psychostimulants that block dopamine receptors or stimulate dopamine, respectively [706–710], which fits with our pharmacological understanding of up- and down-regulation, i.e. an increase or decrease in the number of receptors for that neurochemical [711], and one has to be careful that one is not in fact measuring that in neuroimaging studies.
The imaging world has recently been criticized from within, where high-profile journals have been shown to publish imaging studies that are guilty of statistical crimes [106].1 The technology of imaging is as much dependent on statistical analysis as any other type of study. The extent to which such practices are involved in the ADHD research is uncertain, but it does highlight the need to look closely at what people are doing.
Psychophysiological Studies
Although not strictly neuroimaging, measuring the electrical activity via surface electrodes placed on the scalp has one distinct advantage over magnetic or nuclear imaging: that is, the temporal resolution is excellent. Scans take a measure over a relatively long period, whereas psychophysiology can deal with changes measured in milliseconds. However, the spatial resolution of psychophysiological imaging is not as good as other imaging technologies.
Psychophysiological studies are essentially measuring the action potentials generated in the brain (see chapter 7). The two types of studies that are frequently used are EEG (electroencephalogram) and ERPs (event-related potentials). The former measure general activity whereas the later measure activity in response to a stimulus or action. EEG studies have generally found differences in cortical activity in ADHD [509–511, 680, 712]. Such studies have claimed to be able to differentiate between subtypes [510] and potential positive response to treatment [713]; however, it would probably be cheaper to give a child a short-acting dose and observe what happened for the next four hours! The fact that there is general cortical under-arousal in ADHD [714] somewhat supports Mark Rapport’s [519] view on working memory deficit and hyperactivity (see chapter 4).
EEG is about measuring activity during resting states – but of course the brain is never really at rest! ERP studies look at responses to tasks or stimuli. Such studies have found differences in ADHD groups, with a slowing during EF tasks [715].
Ultimately the general view is that there is a dysfunctional fronto-striatal circuit in ADHD which corroborates the neuroimaging data, although subcortical regions are beyond the electrodes’ reach. A review of the data on imaging and psychophysiology summed up with a prediction that, in future, combining the two measures will open up the understanding of processing and location in ADHD more reliably [716].
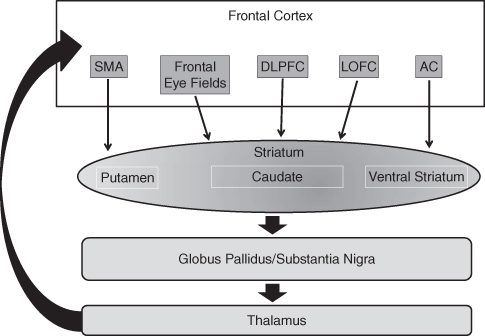
The Fronto-Striatal Circuits
“Fronto-striatal” is a general term for the numerous circuits that link the frontal cortex and the striatum. Bradshaw [702] has identified five circuits: (1) the motor circuit (supplementary motor area, SMA), (2) the oculomotor circuit (frontal eye fields), (3) the dorsolateral prefrontal cortical circuit (DLPFC), (4) the lateral orbitofrontal cortical circuit (LOFC), and (5) the anterior cingulate circuit (AC) (see Figure 6.4). All have been implicated in ADHD, with the latter four being associated with pervasive cognitive dysfunction [678, 717–719]. The differing effects of dysfunction in each circuit may contribute to the heterogeneous nature of ADHD: different severities in the anterior cingulate may reflect more on inhibition, whereas the oculomotor circuit may malfunction in preparing to make a response.
Figure 6.4 The regions of the frontal cortex communicate with striatal regions, which go on to communicate with other regions of the basal ganglia and the thalamus (see text for details)
Summary
Imaging studies have indicated that the brains of those with ADHD differ from typically developing controls or adults. The studies that have demonstrated such differences generally use small numbers. This means that diagnosis is extremely important in the imaging process, along with other variables such as age and sex. When a study finds a difference, it is often small but statistically significant. The imaging studies have yet to determine if the differences in the brain are of clinical importance. There are many differences in people’s brains: some can function with large regions destroyed, and again some variables can mitigate the damage, e.g. age at trauma, treatment, and region of the brain affected.
I was somewhat surprised when I started writing this chapter that imaging studies actually did not tell me as much as I thought they would. I thought there would be many studies and that this chapter would be long. In fact when I look at the academic textbooks on neuroimaging in ADHD, they are often the shortest in the book. This is not because the results are unequivocal! The data are complex and varied. The scarcity of solid studies may in part be due to the relatively recent birth of fMRI and other imaging tools. However, it is noteworthy that the studies offer little in the way of a conclusion about the neural processing deficits in ADHD. The closest one gets to a conclusion is that there is a reduction in volume and function of the frontal lobe and the knock-on effects within the frontal-subcortical neurocircuitry.
One has to be careful not to be seduced by this technology and what it offers. As I have stated several times, imaging studies are of little use in the diagnostic process, but with increased resolution and further research this may change one day.
Again Lyall Watson’s comment springs to mind, “If the brain were so simple we could understand it, we would be so simple we couldn’t.” Clearly there is a challenging time ahead!
Note
1 For the brave of heart, papers can be obtained from http://www.edvul.com/publications.php.