CHAPTER 1
History of Dermatology
Nick J. Levell
Norwich Medical School, Norfolk and Norwich University Hospital, Norwich, UK
Introduction: when did dermatology history begin?
The history of dermatology is the history of mankind. Failure to care for the skin increases the risk of skin infections leading to morbidity and disability, and caring for the skin improves the chances of being perceived as being attractive to others thereby enhancing survival of an individual's genes. Primates demonstrate mutual grooming behaviour to reduce infestation and many species lick their wounds. Dermatology activity, removing parasites, applying grease to dry skin and cleaning and dressing wounds and burns, must have been an important role for the Shamans and Wise Women who were responsible for medical care in primitive hominid tribal groups.
Prior to the invention of writing, archaeologists provide evidence of disease and early medical activity. Findings, such as the radiological appearances of possible metastatic melanoma in 2400-year-old pre-Colombian Inca mummies, provide early evidence of the impact of skin disease [1].
The invention of writing coincided with early cities in Africa (Egypt c. 3100 BC), the Middle East (Mesopotamia c. 3000 BC), India (Indus valley c. 2500 BC), Europe (Crete c. 1800 BC) and China (Shang c. 1400 BC). Early texts were mainly for administrative or religious purposes, but medical writings soon appeared. Many of these related to skin disorders.
Ancient dermatology writings
The first medical texts
Medical writings between c. 3000 BC and 400 BC in most cultures had a theoretical basis founded on religious beliefs with pragmatic practical tips. Historians have often stated that there was an initial age of medicine dominated by magic, followed by the growth of rational medicine led by Hippocrates around 400 BC. However the reality was probably not so clear-cut. Experience makes it obvious that doctors who relied totally on magic and religion would not have cured many patients, so all systems of health care contained practical measures.
A pharmacopoea, written by an unknown Sumerian (Mesopotamia in the Middle East) in the third millienium BC may be the earliest medical writing [1]. It is on a clay tablet and describes a selection of external salves comprising cedar oil, wine and botanical, mineral and animal materials. Other preparations include clay mixed with honey, water and oil.
Medical writing moved from clay tablets, to papyrus to paper and now in the 21st century is moving back to tablets of a different type.
Ancient Egypt
Imhotep, the Chief Vizier to the Pharaoh Zoser (2700 BC), was renowned as a physician and was soon deified by the Egyptians (Figure 1.1). Egyptian medical writings date from a millennium later. The Edwin Smith Papyrus (c. 1600 BC) known as the ‘Book of Wounds’ mentions wound dressings using fresh meat and then honey, grease and lint. However, the most important medical text is the Ebers Papyrus (1550 BC) written on over 20 metres of papyrus [2]. This describes 700 magical formulae and 800 formulae to treat 15 diseases of the abdomen, 29 of the eyes and 18 of the skin. The text includes a baldness cure: a drink made from black ass testicles, or vulval and penis extracts from a black lizard. The Ebers Papyrus also describes an effective treatment for the Guinea worm: wrap the emerging end of the worm around a stick and slowly pull it out.

Figure 1.1 Imhotep, seated on the right with a surgical instrument.
Mesopotamia
Over 1000 clay tablets that refer to medicine, of which 40 comprise a medical diagnostic handbook, and written c. 1000 BC, are attributed Esagil-kin-apli, a Babylonian physician. The writings on skin disease demonstrate the interplay of magic and empricisim [3]:
- Tablet 9, line 48: ‘If his face is covered in white boils: Hand of the Sun God Ama, he will survive …’.
- Tablet 9, line 49: ‘If his face is covered in black boils: Hand of the God I tar, he will die …’.
- Table 14, line 128: ‘If his testicles are black he will die …’ (possibly the first description of Fournier gangrene).
Ancient Greece
Asclepius is thought to have practiced about 1000 BC in Greece. The reality of his work is lost in stories around his deification. Greek legend confuses him with the Egyptian God/physician Imhotep and also describes him as a son of the God Apollo (the healer) and the Goddess Panacea. Ascelpius is said to have been executed by the gods for taking gold to raise the dead, a lesson for all modern clinicians tempted by greed. Temples to Asclepius included healing dogs to lick wounds. His followers in Greece persisted for centuries and included Hippocrates and Aristotle.
Ancient India
Early Brahmana (hereditary priests) guarded the Sanskrit religious teachings, the Veda (knowledge) from 1500 BC. Much of the medicine revolved around a magico-religious approach that paralleled that of Mesopotamia and Egypt. Vedic rites probably involved human sacrifice but writings included information on practical dermatology such as the use of cautery for haemostasis.
Growth of rational medicine
The Silk Road: the pathway of rational medicine
The trading routes known as the Silk Road linked China, India, the Middle East and eastern Europe c. 400 BC. At around this time, a growth of rational medicine appeared in Europe along with similar ideas in south India and China so it seems likely that a flow of medical ideas took place in parallel with the trade items. It can be argued whether knowledge flowed mainly from East to West or from West to East. The ‘Diagnostic Handbook’ from Mesopotamia, from 1000 BC, remained in print but between 600 and 400 BC changed radically in nature to show that disease was subject to the forces of nature and originated from the body rather than being of a divine nature.
China
Existing texts date back to at least 200 BC but some people contend that they originate over 2000 years before. Some of the original formulae are thought to still be in use today. Although there is little relationship to what western medicine considers to be an anatomical- or physiological-based system, the underlying concepts were not based on religion or spirits. Disease is seen to be based on a loss of harmony of the yin/yang system upsetting the qi (energy) and the meridians [1]. This is a generalist approach: skin disorders are considered to be an internal problem. Sections on skin disease exist in classic works from 652 BC. Urticaria or ‘wind type concealed rash’ was considered to be due to excess lesser yin causing fluid obstruction in the skin. The ‘Yellow Emperor's Inner Canon’ describes urticaria and eczema.
South Indian early Buddhism
The Pali scripts date back to around 400 BC and describe the work of the Buddha [2]. The Girimananda Sutra described dermatology nursing, psychodermatology, occlusion therapy for foot eczema and possible early descriptions of skin diseases including leprosy, boils/abscesses, scrofula, ringworm, scabies, pustular eruptions, plethora, fistula and sexually transmitted diseases.
The Holy Bible
The Book of Leviticus written c. 450 BC gave an account of how to diagnose ‘leprosy’ – although the descriptions of skin disease in this text could include many chronic cutaneous infections including tinea infection, impetigo and infected eczema. Practical tips on the management of contagious cutaneous disease include burning clothes and isolation of those afflicted.
Greeks: the rational age
Hippocrates (c. 400 BC) was known to his contemporaries as Hippocrates the Great – an accolade in the age of Plato and Socrates. He was an Asclepian physician and teacher on the island of Cos. Some of his great ideas may have been written by his pupils who built up a body of medical knowledge at his school over later generations. Hippocrates’ school moved away from the magical and religious approach to medicine and adopted a method based on logic and reason. His approach was, like the Chinese, to see disease in the context of the whole patient and to see people as physical entities subject to the same laws of nature as the world. He used diet and exercise as therapies and adopted an expectant approach, not rushing to intervene. His writings on leg ulcers are relevant now: ‘In the case of an ulcer, it is not expedient to stand; more especially if the ulcer be situated in the leg; but neither, also, is it proper to sit or walk. But quiet and rest are particularly expedient …’.
The Roman Empire
Galen was born in Pergamon, Turkey in 120 AD and travelled to Egypt to learn about African and Indian medicine prior to settling in Rome. He studied anatomy through the dissection of animals (not humans), but then set Hippocratic ideas into an incorrect anatomical and physiological framework. This was based on four humours that might lead to fever if in excess: yellow bile, black bile, phlegm and blood. This led to an enthusiasm for blood-letting to restore balance in those with fever or if the physician wished to prevent fever.
Galen had a powerful intellect, an overbearing personality and a gift for self-publicity and was a prolific writer. Consequently, perhaps, this theoretical basis for medicine became entrenched in Europe and the Middle East. A period of relative intellectual stagnation regarding underlying disease processes persisted for over 1500 years. This may have been partly due to religious and cultural bans on human dissection until Renaissance times.
Over the next 500 years a series of Greek and Roman writers defined diseases within this flawed model of basic science. Therapeutic advances were made with various herbal and mineral remedies for skin disorders. Wood tars and coal tars were described for inflammatory skin disorders, presumably eczema and psoriasis [3]. The last of the series of Greco-Roman authors was Paul of Aegina (around 700 AD) who wrote a medical encyclopaedia in seven books of which book IV concerns skin disease [4]. This may be considered the earliest dermatology textbook.
Dermatology after the fall of Rome
Early Islamic medicine and dermatology
With the failure of the Roman Empire and the onset of the Dark Ages in Europe, the baton of medical knowledge in the West was passed back to the Middle East. Much would have been lost were it not for translations into Arabic by Christian and Islamic scholars at the Bayt al Hikma centre set up in 832 in Baghdad, the capital of the Islamic Empire. Hundreds of Greek, Latin and Sanskrit texts were translated, making Islamic culture the centre for learning. A series of medical compendia were produced, the first being the ‘Paradise of Wisdom’ (Firdaws al-bikma) by Ali ibn Rabban al-Tabari (c. 850 AD).
The great Persian physician, Muhammad ibn Zakariya al-Razi (865–925; known as ‘Rhazes’ in the West) studied in Rayy near Tehran, before settling in Baghdad. He wrote over 200 texts and initially challenged many of Galen's precepts – although ultimately describing himself as a Galen's disciple. He wrote al-Jadari wa'l-basha (‘Smallpox and Measles’) in which he was the first to distinguish between febrile exanthemas: ‘The rash of measles usually appears at once, but the rash of smallpox spot after spot’. Al-Razi's work was renowned in the Arabic world and was translated to Latin, still being reprinted in the West in 1542, over 600 years after his death.
The Persian writers, al-Majusi (Haly Abbas: 10th century), Ibn Sina (Avicenna: 980–1037) and al-Zahrawi (Albucasis: 936–1013) all wrote influential medical texts.
Italy during the European Renaissance
In the mid-16th century Europe was slowly struggling out of the religious superstition that characterized the Dark Ages and Middle Ages. A group of brilliant doctors in Padua, including Vesalius and Mercurialis (Geronimo Mercuriale), set up a system of learning and wrote medical texts that revitalized medicine in Europe. Mercurialis wrote De Morbis Cutaneis in 1572: this summarized work of earlier writers and had a focus on hair disorders, but still represents the first dermatology textbook in the West since the time of Paul of Aegina, 800 years before.
European Enlightenment
A series of dermatology textbooks written in the 18th century pulled dermatology through to the beginning of the modern age.
Daniel Turner (Figure 1.2) wrote the first English language dermatology textbook in 1712 [1] (Figure 1.3). This was a series of case reports and was popular, running to four editions over 20 years. Turner was an English surgeon, who aspired to be a physician, and he dedicated this book to the President of the London Royal College of Physicians. He was awarded association to the Royal College as a ‘Licentiate’, but a medical degree from Oxford or Cambridge was required to be a full member. Turner then endowed a medical library at Yale University in America and was given the first medical degree awarded in America, but this distinction still failed to achieve his college membership.

Figure 1.2 Daniel Turner. (From http://wellcomeimages.org/. Copyrighted work available under Creative Commons Attribution only licence CC BY 4.0 http://creativecommons.org/licenses/by/4.0/. Wellcome Library, London.)

Figure 1.3 The first English language dermatology textbook by Turner. (From http://wellcomeimages.org/. Copyrighted work available under Creative Commons Attribution only licence CC BY 4.0 http://creativecommons.org/licenses/by/4.0/. Wellcome Library, London.)
Dermatology was linked with venereology in Europe, and Jean Astruc, physician to the Parisian Court, wrote a definitive text summarizing all knowledge on syphilis. He described the anatomy of the skin and linked cutaneous diseases to the sebaceous glands.
In Italy, Bernadino Ramazzini wrote a textbook on industrial disease in 1700, which classified occupational dermatoses ranging from varicose veins in priests to syphilis in midwives and wet nurses [2].
Classification was in the air: following Linnaeus, clinicians across Europe strove to classify cutaneous disease. Joseph Jacob Plenck, a Viennese-born professor in Buda, wrote a classification of skin disease in 1776 that divided skin disease into 14 categories [3]. This was a landmark for dermatology, being the first serious attempt to classify skin diseases. The following year, Antoine Charles Lorry in France wrote a text that considered the pathology, physiology and aetiology of skin diseases [4].
Growth of scientific dermatology
Willan and Bateman: definition of skin diseases
Prior to Robert Willan, terms were used loosely to describe skin diseases. Two doctors might use the same descriptive term to mean different appearances. Attempts to describe disease characteristics in classifications were ambiguous. Willan (Figure 1.4) defined precisely the terms used to describe skin disease. He wrote a classification based on these definitions, first published in Breslau from 1798 onwards [1] (Figure 1.5). He died before finishing his next work, but it was completed by his friend and student, Thomas Bateman in 1813. Bateman's A Practical Synopsis of Cutaneous Disease was translated into the main European languages and remained the standard textbook until the 1830s [2].
Figure 1.4 Robert Willan. (From http://wellcomeimages.org/. Copyrighted work available under Creative Commons Attribution only licence CC BY 4.0 http://creativecommons.org/licenses/by/4.0/. Wellcome Library, London.)
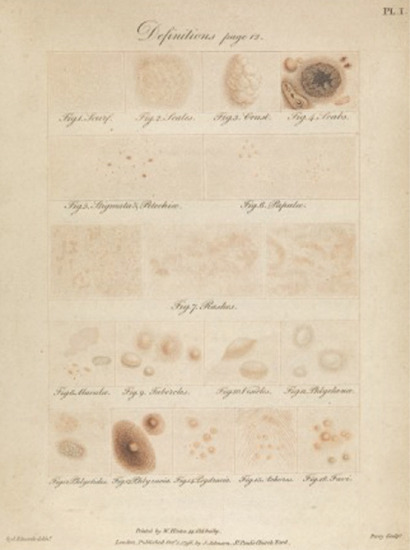
Figure 1.5 Willan's definitions. (From http://wellcomeimages.org/. Copyrighted work available under Creative Commons Attribution only licence CC BY 4.0 http://creativecommons.org/licenses/by/4.0/. Wellcome Library, London.)
Willan produced images of skin diseases in his textbook (Figure 1.6), the first dermatology atlas, that was completed by Bateman in 1817 [3]. This atlas went through many editions and was still in print in 1877.
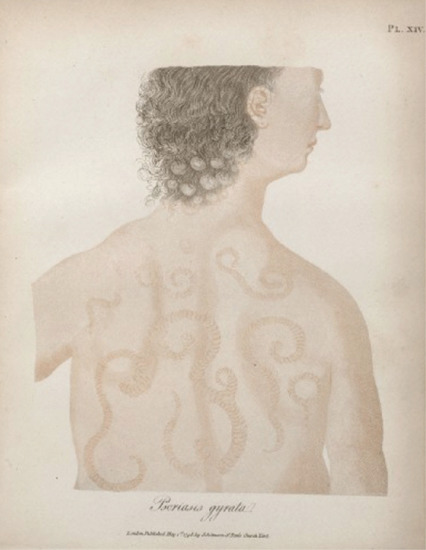
Figure 1.6 Psoriasis gyrata in Willan's textbook. (From http://wellcomeimages.org/. Copyrighted work available under Creative Commons Attribution only licence CC BY 4.0 http://creativecommons.org/licenses/by/4.0/. Wellcome Library, London.)
Willan and Bateman changed the way dermatology was practised, with followers all around Europe: Biett and Cazenave in France, Chiarugi in Florence, Alfaro in Spain and Klaatch and Schreiver in Germany.
L'Hôpital St Louis, Paris: the first skin hospital
The time of war in Napoleonic Europe not only produced a great step forwards in England, but also led to the encouragement of science in France. In 1801 the L'Hôpital St Louis became a dermatology hospital under the leadership of Jean-Louis Alibert (Figure 1.7). His flamboyant personality, prolific writing and elegant descriptions and atlases included the famous ‘arbre des dermatoses’ classification (Figures 1.8 and 1.9). He was balanced by the scholarly Laurent Biett, his student, who studied under Bateman in 1816 and brought Willanism to France. Biett then further developed and refined this work with Cazenave, Rayer and Bazin, making France and L'Hôpital St Louis the leading centre for dermatology in the early 19th century.

Figure 1.7 Jean Louis Alibert. (From http://wellcomeimages.org/. Copyrighted work available under Creative Commons Attribution only licence CC BY 4.0 http://creativecommons.org/licenses/by/4.0/. Wellcome Library, London.)

Figure 1.8 Alibert's syphilide pustuleuse en grappe. (From http://wellcomeimages.org/. Copyrighted work available under Creative Commons Attribution only licence CC BY 4.0 http://creativecommons.org/licenses/by/4.0/. Wellcome Library, London.)
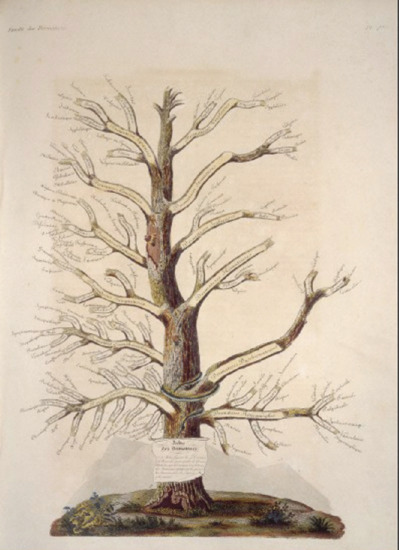
Figure 1.9 Alibert's arbre des dermatoses. (From http://wellcomeimages.org/. Copyrighted work available under Creative Commons Attribution only licence CC BY 4.0 http://creativecommons.org/licenses/by/4.0/. Wellcome Library, London.)
Natural Sciences and the German-speaking Europeans
The integration between hospitals and universities was pioneered by German-speaking countries in central Europe in the second half of the 19th century. The new sciences of bacteriology and histopathology led to the understanding of underlying disease processes in dermatology. This finally ended Galen's ancient teachings and marked the origin of modern scientific dermatology.
In Vienna, Austria, the Allgemeines Krankenhaus became the world centre for medical teaching. From a group of brilliant clinicians, Ferdinand von Hebra (Figure 1.10) arose to introduce the new science of pathology into dermatology. He reclassified skin diseases using an anatomical and pathological framework, defined cutaneous fungal infections, and made great contributions to the definitions of many inflammatory disorders including eczema. Many great dermatologists studied under him and took his methods across the world; including Filip Pick to Prague and Schwimmer to Budapest [4].
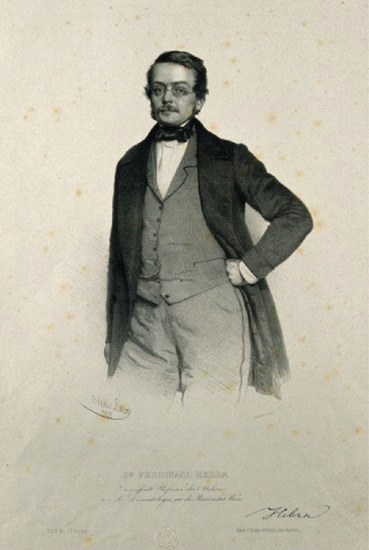
Figure 1.10 Ferdinand von Hebra. (From http://wellcomeimages.org/. Copyrighted work available under Creative Commons Attribution only licence CC BY 4.0 http://creativecommons.org/licenses/by/4.0/. Wellcome Library, London.)
Heinrich Köbner, and then Oscar Simon and Albert Neisser in Breslau (now Wrocław), developed the Allgemeines Krankenhaus as the centre for German and Polish dermatology. Köbner moved to Berlin in 1872 to set up the Berlin Dermatology Society. Neisser utilized his knowledge of histopathology, microbiology, immunology, X-rays and ultraviolet and by the age of 25 had discovered the gonococcus and worked with Hansen to stain the lepra bacillus. He became the pre-eminent figure in European dermatology with advances in many areas, including work with Wassermann in syphilis [5].
Britain in the late 19th century
Sir Erasmus Wilson (Figure 1.11) was the most famous Victorian dermatologist. A wealthy and charismatic surgeon, who founded a dermatology chair for himself at the Royal College of Surgeons, paid for Cleopatra's needle to be transported from Egypt to London, and founded and edited the first English dermatology journal in 1867, he was also responsible for abolishing flogging in the British Army. He co-founded the controversial St John's Hospital for dermatology in London, with John Laws Milton. Another co-founder, William Tilbury Fox, became the first British university hospital consultant, defined impetigo and wrote an early text describing skin disease in India.
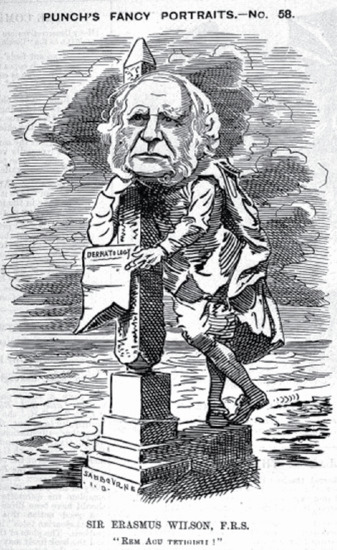
Figure 1.11 Erasmus Wilson. (From http://wellcomeimages.org/. Copyrighted work available under Creative Commons Attribution only licence CC BY 4.0 http://creativecommons.org/licenses/by/4.0/. Wellcome Library, London.)
Sir Jonathan Hutchinson was a polymath surgeon, ophthalmologist, neurologist and dermatologist who described signs in syphilis and a host of other dermatology conditions. He often renamed these, causing confusion when diseases had previously been named by others, for example the recurrent summer eruption of Hutchinson, previously described by Bazin as hydroa vacciniforme.
United States in the 19th century
Henry D. Bulkley studied under Cazenave and Biett in France, and then returned to New York City to set up the Broome Street Infirmary for Diseases of the Skin in 1837 with John Watson. He translated Cazenave into English and was the first President of the New York Dermatology Society in 1869 – the first dermatology society in the world. Noah Worcester was influenced by Willan and Bateman to write Diseases of the Skin, the first American dermatology textbook in 1845.
Faneuil Weisse studied under Sir Erasmus Wilson in Britain, and then helped establish the New York Dermatology Society when working as lecturer on skin disease at the University of New York City from 1865. In 1871 James White, a student of von Hebra, was appointed to the new chair of dermatology at Harvard, after lecturing for 8 years at the medical school, then practising at Massachusetts General. White was a strong force in developing American dermatology and medical education at Harvard and was president of the Massachusetts Medical Society.
Louis Duhring (Figure 1.12), another student of von Hebra, occupied the first chair of dermatology at the University of Pennsylvania from 1875 for 35 years. He had also studied in Paris and London, influencing his vision of dermatology as a part of general medicine. Duhring's book, A Practical Treatise on Diseases of the Skin, and work on dermatitis herpetiformis, together with great wealth and benefactions to the specialty, helped establish dermatology in the United States.
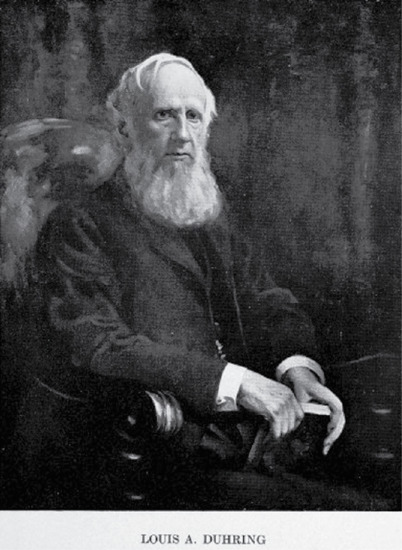
Figure 1.12 Louis Duhring. (From http://wellcomeimages.org/. Copyrighted work available under Creative Commons Attribution only licence CC BY 4.0 http://creativecommons.org/licenses/by/4.0/. Wellcome Library, London.)
Development of dermatology as a world specialty in the 20th century
At the beginning of the 20th century, dermatology was developing in most European and North American countries with fledgling dermatology societies and dermatology journals. The work often crossed national boundaries. From this point on we can consider the development of dermatology as a world specialty, considering the growth of subspecialty areas and science. The early 20th century saw the conquest of infections that had ravaged mankind for centuries and the development of effective treatments for inflammatory diseases. This, together with public health initiatives, led to great increases in longevity. The later 20th century saw skin surgery develop to deal with the skin cancers that arose in an ageing population, and the birth of molecular genetics that promises an even greater revolution in redefining diseases and predicting responses to treatment in a future era of personalized medicine.
Skin infections
Paul Ehrlich from Germany and Sarachiro Sata from Japan, working with Paul Uhlenhuth in Frankfurt, developed arsphenamine in 1910, Ehrlich's silver bullet, which offered effective chemotherapy for syphilis. This remained a mainstay of treatment until Alexander Fleming, in London, by serendipity discovered penicillin in 1928. This was produced commercially after its first synthesis by Florey, Heatley and Chain in Oxford and provided a cure for syphilis and many other cutaneous infections in the 1940s.
Leprosy has been a misdiagnosed, stigmatizing and confused condition since biblical times. It is likely that many cases who were excluded from society in all ages of mankind actually suffered from other skin diseases. Norwegian Gerhard Hansen together with Neisser in Breslau, described the bacterium between 1873 and 1880. Promin, a sulfone drug, was introduced in 1941; R. G. Cochrane then introduced dapsone in 1950 following research in Carville, Louisiana. Research in Malta resulted in multidrug therapy in the 1970s, which was then adopted by the World Health Organization in 1981 and since has led to the reduction or eradication of the disease in many countries.
Inflammatory disease and immunomodulatory treatments
The discovery of corticosteroids revolutionized dermatology in the middle of the 20th century [1]. Further drugs that modified the immune system and that were introduced later in the 20th century, such as azathioprine, methotrexate and ciclosporin, enabled the control of serious inflammatory diseases that had scourged humankind. Management of these disorders changed from long-term admissions to hospital into management as outpatients with potentially toxic systemic agents. Increasing knowledge of the molecular basis for diseases has led to more targeted and personalized treatment as dermatology moves into the 21st century.
Dermatology surgery
The practice of dermatology changed in the last three decades of the 20th century in Europe and North America due to the great increase in skin cancer in white-skinned populations. This has been paralleled by the growth in dermatology surgery. Dermatologists have developed the technique of Mohs micrographic surgery and have adopted many plastic surgery procedures such as flap and graft repairs [2]. Many innovations in skin surgery have been introduced by dermatologists as the number of practitioners has grown. Recent advances in the understanding of the mechanisms underlying basal cell carcinoma and melanoma has heralded new drugs offering medical treatments for skin cancers.
The adoption of skin surgical techniques by dermatologists, consumer demand and financial rewards have led to the growth of cosmetic dermatology in affluent societies since the end of the 20th century. Hair dyes, tattooing and other cosmetic procedures have been found in mummies from ancient Egypt, however the growth and spending on cosmetic products to adorn and preserve the skin has paralleled economic growth. The spending on fillers, muscle relaxants, cosmetic surgery and hair transplantation has provided a change in direction for some dermatologists.
Contact dermatitis and allergy
Industrial skin disease has been present since antiquity but patch testing was developed by Jadassohn in Breslau in 1895 [3]. Bloch in Basle and Zurich, Bonnevie in Copenhagen and Sulzberger in New York developed the technique and led its introduction across the world. In 1967 Niels Hjorth founded the International Contact Dermatitis Research Group, a group of clinicians from Europe and the United States (including Darrell Wilkinson, an original editor of this book), which standardized patch testing technique across the world.
Phototherapy
Niels Finsen's academic studies from 1894–7 on the value of ultraviolet light as a treatment for tuberculosis put phototherapy on a scientific basis [4]. However, the use of topical and oral plant extracts combined with sunlight was used over 3000 years ago in India and Egypt. Broad-band UVB was used until the development of psoralen and UVA (PUVA) in 1974. The initial enthusiasm for this treatment was tempered by caution when the first patients who were on maintenance treatment began to develop skin cancers. Intermittent phototherapy was introduced and the use of PUVA further declined when narrow-band UVB equipment became available from 1990. Extracorporeal photophoresis for cutaneous T-cell lymphoma was introduced in 1987 and in the 1990s photodynamic therapy was developed.
Genital dermatology
In most of the world dermatology and genito-urinary medicine have developed as the same specialty, whereas in the USA and UK they have become separate specialties since the mid-20th century. In these countries, male and female genital dermatology has developed as a subspecialty with increasing awareness of the disability and distress caused by genital disorders.
Psychodermatology and social medicine
Medicine and dermatology has changed its focus diametrically in the latter half of the 20th century. It has moved from being a process applied to passive patients to correct disease as perceived by doctors, to an engagement with an active patient who is encouraged to express their needs and wishes, which the medical team aims to fulfil. With this change has come an awareness of the morbidity that all disease, and skin disease in particular, has due to depression and anxiety. There has been a change in how to measure success in medicine. Disease outcome measures focus on the experience of the individual who is being treated and the effect that the treatment has on the patient's ability to function in their normal activities.
The subspecialty of psychodermatology has developed in recent years, usually by practitioners working closely with psychiatrists and psychologists.
Paediatric dermatology and genetics
A greater understanding of molecular genetics is revolutionizing the relatively new subspecialty of paediatric dermatology. Diseases that were originally described by appearance, phenotype, are now being defined by their genetic abnormalities. This understanding is allowing a reclassification of dermatology based on genetic abnormality, which will progress onto a new understanding of more complex inflammatory diseases and cancers associated with multiple genetic abnormalities. This will result in splitting up diseases and enabling personalized treatment, maximizing benefit and reducing the risks from new drugs targeting the precise molecular abnormality.
Dermatology has never been at a more exciting time in its history. Read on.
References
Introduction: when did dermatology history begin?
- Selby HM, Sherman RS, Pack GT. A roentgen study of bone metastases from melanoma. Radiology 1956;67(2):224–8.
Ancient dermatology writings
- Kramer SN. The first pharmacopoeia. In: History Begins at Sumer. Philadelphia: University of Pennsylvania Press, 1956:60–4
- Ebbell B, translator. The Papyrus Ebers: the Greatest Egyptian Medical Document. Copenhagen: Levin and Munksgaard, 1937.
- Heeβel NP. Diagnosis, divination and disease: towards an understanding of the rationale behind the Babylonian Diagnostic Handbook. In: Horstmanshoff HFJ, Stol M, Van Tilburg C, eds. Magic and Rationality in Ancient Near Eastern and Graeco-Roman Medicine. Boston: Brill Publishers, 2004:97–116.
Growth of rational medicine
- Tan EK, Millington GW, Levell NJ. Acupunture in dermatology: an historical perspective. Int J Dermatol 2009;48:648–52.
- Elangasinghe V, Lee KYC, Levell N. An historical account of dermatology from Buddhist Sri Lankan literature. Int J Dermatol 2014;53(3):390–2.
- Levell N, Peters T. Care and punishment: a history of coal tar and wood tar in dermatology. Br J Dermatol 2011;165:69.
- Adams F. The Seven Books of Paulus Aegineta: Translated from the Greek with a Commentary Embracing a Complete View of the Knowledge Possessed by the Greeks, Romans, and Arabians on All Subjects Connected with Medicine and Surgery. Sydenham Society, 1844.
Dermatology after the fall of Rome
- Turner D. De Morbis Cutaneis. London: Bonwicke, Walthor, Wilkin, Ward and Tooke, 1712.
- Ramazzini B. De Morbis Artificum Diatriba. Modena Typis Antonii Capponi, 1700.
- Plenck JJ. Doctrina De Morbis Cutaneis. Vienna: Graeffer, 1776.
- Lorry AC. Tractus De Morbis Cutaneis. Paris: P Cavelier, 1777.
Growth of scientific dermatology
- Willan R. On Cutaneous Diseases. London: Johnson, 1808.
- Bateman T. A Practical Synopsis of Cutaneous Disease. London: Longman, Rees, Orme, Brown and Green, 1813.
- Bateman T. Delineations of Cutaneous Diseases. London: Longman, Hurst, Rees, Orme and Brown, 1817.
- Pusey WMA. The History of Dermatology. Baltimore: Charles C Thomas, 1933.
- Bilianicki-Birula R. The 100th anniversary of the Wasserman–Neisser–Bruck reaction. Clin Dermatol 2008;26:79–81.
Development of dermatology as a world specialty in the 20th century
- Lamb JH, Lain ES, Keaty C, Hellbaum A. Steroid hormones: metabolic studies in dermatomyositis, lupus erythematosus and polymorphic light sensitive eruptions. Arch Derm Syphilol 1948;57(5):785–801.
- Mohs FE. Chemosurgical treatment of cancer of the nose: a microscopically controlled method. Arch Surg 1946;53:327–44.
- Adams R. Profiles of greats in contact dermatitis. Josef Jaddasohn (1863–1936). Am J Contact Dermatitis 1993;4:58–9.
- Honigsmann H. History of phototherapy in dermatology. Photochem Photobiol Sci 2013;12(1):16–21.