CHAPTER 86
Psychodermatology and Psychocutaneous Disease
Anthony Bewley1 and Ruth E. Taylor2
1Department of Dermatology, Barts Health NHS Trust, London; and Queen Mary College of Medicine, University of London, London, UK
2Department of Liaison Psychiatry, Barts Health NHS Trust, London; and Queen Mary College of Medicine, University of London, London, UK
Introduction
What is psychodermatology?
The links between the mind and the skin have long been recognized. The skin has been described as the mirror of the mind, and so it is not surprising that the interface between dermatology and psychiatry (’psychocutaneous medicine’ or ’psychodermatology’) is emerging as a specific subspeciality of dermatology. Psychodermatology is an increasingly recognized and important branch of dermatology. It encompasses disease that involves the complex interaction between the brain, the cutaneous nerves, the cutaneous immune system and the skin. Patients with psychocutaneous disease are often variably managed as dermatologists struggle, in general dermatology clinics, to meet the complex needs of these patients. Most patients with psychocutaneous disease are reluctant to attend purely psychiatric clinics. For these reasons, over the last few decades, the sub-specialty of psychodermatology has emerged to address the clinical–academic needs of this group of patients.
Skin–psyche interactions may be any of the following:
- Primarily cutaneous disorders that can be substantially influenced by psychological factors, e.g. psoriasis.
- Primary psychiatric disease presenting to dermatology health care professionals (HCPs), e.g. delusional infestation, body dysmorphic disorder.
- Psychiatric illness developing as a result of skin disease, e.g. depression, anxiety or both.
- Co-morbidity of skin disease with another psychiatric disorder, e.g. alcoholism.
Psychodermatology multidisciplinary teams
Though patients often present to the dermatology department, dermatologists will usually need the support of a variety of colleagues in managing patients with psychodermatological disease. For these patients, there is increasing evidence that a psychodermatology multidisciplinary team (MDT) can improve outcomes [1,2]. Specialists who make up a psychodermatology MDT (Box 86.1) require dedicated training in the management of patients with psychocutaneous disease. Such training is not always readily available, but national and international groups are now becoming pre-eminent in meeting the training needs of the psychodermatology MDT, as well as championing the clinical–academic development of the subspeciality (Box 86.2).
Models of provision of psychodermatology services
There are several models of how psychodermatology services are delivered, all of which are compatible with a psychodermatology MDT. These include:
- A dermatologist who refers to a psychiatrist or psychologist as a clinical adjacency.
- A dermatologist who refers to a psychiatrist or psychologist who is in a remote clinic (who will be able to support and supevise decisions taken by a dermatologist).
- A dermatologist who has a psychiatrist sitting in the clinic at the same time. Patients are seen by both specialists concurrently.
- A dermatologist who has a psychologist as a clinical adjacency (psychologists rarely sit in on clinics with dermatologists or psychiatrists).
Classification
Classification of psychodermatological disease is useful, but more complicated than it may first appear [1]. The American Psychiatric Association has published the Diagnostic and Statistical Manual of Mental Health Disorders 5 or DSM-5 [2]. The aim of the DSM manual is to provide general categorizations and diagnostic criteria for psychiatric disorders. These manuals are tools for HCPs and do not represent a substitute for expert clinical opinion. The World Health Organization's International Classification of Disease 10 or ICD-10 offers a general classification of all disease rather than specifically psychiatric/psychological disease [3]. ICD-11 is due for publication [4].
Psychological co-morbidities of chronic skin disease and the ’golden rules of psychodermatology’
Psychological stress is an integral cause of skin disease either as an initiating or an exacerbating factor leading to increased disease morbidity (see Chapter 11). It is therefore essential that the skin condition is treated concomitantly with the psychological co-morbidities (or the psychiatric/psychological aetiology). Part of the ’appropriate treatment’ of concomitant psychiatric/psychological disease is the assessment of risk and suicidality that should be in one's mind for every dermatology consultation. Treating the skin disease without treating the psychiatric/psychological disease makes no sense and yet a lot of training in dermatology makes little reference to the treatment of psychological disease. This leads to the golden rules of psychodermatology:
- Exclude organic disease.
- Appropriately assess and treat the dermatological disease at the same time as appropriately assessing and treating the psychological disease.
The following four discussions of different diseases illustrate the principle.
- Atopic eczema. The complex biopsychosocial realities of living with atopic eczema are clear (see www.atopicskindisease.com for useful information; last accessed August 2015). Atopic children and adolescents show more anxiety, handle situations less well and are provoked to anger more readily. In school and college, the psychosocial issues of mixing in peer groups and making personal relationships may be blighted by feelings of stigmatization and disfigurement. Stress makes atopic eczema worse [1]. Psychotherapies have a part to play in the holistic (skin and psychosocial) treatment plan.
- Psoriasis. Psoriasis is much more than a skin disease. Functional magnetic resonance imaging (fMRI) studies of patients with psoriasis show changes in the brain in response to ’disgust’ images [2]. Anxiety, depression and suicidal ideation are more common than in patients with eczema, acne or alopecia [3]. Depression is particularly significant and may remain undetected but is important because patients need to be treated holistically in order to improve [4]. Many patients indicate that stress has triggered the onset of the skin disease, but the latent period between a significant life stress and the onset or exacerbation of psoriasis has been difficult to assess. The response to phototherapy in highly worried individuals was almost half that of those who were deemed to have low worry and was constant for disease severity, disease duration, gender, age and skin type [5].
- Chronic urticaria. Chronic spontaneous urticaria has a significant effect on quality of life. It is significantly associated with depression, dysthymia and anxiety. Psychological factors may be prominent at the onset and contribute to disease progression, and negative coping may be associated with exacerbations [6].
- Alopecia areata. There has always been a strong anecdotal belief that the onset and recurrence of alopecia areata is related to stress and major life events [7]. Management of the grieving process and the psychosocial implications of living with hair loss is very much part of managing the patient's disease. Individual case reports continue to record success with individual psychotherapy, or use of antidepressants, either imipramine or selective serotonin reuptake inhibitors (SSRIs), and not always in the presence of clinical depression [7].
Stigmatization, visible differences and coping strategies
The word stigma referred originally to a mark or brand on Greek slaves, distinguishing them from those who were free. The term describes the situation of an individual who is disqualified from full social acceptance. The stigmatized individual is normal until abnormalized by societal views. These events may occur early, for example in those afflicted by congenital skin problems, or later in individuals with an acquired visible difference. But stigma is not just confined to the alterations in the visible body. Stigmatization may be an issue following individual behaviours and social factors such as substance abuse and unemployment. Or stigmatization may be associated with psychiatric disease. In addition there are the population prejudices of ethnicity and religion.
Some common situations where stigma may be encountered by patients include the following.
- Physical visible differences: congenital naevi (e.g. port-wine stain), acquired visible differences such as vitiligo, widespread inflammatory skin disease, surgical or post-traumatic visible differences.
- Behavioural and social factors: alcoholism and substance misuse, imprisonment.
- Psychiatric disease and learning disabilities.
- Race and religion.
Stigmatization in later life may present a different perspective because the patient has become a physical stranger to themselves. This is most striking and obvious in those who have developed disfiguring facial scarring, but is also as valid for the patient with a late-onset dermatosis or those who suffer the odour of hidradenitis suppurativa. Patients who experience stigmatization often refer to the guilt and shame that inhibits them from seeking help.
Stigma in psychiatry
Some people may hold a negative image of those with mental illness [1]. As with skin disease, there is a traditional stereotyping from historical attitudes towards psychiatric patients. HCPs who do not work with psychiatric patients may be inexperienced in accommodating the needs of this group. The importance in reducing the impact of stigmatization [2] is better understood in relation to social exclusion theory, which holds that:
- Humans possess a fundamental motive to avoid exclusion from social groupings.
- Much social behaviour attempts to improve the chances of inclusion.
- Negative effect (including loneliness and depression) results when a person does not or cannot achieve a desired level of social inclusion [3].
The measurement of stigma in dermatology and psychiatry has tended to rely on general measures of mental health with depression and anxiety scores, but also with psychometric measures of self-esteem such as the Rosenberg self-esteem scale. This has been used to assess stigmatization in psoriasis and eczema as well as mental illness. Furthermore the stigma scale for mental illness [4], developed to examine discrimination, disclosure and potential positive reactions to mental illness, demonstrated that stigma scale scores were negatively correlated with global self-esteem. Interventions in dermatological stigmata are concentrated on firstly the reduction in visibility, and secondly psychological-based approaches to forestall stigmatization.
Help for the stigmatized begins with information control from both physician and family. Self-help and contact with patient advocacy groups can be invaluable, such as Changing Faces in the UK (Box 86.3). A tolerant and informed grouping allows the expression of the normal developmental skills of the individual. Methods to change entrenched reactions within society to physical and psychological difference are more difficult to evaluate.
Disability, quality of life and assessment in psychodermatology
Quality of life (QOL) is defined as an individual's perception of their position in life in the context of the culture and value system in which they live and in relation to their goals, expectations, standards and concerns. It is a broad-ranging concept, affected in a complex way by the person's physical heath, psychological state, level of independence and social relationships and their relationship to salient features of their environment. Dermatologists increasingly understand that physical disease and QOL are intimately, but not linearly, associated. Patients with skin disease are often very clear that their disease has an impact on their lives. This impact may be huge or relatively minor. The amount of skin disease, though, does not correlate with the extent of psychosocial co-morbidity; nor does greater disease extent and longevity necessarily correlate with a lower QOL.
Managing patients holistically means that clinicians must be able to assess how the patient is feeling and what the impact of their disease is on their QOL. Assessments may be unstructured following Socratic question principles, or may be validated and reproducible tools (Box 86.4). There is a growing interest in cumulative QOL assessments (i.e. lifetime QOL).
There are some very short screening tools; for example the generalized anxiety disorder (GAD) two-question screen. If a patient answered affirmatively for either of the following questions, further assessment may be important.
- Question 1 During the past 4 weeks, have you been bothered by feeling worried, tense or anxious most of the time?
- Question 2 Are you frequently tense, irritable and having trouble sleeping?
These questions are used extensively in research, but are becoming increasingly important in everyday dermatology practice as they offer a standardized snapshot of patient psychosocial well-being (some research results also include scores of disease extent). There is an increasing recognition that it is not just the life of the patient affected by a skin disease, but also the lives of family, partners, carers and loved ones who are often affected by the patient's journey through treatment. Assessing the impact of disease on partners and family is crucial to the well-being of the patient. There is a growing interest in cumulative QOL scoring and meta-analyses of QOL tools.
DELUSIONAL BELIEFS
Introduction and general description
A true primary delusion is a false, unshakeable belief that arises from internal processes in a patient, which are not amenable to logic and are out of keeping with the person's educational and cultural background. Primary delusions can be an isolated phenomenon (a monosymptomatic hypochondriacal psychosis such as delusional infestation) or part of a broader psychosis (e.g. schizophrenia). A secondary delusion more commonly occurs with affective disorder and the delusion is secondary to the mood (e.g. a nihilistic delusion in severe depression may influence the patient into believing that his/her skin is rotting away). The intensity with which a delusional belief is held may be varaible. Delusional infestation, for example, may arise as an overvalued idea, and this somewhat less intensely held belief may be more amenable to negotiation and reason [1].
Delusions of infestation
Introduction and general description
Delusional infestation (DI) is an uncommon, but very disabling, condition where the patient is convinced that s/he is infested with a mite, parasite, bacteria, worm, insect, virus or animate material [1]. As this is a delusional disorder, the patient will hold this belief unshakeably and very often tenaciously. The patient believes wholeheartedly that s/he is infested even though no infesting organism or material can be found by clinicians. Although delusions are usually unshakeable and fixed, a few patients present with an overstated ideation of infestation (i.e. the patient believes that it is possible rather than unshakeably convinced that s/he is infested despite all evidence to the contrary). Patients with DI will usually present to dermatologists and be extremely reticent about seeing psychiatrists; they will frequently consume large amounts of resources having often seen a wide range of HCPs whilst remaining unengaged with treatment [2]. Some special forms of DI exist:
- DI as a shared delusion (folie à deux, etc.). Family members, carers and friends may believe that they too are infested, or delusionally share the belief of the individual who is presenting with DI. This is common.
- DI by proxy. Patients complain that their child, pet or friend is infested despite all evidence to the contrary.
DI may be primary (no underlying cause is found) or a secondary (to concomitant organic or psychiatric disease). Approximately half of patients presenting with DI will have secondary DI. The condition is usually a monosymptomatic delusion in that most patients hold no other delusional beliefs (as in, for example, schizophrenia). Occasionally patients may have other delusional ideations (usually when the DI is secondary to a co-morbid psychotic disease). Most patients can ’see’ the infestation but some remain uncertain whether what they see is actually the infesting organism or some other material. Patients are often isolated and have lived with their disease for a long time. Many fail to be engaged with HCPs, as the latter may try to reason that the disease is ’all in their head’. However, patients’ lives are extremely disabled by their disease and they often find themselves unemployed, in debt (e.g. some patients, in an attempt to rid their home of the infesting organisms, repeatedly buy new furniture and carpets), isolated (as loved ones may become more and more exasperated) and distraught (many patients go to great lengths to wash or clean their bodies).
The terms used prior to DI are now inappropriate as they refer to ’phobias’ (DI is a delusional not a phobic disorder) and ’parasitosis’ (DI patients present with a range of infesting organisms and animate material, not just parasites).
Epidemiology
Incidence and prevalence
These are unknown, but estimated at 17 per million people per year, although this is probably an underestimate.
Age
Delusional infestation can occur at any adult age but the peak incidence is said to be in 50-year-olds. It is rare in children although shared delusions in children of patients with DI have been reported.
Sex
The occurrence of DI is probably equally distributed in the sexes (as affected men present to clinicians much less with this disease than women), but is reported to occur in a ratio of male : female 1 : 2.5.
Ethnicity
Delusional infestation is found in all ethnicities.
Associated diseases
For diseases associated with secondary DI see Table 86.1.
Table 86.1 Diseases associated with or causing delusional infestation (DI).
| Primary DI | DI secondary to organic disease | DI secondary to psychiatric disease |
| No underlying disease | Substance abuse (Figure 86.1) Alcohol Recreational drugs Prescribed medications, e.g. anti-parkinsonian medication such as ropinerole Infections Tuberculosis HIV Endocrine disorders Thyroid disease Cancer Tumours Haematological cancer Chronic or acute liver disease Renal failure Metabolic disease Vitamin B12 deficiency Autoimmune disorders Systemic lupus erythematosus Multiple sclerosis Brain disorders Cerebrovascular disease Parkinson disease |
Schizophrenia Bipolar depression with psychotic symptoms Borderline personality disorder Anxiety disorder |
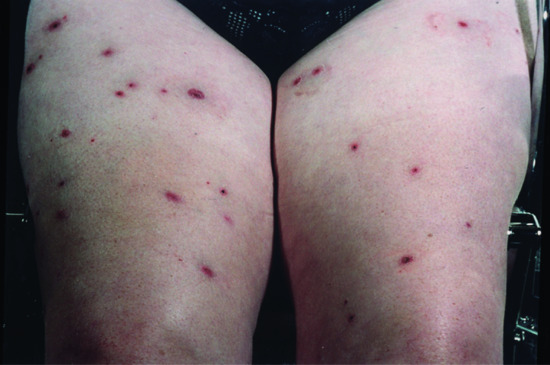
Figure 86.1 Excoriations in delusions of parasitosis in an amphetamine addict.
Pathophysiology
Many patients describe an initiating event. This can be a real insect bite, a misinterpretation of a real perception (an illusion) or a true hallucination (sensory experience in the absence of a sensory stimulus). Rather than dismissing the misinterpretation of an infestation, altered reasoning may occur (which may have a genetic and/or neurological basis), which leads the patient to believe there is a true infestation. Functional MRI in DI patients indicates that there may be abnormailities in the cortical and mid-brain areas associated with the interpretation of perceptions [3]. The involvement of the dopaminergic mid-brain structures and the therapeutic efficacy of antipsychotic D2-dopamine antagonists may indicate dopaminergic dysfunction in DI. For patients with DI secondary to organic disease, there is often a reason why brain function may be compromised (Table 86.1).
Predisposing factors
There may be a genetic predisposition for patients with primary and DI secondary to psychiatric disease. Patients with DI may be more likely to be socially isolated.
Pathology
Skin biopsy is best avoided except to exclude other cutaneous differential diagnoses. Histology (if it is taken) shows cutaneous excoriations or external trauma at various stages of the healing process.
Clinical features
History
The diagnosis of DI is usually not difficult and is initially considered following the history alone. Patients present with a belief that they are infested by an organism or animate material. They will often describe itching, biting, burning or crawling sensations on the skin that may be localized or generalized. These sensations may be intermittent or, more often, persistent and disabling. Patients often make great effort to prove the infestation (see section on the ’specimen sign’) [4].
Presentation
It is crucial that HCPs carefully examine the skin of patients with suspected DI for several reasons [2]. Firstly, it is important to check for a genuine infestation. Secondly, it is important to exclude differential diagnoses of DI and to look for clinical evidence of secondary causes of DI. It is essential for the patient to experience the clinician checking for an infestation, thereby confirming that his/her symptoms are being addressed. On examination, patients often have localized or generalized excoriations, erosions and sometimes ulceration. These skin changes are produced in an attempt to extricate the organism, usually with the fingernails, but occasionally nail files, scissors, needles, penknives, tweezers and nail clippers. Some patients go to much greater lengths to eradicate the perceived infestation by using surgical implements, handicraft knives and chemical corrosives (Figure 86.2). These can inflict significant damage. Occasionally there are no physical signs at all, but the patient will still maintain that the infestation is present and the itching/biting/stinging sensations are there.

Figure 86.2 Patient with delusional infestation. The marks on the legs are where the patient applied elastic bands to stop the ’worms’ from travelling up his leg beneath the skin.
Differential diagnosis
Differential diagnoses include:
- A genuine infestation.
- Causes of generalized pruritus (see Chapter 0).
- Immunobullous disease (usually this is easily distinguished from DI by the clinical picture).
- Organic disease that leads to secondary DI.
Complications and co-morbidities
Coexistent affective disease (anxiety, depression or both) is common in patients with DI. Assessing psychosocial co-morbidities is important. There is a considerable (but not fully charted) risk of suicide in patients with DI. Bacterial superinfection of excoriations and irritant dermatitis (e.g. from the patient's own use of cleansing agents) are common. Some patients create severe ulcers and extensive erosions from attempts to eradicate perceived organisms.
Disease course and prognosis
The crucial step in managing patients with DI is engagement of the patient [5, 6]. As with all psychodermatology disease, HCPs should treat the skin and the psychological disease concurrently (the ’golden rules’). Psychodermatology specialist centres are probably the best places to treat patients with DI, and most psychodermatologists will try to commence a treatment plan on the first appointment. Treatment is usually continued for several months until the delusion has settled. Patients at this stage will tell clinicians that the infesting organisms have ’gone’. Treatment of substance abuse and co-morbid affective disease may be necessary. Treatment may be slowly withdrawn a few months after the delusion has disappeared [6, 7], but recurrence of DI symptoms may occur in up to 33% of patients (especially those who have not managed to control recreational drug and alcohol abuse). Reported adherence to medication is good once engagement of the patient is established [6], but this may be in specialist centres with extensive experience of managing patients with DI. The prognosis in these centres is favourable, with up to 75% of patients responding to treatment. Suicide is always a risk in patients with DI, and clinicians must be aware of local services to which suicidal patients can be referred urgently [8].
Investigations and the ’specimen sign’
Patients with DI will usually be keen to prove their infestation. Many will bring along specimens of the organisms that they believe are infesting them (Figure 86.3). This used to be called the ’matchbox sign’, but more recently clinicians have recognized that patients may have access to sophisticated equipment and may bring along hi-tech audio or computer images of material they have themselves analysed. This has been termed the ’specimen sign’ [4]. It is imperative that these specimens are taken seriously and carefully reviewed by clinicians. Skin debris and specimen material may be analysed for human pathogens by microscopy in the local microbiology laboratory. A catalogue of normal results will assist the patient in understanding that the clinician understands the patient's experience and continues to seek and exclude a genuine infestation. Patients may repeatedly canvas clinicians to take skin biopsies to prove the infestation, and be unsatisfied with biopsies that fail to show a genuine infestation. Otherwise, investigations may be led by the clinical picture. A pruritus screen is undertaken routinely in some centres, but investigations that are informed by the clinical picture are usually acceptable. Assessment of coexistent affective disease and suicidality is imperative and careful assessment of recreational drug and alcohol usage is important.
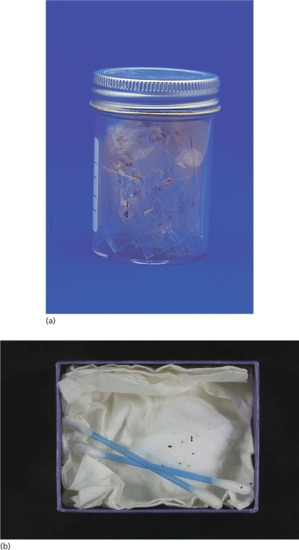
Figure 86.3 (a) Container brought in by a patient with delusional parasitosis. (b) ’Specimen sign’ for delusional infestation.
Management
Engagement of the patient is crucial in the management of DI [9]. HCPs must develop a sympathetic, understanding approach to the patient. It is usually futile to try to dissuade patients of the validity of their infestation. Instead it is better to let the patient know that you understand the difficulties that they are experiencing, and that you have successfully looked after patients with a similar disease. The enormity of patient experience is often halfway to engaging the patient with appropriate treatments.
Research in DI is difficult and very few randomized controlled clinical trials exist. Evidence tends to come from case series and is eminence based rather than evidence based. The choice of antipsychotic medication is often based on patient age, co-morbidities and lifestyle rather than any direct comparison of efficacy. Most psychodermatologists now avoid pimozide due to its cardiotoxic risks. Instead, most recommend atypical antipsychotics as the first line of treatment, together with treatment of the skin and any co-morbid affective disease (Figure 86.4).
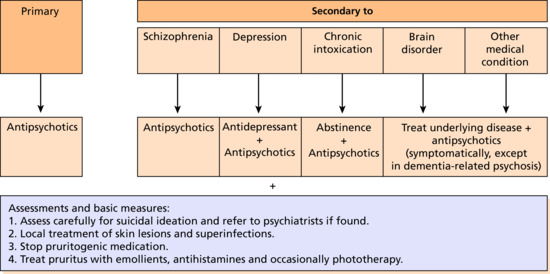
Figure 86.4 Management algorithm for delusional infestation. (From Lepping et al. 2014 [9].
Reproduced with permission of Wiley.)
Many patients will accept medication to help their distress even though it is not directed at the eradication of the ’parasites’. If broached in terms of using a medication that ’has helped others before’ and ’getting started to help in some way’ or ’to help with the sensations in the skin’, psychotropic medication may be commenced in the dermatology clinic by experienced physicians [10]. Management is ideally effected with close liaison between dermatology and psychiatry. It is mandatory to refer to a psychiatrist immediately if there is any indication of risk of suicide. Adherence to medication is actually very good once the patient is engaged with medication, as is the prognosis.
First line
There is only one (fairly poor) randomized controlled clinical trial of pimozide versus placebo. However, atypical antipsychotics are probably more effective and have a better side effect profile than conventional antipsychotics [6]. The antipsychotic rispiridone is both a dopamine blocker and a serotonin antagonist and has proved of further use in doses of 1–8 mg per day [7]. Olanzapine has a higher affinity as a serotonin blocker than a dopamine antagonist and can be effective in surprisingly small doses.
Resources
Patient resources
- Mind: www.mind.org.uk.
- Samaritans: www.samaritans.org.
- Skin Support: www.skinsupport.org.uk.
- (All last accessed August 2015.)
Olfactory delusions
Introduction and general description
Olfactory reference syndrome (ORS) is one of several unique primary psychiatric disorders that present to dermatologists. Published descriptions of ORS date back to the late 19th century and cases have been reported across the globe. The term ORS was coined by Pryse-Phillips [1] who described the condition as follows: ’The association of an “intrinsic” smell hallucination and a “contrite” reaction in the absence of a history of preceding depression’ (though anxiety and depression may be a consequence of ORS). ORS is probably a spectrum of different disease presentations and there remains some discussion about its classification. Patients may present with a true delusional and hallucinatory illness, but some may present as part of a body dysmorphic disease or obsessive–compulsive disorder (OCD).
Characteristically, the smell in ORS is described as being emitted from the patient – that is intrinsic as opposed to extrinsic (commonly described by patients with temporal lope epilepsy or schizophrenia). The term ’contrite reaction’ has been described in more recent literature as a ’preoccupation with body odour’ where patients may become sensitive to ideas of reference (e.g. people holding/scratching noses or opening windows), excessively wash themselves and change clothing, become socially withdrawn and in some cases suffer mild depression [2]. Hallucinations of various types occur as part of many disease processes, in ORS, however, the hallucination is olfactory only. It is accepted that persistent preoccupation with body odour may be seen in certain psychiatric illnesses or may be associated with organic brain injury and such disorders must therefore be excluded when diagnosing ORS [3, 4].
Much dispute has surrounded the classification of ORS [5]. This is largely due to the presence of the primary symptoms in other conditions. Most regard ORS as a delusional disorder. Since the behaviours that describe the contrite reaction are commonly seen in obsessed patients, the question has arisen as to whether or not ORS is in fact a variant of OCD. Much of the published literature is in the form of case reports, which makes this investigation more difficult; however, particular patterns have emerged and young males without any concurrent psychiatric disorder have been identified as the most frequent presenters.
Epidemiology
This is a rare condition, which is more common in young male adults (male : female 4.5 : 1), and occurs in all ethnic groups. Associated diseases include:
- Depression.
- Obsessive–compulsive disorders.
- Body dysmorphic disease.
- Dementia.
- Temporal lobe epilspsy.
Pathophysiology
Olfactory reference syndrome is poorly researched and the pathophysiology is not understood [6]. There are some clues, though, from case reports. Some patients with ORS present at the onset of dementia, and some cases are precipitated by dopaminergic medication for Parkinson disease. There are some patients who present with ORS as part of other psychiatric diseases.
Clinical features
Patients will usually present with a long history of experiencing an unpleasant smell from a specific part or from all over their body [7]. The smell is almost always unpleasant and may be faecal, putrific, sweaty, metallic or acrid. Patients will usually go to great lengths to cleanse themselves of the smell and will reject any suggestion that the smell is not experienced by other people. Some patients have organic brain disease. Some patients will also have features of body dysmorphic disease, OCD or both.
Box 86.5 lists the proposed criteria for diagnosing ORS [8].
Differential diagnosis
There are a number of possible differential diagnoses:
- A genuine body odour.
- Trimethylaminuria (fish odour syndrome): the patient has a genetic amino acid metabolic syndrome caused by abnormalities of the production/function of the ezyme flavin containing mono-oxygenase 3, which leads to the build up of trimethylamine (TMA) in body fluids. The ability to smell TMA objectively is genetic and variable. Urine analysis for TMA (usually compared to TMA oxide) is helpful to establish the diagnosis.
- Temporal lobe epilepsy (olfactory hallucinations are common).
- Other organic brain disease: dementia, Parkinson disease, brain tumour.
Investigations
Urinalysis should be used to exclude trimethylaminuria. Clinical examination and then appropriate neurological investigations should be performed as indicated.
Management [7–9]
Management is informed by case reports and case series only. Treatment of underlying body dysmorphic disease or OCD is the prime objective for some patients; treatment of any causative neurological disease is a similar priority.
Morgellons syndrome
In 2001, a biologist whose 2-year-old child developed sores on the skin discovered that the multicoloured fibres coming from her child's lesions were undiagnosable by the many physicians she consulted. The Morgellons were described by Sir Thomas Browne in 1674 in a population from Languedoc [1], one of whose characteristics was the development of a hairy back. Nevertheless this name was coined to entitle a syndrome, set up a research foundation, raise funds and generate vast media and Internet interest.
The phenomenon comprises:
- Sensations of crawling, stinging and biting under the skin.
- Sores that do not heal.
- Fibre-like filaments, granules and crystals that appear on or under the skin lesions (Figure 86.5).
- Joint and muscle pain and fibromyalgia.
- Debilitating fatigue.
- Cognitive dysfunction, poor concentration and memory.

Figure 86.5 Sample of the fibres that a patient with Morgellons disease brought to clinic.
Many dermatologists point to the commonalities between this constellation of symptoms and patients with DI [2]. Even so, an examination of Internet websites shows that patients who live with Morgellons are very sure that this is not the case and that ’Morgellons’ disease, as yet unrecognized, really does exist. The Morgellons Foundation has suggested that Lyme disease is to blame as well as agricultural filamentous yeasts, but the US Center for Disease Control has set up an independent study to evaluate the phenomenon, and has concluded that there is no objective evidence for ’unexplained dermopathy’ [3–5]. Treatment responses to pimozide and risperidone have been recorded, together with treatment of the skin with topical antiseptics, systemic antibiotics and (sometimes) phototherapy.
Resources
Patient resources
- Morgellons UK: www.morgellonsuk.org.uk.
- Skin Support: www.skinsupport.org.uk.
- (Both last accessed August 2015.)
OBSESSIVE AND COMPULSIVE BEHAVIOUR
Introduction and general description
Studies of obsessive–compulsive behaviour in dermatology outpatients estimate that OCD is present in up to 25% of patients, but this may include some with body dysmorphic disorder [1, 2]. However, excluding this group there were still up to 15% who have other obsessive–compulsive behaviours such as [1, 2]:
- Body dysmorphic disorder.
- Lichen simplex chronicus.
- Nodular prurigo.
- Skin picking disorder.
- Acne excoriee.
- Trichotillosis.
- Onychotillomania and onychophagia.
- Health anxieties.
General principles of treatment
- An empathetic, supportive approach from HCPs is essential.
- Try to find out why the patient has the ’habit’.
- Never attempt the tell the patient that it is ’all in their head’ or that they ’need to snap out of it’.
- Psychotherapy can produce significant improvement. CBT alone has improved some patients, although the management of underlying personality difficulties may require the specific skills of a psychotherapist.
- Habit-reversal programmes may be useful. These can be accessed online or via self-help material.
- SSRIs can be helpful. Usually patients need be encouraged to start treatment with explanations that the benefit will only start to be realized after 4–6 weeks. Higher doses may be necessary but maximal recommended doses must not be exceeded. Clomipramine and doxepin have been reported to work as well.
- The A-B-C model of habit disorders – Affect regulation, Behavioural regulation and Cognitive control – makes use of all modalities to help patients conceptualize and manage skin picking behaviours.
- Treatment is always based on appropriate treatment of the skin together with treatment of the associated psychological disease.
- Complex disease is best managed by a psychodermatology MDT.
- Second and third line treatments should be initiated by a psychodermatology MDT or through appropriate specialists.
Body dysmorphic disorder
Introduction and general description
Body dysmorphic disorder (BDD) is characterized by a preoccupation with a real or an imagined defect in physical appearance, or if there is a slight physical anomaly, concern is out of proportion to the anomaly. There is a spectrum from patients with overvalued ideas to those whose beliefs are held with delusional conviction. The defect that the patient experiences may seem trivial to objective assessors, but for the patient it is a major focus of their consciousness [1, 2].
Body dysmorphic disorder is surprisingly common, occurring in 1–2% of the general population [3]. It is more common in patients seeking aesthetic and cosmetic surgery [4]. There is a high degree of co-morbidity with mood disorders, OCD and social phobia. This is a difficult group of patients to treat; one of the main obstacles being that most patients lack insight and will not accept psychiatric treatment or referral. Patients may have ideas of reference (believing that their ’defect’ has been noticed by others and believing that other people's behaviour has been modified after witnessing the ’defect’). BDD is very disabling for the patient, and for those around them, since the focus on their perceived defect seems illogical but is also unshakeable. Co-morbid affective disease is common, as is suicidal ideation (up to 25% of patients will act on their suicidal ideation) [1]. Patients are therefore best seen in a joint psychodermatology clinic where possible. There are screening tools for HCPs to identify patients with BDD (especially for those patients seeking cosmetic surgery as the surgery may not address the primary BDD pathology).
Epidemiology
Gender
The female to male ratio is approximately 2 : 1 but this is likely to be evolving (male aesthetic concerns are approaching those of women).
Age
Body dysmorphic disorder often starts in adolescence but may affect any age group. It is often linked to low self-esteem (hence the preponderance of adolescent patients). Younger patients may have a better prognosis, in that relative dissatisfaction with appearance may be a relatively normal experience in this age group and may be self-limiting. HCPs need to be more worried when patients have severe symptoms, such as social avoidance and co-morbid mood disturbances (see Boxes 86.6 and 86.7).
Ethnicity
This disorder occurs in all ethnic groups.
Associated diseases
The following co-morbidities may be seen:
- Chronic skin picking.
- Depression may occur in 60% with a lifetime rate of up to 80%.
- Social phobia, that is fear of a negative impact (37%).
- Substance abuse (40%).
- Deliberate self-harm.
- Avoidant personality disorder.
- Anorexia nervosa patients very frequently have a degree of BDD.
- Suicide.
Pathophysiology [1,3,5]
Theories suggest that sufferers from BDD have self-defeating thoughts, cognitive distortions and destructive beliefs about themselves and their appearance. The development of selective processing of emotional information about body image, physical appearance and interpersonal contact may be related to anxiety disorders and social phobia. BDD patients exhibit more perfectionist thinking and maladaptive attractiveness beliefs, and it is assumed that these are aetiological rather than symptomatic. It has been suggested that childhood abusive experiences may result in body dissatisfaction, bodily shame, low self-esteem and body image distortion. Neurobiological theories relate BDD to acquired brain abnormalities and parietal lobe function. Neurochemical and psychopharmacological evidence suggests that abnormal serotonin metabolism also contributes to BDD. By contrast, social and cultural influences are assuming an increasing importance in personal bodily appearance due to the perceived concepts of beauty, and the quest for perfection, currently prominent in media-driven societies. These pressures shape the attitudes of both women and men. Women have traditionally been driven to view and treat themselves as objects whilst men are pushed towards an often unattainable body image, the Adonis complex of muscular perfection.
Clinical features
Patients with BDD may present with symptoms according to their gender. Women may present with a focus on the skin of the face, breasts, nose and stomach, whereas men may present with concerns about hair (usually thinning), nose, ears, genitals and body build. Facial symptoms are common, but patients with BDD may perceive ’defects’ affecting any part of the body. Concerns about hair (too much, too little or hair in the ’wrong’ place) are common. Some authors indicate that when patients find defects affecting the genital and (in women) breast area, HCPs may need to ask about sexual abuse. Patient's focus on their perceived defect is notoriously tenacious.
Patients will often behave in the following ways:
- Socialize poorly.
- Have a difficult relationship with mirrors (having to ’brace themselves’ to look in a mirror or avoiding mirrors completely).
- Pick at their skin.
- Hide their ’defect’.
- Have very persistent and intrusive thoughts about their perceived ’defect’.
- Repeatedly seek help from different HCPs (’doctor shoppers’).
- Repeatedly attend for cosmetic or aesthetic surgery.
Uncommonly, the delusional type of BDD gives rise to familial BDD where a parent imposes a delusional idea upon a child who in turn develops BDD or, even more rarely, the patient believes that their child has a bodily defect – BDD by proxy.
Prognosis
The prognosis for patients with BDD [6, 7] is variable, but good, when treated by dedicated BDD teams.
Investigations
Body dysmorphic disorder is a clinical diagnosis, but objective assessments of severity and screening tools do exist.
- Assess for potential suicide risk and refer where necessary.
- Assess for any underlying abuse (physical and mental abuse in a vulnerable adult/child).
- Assess for underlying psychiatric disease (depression, anxiety or both).
- Acknowledge genuine skin disease (e.g. hair loss or skin pigmentation changes).
- Investigate skin changes appropriately (this may mean no investigations at all or may mean appropriately investigating a differential diagnosis).
- Ask about substance abuse.
- Investigate any underlying psychiatric disease appropriately.
There are a number of scales (Box 86.6) and screening questions (Box 86.7) for the assessment of BDD.
Management
These treatments are in addition to the general approach to management outlined at the beginning of this section.
First line
Treatment of the skin
As always patients with psychodermatological disease need to have their skin and their psychological disease treated concurrently. Appropriate treatment of the patient's skin will facilitate engagement of the patient – but it is appropriate treatment rather than inappropriate surgery, which may not satisfy the patient's expectations. From the outset it is important to treat the psychological disease whilst addressing the perceived skin disease. Often there are some skin changes (however minimal) and acknowledging these changes rather than dismissing them will facilitate patient engagement.
Education for patients and their friends and family
There are excellent patient support books and organizations (see Resources).
Psychopharmacological treatments
Selective serotonin reuptake inhibitors and CBT are the treatments of choice. Fluoxetine [8], fluvoxamine and citalopram are the best-studied SSRI agents, but recent evidence suggests that all SSRIs are probably effective. Higher dosing regimens than those used for depression are usually required. Patients should receive a trial of 12–16 weeks before efficacy is assessed [9]. If one agent fails another should be substituted, as some patients idiosyncratically respond more favourably to one agent over another. Interestingly, SSRIs appear to be more effective than antipsychotic agents, despite the fact that BDD may sometimes be a delusional disorder. Only about 20% of delusional BDD patients will become free of their delusional thinking with SSRIs however. But, in delusional patients with BDD, the intrusiveness of the thoughts and distress will diminish sufficiently, such that many patients will be able to resume some social and vocational functioning. CBT may be used in conjunction with SSRIs or independently of SSRIs [10].
Talk therapies
There are various CBT techniques that can be used in the management of BDD [10, 11], although there are no trials comparing the different CBT techniques in a randomized, controlled clinical setting. Supportive psychotherapy can be helpful in patients with overvalued ideas and who are not truly deluded, but it is very time consuming and emotionally demanding. Patients with BDD are often poor communicators and difficulty with interpersonal relationships may be one of the central, crucial and earliest features of this disorder. The physician undertaking supportive psychotherapy has to be patient and realize that further skilled directive intervention will eventually be needed from psychiatrists or clinical psychologists. BDD patients are often poor attendees at clinics, but the consultation may in some cases be the only opportunity that a patient has to talk to another human being, which is a reflection of the isolated life these patients often lead. The dermatologist's essential role is to recognize the problem and sympathetically steer the patient on the correct path to help. Narrative therapy addresses the sociocultural causes that may establish beliefs, in this case about the body. The change process in narrative therapy involves helping patients replace these influences by more preferred stories about their problems and lives. Single case studies have been encouraging.
CBT has been shown to be effective in the management of patients with BDD, but trials are often open labelled or uncontrolled. There are a few randomized controlled clinical trials that clearly demonstrate the benefit of CBT, though the numbers of patients in these trials is small.
Second line
Antipsychotics
The evidence that antipsychotics are beneficial for patients with BDD (even those with delusional BDD) is sporadic and based on case studies only. It is very difficult to run controlled clinical trials with antipsychotics in patients with BDD. Although the evidence is not robust, there are some patients who will need to be treated with (usually newer atypical) antipsychotics such as risperidone, aripiprazole and others. These medications need to be initiated and monitored by specialists with extensive experience of their usage.
Resources
Patient resources
- Mind: www.mind.org.uk.
- OCD-UK: www.ocduk.org.
- Phillips KA. The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder. Oxford: Oxford University Press, 2005.
- Skin Support: www.skinsupport.org.uk.
- (All last accessed August 2015.)
Lichen simplex chronicus and nodular prurigo
Introduction and general description
Lichen simplex describes characteristic localized skin thickening in response to repeated rubbing and scratching (see Chapter 83). In some instances a minor initiating event, such as trauma, infection or an insect bite, precipitates episodic insistent scratching and rubbing. Irresistible itching is the major complaint, and scratching the chronic accompaniment. In the majority of patients, however, it is the response to anxiety, OCD or an irresistible, persistent itch [1]. Nodular prurigo is more generalized and complex (see Chapter 83). Many authors believe that nodular prurigo patients fall into two categories: atopic patients (see Chapter 0) and patients who are chronic skin pickers (see below).
Epidemiology
Incidence and prevalence
Lichen simplex chronicus and nodular prurigo are both common, occurring in between 1% and 10% of the population depending on the report.
Age
Patients probably represent two populations: an early-onset atopic group with a mean age of 19 years, and a later, non-atopic group with a mean age of 48 years. The earlier onset group consists of both men and women, but the older group is predominantly female.
Sex
These diseases are more common in women.
Ethnicity
All ethnicities are found, although Afro-Caribbean and oriental patients are slightly more commonly affected.
Clinical features
Regular rubbing and pressure on the skin produces characteristic thickened, coarsely grained papules and nodules with hyperpigmentation (Figure 86.6). The classic sites of involvement are within easy reach, particularly on the nape and sides of the neck, elbows, thighs, knees and ankles. These areas may be in varying stages of evolution, from early, small, violaceous papules with surface excoriations to chronic areas that present as hyperkeratotic plaques with pigment changes, described as ’dermatological worry beads’. Affected areas are more often localized, and patches of lichen simplex chronicus affecting the vulval or scrotal skin are very common [2]. Scratching or rubbing is carried out using either the hands, back of nails or knuckles, and sometimes with the use of a convenient instrument such as a hairbrush or pen. The actions may be subconscious but more often patients engage in conscious episodes of scratching, which continue until the pruritus is relieved and is replaced by soreness and pain. The change from itch to pain is quite sudden and this abrupt cessation has been described as ’orgasm cutanée’.

Figure 86.6 (a) A patient with nodular prurigo. (b, c) Close up of noduar prurigo.
Complications and co-morbidities
Most authors have commented on the relationship of emotional tension to bouts of scratching. Patients are usually described as stable but anxious individuals [3], whose reactions to stress are relieved by habitual behaviour such as rubbing. Aggression and hostility related to anxiety caused by emotional disturbance may lead to itching. There is considerable evidence that habitual scratching sets up neurotransmitter changes in the brain that act as temporary ’stress busters’. Habitual scratching is often opportunistic (i.e. when the patient can get to the skin) but may become ’addictive’ and so potentially out of control. The freqency of scratching episodes often increases with perceived stress.
Management
There are a number of treatments in addition to the general approach to management outlined at the beginning of this section [5–8].
Skin picking disorder
Epidemiology
Incidence
This disorder occurs in 2% of dermatology patients, but the majority of these have pathological picking associated with atopic and other cutaneous diseases. Skin picking disease in the absence of cutaneous inflammatory disease is rarer but still common [1].
Age
There are two peaks of occurrence: (i) in adolescence and early adult life [2, 3]; and (ii) in middle-aged women. Any age can be affected, although it is rarer in younger children.
Gender
Females are more commonly affected than males.
Ethnicity
Any ethnicity can be affected.
Clinical features [4]
The lesions differ from other artefactual disorders as those who suffer admit to an urge to pick and gouge at their skin (Figure 86.7). There may be an initial reluctance to own up to the self-damage but patients are usually willing to discuss the picking as a ’response to stress’. Any area may be affected. The average duration of disease before presentation is up to 10 years. Patients spend up to 3 hours per day picking, thinking about picking or resisting the urge to pick. These bouts can be ritualized to a set time and place, often the bathroom, frequently at bedtime. Although these activities are usually executed fully consciously, rarely a fugue or trance state can be apparent. Lesions may be quite deep, extending into the dermis, and are more commonly distributed within reach of the dominant hand. Older lesions show pink or red scars, some of which may be hypertrophic. Chronic lesions may also show atrophic scars, which merge and are eventually seen as linear, coalescent areas. Lesions appear at all stages of development and may number from a few to several hundred. Concealment behaviour, for example make-up and clothing, is present in 65% of chronic cases and active avoidance of social situations found in 40%. Up to a quarter of patients may increase alcohol, tobacco or recreational substance habits to counter the burden of disease.

Figure 86.7 (a,b) Facial picking disorder.
Differential diagnosis
It is important to exclude excoriations caused by generalized pruritus, bullous disorders (such as pemphigus) and linear excoriated lesions, which may be the presenting signs of lichen planus or lupus erythematosus. Rarities such as mucinoses that cause scarring are usually distinguishable entities. Another differential is acne excoriée (see separate section).
Complications and co-morbidities [5]
Pre-existing skin disease (e.g. atopic eczema or acne) is very common, as are psychosocial co-morbidities. There may be precipitating psychological events such as divorce, bereavement, abortion or separation. Depression and/or anxiety are often found. Family members with chronic disease is also a common finding.
Complications may include:
- Cellulitis, bacteraemia and septicaemia.
- Scarring.
- Anxiety, depression and guilt.
- Rarely, self-mutilating amputation of a body structure (e.g. breast).
- Suicidal ideation.
Management [6–9]
Acné excoriée
Introduction and general description
There are few patients with acne who can resist squeezing skin lesions. Brocq described acne excoriée particularly in adolescent girls under emotional stress, who picked and squeezed acne lesions [1]. Although some patients develop these lesions after picking acne, most had no acne at all. The condition should be considered a variant of skin picking disorder with the lesions largely confined to the face (Figures 86.8 and 86.9) [1–3].
Epidemiology
Acne excoriée is usually seen in young (often white) women [3], with a second peak in women in their thirties.
Clinical features [4]
The clinical lesions resemble those of chronic excoriations (Figure 86.8b). They are found predominantly around the hairline, forehead, preauricular cheek and chin areas. Extension to the neck and occipital hairline is common. Chronic lesions characteristically show white, atrophic scarring with peripheral hyperpigmentation. Lesions are picked as a ritual, apparently as a response to itch or throbbing. The lesions are excoriated until ’emptied’. There are usually some acneform lesions, at least when the disease first appears.
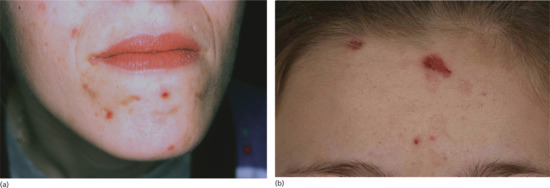
Figure 86.8 Acne excoriée. (a) Habitual scarring lesions of the cheek and chin. (b) Lesions on the forehead.
Differential diagnosis
Differential diagnoses include the facial picking disorder (where there are no acneform lesions originating the picking habit), trigeminal trophic syndrome (see Chapter 84) and dermatitis artefacta.
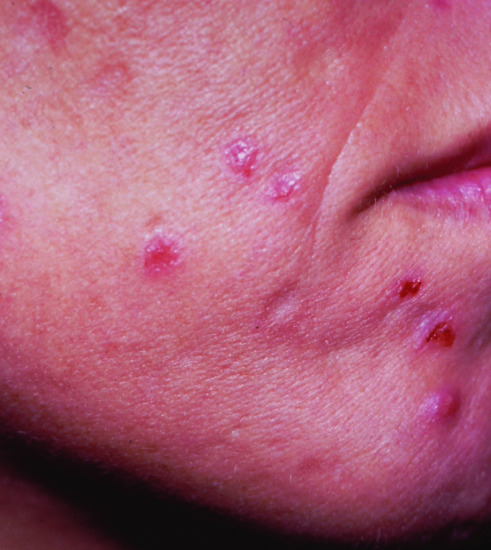
Figure 86.9 Acne excoriée.
Management [5–8]
Trichotillomania/trichotillosis
Introduction and general description
The term trichotillomania.was first used by Hallopeau in 1889 and is derived from the Greek thrix (hair), tillein (pull out) and mania (madness). Current thinking is that the term trichotillosis is more accurate as the condition is not a ’mania’ but more of an OCD spectrum disorder. Diagnostic criteria that have been cited include:
- Recurrent pulling out of one's own hair resulting in hair loss.
- An increasing sense of tension immediately before pulling out the hair or when attempting to resist the behaviour.
- Pleasure, gratification or relief when pulling out the hair.
- The disturbance is not better accounted for by another mental disorder.
- The disturbance provokes clinically marked distress and/or impairment in occupational, social or other areas of functioning.
Many subdivide patients into younger and older groups and those with dissociative symptoms [1]. Patients with an earlier onset with limited progression usually have a better prognosis. Recalcitrant, obsessive and focused hair pulling is usually found in older women, and patients may deny their hair pulling. Automatic hair pulling is also found, and some patients pull their hair in a dissociative or fugue state.
Epidemiology
Incidence and prevalence
This is commoner in children and college students (rates of 0.6–3% have been reported). Overall, later and more severe trichotillosis is not common. Cosmetic hair pulling (eyebrows, etc.) is extremely common, but most do not fulfil diagnostic OCD criteria.
Age
There appear to be two distinct populations: those who present in childhood, mainly between the ages of 5 and 12 years, and more chronic cases who present as adults but who started hair-pulling activities in adolescence or early adult life [2]. The number of affected children may be seven times that of adults and there is evidence of a bimodal distribution with peaks in the preschool years and in adolescence [3]. Preschool children are more likely to be boys (62%), although after this older boys and male adolescents make up only 30% of the group. This early-onset group, usually aged between 2 and 10 years, show benign, self-limiting behaviour and most are probably suffering a habit disorder, perhaps as an extension of hair twirling activity and childhood stress. The adolescent group are much more likely to be female, with ratios of up to 3.5 : 1. In adults there is greater psychopathology and a distinct female preponderance, usually 4 : 1, but this is most evident in the oldest group (F : M 15 : 1).
Ethnicity
Trichotillosis is found in all ethnicities.
Associated diseases
The aetiology of trichotillosis is not fully understood, but seems to be related to the following [4]:
- Underlying anxieties.
- Depression.
- Underlying BDD.
- Psychosocial triggers.
- Family dysfunction (common).
- Other cutaneous ’habits’ such as nail biting and nail pulling.
- Deliberate self-harm ’cutting’, etc.
- Eating disorders.
- Rarely substance abuse.
Familial predisposition is fairly common and successive generations of patients with trichotillosis have been described. It is always worth considering the (rarer) association with emotional or sexual abuse.
Clinical features
Most patients relate that the trichotillosis is a compulsion that is irresistible and that leads to a short-lived sense of relief or release when hair has been pulled out. But the relief usually leads rapidly to a sense of guilt and hopelessness. The habit is often hidden from the partner/close family and the hair loss is usually covered up. Patients may describe a sense of control over their body/psychosocial situation that is briefly facilitated by their hair pulling habits. Some describe pulling hair in a fugue-like state and having no control over the episodes of hair pulling.
Hair pulling and plucking is commonest from the scalp. Some patients select an apparently abnormal hair by feel or texture and extend it into an adjacent area. Most pull hair from the vertex, but temporal, occipital and frontal hair loss in children may be more obvious on the side of manual dominance. The hair loss may be minimal, commonly a solitary patch, but visible hair thinning may progress to virtual total depilation, significantly so in adult women. The hair pulling activity is usually not as a response to any skin symptoms but is either a conscious, deliberate act or more often a subconscious act, almost in some children being part of a hypnogogic (dream-like) state. Some patients may have incomplete awareness until the pattern has been established. The eyelashes, eyebrows, facial and pubic hair may also be primarily affected. Children will also pluck eyebrows and eyelashes (Figure 86.10) but adults almost exclusively pluck hair on the torso. Two-thirds of adults pulled hair from two or more sites and one-third from three areas. Involvement of a second area began after an average of 8 years. Body and pubic hair plucking, commoner in males, may become a ritualized activity done either alone or as a conjugal activity and can indicate a personality or psychotic disorder. Hair is plucked from the scalp on average two to three times per day and daily from other areas. The duration and frequency of activity is variable but adults in general have longer and more frequent activity. Children tend to manipulate hair at times of leisure, for example watching TV, when tired and in the evening. Adults have a more conscious, structured activity, initially seeking thicker or distorted hair and then progressing to larger areas, taking more and more time over the activity. This may become similar to a compulsion with elaboration of the rituals using instruments such as tweezers. The more frequent the plucking episodes, the greater the body image dissatisfaction and the more likely the patient will suffer depression and anxiety. There are similarities and overlap with BDD in some cases.

Figure 86.10 Childhood trichotillomania showing eyelash involvement with hair loss and broken-off hairs. This child also had scalp involvement.
On examination, there are often areas of hair loss together with areas of hair regrowth (stubble and longer hairs) (Figure 86.11). This pattern may involve the eyebrows and eyelashes. There is occasionally frank scarring from where the habit has been repeated incessantly and the follicle has scarred. The patterns of plucking activity are centrifugal from a single starting point or linear, in wave-like activity. In extreme cases, the centrifugal pattern removes all hair except the most difficult to access, namely that on the occiput. This shows as a ’tonsure pattern’ or ’Friar Tuck’ distribution. Patients use wigs, hair weaving, false eyelashes and semipermanent use of hats and scarves to disguise the defects. Chronic folliculitis of the neck, chin, chest, pubic areas or thighs as a result of plucking activity may also be the presenting complaint.
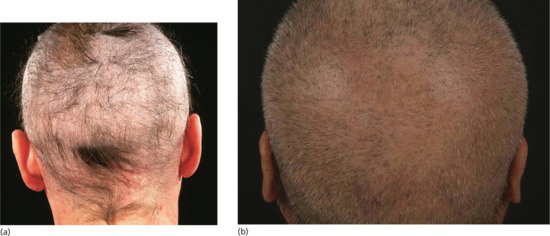
Figure 86.11 Adult trichotillomania. (a) Extensive hair loss with a preserved tuft over the occiput. (b) Patient with hairs at different lengths.
Children may pluck the hair, or stroke or suck the hair root before chewing and swallowing the remainder. The hair root alone may be eaten (trichorhizophagia) as a secretive activity and in a few patients the whole hair is eaten (trichophagia). Patients who eat more hair tend to swallow the longer strands and a very small percentage develop gastrointestinal bezoars.
Complications and co-morbidities
- Scarring hair loss.
- Folliculitis.
- Keloid formation.
- Trichobezoar. This name is derived from the Arabic word badzahr, meaning an antidote or counter-poison (cf the Harry Potter stories). It also relates to the hardened contents of the fourth stomach of the Syrian goat, much prized as a cure for many diseases. Bezoars are ball-like aggregations of vegetable or fibre-like materials in the stomach and small intestine (Figure 86.12). The true incidence of trichobezoar is unknown. It is seen almost exclusively in girls and young women. It is rare but its importance is that morbidity is high with chronicity and severe complications, which can lead to death. Longer hair is more likely to become enmeshed into a ball by the action of peristalsis, and this then becomes too large to leave the stomach via the pylorus. The larger the ball, the more likely it is that gastric atony will develop, leading to symptoms of nausea, indigestion, bloating and pain. The hair ball may eventually completely fill the stomach. Although the condition is very rare, it should be considered in children with trichotillosis who present with a combination of any of the following: abdominal pain, weight loss, nausea, vomiting, anorexia and foul breath. More common is the parental threat to their children that ’if you keep chewing your hair, eventually you'll have a hair ball in your stomach’.
- The Rapunzel syndrome [5]. This describes a trichobezoar with a tail that extends at least to the jejunum; sufferers are highly likely to have gastrointestinal obstructive symptoms. In a review of 27 cases, which included only one male, the mean age at presentation was 10.8 years. Most patients ingested their own long hair although cases have been recorded of bezoar by proxy where another person's hair has been eaten by the patient. In this group 37% had abdominal pain, 33% nausea and vomiting, 26% obstruction and 18.5% developed peritonitis. The hair ball can have a tail as long as 195 cm. The tail may also be broken up into numerous segments distributed throughout the small bowel. Recurrent Rapunzel syndrome has been reported [5]. Life-threatening intestinal obstruction necessitates surgical intervention.

Figure 86.12 Gastric trichobezoar on barium contrast examination showing a lace-like pattern of the mass of hairs.
Investigations
The diagnosis is usually clinical [6]. Scalp biopsy is rarely necessary unless clinicians need to distinguish trichotillosis from scarring alopecia. Trichomalacia is seen as deep distortion and curling of the hair bulb. In severe damage there is intraepithelial and perifollicular damage. Trichoscopy/dermoscopy has been reported as being very helpful in the presence of a corroborating history (broken hair shafts, hairs of different lengths, traumatized hair shafts).
Management
These treatments are in addition to the general approach to management outlined at the beginning of this section.
Onychotillomania and onychophagia
The compulsive habits of nail picking (onychotillomania) and nail biting (onychophagia) have been shown to be common in children and adolescents [1]. The aetiologies suggested include stress, imitation of family members and transference from the thumb sucking habit. Nail biting is usually confined to the fingernails, but nail picking, especially in adults, may involve all digits. Damage to cuticles and nails causes paronychia, nail dystrophy and longitudinal nail scarring [2]. In chronic cases, there is an association with trichotillosis. Compulsive biting, tearing or picking with instruments such as scissors, knives or razorblades may lead to permanent destruction.
Onychotillomania may be a feature of developmental problems in children and is a component of self-destructive behaviours in the Tourette and Prader–Willi syndromes. In adults, chronic nail biting is most commonly an isolated, self-destructive habit, which may respond to cognitive behavioural training [3]. It is also common as a compulsive action as a part of OCD, not always at times of stress. Rarely, onychotillomania is a manifestation of a major depressive disorder that has a suicide risk. Self-induced anonychia of the toenails was produced by one man who plucked out his nails with pliers rather than suffer recurrent paronychia from previously crushed toes.
Health anxieties
Introduction and general description
Health anxieties are irrational fears that are out of proportion with objective reality, and overwhelmingly distort everyday life. They can be regarded as obsessional fears. Dermatology patients may present with focused anxieties about the development of a variety of cutaneous diseases. Predominant cutaneous anxieties (or phobias) can be divided into:
- Anxieties of contamination, e.g. dirt phobia, germ phobia, wart phobia.
- Fear of malignancy, e.g. cancer phobia, mole phobia.
- Others, e.g. blushing, sweating.
- General health anxieties.
Dirt, infection and wart phobias [1]
These are OCDs where the patient has an overwhelming fear of contamination or infection of the skin or body. Hand washing leading to dermatitis is common, but up to 10% will admit to compulsive body washing also. The precipitating factors are fears of dirt and contamination from others who have been infected with real organisms (e.g. meticillin-resistant Staphylococcus aureus or MRSA) or those who might have been (e.g. those recently discharged from hospital). Situational exposure in work to dirt and waste may initiate the fear. Hand washing may occur up to 100 times per day and compulsive showering and bathing 10–20 times daily. Irritant dermatitis that does not resolve with adequate advice should prompt inquiry, not only about washing compulsions but also checking behaviours.
Mole and cancer phobias [2, 3]
This is an OCD where the patient has an overwhelming fear of developing cancer and may stray into delusional disease. A dislike of moles and freckles may be a manifestation of BDD but for most patients who repeatedly demand mole examinations, and sometimes excision, there is an underlying cancer phobia. It occurs in response to various stimuli. For example, the patient may have had a malignant lesion removed and need constant reassurances. Or there may have been malignancy or death from melanoma in family or friends, or concern repeatedly triggered by media, medical or family pressure. It is an excessive response to disease, often related to anxiety. Patients present regularly and acutely to a screening clinic or primary care physicians. They may demand removal of some or all of their moles or even attempt self-surgery. Mole phobia by proxy is not uncommon in parents who worry about their children and their moles to such an extent that normal play activities and family holidays are curtailed because of concerns about sun exposure. Unless the primary pathology (the OCD/anxiety disorder) is addressed, the condition is likely to continue.
Other anxieties and phobias [4]
Topical corticosteroid phobia occurs, predominantly about skin thinning and to a lesser extent stunting of growth in children.
Management [5]
These treatments are in addition to the general approach to management outlined at the beginning of this section.
EATING DISORDERS
Introduction and general description
Eating disorders are considered primarily as psychiatric illnesses that have significant physical complications. Anorexia nervosa, bulimia nervosa and a third group called ’eating disorders not classified’ are particularly common among young women and are increasing in incidence.
Anorexia nervosa and bulimia
Introduction and general description
For anorexia nervosa to be diagnosed, the following criteria must be found:
- An inability to maintain a normal or minimum weight for age and height coupled with an intense fear of gaining weight; the body mass index (BMI) is less than 17.5 kg/m2.
- A distorted perception of weight, size and body configuration.
- Amenorrhoea.
Bulimia nervosa is defined by the following:
- Recurrent and compulsive overeating episodes (binge eating).
- Recurrent and inappropriate compensatory behaviour in order to avoid gaining weight; these include induced vomiting and abuse of diuretics and laxatives.
- Binge eating and weight reduction behaviours occurring at least twice per week for 3 months.
- Self-esteem affected by weight and body configuration.
Epidemiology
Incidence and prevalence
Anorexia nervosa now has an incidence of up to 1% and bulimia up to 5% of the general population [1]. Reviews suggest a lifetime prevalence of 2.2%, with over half the cases not detected initially in the health care system. The annual prevalence is about 0.3% for anorexia and 1% for bulimia, although this may be higher in women aged 15–24 years [2]. The incidence is 270 per 100 000 person years in this group of younger women compared to 8 per 100 000 person years in the group of women as a whole.
Age, sex and race
Anorexia occurs earlier in life, usually in adolescence, whilst bulimia has its peak in the later teens and early twenties. The majority of sufferers are young women; the proportion of men being 1 : 20 though there is increasing evidence that this is moving closer to 1 : 5. White races predominate in published studies. The prevalence in Afro-Caribbean and Asian women is rare. It is commoner in industrialized societies and much more frequent in those of high social class.
Clinical features
Cutaneous co-morbidities [3]
There are a number of skin problems commonly found in sufferers of anorexia and bulimia:
- Xerosis and pruritus.
- Russell's sign (knuckle pads from chewing the skin overlying the knuckles) (Figure 86.13).
- Nutritional disease:
- Pellagra.
- Dermatitis enteropathica.
- Anaemia and hair loss secondary to iron deficiency.
- Cutaneous microvasculature:
- Raynaud phenomenon.
- Acrocyanosis and perniosis.
- Hair abnormalities:
- Hypertrichosis.
- Hair loss.

Figure 86.13 Russell's sign: callosities of the knuckles from manual forced vomiting in bulimia.
Psychodermatological co-morbidities
- Self-injurious behaviours [5].
- Trichotillosis.
- Severe onychophagia.
- Fabricated dermatitis.
- Suicide; the risk is much higher than in the normal population [6].
- Substance abuse.
- BDD [7].
Investigations and management
Dermatologists should suspect anorexia nervosa when presented with these suggestive signs, particularly in an underweight girl. A simple screening questionnaire is helpful for detecting eating disorders (Box 86.8). Eating disorders are largely undetected in the community. Patients not resistant to the suggestion of specialist care should be referred to a psychiatrist. Dermatologists may be able to help with advice about treatment of skin manifestations.
PSYCHOGENIC ITCH
Psychogenic pruritus
Introduction and general description
Pruritus is a multifactorial symptom. Dermatological, neurological, iatrogenic illness and internal disease are well-recognized causes [1] (see also Chapter 83). The propensity for individuals to sense itch after psychological provocation by pictures of insects, rashes and watching other subjects scratching demonstrates the ready ability of simple measures to induce psychosomatic pruritus. Misery and colleagues have proposed diagnostic criteria for psychogenic pruritus [2]. There are three compulsory criteria:
- Localized or generalized pruritus sine material.
- Chronic pruritus (>6 weeks).
- Absence of a somatic cause.
Localized or generalized psychogenic itch may begin as a stress response [3]. Patterns of itching and scratching may predominantly occur during periods of relaxation or non-occupied time. Pruritic episodes may be unpredictable in onset and present with abrupt and sudden termination. The quality of itch may be unusual, described as crawling, stinging or burning. Sites of predilection in two-thirds of subjects were the legs, arms and back. Localized itching may lead to generalized body itch within a short time. In some individuals, intense scratching can induce a feeling of pleasure which may be related to the release of opioids centrally.
Patients with psychogenic itch may go on to develop [4, 5]:
- Nodular prurigo.
- Depression (about 30%).
- Anxiety and depression (10% for out-patients and 20% for in-patients).
Management [6–10]
Treatment of psychogenic itch is best seen as concurrent treatment of itch sensations at the same time as treating the underlying or associated psychosocial co-morbidities.
FACTITIOUS SKIN DISEASE
Introduction and general description
Doctors usually believe what the patient tells them. The unwritten contract of the consultation process is that the patient will relate the details of the illness as truthfully as they see it and respond to the physician's questions as openly as possible, neither deliberately hiding nor distorting the facts. The physician makes these assumptions in assessing the combination of signs and symptoms of the illness. Some patients may exaggerate or minimize symptoms. Patients may misattribute causation on the basis of experience, culture and a need to place the illness in a context. They may have mistaken beliefs because of advice from other medical or, increasingly, media- or Internet-inspired sources. These consultation behaviours are common and do not constitute a fabrication, although if persistent this conduct can alienate a clinician's objectivity.
Clinical deception refers to a spectrum of illness that lies in a continuum depending on the level of intention to deceive at the time of the act, and the motivation for the induced illness. The definition of factitious behaviour is not completely clear since the level of intention may vary, but for the dermatologist the definition by DSM-5 includes:
- A Falsification of physical or psychological signs and symptoms, or induction of injury or disese, associated with identified deception.
- The individual presents himself or herself to others as ill, impaired or injured.
- The deceptive behaviour is evident even in the absence of obvious external rewards.
- The behaviour is not better explained by another mental disorder such as a delusional disorder or another psychotic disorder.
In factitious disorder imposed on another (previously factitious disorder by proxy), DSM-5 criteria are similar except criterion ’B’ refers to an individual presenting another person as being injured or harmed in some way.
Criterion A supposedly excludes disorders characterized by unintentional production of symptoms, thereby marking a distinction between factitious disorders and somatoform, conversion and dissociative disorders. Criterion B assumes an internal incentive which the patient may deny even to themselves, and criterion C excludes the intentional production of symptoms for external gain, thereby marking a distinction with malingering.
The nomenclature for dermatological lesions produced by patients, as defined above, is multifarious. Artifice is a noun meaning the use of cunning plans or devices in order to trick or deceive whilst an artefact is defined as man-made and artistic or decorative. A fabrication is an invention often, in certain contexts, meaning with deceitful intent, whilst factitious is an adjective meaning artificial or contrived. The term factitious dermatitis will be used preferentially here in keeping with the revised definition of Münchausen syndrome by proxy as factitious or induced illness (FII). Factitious falsification of information, that is lying, is a consequence of the manufacture of skin lesions, the occult use of others (proxy disease) and disease produced for material profit or retribution. The lying may have a different quality in these cases, such that the psychosocial lies of the impulsive, immature, young girl are mainly used to avoid the shame and denigration of exposure, whereas the pathological lies (pseudologica fantastica) of the accomplished malingerer are used to embellish his or her performance.
There are a series of recognized factitious skin diseases characterized by the following features: firstly, the dermatoses are caused by the fully aware patient; secondly, there is a desire to hide the cause from their doctors. This definition includes dermatitis artefacta, dermatitis simulata, dermatological pathomimicry and dermatitis passivata. These syndromes are additionally distinguishable from others where there is overt secondary gain, such as Münchausen syndrome, Münchausen by proxy and malingering.
For all factitial skin disease (including dermatitis artefacta) it is crucial to make sure that organic disease is safely excluded and to try to prioritize why the patient is presenting with the condition rather than how.
Dermatitis artefacta
Introduction and general description
Dermatitis artefacta is a skin disease caused entirely by the actions of the fully aware (i.e. not consciously impaired) patient on the skin, hair, scalp, nails or mucosae (Figure 86.14) [1]. These patients hide the responsibility for their actions from their doctors. Deliberate self-harm differs from dermatitis artefacta in that patients will often own that they are ’mutilating’ their skin (Figure 86.15).

Figure 86.14 Dermatitis artefacta. (a) Symmetrical and predominantly monomorphic lesions on the hands. (b) Severe dermatitis artefacta resulting from a patient who extensively pulled apart the scalp and needed a plastic repair.

Figure 86.15 Scarring from deliberate self-cutting over a birthmark.
Epidemiology
In adults, all studies have shown a female preponderance, with the ratio of female to male varying from 20 : 1 to 4 : 1. Lesions have been found in children from the age of 8 years; prepubertal children have an equal sex ratio, which rises to 3 : 1 female predominance by the early teenage years [2]. These series confirm that the majority of cases begin in adolescence and in adults under 30 years of age, although there is an important subgroup whose age of onset is significantly older. This latter subgroup is distinguished by being more likely to be male (male to female ratio 2 : 1), to produce more subtle skin lesions and to have a past history of somatizing illness. Complaints may take the form of pseudoseizures, abdominal pain, syncope, chronic fatigue and backache.
Pathophysiology [3]
The motivation of patients is variable. There is a distinction between disease, illness and sickness. Disease refers to primarily biological forms of pathology, illness to the subjective experience of being diseased and sickness involves the process of being ill. People differ in the way that they perceive, assess, act or fail to act upon the symptoms that they experience. This is recognized as a personal ’illness behaviour’ and shapes the role, firstly, within the family and, secondly, with professional health advisors. The psychopathology underlying the production of factitious lesions suggests that the patient wants the sickness role as the essential pathology. It is suggested that these patients have complex underlying drivers, for example self-hate and guilt, and an illness allows inappropriate regression and avoidance of adult responsibilities. Factitious illness symbolizes both anger at, and/or conflict with, authority figures, for example school phobia. Psychiatric or medical care fulfils massive dependency needs, such as inadequate coping strategies.
In many cases, the psychosocial stress of a major life event may be apparent. Children and adolescents commonly show anxiety and immaturity of coping styles in response to a dysfunctional parent–child relationship, bullying, physical body changes, or sexual and substance abuse. Adults may be reacting to adverse situations in an immature, impulsive manner. The more chronic patients tend to have a demonstrable personality disorder, most often borderline personality disorder.
The development of dermatitis artefacta is more common in those with memorable early (and sometimes continuing) experience of illness, or in those who have a family member who is (or has been) unwell, or who is a health care professional.
Clinical features [4]
The diagnosis of dermatitis artefacta can usually be suspected quite early on. The two characteristics are the physical signs and the fabricated story that accompanies them.
The ’hollow history’ and shared beliefs
The story is either a series of fabricated lies or, more commonly, a ’not knowing how the skin lesions happen’ (the ’hollow history’). The patient often describes the sudden appearance of complete lesions with little or no prodrome. There is no complete description of the genesis of individual skin lesions. The lesions appear or are ’discovered’, often on waking. Lesions appear at an identical stage in development, in crops or groups, more often symmetrically but rarely scattered, apparently at random. There is usually a lack of disease progression history. By contrast there is a prolonged and elaborate description of the complications and the failure to heal. Characteristically, established lesions may undergo sudden deterioration at the same time as new areas appear. Only rarely do patients use more than one method to produce lesions. It has been suggested that the patients show a ’belle indifference’ to their predicament as part of a dissociative state and that, in the presence of visible disease, manifest a nonchalance and innocence transmitted through an enigmatic ’Mona Lisa smile’ (Figure 86.16). Patients are more often passive than aggressive, even though they have a widespread disfigurement. However, considerable anger is commonplace from parents, carers, spouses or partners, who complain at the incompetence of a succession of doctors. Patients and their relatives may consume huge amounts of medical resources to seek the cause and resolution of the ’problem’. Relatives are usually convinced that the patient is genuinely ill. Official complaints to hospital management and to local or other government officials may follow.
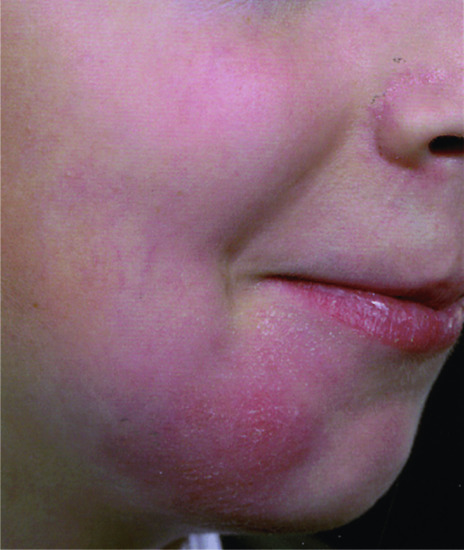
Figure 86.16 Factitious disease of skin on the chin and the ’Mona Lisa smile’.
Clinical signs [5, 6]
For all age groups, the commonest site of involvement is the face, particularly the cheeks, representing over half the presentations in children (Figure 86.16). The dorsa of the hands rather than the palms are the next commonest site, then the forearms, most frequently of the non-dominant limb. There is a particular covert pattern on covered skin where the clothes hide significant mutilation of the breasts, abdominal areas and sometimes the genitalia. These areas of damage in young girls should prompt inquiry about sexual abuse. Involvement of the back, axillae and external ear is uncommon.
Cutaneous lesions have been produced by every known means of damaging the skin and are therefore polymorphic, bizarre and mimic any of the known inflammatory reactions in the skin (Figure 86.17). Factitial dermatitis should enter the differential diagnosis of every chronic, puzzling and recurrent dermatosis. The lesions are usually linear, angulated or assume patterns that do not conform to recognized skin disease morphology, and are often the result of thermal, chemical or instrumental injury (Figure 86.18). Commonly, circular erosions or blisters of a uniform size can be manufactured (e.g. by cigarette burns or cryodamage from a closely applied pressurized aerosol such as an antiperspirant or asthma inhaler). Perfume may remain detectable in the lesions for some days. Less commonly, dermal lesions from blunt trauma presenting as odd haemorrhages or dramatic dermal indurations and necrosis are found from foreign body injections of milk, cosmetic oil or industrial grease [7]. These are found more often in the breasts, thighs or penis, the latter as covert body augmentation.

Figure 86.17 Dermatitis factitia. (a) Crude, linear, angulated and destructive factitious dermatitis. (b) Note the straight edges and sharp angulation of some of the lesions.

Figure 86.18 Persistent ulceration of the breast from covert injections of milk and talcum powder.
Excoriations may be made with nail files, sanding boards, cheese graters or wire brushes to produce raw, crusty, linear or arciform lesions with characteristic geometrical edges. Urticarial lesions are initially produced by chemical damage and progress subsequently to blistering, crusting and scarring (Figure 86.19). Characteristically, these areas may show the ’drip sign’, where corrosive liquids have been uncontrolled and allowed to run over the skin (Figure 86.20). Bleaches, soaps and household cleaners are most commonly employed by women; industrial acids and automotive fluids by men. These chemicals may produce a persistent, detectable smell on the skin.

Figure 86.19 Dermatitis artefacta (a) of the ankle, and (b) close up of a lesion.

Figure 86.20 Dermatitis factitia showing the drip sign.
Clinical variants
Factitious cheilitis.
Factitious cheilitis (also known as le tic des levres), or the production of artefactual lesions of the lips, is not common. It is most frequently seen in girls and young women but the incidence is equal in male and female older patients. Simulation of cheilitis has been produced by applying a crust of paper, glue and colourant. Reactions of the lips are limited and appear in particular as persistent inflammation with crusting and variable haemorrhage. The crusts may be very thick with a succession of layers of congealed haemorrhagic exudates resembling a carapace or oyster shell. The haemorrhage can also be impressive with coagulated blood and serum extruding over the lips. This is caused by picking, biting, rubbing and licking. Occasionally, young adolescents will develop a disuse crusting of the lips because they become dysmorphic about cleaning and washing their mouth. Removal of the crusts leaves a relatively normal lip although with time there is some superficial erosion. Differential diagnosis includes contact dermatitis, actinic damage, chronic lip licking habit and causes of granulomatous cheilitis.
Factitious nail disease.
Traumatic and chemical damage to both the nail and nail fold have been seen in children and adults. The paediatric cases show chronic paronychia caused by the insertion of nails, pins or splinters. Soldiers avoiding duty have habitually used caustics to damage their fingers. The characteristic lesions show purpura and haemorrhage around the nail fold but also subungual haemorrhage and pustules. A significant sign is repeated traumatic nail loss occurring singly or multiply on one hand only.
Hair artefact.
A distinctive pattern of hair loss may occur after cutting or shaving. It differs from the plucked appearance of trichotillosis, with obvious gross changes such as rough, cropped areas of hair loss or unnatural, patterned shaved alopecia of the scalp or eyebrows.
Witchcraft syndrome [8, 9].
Artefact dermatitis can be provoked on an unknowing and unsuspecting victim by proxy. For example, as an act of revenge, a hairdresser applied benzyl ether to a customer's skin. This induced hyperaemia with some oedema within 10 minutes but not on the perpetrator since absorption of the agent is very low on the palm of the hand; thus she could easily apply it to the customer's skin without harm to herself.
Dermatitis artefacta with artefact of patch tests.
Bullous dermatitis artefacta in a female veterinary assistant healed with occlusive dressings. New bullae on the other arm prompted the parents to demand ’allergy’ tests. Ten patch tests to yellow petrolatum were applied to the back, which provoked a non-inflammatory bulla on one of the sites 2 days later [10]. In another case the patch test reaction was mimicked by scarification in an attempt to claim compensation [11].
Constriction artefact.
Oedema of limbs from constricting bands has been described (Secretan syndrome). It is characteristic that one digit, usually a toe, will be constricted at a time whilst the others are unaffected. A repeated series of single, different ischaemic toes, whilst all the others are healthy, should raise suspicion of external banding. Embolic disease can be excluded by vascular scan.
Purpura artefact.
Purpura and bruising are seen after suction, friction or blunt trauma. Children produce purpura on the chin by sucking on cups and on limbs by direct mouth suction or with the use of a toy or tool. Shearing stress also produces purpura, tending to present as linear limb lesions. Extensive bruising and bleeding in a child means that factitious and induced illness (see Fabricated and induced illness) should be excluded, caused not only by trauma but also drug-induced by anticoagulants.
Dermal artefact.
Dermal skin lesions may take the form of panniculitis-type lesions and boggy, fluctuant swellings. Careful examination of an acute lesion may reveal the presence of a needle track where milk, air, faeces, urine, cooking oil, silicone, grease or engine oil has been injected. Access to needles and syringes may be via medical or paramedical family and friends.
Postsurgical artefact.
There is a group that presents with a non-healing, postsurgical wound (Figure 86.21). This may follow a small operation after minor skin trauma, breast biopsy or instrumentation such as a laparoscopy. Wounds ’burst’ after the sutures are removed, become recurrently infected and real organisms such as MRSA appear. Unfortunately, further ’wound repairs’ exacerbate and legitimize the continuing wound. It is not unusual to see patients who have had up to eight operative revisions before a further referral is made to a dermatologist.
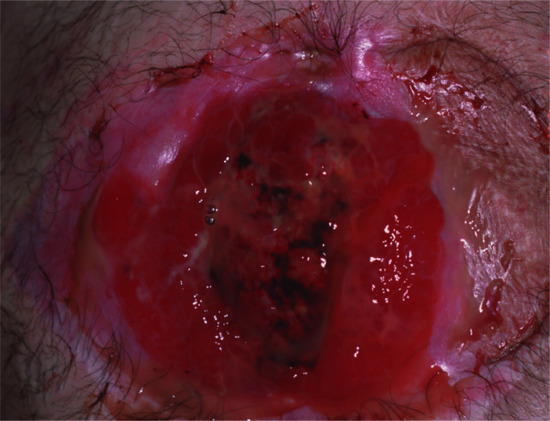
Figure 86.21 Non-healing wound after surgery with characteristic central ’interference haemorrhage’.
Complications and co-morbidities
Twenty per cent of patients have a somatization disorder and hypochondriasis. These are co-morbid with anxiety, depression and substance abuse. Borderline personality disorder is a factor for chronicity in both sexes. True hysteria, where there is dissociation between the act of self-damage and the awareness of performing the action, is debated at length based on the premise that the patient may be performing a conscious act for unconscious reasons.
Complications of dermatitis artefacta include:
- Pigmentation disturbances.
- Scarring.
- Cutaneous infection.
- Osteomyelitis.
- Fistulae.
- Severe infection such as cerebral abscess.
Investigations [12]
The diagnosis is usually not very difficult to make and is considered usually quite early on in the patient's journey. Nevertheless, it is essential to exclude organic disease (see the ’golden rules of psychodermatology’). Any skin biopies must be carefully assessed with very close clinicopathological correlation to avoid under- and overdiagnosis. For this and a range of other reasons, it is essential that dermatitis artefacta is managed in a psychodermatology MDT setting. A skin biopsy may provide essential supportive information but may help to exclude organic disease, but a skin biopsy is not necessary in the majority of cases.
Histological appearances can include an epidermis damaged by friction or chemicals with a vacuolar dermatitis and lymphocytes around degenerating keratinocytes. Superficial acute and dramatic epidermal necrosis from physical and chemical damage is characteristic of crude damage to the skin. Subepidermal blistering can be produced by thermal and cryodamage. In contrast, the subjacent deeper dermal tissues can appear spared. Some chemicals, for example toothpaste, can induce unusual inflammatory dermal appearances suggestive of cutaneous lymphoma (pseudolymphoma). Injections into subcutaneous tissues can also produce deeper lesions that show as vasculitis or an odd panniculitis. Ink shows as pigment with limited inflammation, and talc excites a macrophage reaction with giant cells. Injected oils and greases produce deep continuing panniculitis.
Special stains can reveal silver from silver nitrate caustic damage. Examination under polarized light can identify foreign material and further refinement can be found with energy-dispersive X-ray analysis and infrared spectrometry. Unlike disease states, the histopathology of factitious disease may vary with time and it has been shown that serial biopsy may be diagnostically helpful because differing patterns of change may be present on each occasion. Occasionally, patients will bury needles completely into their skin to produce recurrent abscesses. A straight X-ray will visualize these. Some patients have inserted hundreds of needles throughout the skin; if one is identified, then other body areas should also be X-rayed. Wooden skewers may also be inserted; these are best seen via MRI scans.
There are psychometric tests that can be used for the assessment of factitial disorders, but these are essentially research tools.
Management [12–14]
The management of factitious dermatitis is not an interrogation. There are three therapeutic aims.
- Treat the skin appropriately. The skin damage may be extensive, disfiguring and infected, with the potential for scarring and dyspigmentation. The process of tissue repair may take time but this allows the opportunity for patient–clinician relationship building. It is important that the physician has a helpful, non-aggressive, sympathetic approach. Very occasionally, occlusive bandaging will allow lesions to heal (except for those of the most determined patients).
- Time should be taken to identify the nature and extent of the psychological problem. The dilemma has always been whether patients should be confronted or not. Generally, most psychodermatologists advocate not confronting the patient unless there are specific benefits (secondary gain, fugue states, etc.). The doctor must avoid personalizing the episode and needs to consider the approach that is most likely to change the patient's behaviour. The patient's psychological problems should be approached in a non-intrusive manner, allowing the patient freedom to express their difficulties in a confidential environment. Children usually respond well to this approach, particularly if a cause of psychosocial pressure is identifiable. Any concerns about abuse should be addressed with protection teams immediately, and concerns about significant psychiatric disease warrant an urgent referral to psychiatric services.
- Clinicians need to address why the patient is presenting with dermatitis artefacta. Usually a cause for the dermatitis artefacta will be revealed as soon as the patient feels safe with the clinician and the environment. This can be very quickly after presentation or may take a very long time. The reasons why a patient presents with dermatitis artefacta are very variable and may be relatively easily addressed (e.g. parental pressure to succeed at examinations) or may be very difficult to address (e.g. sexual and physical abuse). Concommitant affective disease is fairly common and may need to be treated at the same time.
Adult patients may respond to a non-confrontational ’narrow escape’, ’quasi-confession’, ’recovery’, ’face-saving’ or ’escape with honour’ strategy. This mechanism works by suggesting that the patient does some ’personal homework’ to find a solution to their illness by offering a rationale for recovery. The patient may claim that alternative medicine such as hypnosis, homeopathy or fringe methods such as manipulation and aromatherapy has ’cured’ them. It is important to follow up the patient to establish that psychological and social factors were intrinsic to the remission.
One additional technique is the double-blind strategy where the physician explains that the treatment carries an expectation for recovery. If this does not occur then they will be forced to conclude that failure to improve constituted conclusive evidence that the problem is psychological or factitious. A study of behavioural interventions of this type in acute and chronic non-organic (conversion/factitious) motor disorders showed that this produced positive resolution in chronic cases resistant to more passive techniques. This strategy worked particularly well where members of the family were angry or sceptical about the nature of the symptoms.
The prognosis is that of the primary psychological disorder. Acute stress reaction can be addressed in a series of short consultations at the time when the dressings are changed. Approximately one-third to one-half of patients continue to develop chronic lesions. Such patients may have a personality disorder (commonly borderline) and need psychiatric assessment. Unfortunately, this is frequently unacceptable to the patients who may default the clinic or ask to be referred elsewhere.
Dermatitis simulata
Apparent skin disease can be represented by patients who are ingenious enough to use external disguise to simulate disease (Figure 86.22). These patients do not significantly damage their skin. Make-up has been used to paint on a rash or simulate a birthmark. This is most common in children. Glue and crystallized sugar can produce a coagulum to simulate a desquamating rash or chronic cheilitis, drugs to induce skin discoloration and topical printing dyes to produce discoloured sweat. These discolorations can be removed by aqueous or alcohol swabs and analysed if necessary. Sugar crusts dissolve easily in water, keratin ones do not. Red make-up has been used to simulate a port-wine stain on the face. These deceptions may be clever enough to confuse their doctors for months.

Figure 86.22 Glue applied to look like herpes zoster.
Dermatological pathomimicry
Some patients may intentionally aggravate an existing dermatosis using the explanation of its genesis given by their dermatologist. It is distinguishable from dermatitits artefacta because the disease looks like an exacerbation of an established skin disease with none of the bizarre physical signs typical of mechanical, chemical or thermal interference. It should also be differentiated from self-inflicted, delayed healing of surgical and traumatic wounds, which is achieved by external damage. A clinical suspicion should arise when patients suffer unexplained exacerbations of disease or are particularly unresponsive to adequate supervised therapy. More direct confrontational discussion without recrimination may prove useful.
Dermatitis passivata
The cessation of normal skin cleansing will produce an accumulation of keratinous crusts. This is commonly seen in geriatric or demented patients who suffer from self-neglect, and in its extreme form has been called the Diogenes syndrome. The lesions are the result of self-neglect and comprise cumulative accretions of keratin and dirty debris that forms a thick carapace with time (Figure 86.23). Lesions are usually found on the upper central chest, over the back and accumulated as coagulated debris in the groins. Elderly patients may be paranoid, have mood disorders or have temporofrontal dementia. Alcohol abuse may be a co-factor. Younger patients may present with lesions on the scalp, face or arms and are invariably accompanied by parents or family. Significant psychopathology is common with schizoid thought disorder and social withdrawal. Specialist psychological therapy is usually necessary, either as day care or community psychiatric support.

Figure 86.23 Diogenes syndrome in a young man showing accretions of facial keratin and debris.
Malingering
Asher defined malingering as the imitation, production or encouragement of illness for a deliberate end [1]. The American Psychiatric Association DSM-5 definition states that the ’essential feature of malingering is the intentional production of false or grossly exaggerated physical or psychological symptoms, motivated by external incentives such as avoiding military duty, avoiding work, seeking financial compensation, evading criminal prosecution, or obtaining drugs’.
Malingering may be co-morbid with conversion disorders [2], personality disorders [3] and other factitial behaviour. However, it usually differs from most factitial disease in being short term and opportunistic. Other illness falsification tends to be chronic and persistent. Fear, desire and escape are the three main motives for producing false or grossly exaggerated physical or psychological symptoms. Soldiers feigning disease and disability hope to avoid duty, suspend transfer or be discharged from the service [5]. Workers can prolong sick leave, delay corporate change of job or seek to obtain early retirement with an apparently extended illness. Some patients may seek compensation for a contrived illness, for example alleged burns, or aggravate and continue an existing disease, for example industrial dermatitis, out of a sense of grievance or retribution. Prolonged legal cases of supposed medical negligence are common in those with manufactured illness whose dissatisfaction with their doctors, or the care they have been given, may lead to a financial settlement as a reward [6]. Chronic, non-healing, postoperative scars are manipulated with instruments, or even faecal injection, to maintain sepsis. Hand dermatitis, both irritant and allergic contact, may be perpetuated to seek higher compensation awards.
Treatment depends on the underlying psychiatric illness, if significant psychopathology can be found, but the opportunist response in patients with an underlying personality disorder is poor [7].
Pseudologia fantastica and Münchausen syndrome
Asher used the term Münchausen syndrome to describe notorious hospital hoppers who present with a dramatic and untruthful story of illness [1]. This is a chronic, severe and dramatic subtype of factitious disease. The essential elements are the recurrent nature of the illness, and the frequency and similarity of the repetitive pattern of the complaint in different hospitals (peregrination). The simulated illnesses may be esoteric and rare, with the patient often presenting a dossier to the doctors. Whilst dermatological complaints are uncommon in Münchausen syndrome, simulated porphyria and connective tissue disease, for example, may present to the dermatologist. The last element in the syndrome is pseudologia fantastica (pathological lying) [2, 3]. This describes the telling of lies about past social history and connections, exploits, wealth and invention of an alias. The patients are usually male, over 30 years of age and travel widely from hospital to hospital. They complain of abdominal pain, haemorrhage or some neurological incapacity. Skin lesions are rare. The commonest signs are non-healing wounds, widespread blistering or multiple excoriations associated with other somatic complaints. Serious consequences such as septicaemia and paraplegia have occurred from induced cutaneous ulceration. Characteristically, patients take their own discharge if they sense their deception has been discovered.
The Internet provides access to those interested in health and medicine and is a rich resource for some patients [4]. As the Internet offers ’virtual support groups’ these individuals may offer ’virtual’ factitious disorders. Cases have been reported showing the facility with which they can attract attention, mobilize sympathy and control others.
Fabricated and induced illness
In 1977, Meadow had the clinical acuity and personal courage to describe the syndrome of Münchausen by proxy where the illness in a child is fabricated by the parent, usually the mother, or someone in loco parentis [1]. This phenomenon has been redefined as fabricated and induced illness [2]. Other carers may be involved and may include health professionals [3].
Doctors and others may not only fail to understand the origins of a child's symptoms but also institute further harm by inappropriate investigations, treatment and surgery. The guidelines for identifying cases mirror many of those discussed for dermatitis artefacta. The history is ’hollow’ with a lack of detail. Most parents and carers can give a clear account of an accident. Risk factors include single parent, previous abuse, frequent visits to the GP or accident and emergency departments, poverty, overcrowding and young parents [4]. The victims have a persistent or recurrent illness that cannot be readily explained. The previous diagnoses remain descriptive and not stringent. Symptoms do not respond and laboratory tests are incongruous. The reported symptoms are inconsistent with the presenting health and the symptoms fail to appear in the absence of a certain parent (usually the mother) [5]. The perpetrator is reluctant to leave the child even for a few minutes, but remains oddly impassive even in an emergency. They refuse treatments and hospital admission and may become hostile and abusive. Characteristically, these carers attempt to make close relationships with some medical staff, usually nurses, with a blurring of the professional–parent objective relationship. There may be fabrication of family details and a disturbed marital and social structure. Rarely, parents exhibit the syndrome themselves and produce proxy lesions on the child.
The victims are usually infants or toddlers with a mean age at diagnosis of 40 months. The mean delay between presentation and diagnosis is approximately 15 months. The most common presentations in a literature review [6] were bleeding and bruising (44%), central nervous system depression (19%), apnoea (15%), diarrhoea (11%), vomiting (10%), fever (10%) and rash (9%). Skin lesions are amongst the five commonest signs. Bruises in children are common on the lower legs and arms. Bruises at certain sites should raise concern – these sites are the face and head of a child less than 1 year old, the sides of the face and ears, black eyes and bruising on the buttocks/lower back and outer thighs. These are the ’punishment’ sites [7]. The pattern of bruising may show fingertip marks, striate finger stripe effects from slapping, or pinch marks as opposing crescent-shaped lesions. Kicks to the lower body show as irregular, large, deep bruises. Belt and strap damage appears on the trunk as parallel curved marks. The other skin lesions are usually crude forms of factitious dermatitis produced by thermal burns or caustic corrosives on the skin [8].
A large review of countries outside the English-speaking industrialized populations produced similar results [9]. The long-term consequences of childhood victimization might contribute to the development of factitious disease in adult life. Elements of the child victim experience, including feelings of powerlessness, lack of control and disappointment in the physician, are the suggested dynamics for the development of independent illness falsification. A full discussion of the issues in these cases with paediatric services is essential.
Fabricated and induced illness is occasionally seen in the elderly, special needs or other vulnerable adults perpetrated by relatives, nurses and care home personnel [10].
MEDICOLEGAL ISSUES IN SUSPECTED FACTITIOUS SKIN DISEASES
The most important action for the physician who suspects factitious disease is to share the suspicion with colleagues at a very early stage [1]. Case conference discussion and involvement of the institution's management and legal services after these group discussions help to avoid isolation and persecution of the physician. Structures will differ according to health providers in each country but the solitary physician may find support disappointing if an acrimonious dispute arises and legal action has been taken.
DELIBERATE SELF-HARM
Definition and nomenclature
Self-mutilation of the skin may present with a wide range of lesions. Cutting and scratching are frequent, but other methods, such as grazing, burning with fire or chemicals, or the insertion of foreign bodies under the skin are also seen [1]. The damage can be to a wide range of body parts, including the face and genitals. Cases of self-harm may present to accident and emergency departments with acute damage in need of treatment, or to the clinic with chronic lesions or scarring [2].
The relationship between such self-harming behaviours and suicide is complex and varies widely amongst cases. Authors have made a distinction between repetitive cases of self-mutilation that occur in the context of suicidal ideation, or ambivalence towards suicide, and those cases that clearly occur outside the context of suicidal ideation [3]. It should be noted, however, that there is a potential for overlap between the two, due to the difficulty in measuring or categorizing ’intent’ and because there are cases of repetitive self-harm, apparently without suicidal intent, progressing to completed suicide [4].
Deliberate self-harm with suicidal ideation
Self-mutilating behaviour is often grouped with other behaviours, such as self-poisoning, attempted hanging or jumping from heights, as ’parasuicide’ or ’deliberate self-harm’ [4]. The patient describes suicidal ideation, or ambivalence about continuing to live, at the mental state examination. The most frequent lesions are caused by self-cutting, often to the wrists. Burns and ligature marks, and their scars, may also be seen. The predisposing and precipitating factors for this behaviour are numerous. The act may be in response to the symptoms of an underlying psychiatric illness, such as depression, substance misuse or schizophrenia. Vulnerable individuals may respond with parasuicidal behaviour to social or interpersonal stressors. Often a combination of psychiatric and social factors is elicited from the history. Patients often present to accident and emergency departments with acute lesions; in many areas, psychiatric screening of such cases by specialist services is standard. Some patients, however, commit these acts and do not present for emergency medical treatment. Patients may present with chronic lesions or scarring when this behaviour has become a frequent response to stressors, and such stressors are chronic, such as untreated illness or continuing social problems. Referral for treatment of underlying psychiatric illnesses is indicated where one is present. There is evidence that social intervention is of benefit in improving outcome where these factors are precipitants [5].
Deliberate self-harm without suicidal intent
Introduction and general description
A number of authors have made the case for a distinct syndrome of self-injurious behaviour, or self-mutilation, occurring outside the context of conscious suicidal ideation. Further classification into categories is based on the degree of tissue damage and the rate and pattern of the destructive behaviour [6]:
- Major.
- Stereotypic.
- Superficial/moderate.
Epidemiology
Gender
An increased prevalence in women is reported.
Age
The onset is typically in early life, below the age of 30 years. The mean duration of the syndrome is 12 years.
Pathophysiology
Predisposing factors
Recent work has demonstrated a potential genetic link [7]. Deliberate self-harm has been associated with numerous other psychiatric conditions. Personality disorders, especially borderline type [8], are found in many studies and reviews. There is an association with childhood trauma, including abuse. Eating disorders, depressive and bipolar affective disorders, anxiety disorders, somatoform disorders, OCD, substance misuse disorders and schizophrenia have also been described in association with self-harm. Another major group of patients who self-mutilate is found in those with learning disability.
Psychological symptoms described by repetitive self-mutilators include dysphoria, anxiety, depersonalization and aggression. The patient may experience and describe a strong compulsion to self-harm, similar to compulsion in OCD. The act of self-mutilation may provide relief from the unpleasant emotions or compulsion to self-mutilate, and may also induce feelings of self-control, power or euphoria. Relief may last from several hours to several weeks. In addition, a marked reduction in pain sensation, or increase in pain tolerance, is described in self-mutilators, although this is not uniform. The act is usually performed in private.
Reviews of biological correlates of self-injurious behaviour have suggested changes in opiate, dopaminergic and serotonin systems [9]. One study found reduced imipramine-binding sites in platelets, a marker for serotinergic dysfunction, associated with self-harm. Other proposed biological mechanisms are reinforcement of self-mutilating behaviour due to dysregulation of the dopamine system.
Management [10]
Treatment should include appropriate referral where the disease is associated with another psychiatric diagnosis. There are no clear guidelines for pharmacological treatment of self-mutilation syndrome itself, and a lack of randomized trials. Indeed some authors do not feel there are any general recommendations for the use of psychotropic medication. Where suggestions have been made, SSRIs have been used, in line with the serotonergic hypofunction hypothesis. Dopamine antagonists and opiate antagonists have also been suggested. Mood stabilizers, β-blockers and analgesics have all been used.
Psychological approaches to treatment are varied. Behavioural and psychodynamic techniques are used in group and individual settings. Dialectical behaviour therapy has been described as successful, but access to this therapy varies regionally. Authors make the point that therapy can be long term, difficult and, in serious cases, involve periods of in-patient care.
Patients presenting with self-harm are a heterogeneous group, and likely to have complex problems in any of the biological, psychological and social domains. An understanding of the aetiological factors behind an individual's presentation is a key first step to deciding upon a programme of treatment. This may include pharmacological strategies, but there is as yet no clear core medication recommendation for these cases, and treatment is often complex and specialized.
OTHER PSYCHODERMATOLOGY AND PSYCHOCUTANEOUS DISEASES
Cutaneous disease and alcohol misuse
Alcohol may have an effect on the skin either directly (toxicity) or indirectly (via mast cells and the peripheral and central nervous system) [1, 2]. The effect of alcohol on the liver may also lead to skin disease (porphyria cutanea tarda). Alcohol dependence and alcohol abuse are on the increase. They rank among the three commonest psychiatric disorders in the community. The prevalence of alcohol abuse and dependence is 4.65% and 3.8%, respectively [3]. There are significant medical and economic consequences because of differing effects of alcohol on metabolism, health, treatment behaviour and motivation.
Alcohol abuse can be missed as a diagnosis by experienced physicians even though the problem is common. Mechanisms for screening and brief interventions are well established and show robust stringency [4]. The four-question CAGE questionnaire (Box 86.9) used as part of a general health enquiry is a consistent indicator of alcohol problems [5]. A two-question screen consisting of, firstly, an enquiry about past alcohol problems and, secondly, significant drinking within the last 24 h is also a sensitive index. The combined sensitivity of these tests shows a 90% accuracy.
Up to 15% of admissions to hospital are directly or partially related to alcohol intake. Alcohol abuse is also co-morbid with psychiatric disorders such as depression, OCD and anxiety states.
The cutaneous manifestations of alcohol abuse include diseases that may be exacerbated or caused by the alcohol (Box 86.10) [6, 7].
The psychosocial effects of chronic and disfiguring skin disease often produce feelings of stigma and rejection. Recreational substances such as alcohol are commonly used by affected patients as a negative coping mechanism [8]. Most itchy skin diseases are at least exacerbated by alcohol abuse. Seborrhoeic dermatitis is twice as common with alcohol abuse and this may be related to immunosuppression and the effect on cutaneous microflora.
Studies have suggested that female as well as male psoriatics showed an excess rate of alcoholism [9]. Also, whilst alcohol abuse was not a factor in the onset of psoriasis, it became significant in women after the disease was present. Up to 30% of patients with psoriasis thought they had difficulties with alcohol and 13% a current drinking problem. Furthermore, a daily intake of alcohol of more than 80 g was associated with poor treatment responsiveness in patients with psoriasis. It also appears that the changed character and distribution of psoriasis make it more difficult to treat. In studies of patients with psoriasis, alcohol abuse was not marked by elevated liver function tests [10]. Alcohol abstinence helped to induce remission and relapse was induced by re-consumption. The effects of alcohol on immune function and skin vasculature are thought to precipitate exacerbations of rosacea and postadolescent acne.
Genuine infestations of the skin (scabies and pediculosis) and superficial skin infections (usually related to Staphylococcus aureus) were found more often in alcoholic vagrants than in non-alcoholics and those with other psychiatric disorders. This also suggests that more specific alcohol-related immune factors may be active.
Depression in dermatological patients
The concept of depression is frequently used to mean disillusion, disenchantment, helplessness, frustration or mental fatigue. True depressive illness is an important but frequently missed diagnosis for non-psychiatrists. Up to one-third of medically ill patients have depressive symptoms and depression has a greater impact on mean health scores than angina, asthma or diabetes and more so when combined with chronic physical illness [1]. This is also true for dermatology. A study of the UK General Practice Research Database involving more than 900 000 patients found that patients with psoriasis were 37% more likely to have a diagnosis of depression than matched controls, and that this increased with the severity of the psoriasis [2]. Depression, and to a lesser extent all forms of substance abuse, were the most overlooked diagnoses by dermatologists in 500 unselected dermatology patients examined by Musalek [3]. Screening for depressive diseases in patients with skin disease showed a prevalence of major depressive disorder in 8.4% and dysthymic disorder in 6.3%. Clinicians may underestimate the importance of depression believing that it is an almost inevitable reaction to a severe chronic skin condition. However, the importance of a mood disorder in skin disease is that it may increase distress, cause loss of function and reduce treatment adherence (see Chapter 11).
Depression may affect the skin in several ways:
- Skin disease may lead to a loss of self-esteem and so to depression.
- Depression may be a co-morbidity of skin disease.
- Depression may lead to skin disease.
- Medication for depression may lead to skin disease (e.g. lithium and psoriasis).
Clinicians need to be able to make a clear distinction between appropriate sadness in response to life events and a clinical depression. This is not to say that appropriate sadness should be dismissed or not addressed (for example, by suggesting opportunities for bereavement counselling or other support where suitable). There are three main types of mood disorder:
- Major depressive disorder.
- Dysthymia.
- Bipolar disorder.
Major depressive disorder.
DSM-5 criteria for major depressive disorders are the duration of 2 weeks or longer of one the following:
- Depressed mood most of the day, nearly every day.
-
Diminished pleasure or interest in the activities of the day (anhedonia).
Plus three or more of the following:
- More than 5% weight loss in a month or persistent increase or decrease in appetitite.
- Insomnia or hypersomnia most days.
- Psychomotor retardation or agitation.
- Fatigue or loss of energy.
- Feelings of worthlessness or inappropriate guilt (which may be delusional).
- Reduced concentration or indecisiveness.
- Suicidal ideas.
Dysthymia.
This is a chronic state of depression that may not be severe enough to meet the criteria for major depression. A depressed mood must be present for most of the day on most days for at least 2 years. The patient must not have gone more than 2 months without experiencing at least two of the following symptoms:
- Poor appetite or overeating.
- Insomnia or hypersomnia.
- Low self-esteem.
- Poor concentration.
- Feelings of hopelessness.
Bipolar disorder.
This is defined by episodes of low mood as well as those of elevated mood. Manic episodes occur in type 1, while in type 2 milder hypomanic episodes occur.
DSM-5 mania is defined by the duration of 1 week (or any duration requiring hospitalization) of three (or four if mood is only irritable) of the following:
- Inflated self-esteem/grandiosity.
- Reduced need for sleep.
- More talkative.
- Subjective experience of racing thoughts or flight of ideas.
- Increased goal-directed activity or agitation.
- Increased distractability.
- Increased risk-taking in pursuit of pleasure.
DSM-5 hypomania is defined by the duration of 4 days or longer of three (or four if mood is only irritable) of the symptoms of mania above plus all three of the following:
- Definite uncharacteristic changes in behaviour.
- Disturbance of mood observable by others.
- Episode not severe enough to disturb function markedly, hospitaliztion is not required, and no psychotic features.
Assessment of mood disorders
This is undertaken by careful history taking and mental state examination. There are several depression screening questions that dermatology HCPs can ask patients.
Patients with chronic forms of depression are at risk of subsequent major depression, considerable social disability and unhealthy lifestyle choices such as poor diet, alcohol abuse and smoking. Depression in the elderly may be more manifested by irritability, self-neglect, somatic complaints or forgetfulness than conventional symptoms. In children, depression may be insidious and present as disruptive behaviour, irritability, truancy or somatic complaints [4].
A number of robust screening instruments [5] have been developed and validated to detect depression. These can be either administered by the physician (e.g. the Beck depression inventory or the hospital anxiety and depression scale) or self-reported. One- and two-question screening tools have the merit of speed but a high false positivity. The patient health questionnaire 9 (PHQ 9) for depression appears well-validated as a diagnostic and treatment outcome measure [6].
Suicide in dermatological patients
The mistake that is often made by non-dermatology HCPs is that skin disease does not carry a mortality risk. Suicide refers to a range of self-destructive behaviours ranging from non-lethal acts, which have been called suicidal gestures, attempted suicide, parasuicide and more recently self-injury, to a lethal action in which a patient dies, defined as a completed suicide. The rates of completed suicide in the UK are 8–10 per 100 000 people and in the USA a little higher [1]. The rate is rising in young men, particularly in those with behavioural disturbance, substance misuse (25%) and persistent psychosocial difficulties. Suicide is an essential feature of depressive disease and 15% of patients with major depression kill themselves. It is therefore one of the 10 most common causes of death in the UK. Psychiatric disorders are the main risk factors but numerous studies have also identified physical illness as an important contributory factor.
Chronic illness is a risk factor in suicidal ideation and 50% of patients who attempt suicide have a physical illness, especially chronic debility and pain [2]. Not surprisingly, disfiguring chronic dermatoses have been shown to put patients at risk. In a study of 217 patients with psoriasis [3], 10% of patients reported a death wish and 6% reported active suicidal ideation at the time of the study. In another group, 2.5% of out-patients and 7.2% of in-patients with psoriasis expressed suicidal ideas. The severity of the psoriasis was reflected in the frequency of suicidal ideation and the level of measureable clinical depression. Facial acne was also associated with significant risk (5.6%) of suicidal ideation [4], which is also higher than the levels reported in general medical patients. Suicidal ideation was found in seven of 11 patients with Darier disease related to the disfigurement, intractability, social exclusion and smell of the dermatosis [5].
Unfortunately, some dermatological patients become so unhappy that they commit suicide successfully. A group of 16 patients – seven males and nine females – who committed suicide successfully after presenting with dermatological problems to two dermatologists working in the same skin department, have been described [6]. The majority of these patients had either body image disorders (BDD) or a chronic, potentially disfiguring skin disorder. It is important to recognize that patients with BDD, and particularly females with facial complaints, may be extremely depressed and at risk of suicide. Even more strikingly, BDD in children and adolescents carries a much larger risk, 67% had experienced suicidal ideation and 21% had attempted suicide [7]. Acne scarring can have just as profound an effect, or even a more profound effect, on body image, self-esteem and confidence as inflammatory acne. The positive therapeutic role of isotretinoin in the management of moderate to severe acne has been described for many years [8], and this may need to be borne in mind when considering the more recently reported association of suicidal ideation in patients treated with isotretinoin. Controversy remains over the relationship between isotretinoin and suicidal thoughts, so it is important for the prescriber to monitor suicidal ideas and refer high-risk patients to the mental health services.
Assessment of risk
Dermatologists are not always accustomed to asking patients about their intentions for self-harm. However when a depressed patient has confided their distress, it is essential that they should be asked about suicidal thoughts. Dermatology HCPs, like all HCPs, have a duty to assess suicidal risk and to make sure that their patients are safe. Dermatologists should be aware of the risk factors for suicide:
- Prior suicide attempts.
- Suicide plans.
- Ruminations about suicide.
- Depression or anxiety disorder.
- Psychotic symptoms.
- Unstable mood states, for example as in emotionally unstable personality disorder or in bipolar illness.
- Hopelessness.
- Substance misuse.
- Social isolation.
- Physical illness, especially those that are chronic, painful and debilitiating.
- Recent substantial loss, for example bereavement, job loss, relationship loss or recent health deterioration.
- Impaired insight or impulsivity.
Dermatologists must explore suicidal thoughts. It is appropriate to ask ’How difficult have things become? Do you wonder whether you can go on?’, gradually pressing to ’Have you ever thought you can't go on, or even don't want to go on?’, and eventually ’Have you ever thought about harming yourself, or even ending your life?’ It is important not to try and persuade the patient out of their suicidality by false reassurances but to assess whether they have suicidal thoughts, have an intention to act, have plans and have the means to implement the plan. Record the interview and seek permission to call a psychiatrist.
Dermatology HCPs need to act on suicidal ideation from patients by assessing if the patient is at risk of harming themselves or those around them; and if sufficiently worried, then an immediate referral to the local acute mental health team is crucial. However, there are risks of referring to an acute team, as the patient's relationship with the dermatologist may then be compromised. Where possible, and where there is a high risk of suicide, the acute mental health team will encourage the patient to be admitted voluntarily, if necessary. In these circumstances it is somewhat unusual that a patient will be admitted against his or her will via the national mental health acts.
Isotretinoin and mood changes
Following the introduction of oral isotretinoin for the systemic treatment of acne in 1982 there has been some controversy over the relationship of this treatment to the apparent development of depression and suicidality. Shortly after the introduction of oral isotretinoin there were isolated case reports of mood change and depression. Large doses of vitamin A have well-recognized toxic effects including fatigue, confusion, headache and diplopia. Reported psychological effects include aggression, personality changes, poor concentration, tearfulness, depression, ruminations of guilt and psychosis. These neuropsychological adverse effects have been suggested as a general model for retinoid side effects. The relationship between the drug and depressive illness was made more acute by reports of suicide in isolated rare cases. Some case reports have described depression developing during treatment, some with resolution during the discontinuation of the drug – so-called positive dechallenge – and a few with the recurrence of symptoms on rechallenging with the drug. In addition, there have been descriptions of an increase in frequency and/or severity with increased dosage, simulating a dose–response relationship.
A recent study reported a rise in the risk of attempted suicide in patients both on treatment and after treatment with isotretinoin (incidence ratio 1.57, 95% confidence interval 0.86–2.63) [1, 2]. However, the risk of attempted suicide had been increasing before the treatment was started, so it could not be established whether the increased risk during and after treatment was because of the isotretinoin. A systematic literature search for studies reporting primary data on depression and suicidal behaviour in patients treated with isotretinoin for acne could only analyse nine studies that met the inclusion criteria out of 214 studies examined [3]. Rates of depression varied from 1% to 11%. A period prevalence of 11% was found in a 4-month treatment period in one study and a monthly prevalence of 4% in another [2]. These rates are similar to those seen in the 12-month prevalence rates of 10% in the USA, of 6% in Canada and 9% in Europe [4]. The incidence of newly diagnosed depression whilst taking isotretinoin was 1.5% over 20 weeks [5]. The annual incidence rate of depression varies from 1.6% to 7.5% by country [6]. In other controlled studies, low self-esteem and measurable depression were improved by therapy with isotretinoin. Before and after comparisons of mood changes in matched groups of patients receiving either antibiotics or isotretinoin showed no difference in mood change.
There still remains enough doubt about the validity of a relationship between isotretinoin and mood changes to suggest that clinicians need specifically to enquire about depression at each out-patient visit. Most national dermatology associations have produced guidelines to assess this risk of mood change in patients on isotretinoin. Most dermatologists will now routinely ask about mood change at each clinic visit and if indicated use a depression inventory, for example the Beck depression inventory (BDI) or the hospital anxiety and depression (HAD) scale. Positive scores (BDI >10) should prompt withdrawal of the drug and referral to the psychiatry team. Similarly, regularly assessing patients for suicide before, during and after treatment should be routine for patients with acne and psychosocial co-morbidities, especially those for whom isotretinoin is prescribed. It is also important to remember that istretinoin is a very effective and useful drug that has helped enormously the well-being of many pateints with acne.
Psychiatric therapies in dermatology
Psychiatric treatments are traditionally divided into physical and psychological. Physical treatments now most often refer to medication, but also include some other infrequently used modalities, such as electroconvulsive therapy, light box treatment and even psychosurgery. Psychological treatments cover a wide range of interventions, including anxiety management techniques, cognitive behavioural therapies and psychoanalytical therapies. The treatment of psychiatric conditions also often involves social interventions, such as attention to housing, occupational or educational interventions and arranging appropriate access to benefits or resources. The synthesis of the three approaches is often termed the biopsychosocial approach.
Some dermatologists are beginning to become increasingly familiar with psychopharmacological interventions and also recommending talk therapies. The rise of psychodermatology as a subspecialty has seen more dermatologists experienced and trained in basic psychiatric and psychological interventions (albeit under the supervision of trained psychiatrists and psychologists). Useful guidance in this may be found in the UK National Institute for Health and Care Excellence (NICE) recommendations published for psychiatric interventions that cover primary care and secondary care. Guidelines have been produced for anxiety, bipolar affective disorder, dementia, depression (both in adults and children and in adults with chronic physical health problems), drug misuse, eating disorders, OCD (which contains specific guidelines for BDD), post-traumatic stress disorder, pre- and postnatal mental health disorders, schizophrenia and self-harm [1–8]. A useful publication is the NICE pathway on common mental health disorders [9], which is a ’one-stop shop’ for advice; this brings together all the NICE recommendations for non-psychotic mental health conditions. There is also a growing literature in psychodermatology that is written by dermatologists, psychiatrists and psychologists who work in psychodermatology clinics and which offers clear guidance for the psychopharmacological and psychological management of psychodermatological disease [10].
Drug therapies (medications)
Antidepressants
Antidepressants are widely used, not only in depression but also in anxiety and panic disorder, OCD and BDD, post-traumatic stress disorder, bulimia nervosa and pain. They are also occasionally used cautiously in depression in the context of bipolar affective disorder, but as there is a risk of triggering a manic episode they should only be prescribed in such patients by a mental health specialist. The introduction of antidepressants with a better safety profile in overdosage than the old tricyclics has led to an increase in their prescription in recent years. Arguments have been made that there is now overprescription, and there are concerns that SSRIs may be associated with suicide, particularly in adolescents [11]. These concerns have been contested but guidelines for treatment now reflect an increased caution in the prescribing of antidepressants. Fluoxetine is the only antidepressant that has been shown in clinical trials to be effective for treating depression and anxiety in children but, as with other SSRIs, it is associated with a small risk of suicidal thoughts and self-harm behaviours. It should only be prescribed by specialists in child and adolescent mental health and is never used as first line treatment in children.
General considerations in antidepressant prescribing
Before starting an antidepressant it is important to ensure that the patient understands the rationale for their use and has information about what to expect. Emphasize to the patient that depression is an illness which is treatable. Explain that antidepressants work by increasing the levels of certain brain chemicals and that this takes a while so there will be no immediate therapeutic effect. Antidepressant effects can be evident at 1 week, and by 2–3 weeks at therapeutic dose an effect is often seen. If there is minimal effect, consider increasing the dose after 3–4 weeks, but if there is no response at all after 3–4 weeks consider changing to another agent. Side effects, however, can be more immediate, for example the sedative and appetite increasing side effect of mirtazapine. Explain what side effects to expect and whether these will settle. For example, SSRIs often have an immediate effect of causing nausea and sometimes increased anxiety but this usually settles in a few days. Patients are often concerned that antidepressants are addictive. Explain that they are not but they can have a discontinuation syndrome in which if the antidepressant is stopped suddenly the patient may experience flu-like symptoms and odd electric shock sensations. These symptoms disappear on restarting the antidepressant, which should then be withdrawn gradually. Antidepressants with a shorter half-life, for example paroxetine, are particularly prone to have a discontinuation syndrome, whereas fluoxetine with its long half-life is much less likely to manifest this problem. After starting an antidepressant the patient should be monitored carefully for suicidal ideation, this is especially important for patients under the age of 25 where the risk of this effect is greater.
A review after 1 week may be important for those felt to be at high risk of self-harm, or those under 25 years of age, while a review after 2–6 weeks is suitable for others. Antidepressants should be continued for 6–9 months past the remission of symptoms as this helps reduce the risk of relapse. The Maudsley prescribing guidelines, published in the UK, provide an up-to-date and comprehensive reference for psychotropic prescribing [12].
Selective serotonin reuptake inhibitors
Selective serotonin reuptake inhibitors are now recommended for first choice use in depression and OCD, specifically including BDD and anxiety disorders, due to their relatively low side effect profile and lower toxicity in overdosage when compared with the older tricyclic antidepressants (Table 86.2). They are usually very well tolerated. The most common side effects are nausea, dyspepsia and gastrointestinal upset, headache, agitation and anxiety, sweating, rashes, insomnia and sexual dysfunction. Rarely, SSRIs may lead initially to an exacerbation of anxiety, and, in the under 18 years age group, the association with agitation leading to increased suicidal behaviour and hostility has led to the recommendation that SSRIs should only be prescribed by child and adolescent mental health specialists (CAMHs). Hyponatraemia and increased risk of bleeding due to an effect on platelets can rarely occur. There is increasing concern about the propensity for some psychotropics to prolong the QT interval, thus increasing the risk of fatal arrhythmias. The SSRIs are generally regarded as having low cardiotoxicity but recent studies have indicated that of this group citalopram and escitalopram can prolong the QT interval. Citalopram should not now be used in daily doses above 40 mg. Caution should be excercised and the prescriber should avoid combination with other drugs known to cause a prolonged QT interval.
Table 86.2 Use of selective serotonin reuptake inhibitor (SSRI) antidepressants in depression.
| Name | Dose (adult under 65 years) | Indications [27, 28] | Notes |
| Citalopram | 10–40 g/day | Depression Panic disorder |
Recommended as good choice in hepatic impairment [30] Few drug interactions Prolongs QT interval |
| Duloxetine | 30–120 mg/day | Depression Generalized anxiety disorder |
Used often by pain clinics as there is some evidence that it is helpful in neuropathic pain |
| Escitalopram | 5–20 mg/day | Depression Panic disorder Social anxiety disorder Generalized anxiety disorder. |
Isomer of citalopram Few side effects and tends to be well tolerated Few drug interactions Prolongs QT interval |
| Fluvoxamine | 50–300 mg/day | Depression OCD |
Split dosing if above 150 mg/day |
| Fluoxetine | 20–60 mg/day | Depression OCD BDD Bulimia nervosa |
Long half-life, useful in patients with poor adherence who may miss doses Does not cause discontinuation syndrome if abruptly stopped SSRI with most experience of use in pregnancy |
| Mirtazapine | 15–45 mg/day | Depression | Sexual side effects and nausea uncommon Increased appetitie and weight gain Sedative so give at night |
| Paroxetine | 10–60 mg/day | Depression OCD Panic disorder PTSD Social anxiety disorder Generalized anxiety disorder |
Marked withdrawal syndrome Associated with extrapyramidal side effects Recommended as good choice in liver impairment [29] Recommended as good choice in breast feeding [30] |
| Sertraline | 50–200 mg/day | Depression OCD Panic disorder PTSD (women) |
Recommended as good choice in hepatic impairment [30] Few side effects and drug interactions |
| Venlafaxine | 37.5–225 mg/day | Depression Generalized anxiety disorder |
Blood pressure should be monitored at higher doses |
BDD, body dysmorphic disorder; OCD, obsessive–compulsive disorder; PTSD, post-traumatic stress disorder.
Other newer antidepressants
The serotonin and norepinephrine reuptake inhibitors (SNRIs) act on both serotonin and norepinephrine (e.g. venlafaxine and duloxetine). They tend to be used as second line agents. Generally they are less well tolerated than SSRIs but better than the old tricyclic agents. They have similar side effects to the SSRIs in terms of gastrointestinal side effects and increased anxiety, but generally have fewer sexual side effects (Table 86.3). They can be alerting, which may worsen insomnia. Mirtazapine belongs to the class called noradrenergic and specific serotonergic antidepressants (NaSSAs). It has minimal sexual side effects but is sedative and causes increased appetite and weight gain. These side effects can be helpful in patients with insomnia and loss of appetite, but it is important to warn normal-weight patients of the propensity to gain weight and it is best avoided in overweight patients.
Table 86.3 Use of noradrenergic and specific serotonergic antidepressants (NaSSAs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) in depression.
| Name | Dose (adult under 65 years) | Indications | Notes |
| Duloxetine | 30–120 mg/day | Depression Generalized anxiety disorder (Also diabetic neuropathy and stress incontinence) |
SNRI Often used by pain clinics as there is some evidence it is helpful in neuropathic pain |
| Mirtazipine | 15–45 mg/day | Depression | NaSSA Relatively free of anticholinergic and sexual side effects Appetite increase and weight gain Sedating, often used if sleep is poor |
| Reboxetine | 8–12 mg/day | Depression | Not sedating Sexual side effects can occur Split dosing |
| Venlafaxine | 37.5–225 mg/day | Depression Generalized anxiety disorder |
SNRI Tends to be used as second line Split dosing, or up to 225 mg/day can be given as a modified-release form Blood pressure should be monitored at higher doses |
Tricyclic antidepressants
Tricyclic antidepressants are no longer recommended for first line use in depression. They are still useful when sedation is required, as this can provide some immediate relief from the insomnia of depressive states, and aid concordance (Table 86.4). In lower doses tricyclics are commonly used by dermatologists for pruritus and urticaria (as patients may find both the antipruritic and sedative effects useful), and for dysaesthesias and atypical pain syndromes (e.g. burning mouth syndrome). Side effects include dry mouth, blurred vision, constipation, sedation, urinary retention, open-angle glaucoma and postural hypotension. Cardiotoxicity, including heart block, is recognized in larger doses and overdoses. Prolongation of the QT interval is caused by most tricyclics and amitriptyline in particular can cause marked QT prolongation so caution needs to be exercised in the use of high doses or if there is a potential combination with other drugs that prolong the QT interval. Do not prescribe in patients where there is a risk of overdose as they are lethal in overdose. Reduction of the seizure threshold is greater than with the SSRIs so they should be avoided in epilepsy.
Table 86.4 Use of tricyclic antidepressants (TCAs) in depression.
| Name | Dose (adult under 65 years) | Indications [31] | Notes |
| Amitriptyline | 10–200 mg/day | Depression Neuropathic pain |
Noted cardiotoxicity |
| Clomipramine | 10–250 mg/day | Depression Phobic states Obsessional states |
Cardiotoxic |
| Dosulepin | 75–225 mg/day | Depression | Cardiotoxic Previous name dothiepin |
| Imipramine | 75–300 mg/day | Depression | Cardiotoxic Less sedating Split dose twice daily above 150 mg/day |
| Lofepramine | 140–210 mg/day | Depression | Less cardiotoxicity than other TCAs Split dose twice daily Less toxic in overdose Occasionally hepatotoxic |
| Nortriptyline | 10–150 mg/day | Depression Neuropathic pain |
Cardiotoxic Plasma level monitoring often available |
| Trimipramine | 50–300 mg/day | Depression | Regarded as most sedating |
Switching antidepressant drugs
The need to switch between antidepressant drugs is common, not only because response rates to the first drug are around 50% [13] but also due to the intolerance of side effects or troublesome interactions. When switching from drug to drug it is necessary both to consider the potential for withdrawal reactions from the first drug, and also the possibility of interactions between the old and new agent. It has been recommended that if antidepressants have been taken continuously for 6 weeks or more they should not be stopped abruptly unless a serious adverse event has occurred (e.g. arrhythmia). They should be withdrawn gradually and doses of new drugs are cross-tapered upwards if possible. Interactions described on switching include the serotonin syndrome, cholinergic rebound, elevated levels of drugs due to pharmacokinetic interactions and excessive side effects due to pharmacodynamic interactions. Certain drugs are particularly troublesome in switches, such as monoamineoxidase inhibitors (MAOIs) (due to their mechanism of action) and fluoxetine (due to a long half-life). A good rule of thumb is to wait 2 weeks after withdrawing an antidepressant before starting a MAOI and 2 weeks after stopping the MAOI before starting another agent, but due to its long half-life this should be extended to 6 weeks for fluoxetine. Read the manufacturer's prescribing guidelines; MAOIs are probably best left to mental health specialists.
Antipsychotic medication
Increasingly some dermatologists (with appropriate training and experience) are in a position to prescribe antipsychotics. Dermatologists are most likely to be considering prescribing antipsychotics in DI or in other delusional disorders. In these conditions, particularly where there are somatic delusions and no insight, it is unlikely that the patient will accept referral to psychiatry and therefore prescription by the dermatologist is the only possibility of attempting a pharmacological intervention. There is no robust evidence from randomized controlled trials for the treatment of DI or other delusional disorders [14]. However, as mentioned in the section on DI, there is case series evidence that antipsychotics help [15] and a review by Manschrek and Khan [16] suggested antipsychotics are effective in delusional disorders.
Second and subsequent generation antipsychotics
For most dermatology-related psychotic conditions, the agents of choice are the second and subsequent generation antipsychotic drugs as they have a lower incidence of extrapyramidal and cardiotoxic side effects (Table 86.5). Some second and subsequent generation antipsychotics may be associated with drowsiness, weight gain, metabolic syndrome (abnormal glucose tolerance and lipid metabolism) and hyperprolactinaemia. Olanzapine has been particularly problematic in causing the metabolic syndrome. Some are still associated with prologation of the QT interval and possible cardiotoxicity, although this is less common than in the first generation antipsychotics. Rarely, there is an association with impaired glucose tolerance. Clozapine, in particular, is reserved for psychiatrist only use due to its association with severe agranulocytosis which requires close monitoring of the full blood count.
Table 86.5 Use of second and subsequent generation antipsychotics in depression.
| Name | Dose (adult under 65 years) | Indications [31] | Notes |
| Amisulpiride | 400–1200 mg/day | Schizophrenia | Potent raiser of prolactin Split dosing |
| Aripiprazole | 10–30 mg/day | Schizophrenia | Can cause nausea. Is usually weight neutral |
| Olanzapine | 5–20 mg/day | Schizophrenia Mania |
Weight gain Sedating Avoid in stroke disease and dementia in the elderly |
| Quetiapine | 25–800 mg/day | Schizophrenia Mania |
Split dosing or available in modified-release form |
| Risperidone | 2–16 mg/day | Acute and chronic psychoses Mania |
Avoid in stroke disease and dementia in the elderly |
First generation antipsychotics
A wide number of first generation antipsychotics are still available, although these are unlikely to be prescribed by a dermatologist. Chlorpromazine, the first of the antipsychotics, is still available. Haloperidol has a wide range of uses, not only in psychoses, but also in tic disorders, hiccup and nausea. Some dermatologists have used it in the early part of their medical career to treat delirium in elderly in-patients. Sulpiride is very similar in structure to amisulpiride, and is less expensive. Many antipsychotics prolong the QT interval and this is particularly a problem with haloperidol and pimozide. The newer antipsychotics aripiprazole, amisulpiride and olanzapine have not been found to prolong the QT interval. Some dermatologists may still be familiar with pimozide for the management of DI but it has been associated with sudden death syndrome and so should be avoided in favour of newer, safer agents. Antipsychotics should be used with caution in patients with cardiac disease and a pre-treatment electrocardiogram (ECG) with subsequent ECG monitoring should be considered in some patients. In elderly patients with dementia there is an association beween antipsychotic use and increased risk of stroke and transient ischaemia attack. There is a suggestion that quetiapine and aripiprazole have a lower risk of cerebrovascular accident. These risks should be considered before prescribing in the elderly, and appropriate monitoring should be undertaken.
Although there are no randomized controlled trials of the use of second generation antipsychotics, there are accumulating data in the literature about their use. A systematic review found that response rates for second generation antipsyhcotics are about 75% compared with 60–100% for first generation antipsychotics [15]. The most widely used for DI are probably risperidone and olanzapine, but amisulpiride has also been recommended. DI often responds to lower doses than those used in schizophrenia (e.g. risperidone 0.5–4 mg daily, olanzapine 2.5–10 mg daily, amisulpiride 200–400 mg daily).
Anxiolytics
The benzodiazepine anxiolytics can appear initially very effective in alleviating anxiety symptoms and states, but problems with tolerance and dependence rapidly develop, and they are frequently misused. They should be avoided, but if needed use should be limited to the short term (2 weeks). Buspirone has low dependence potential and is rarely misused, and is licensed for short-term use in anxiety. Beta-blockers are used for autonomic anxiety symptoms but do not affect psychic symptoms or muscle tension. Many of the SSRIs and some other antidepressants are licensed for use in anxiety disorders (see Tables 86.2, 86.3 and 86.4) and are effective anxiolytics.
Mood stabilizers
Mood stabilizers are usually used in dermatology for dysaesthesias and postherpetic neuralgia, or are encountered when other specialists have initiated them. Many anticonvulsants are used as mood stabilizers. Pregabalin and gabapentin are the commonest medication to be commenced by dermatologists. These drugs are often started at lower doses and then titrated upwards according to clinical benefit. Some patients experience sedation and/or weight gain. Valproate in various forms is used for different reasons in dermatology (including dysaesthesias and postherpetic neuralgia). Modified-release forms of valproate are frequently used off licence for prophylaxis of bipolar disorders. Carbamazepine is licensed for the prophylaxis of bipolar disorder, and is also used in augmentation strategies for refractory depression. Other antiepileptic drugs have been used off licence for treatment and for prophylaxis. The use of lamotrigine has become widespread, and topiramate and gabapentin have also been used. Lithium is the oldest of the mood stabilizers, but is still widely used and is effective in acute mania, prophylaxis of bipolar disorder and augmentation of treatment in refractory depression. It has a narrow therapeutic index and a wide array of side effects, especially on the kidneys and thyroid, and requires careful monitoring through blood tests. It is also known for causing exacerbations of psoriasis. Lithium and anticonvulsants are known teratogens and should be avoided in women of childbearing age. They should only be used in this group with appropriate consideration of the risks and counselling about potential hazards if the patient becomes pregnant.
Psychological therapies
The use of psychotherapies in disorders that combine somatic and psychological factors is widespread, but there is often confusion about how these conditions are defined, and the evidence base is incomplete [17]. An example of the difficulties in this area is given by a recent Cochrane review of conversion disorder [18] in which all but three of only 43 identified references were excluded on grounds of quality. There is more evidence for specific therapies in certain psychiatric illnesses, and recommendations for use of therapies have been included in clinical guidelines [1–8].
The therapeutic relationship
The relationship between the clinician and patient has a potentially powerful therapeutic (or sometimes counter-therapeutic) effect, even before formal psychological techniques are considered. The effect of an empathic approach can be very powerful in those cases presenting with emotional distress related to dermatological problems. Although efforts are constantly made to reduce stigma, some patients may feel stigmatized by both their skin and psychiatric symptoms. The opportunity to express their anxieties and fears may provide significant relief. It may be necessary for the clinician to question gently any defensive explanations that a patient uses for their symptoms. The effect of touch during examination has been described as relieving the anxiety of patients who feel stigmatized by their skin lesions. The effect of actively listening within a therapeutic relationship allows patients to address their own problems, and is the basis of client-centred counselling, described by Rogers [19]. Of course, the dermatologist will need to give clinical advice, but a confident, authoritative rather than authoritarian approach, where the clinician offers explanation and clinical advice when indicated, but is able to tolerate this advice initially being partially taken or prevaricated on, will aid sustained engagement.
It should also be noted that a small, but significantly morbid, population of patients can experience a marked negative effect through the therapeutic relationship. With such patients, who usually have severe neurotic or personality pathologies, the clinician can feel pressed into making unusual decisions, ordering unusual investigations and going to extreme lengths to manage the patient's anxiety, anger or demands. It is not unusual for such patients to initially present with the impression that the clinician is ’the best they have seen’ or ’the only one who has understood’ – a relationship that can rapidly change to one of dissatisfaction, complaint or litigation. In such patients, although presenting as seeking a ’cure’, there may be an unspoken or unconscious need to remain in the sick role, and the clinician has an apparently impossible task. It is important for the clinician to recognize when such dynamics are potentially distorting practice, and seek appropriate advice if a severe neurosis or personality disorder are suspected.
Cognitive behavioural therapy
Increasingly, CBT has become the first line psychological therapy in depression and anxiety disorders, including BDD [1–8]. Randomized trials have found efficacy of CBT in BDD [20] and it is recommended in national guidelines for the treatment of BDD [1].
The theory of CBT is that the patient automatically responds to certain situations and stimuli with ingrained negative thoughts. These thoughts in turn lead to negative emotions such as fear or depression, and behavioural consequences such as avoidance or rituals. Treatment in CBT is based around the process of sympathetically challenging these negative automatic thoughts and exploring alternative responses that may not lead to behavioural and emotional pathology. The therapeutic process may include exposure and response prevention, wherein the patient is exposed to a troubling thought or stimulus (often, initially, in imagination or abstract) and encouraged to explore alternative thoughts and responses to their ingrained pathological reaction. Often, adjunctive relaxation and anxiety management techniques are an integral part of the therapy. CBT techniques are widely used and have been published in ’self-help’ formats, for example Overcoming Depression and Low Mood [21]. The clinician can incorporate CBT principles and techniques in their clinical practice. Computer packages have been developed to deliver CBT, although guidelines state the evidence is better in depression and anxiety than in OCD [22].
Formal CBT treatment, when provided by a trained therapist, can consist of six to 20 or more hour-long sessions, depending on the severity of the case, complexity, co-morbidities and response. The main concern for many health care providers is insufficient therapist hours to meet demand, resulting in lengthy waiting lists. The therapy can be provided in group as well as individual settings. In the UK, provision of psychological therapies has been enhanced through the Improving Access to Psychological Therapies (IAPT) programme. This is a government-funded initiative to increase the provision of psychotherapy and has mostly provided increased access to CBT delivered by psychologists. Further information and a list of services are provided via the IAPT website (www.iapt.nhs.uk; last accessed August 2015). Although usually effective, CBT is not suitable for all cases and alternate modalities of therapy still need to be considered.
Interpersonal psychotherapy and interpersonal counselling
These forms of therapy are based on the work of Klerman and associates [23]. The focus of interpersonal psychotherapy (IPT) is on the relationships of the patient and how they affect mood states. Problems in relationships are categorized as one of dispute, change in role, grief or deficit. The therapist then assists the patient in working through the problems using techniques such as role play and analysis of communications within relationships. Like CBT, the therapy takes place over a number of hour-long sessions, usually 12 to 16.
Interpersonal counselling (IPC) is a modification of IPT, of a simpler form that can be integrated into the work of health professionals. It was designed for primary care, but can be used in other health settings. IPT has been shown to be effective, and equivalent to the use of CBT in depression and eating disorders. Unlike CBT, it has not yet been shown to be effective in OCD or BDD. It has been suggested that IPT be offered as an alternative to CBT for patients who prefer this approach. However, provision, especially outside the USA, is often limited by a shortage of trained practitioners.
Dynamic psychotherapies and psychoanalysis
There is not scope here to describe the range of these psychotherapies available. Some awareness of, or even familiarity with, the concepts first described by Freud are common in western and European cultures. There are numerous therapist and theorists who have written on the subject. Psychodynamic concepts such as transference, counter-transference, projection and identification can help the clinical interview, and good descriptions can be found for the interested in textbooks such as Introduction to Psychotherapy [24].
Short-term forms of dynamic therapies (defined as fewer than 40 sessions) have been shown to have efficacy in a wide range of common mental health disorders [25]. Many forms of dynamic therapies and psychoanalytical therapy are long lasting and intensive, with three or more sessions weekly. Due to the complexity of the longer forms of therapy, especially around conducting controlled studies and defining outcomes, there are difficulties with an evidence-based approach to demonstrating efficacy [26]. Whilst this is acknowledged by practitioners writing in this field, the point is often made that these forms of therapy are complex, and used in complicated conditions where the ’drug paradigm’ or ’single intervention for single condition’ approach may not be strictly relevant.
Varieties of psychiatric syndrome presenting to the dermatologist, either as part of or alongside a cutaneous presentation, can be effectively treated by clinicians familiar with the stratagems used in primary care. Although specialist knowledge and training is required to deliver formal psychotherapy, techniques from psychotherapy – especially empathy, a non-judgemental approach, understanding, patience and reflection – can be used to augment safe prescribing where indicated. Specialist referral should be arranged when symptoms are severe or specialist drugs or therapies needed.
Alternative therapies
There has been a long tradition of the use of complementary therapies in dermatology, but especially for those diseases where there is a psychological component. Most reports of therapy are anecdotal, often single cases with no randomized controlled trials. Therapies with a neurogenic basis are claimed to work through neuroimmune mechanisms although no hard evidence is available. Acupuncture, biofeedback and hypnosis in skin disease are summarized by Shenefelt [1] and Freid [2]. The mechanisms of action may be related to the beneficial effects of supportive psychotherapy and relaxation rather than any specific therapeutic component measurable for each treatment type. Hypnotherapy has been the most frequently studied in western literature. Despite the lack of trials, there are strong advocates for the use of hypnosis as an adjunct to control itch [3] and pain [4]. Hypnotherapy for warts in children showed a 53% success at 3 months compared with none in the control group [5]. The practicality and cost was not assessed.
Alternative herbal medications are used both topically and systemically. In an evidence-based review of the literature [6] there was no compelling evidence for the efficacy of diet, herbal medicines or dietary supplements in atopic eczema. The authors suggested promising data for treatments with a psychological component such as hypnosis, autogenic training and biofeedback. For chronic venous insufficiency, oral horse chestnut seed extract appeared to have a real effect as opposed to topical aloe vera gel or tea tree oil. Two fuller reviews of phytopharmaceutical agents explored not only the therapeutic uses of herbs but also the toxic and allergic skin reactions [7, 8].
Resources
Further information
- Association of Psychoneurocutaneous Medicine of North American (APMNA): www.psychodermatology.us.
- European Society for Dermatology and Psychiatry: http://www.psychodermatology.net/.
- Psychodermatology UK Society: www.psychodermatology.co.uk
- (All last accessed August 2015.)
Patient resources
- Atopic Skin Disease: www.atopicskindisease.com.
- Changing Faces: http://www.changingfaces.org.uk. Changing Faces is a UK-based charity that has advice for patients with visible differences. The coping strategies used are 3-2-1 Go! and REACHOUT.
- Skin Support: www.skinsupport.org.uk.
- (All last accessed August 2015.)
References
Introduction
Psychodermatology multidisciplinary teams
- All Party Parliamentary Group on Skin (APPGS). The Psychological and Social Impact of Skin Disease on People's Lives. London: APPGS, 2013. www.appgs.co.uk/publications (last accessed August 2015).
- Bewley A, Affleck A, Bundy C, Higgins E, McBride S. Psychodermatology services guidance: the report of the British Association of Dermatologists' Psychodermatology Working Party. Br J Dermatol 2013;168(6):1149–503.
Classification
- Musalek M, Hoble B, Mossbacher U. Diagnostics in psychodermatology. Dermatol Psychosom 2001;2:110–15.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edn. Washington, DC: American Psychiatric Association, 2014. www.dsm5.org (last accessed August 2015).
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization, 1992.
- World Health Organization. The International Classification of Diseases 11th revision is due by 2017. http://www.who.int/classifications/icd/revision/en/ (last accessed August 2015).
Psychological co-morbidities of chronic skin disease and the ‘golden rules of psychodermatology’
- Linnet J, Jemec GB. Anxiety level and severity of skin condition predicts outcome of psychotherapy in atopic dermatitis. Int J Dermatol 2001;40:632–6.
- Kleyn CE, McKie S, Ross AR, et al. Diminished neural and cognitive responses to facial expressions of disgust in patients with psorisis: a functional magnetic resonance imaging study. J Invest Dermatol 2009;129(11):2613–19.
- Picardi A, Pasquini P, Abeni D et al. Stress, social support, emotional regulation, and exacerbation of diffuse plaque psoriasis. Psychosomatics 2005;46:556–64.
- Fordham B, Griffiths CE, Bundy C. Can stress reduction interventions improve psoriasis? A review. Psychol Health Med 2013;18(5):501–14.
- Fortune DS, Richards HL, Kirby B, et al. Psychological distress impairs clearance of psoriasis in patients treated with photochemotherapy. Arch Dermatol 2003;139:752–6.
- Chung MC, Symons C, Gilliam J, Kaminski ER. Stress, psychiatric co-morbidity and coping in patients with chronic idiopathic urticaria. Psychol Health 2010;25(4):477–90.
- Farrant P, McHale S. Psychological impact of hair loss. In: Bewley A, Taylor RE, Reichenberg JS, Magid M, eds. Practical Psychodermatology. Oxford: Wiley, 2014:81–9.
Stigmatization, visible differences and coping strategies
- Kent G. Stigmatisation and skin conditions. In: Walker C, Papadopoulos L, eds. Psychodermatology. Cambridge: Cambridge University Press, 2005:44–52.
- Gray AJ. Stigma in psychiatry. J R Soc Med 2002;95:72–7.
- Baumeister R, Twenge J, Nuss C. Effect of social exclusion on cognitive processes. J Social Clin Psychol 2002;8:17–27.
- King M, Dinos S, Shaw J, et al. The stigma scale of mental illness. Br J Psychiatry 2007;190:248–54.
Disability, quality of life and assessment in psychodermatology
- Basra MK, Fenech R, Gatt RM, Salek MS, Finlay AY. The Dermatology Life Quality Index 1994–2007: a comprehensive review of validation data and clinical results. Br J Dermatol 2008;159:997–1035.
- Chularojanamontri L, Griffiths CE, Chalmers RJ. Responsiveness to change and interpretability of the simplified psoriasis index. J Invest Dermatol 2014;134(2):351–8.
- Bowling A. Measuring Disease. A Review of Disease Specific Quality of Life Scales. Buckingham: Open University Press, 2001.
- Appendix. Screening questionnaires and scales. In: Bewley AP, Taylor RE, Reichenberg J, Magid M, eds. Practical Psychodermatology. Oxford: Wiley, 2014:238–67.
Delusional beliefs
- Freudenmann RW, Lepping P. Delusional infestation. Clin Microbiol Rev 2009;22(4):690–732.
Delusional infestation
- Bewley A, Lepping P, Freudenmann RW, Taylor R. Delusional parasitosis: time to change the name of the condition to delusional infection. Br J Dermatol 2010;163(1):1–2.
- Freudenmann RW, Lepping P. Delusional infestation. Clin Microbiol Rev 2009;22(4):690–732.
- Eccles JA, Garfinkel SN, Ward J, Taylor RE, Bewley AP, Critchley HD. Sensations of skin infestation linked to abnormal cortical and midbrain reactivity and differences in self-representation in patients with delusional infestation (in press).
- Freudenmann RW, Lepping P, Huber M, et al. Delusional infestation and the specimen sign: a European multicentre study in 148 consecutive cases. Br J Dermatol 2012;167(2):247–251
- Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis: outcome and efficacy. J Clin Psychopharmacol 2008;28(5):500–8.
- Ahmed A, Bewley A. Delusional infestation and patient adherence to treatment: an observational study. Br J Dermatol 2013;169(3):607–10.
- Wong S, Bewley A. Patients with delusional infestation (delusional parasitosis) often require prolonged treatment as recurrence of symptoms after cessation of treatment is common: an observational study. Br J Dermatol 2011;165(4):893–6.
- Musalek M. Delusional parasitosis. In: Koo J, Lee CS, eds. Psychocutaneous Medicine. Basel: Decker, 2003:143–52.
- Lepping P, Freundenmann RW, Heuber M. Delusional infestation. In: Bewley A, Taylor RE, Reichenberg JS, Magid M, eds. Practical Psychodermatology. Oxford: Wiley, 2014:117–26.
- Koo J, Lee CS. Delusions of parasitosis. A dermatologist's guide to treatment. Am J Clin Dermatol 2001;2:285–90.
Olfactory delusions
- Pryse-Phillips W. An olfactory reference syndrome. Acta Psychiatr Scand 1971;47(4):484–509.
- Videbech T. Chronic olfactory paranoid syndromes. Acta Psychiatr Scand 1966;42:183–212.
- Senol M, Fireman P. Body odour in dermatological diagnosis. Cutis 1999;63:107–11.
- Konuk N. Frontotemporal hypoperfusion in a patient with olfactory reference syndrome. Gen Hosp Psychiatry 2006;28:174–7.
- Feusner JD, Phillips KA, Stein DJ. Olfactory reference syndrome: issues for DSM-V. Depress Anxiety 2010;27(6):592–9.
- Brewer W, Castle D, Pantelis C. Olfaction and the Brain. New York: Cambridge University Press, 2006:267–70.
- Leopold D. Distortion of olfactory perception: diagnosis and treatment. Chem Senses 2002;27(7):611–15.
- Lochner C, Stein DJ. Olfactory reference syndrome: diagnostic criteria and differential diagnosis. J Postgrad Med 2003;49:328–31.
- Phillips KA, Menard W. Olfactory reference syndrome: demographic and clinical features of imagined body odor. Gen Hosp Psychiatry 2011;33(4):398–406.
Morgellons syndrome
- Kellet CE. Sir Thomas Browne and the disease called Morgellons. Ann Hist Med 1935;7:467–79.
- Murase JE, Koo J. Morgellons disease: a rapport enhancing term for delusions of parasitosis. J Am Acad Dermatol 2006;55:913–14.
- Elkan D. Morgellons disease: real or delusion. New Scientist 2007;195:45–9.
- Koblenzer C. The challenge of Morgellon's disease. J Am Acad Dermatol 2006;55:920–2.
- Pearson ML, Selby JV, Katz KA, et al. Clinical, epidemiologic, histopathologic and molecular features of an unexplained dermopathy. PLOS One 2012;7(1):e29908.
Obsessive and compulsive behaviour
- Veale D, Neziroglu F. Body Dysmorphic Disorder: A Treatment Manual. Chichester: John Wiley and Sons, 2010.
- Phillips KA, Hart AS, Simpson HB, Stein DJ. Delusional versus nondelusional body dysmorphic disorder: recommendations for DSM-5. CNS Spectr 2014;19(1):10–20.
Body dysmorphic disorder
- Veale D, Neziroglu F. Body Dysmorphic Disorder: A Treatment Manual. Chichester: John Wiley and Sons, 2010.
- Veale D, Bewley A. Body dysmorphic disorder. BMJ 2015;350:h2278.
- Koblenzer CS. The dysmorphic syndrome. Fitzpatrick J Clin Dermatol 1994:Mar/Apr:14–19.
- National Institute of Health and Care Excellence (NICE). Obsessive–Compulsive Disorder: Core Interventions in the Treatment of Obsessive–Compulsive Disorder and Body Dysmorphic Disorder 2005. Clinical Guideline No. 31. London: NICE.
- Phillips KA, Hart AS, Simpson HB, Stein DJ. Delusional versus nondelusional body dysmorphic disorder: recommendations for DSM-5. CNS Spectr 2014;19(1):10–20.
- Phillips KA, Menard W, Quinn E, Didie ER, Stout RL. A 4-year prospective observational follow-up study of course and predictors of course in body dysmorphic disorder. Psychol Med 2013;43(5):1109–17.
- Monzani B, Krebs G, Anson M, Veale D, Mataix-Cols D. Holistic versus detailed visual processing in body dysmorphic disorder: testing the inversion, composite and global precedence effects. Psychiatry Res 2013;210(3):994–9.
- Phillips KA, Albertini RS, Rasmussen SA. A randomized placebo-controlled trial of fluoxetine in body dysmorphic disorder. Arch Gen Psychiatry 2002;59:381–8.
- Phillips KA. Pharmacologic treatment of body dysmorphic disorder: a review of the evidence and a recommended treatment approach. CNS Spectr 2002;7:453–60.
- Veale D, Gournay K, Dryden W, et al. BDD: a CBT model and pilot RCT. Beh Res Ther 1996;34:17–29.
- Rosen JC, Reiter J, Orosan P. Cognitive behavioural body image therapy for BDD. J Consult Clin Psychol 1995;63:263–9.
- Veale D, Ellison N, Werner T, et al. Development of a cosmetic procedure screening questionnaire (COPS) for body dysmorphic disorder. J Plast Reconstr Aesthet Surg 2012;65(4):530–2.
- Dufresne RG, Jr, Phillips KA, Vittorio CC, Wilkel CS. A screening questionnaire for body dysmorphic disorder in a cosmetic dermatologic surgery practice. Dermatol Surg 2001;27:457–62.
- Perugi G, Akiskal HS, Giannotti D, et al. Gender-related differences in body dysmorphic disorder (dysmorphophobia). J Nerv Mental Dis 1997;185:578–82.
Lichen simplex chronicus and nodular prurigo
- Allerhand ME, Gough HG, Grais ML. Personality factors in neurodermatitis. Psychosom Med 1950;12:386–9.
- Gibbon KL, Bewley AP. Vulval dermatoses. In: Hollingworth A, ed. Differential Diagnosis in Obstetrics and Gynaecology; an A to Z, 2nd edn. London: Hodder Arnold, 2008.
- Liao YH, Lin CC, Tsai PP, Shen WC, Sung FC, Kao CH. Increased risk of lichen simplex chronicus in people with anxiety disorder: a nationwide population-based retrospective cohort study. Br J Dermatol 2014;170(4):890–4.
- Fried RG. Nonpharmacologic treatment in psychodermatology. Dermatol Clin 2002;20:177–85.
- Van-Os H, Eland P, Kennedy C. Effectiveness of nursing programme coping with itch. Br J Dermatol 2007;156:1235–44.
- Melin L, Noren P. Behavioural treatment of scratching in patients with atopic dermatitis. Br J Dermatol 1986;115:467–74.
- Lavda AC, Webb TL, Thompson AR. A meta-analysis of the effectiveness of psychological interventions for adults with skin conditions. Br J Dermatol 2012;167(5):970–9.
Skin picking disorder
- Flessner C, Woods D. Phenomenological characteristics, social problems, and economic impact of chronic skin picking. Behav Modif 2006;30:944–63.
- Bohne A, Keuthen N, Wilhelm S. Pathologic hair-pulling, skin picking and nail biting. Ann Clin Psychiatry 2005;17:227–32.
- Odlaug B, Grant J. Childhood-onset pathological skin picking: clinical characteristics and psychiatric comorbidity. Compr Psychiatry 2007;48:388–93.
- Wilhelm S, Keuthen N, Deckersbach T. Self-injurious skin picking: clinical characteristics and comorbidity. J Clin Psychiatry 1999;60:654–9.
- Calikusu C, Yucel B. The relationship of psychogenic excoriation to psychiatric disorders. Compr Psychiatry 2003;44:256–61.
- Deckersbach T, Wilhelm S, Keuthen N. Cognitive behaviour therapy for self-injurious skin picking. Behav Modif 2002;26:361–77.
- Fried RG. Nonpharmacologic treatment in psychodermatology. Dermatol Clin 2002;20:177–85.
- Lochner C, Grant JE, Odlaug BL, Stein DJ. DSM-5 field survey: skin picking disorder. Ann Clin Psychiatry 2012;24(4):300–4.
- Grant JE, Odlaug BL, Chamberlain SR, Keuthen NJ, Lochner C, Stein DJ. Skin picking disorder. Am J Psychiatry 2012;169(11):1143–9.
- Jafferany M, Shireen F, Ibrahim A. An open-label trial of topiramate in the treatment of skin picking in pervasive developmental disorder not otherwise specified. Prim Care Companion J Clin Psychiatry 2010;12(2):104–6.
Acne excoriée
- Brocq L, Jacquet L. Notes pour servir a' l'histoire des neurodermites. Arch Derm Syph 1891;97:193–5.
- Sneddon J, Sneddon I. Acne excoriée; a protective device. Clin Exp Dermatol 1983;8:65–8.
- Wrong NM. Excoriated acne of young females. Arch Dermatol Syphiligr 1954;70:574–82.
- Gieler U, Consoli SG, Tomás-Aragones L, et al. Self-inflicted lesions in dermatology: terminology and classification – a position paper from the European Society for Dermatology and Psychiatry (ESDaP). Acta Derm Venereol 2013;93(1):4–1.
- Kent A, Drummond LM. Acne excoriée: a case report using habit reversal. Clin Exp Dermatol 1989;14:163–4.
- Bower L, Alster T. Treatment of facial scarring from acne excoriée with pulse dye laser and cognitive psychotherapy. Dermatol Therapy 2004;30:934–8.
- Gupta MA. Emotional regulation, dissociation, and the self-induced dermatoses: clinical features and implications for treatment with mood stabilizers. Clin Dermatol 2013;31(1):110–17.
- Sheefelt P. Use of hypnosis in acne excoriée. Am J Clin Hypnosis 2004;46:439–45.
Trichotillomania/trichotillosis
- Hautmann G, Hercogova J, Lotti T. Trichotillomania. J Am Acad Dermatol 2002;46:807–21.
- Bruce T, Barwick L, Wright H. Diagnosis and management of trichotillomania in children and adolescents. Paediatr Drugs 2005;7:365–76.
- Harrison JP, Franklin ME. Pediatric trichotillomania. Curr Psychiatry Rep 2012;14(3):188–96.
- Lochner C, Seedat S, du Toit P, et al. Obsessive-compulsive disorder and trichotillomania. Psychiatry 2005;5:2–16.
- Naik S, Gupta V. Rapunzel syndrome reviewed and redefined. Dig Surg 2007;24:157–61.
- Stanley MA, Prather RC, Wagner AL, et al. Can the Yale–Brown Obsessive Compulsive Scale be used to assess trichotillomania? Behav Res Ther 1993;31:171–7.
- Morris SH, Zickgraf HF, Dingfelder HE, Franklin ME. Habit reversal training in trichotillomania: guide for the clinician. Expert Rev Neurother 2013;13(9):1069–77.
- Block M, Landero S, Dombranski P, et al. Systematic review: pharmacological and behavioural treatment for trichotillomania. Biol Psychiatry 2007;62:839–46.
- Rothbart R, Amos T, Siegfried N, et al. Pharmacotherapy for trichotillomania. Cochrane Database Syst Rev 2013;Issue 11: CD007662.
- Gupta MA. Emotional regulation, dissociation, and the self-induced dermatoses: clinical features and implications for treatment with mood stabilizers. Clin Dermatol 2013;31(1):110–17.
Onychotillomania and onychophagia
- Pacan P, Grzesiak M, Reich A, Kantorska-Janiec M, Szepietowski JC. Onychophagia and onychotillomania: prevalence, clinical picture and comorbidities. Acta Derm Venereol 2014;94(1):67–71.
- Baran R. Nail biting and picking as a cause of longitudinal melanonychia. Dermatologica 1990;181:126–8.
- Twohig H, Woods D. Evaluating the efficacy of habit reversal in chronic nail biting. J Clin Psychiatry 2003;64:40–8.
Health anxieties
- Demet MM, Deveci A, Taskin E, et al. Obsessive–compulsive disorder in a dermatology outpatient clinic. Gen Hosp Psychiatry 2005;27:426–30.
- Affleck A, Howells L. Psychodermato-oncology: psychological reactions to skin cancer. In: Bewley AP, Taylor RE, Reichenberg J, Magid M, eds. Practical Psychodermatology. London: Wiley, 2014:206–15.
- Hay J, Buckley T, Ostroff J. The role of cancer worry in cancer screening: a theoretical and empirical review of the literature. Psycho-oncology 2004;14:517–34.
- Charman CR, Morris A, Williams H. Topical steroid phobia in dermatology outpatients with atopic eczema. Br J Dermatol 1999;141:105.
- Kestenbaum T. Obsessive-compulsive disorder in dermatology. Semin Cutan Med Surg 2013;32(2):83–7.
Eating disorders
Anorexia nervosa and bulimia
- Hoek H. Incidence, prevalence and mortality of anorexia nervosa and other eating disorders. Curr Opin Psychiatry 2006;19:389–94.
- Keski-Rahkonnen A, Hoek H, Susser E, et al. Epidemiology and course of anorexia nervosa in the community. Am J Psychiatry 2007;164:1259–64.
- Gupta MA, Gupta AK. Dermatologic signs in anorexia nervosa and bulimia nervosa. Arch Derm 1987;123:1386–90.
- Steinhausen H. The outcome of anorexia nervosa in the 20th century. Am J Psychiatry 2002;159:1283–93.
- Claes L, Vandereycken W, Vertommen H. Self-injurious behaviours in eating disordered patients. Eating Behav 2001;2:263–72.
- Pompili M, Mancinelli I. Suicide in anorexia nervosa: a meta-analysis. Int J Eating Disorders 2003;36:99–103.
- Gupta MA, Gupta AK. Dissatisfaction with skin appearance amongst patients with eating disorders. Br J Dermatol 2001;145:110–13.
- Luck AJ, Morgan JF, Reid F, et al. The SCOFF questionnaire and clinical interview for eating disorders in general practice. BMJ 2002;325:755–6.
Psychogenic itch
Psychogenic pruritus
- Schneider D, Dresch G, Evers S, et al. Psychosomatic cofactors and psychiatric comorbidity in patients with chronic itch. Clin Exp Dermatol 2006;31:762–7.
- Stander S, Weisshaar F, Mettang T, et al. Clinical classification of itch. Acta Derm Venereol 2007;87:291–4.
- Misery L, Alexandre S, Dutray S, et al. Functional itch disorder or psychogenic pruritus: suggested diagnostic criteria. Acta Derm Venereol 2007;87:341–4.
- Vanos H, Eland P, Grypdonck M. Prevalence and predictors of psychosocial morbidity in patients with chronic pruritic skin diseases. J Eur Acad Dermatol 2006;20:810–17.
- Gieler U, Neimeir V. Psychosomatic aspects of pruritus. Dermatol Psychosomat 2002;3:6–13.
- Gupta MA, Gupta AK. The use of antidepressant drugs in dermatology. J Eur Acad Dermatol 2001;15:512–18.
- Freid RG. Non-pharmacologic treatments in psychodermatology. Dermatol Clin 2002;20:177–85.
- Greaves MW. Pathogenesis and treatment of pruritus. Curr Allergy Asthma Rep 2010;10(4):236–42.
- Shaw RJ, Dayal S, Good J, Bruckner AL, Joshi SV. Psychiatric medications for the treatment of pruritus. Psychosom Med 2007;69(9):970–8.
- Calabrò RS, Bramanti P, Digangi G, Mondello S, Italiano D. Psychogenic itch responding to topiramate. Psychosomatics 2013;54(3):297–300.
Factitious skin disease
Dermatitis artefacta
- Millard J, Millard L. Factitious skin disorder (dermatitis artefacta). In: Bewley A, Taylor RE, Reichenberg J, Magid M, eds. Practical Psychodermatology. London: Wiley, 2014:142–50.
- Saez M, Orozco L, Mora I, et al. Dermatitis artefacta in paediatric patients. Paediatr Dermatol 2004;21:205–1.
- Halligan P, Bass C, Oakley D, eds. Malingering and Illness Deception. Oxford: Oxford University Press, 2003.
- Koblenzer C. Dermatitis artefacta: clinical features and approaches to treatment. Am J Clin Dermatol 2000;1:47–55.
- Verraes S, Derancourt C, Poot F, et al. Dermatitis artefacta: a retrospective study of 31 patients. Ann Dermatol Vénéréol 2006;133:235–8.
- Ahmed A, Bewley A, Taylor R. Dermatitis artefacta in a vulnerable adult with a dissociative state. Clin Exp Dermatol 2013;38(8):921–3.
- Angus J, Affleck A, Leach IH, Millard L. Factitious disease presenting as non-healing wounds. J Eur Acad Dermatol Venereol 2005;19:70.
- Bandmann HJ, Wahl B. Contact urticaria artefacta (witchcraft syndrome). Contact Dermatitis 1982;8:145–6.
- Simani VK. Witchcraft syndrome. Int J Dermatol 1998;37:229–31.
- Maurice PDL, Rivers JK, Jones C, Cronin E. Dermatitis artefacta with artefact of patch tests. Clin Exp Dermatol 1987;12:204–6.
- Meigel WN, Koops DH. Scarification artifacts in the test reaction in an expert opinion of occupational dermatosis. Hautarzt 1976;27:349–51.
- Mohandas P, Bewley A, Taylor R. Dermatitis artefacta and artefactual skin disease: the need for a psychodermatology multi-disciplinary team to treat a difficult condition. Br J Dermatol 2013;169(3):600–6.
- Greene RL. Assessment of malingering and defensiveness. In: Rogers R, ed. Clinical Assessment of Malingering and Deception. New York: Guilford Press, 1997:169–207.
- Mayou R, Sharp M, eds. The ABC of Psychological Medicine. London: BMJ, 2002:325–7.
Malingering
- Asher R. Malingering. In: Avery Jones F, ed. Richard Asher Talking Sense. Bath: Pitman Press, 1972:145–5.
- Bass C. Factitious disorders and malingering. In: Halligan P, Bass C, eds. Contemporary Approaches to Hysteria. Oxford: Oxford University Press, 2001:127–42.
- Raine A. Malingering and criminal behaviour as psychopathology. In: Halligan P, Bass C, Oakley D, eds. Malingering and Illness Deception. Oxford: Oxford University Press, 2003:93–107.
- Cunnien AJ. Psychiatric and medical syndromes associated with deception. In: Rogers R, ed. Clinical Assessment of Malingering and Deception. New York: Guilford Press, 1997:33–46.
- Palmer I. War based hysteria: the military perspective. In: Halligan P, Bass C, eds. Contemporary Approaches to Hysteria. Oxford: Oxford University Press, 2001:12–35.
- Eisendrath SJ. When Munchausen becomes malingering. Factitious disorders that penetrate the legal system. Bull Am Acad Psychiatry Law 1996;24:471–81.
- Hutchinson GL. Disorders of Simulation. Madison: Psychosocial Press, 2001:195–221.
Pseudologia fantastica and Münchausen syndrome
- Asher R. Munchausen's syndrome. Lancet 1951;1:339–41.
- Menninger K. Polysurgery and polysurgical addiction. Psychoanal Q 1934;4:173–99.
- Newmark N, Adityanjee KJ. Pseudologica fantastica and factitious disorder. Review of the literature. Compr Psychiatry 1999;40:89–95.
- Feldman MD. Munchausen by internet. Detecting factitious illness and crisis on the Internet. South Med J 2000;93:669–72.
Fabricated and induced illness
- Meadow R. Munchausen syndrome by proxy. The hinterland of child abuse. Lancet 1977;2:343–5.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edn. Washington, DC: American Psychiatric Association, 2014. www.dsm5.org (last accessed August 2015).
- Parnell TF, Day DO, eds. Munchausen by Proxy Syndrome. Newbury Park, CA: Sage Publications, 1998:47–67.
- Schreier H, Libow J. Hurting for Love. Munchausen by Proxy. New York: Guilford Press, 1993.
- Meadow SR. Who's to blame – mothers, Munchausen or medicine? J R Coll Phys Lond 1994;28:332–7.
- Feldman MD, Brown RMA. Munchausen by proxy in an international context. Child Abuse Neglect 2002;26:509–24.
- Libow JA. Beyond collusion. Active illness falsification. Child Abuse Neglect 2002;26:525–36.
- David T. Child abuse and paediatrics. J R Soc Med 2005;96:229–31.
- Galvin H, Newton A, Vandeven A. Update on Munchausen syndrome by proxy. Curr Opin Paediatr 2005;17:252–7.
- Sigal MD, Altmark D, Carmel I. Munchausen syndrome by adult proxy. J Nerv Mental Dis 1986;186:696–8.
Medicolegal issues in suspected factitious skin diseases
- Jones MA. Medico-legal and occupational perspectives. In: Halligan P, Bass C, Oakley D, eds. Malingering and Illness Deception. Oxford: Oxford University Press, 2003:209–54.
Deliberate self-harm
- Favazza AR. The coming of age of self-mutilation. J Nervous Mental Dis 1998;18:259–68.
- Winchel RM, Stanley M. Self-injurious behaviour: a review of the behaviour and biology of self-mutilation. Am J Psychiatry 1991;148:306–17.
- Herpertz S. Psychopathological and nosological characteristics in subtypes of self-injurers. Acta Psychiatr Scand 1995;91:57–68.
- Boyce P, Oakley-Browne MA, Hatcher S. The problem of deliberate self-harm. Curr Opin Psychiatry 2001;14:107–11.
- House A, Owens D, Storer D. Psycho-social intervention following attempted suicide: is there a case for better services? Int Rev Psychiatry 1992;4:15–22.
- Kocalevent RD, Fliege H, Rose M, et al. Autodestructive syndromes. Psychother Psychosom 2005;74:202–11.
- Joyce PR, McKenzie JM, Mulder RT, et al. Genetic, developmental and personality correlates of self-mutilation in depressed patients. Aust NZ J Psychiatry 2006;4:225–9.
- Simeon D, Stanley B, Frances A, et al. Self-mutilation in personality disorder: psychological and biological correlates. Am J Psychiatry 1992;149:221–6.
- Starr D. Understanding those who self-mutilate. J Psychosoc Nurs Ment Health Serv 2004;42:32–40.
- Isacsson G, Rich C. Management of patients who deliberately harm themselves. BMJ 2001;322:213–15.
Other psychodermatology and psychocutaneous diseases
Cutaneous disease and alcohol misuse
- Smith KE, Fenske NA. Cutaneous manifestations of alcohol abuse. J Am Acad Dermatol 2000;43:1–16.
- Higgins E, du Vivier A. Alcohol intake and other skin disorders. Clin Dermatol 1999;17:437–41.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edn. Washington, DC: American Psychiatric Association, 2014. www.dsm5.org (last accessed August 2015).
- Volpicelli JR. Alcohol abuse and alcoholism: an overview. J Clin Psychiatry 2001;62(Suppl. 20):4–10.
- Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA 1984:252;1905–7.
- Rao GS. Cutaneous changes in chronic alcoholics. Ind J Dermatol Venereol Leprol 2004;70:79–84.
- Kostovic K, Lipozecik J. Skin disease in alcoholics. Acta Dermatovenereol Croat 2004;12:181–90.
- Hill L, Kennedy P. The role of coping strategies in mediating subjective disability in psoriasis. Psych Health Med 2002;7:261–9.
- Kirby B, Richards HL, Mason DL, et al. Alcohol consumption and psychological distress in patients with psoriasis. Br J Dermatol 2008;158:138–40.
- Gupta MA, Schnork NJ, Gupta AK, Ellis CN. Alcohol intake and treatment responsiveness in psoriasis. J Am Acad Dermatol 1993;28:730–5.
Depression in dermatological patients
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases and decrements in health: results from the World Health Surveys. Lancet 2007;370:851–8.
- Kurd SK, Troxel AB, Crits-Christoph P, Gelfand JM. The risk of depression, anxiety, and suicidality in patients with psoriasis: a population-based cohort study. Arch Dermatol 2010;146:891–5.
- Musalek M. Psychopathology in dermatological patients. Presented at the 11th International Congress Dermatology and Psychiatry (ESDaP), Giessen, May 2005.
- Hazell P. Depression in children and adolescents. In: Barton S, ed. Clinical Evidence, Issue 6. London: BMJ Publishing Group, 2002:278–84.
- Picardi A, Adler D, Abeni D, et al. Screening for depressive disorders in patients with skin diseases. Acta Derm Venereol 2005;65:414–19.
- Kroenke K, Spitzer RL, Williams JB. The PHQ 9: validity of a brief depression severity measure. J Gen Intern Med 2001:16:606–13.
Suicide in dermatological patients
- Diekstra RFW. The epidemiology of suicide and parasuicide. Acta Psychiatr Scand 1993;371;9–20.
- Carson AJ, Best S, Warlow C. Suicidal ideation among outpatients at general clinics. BMJ 2000;320:1311–13.
- Gupta MA, Schork NJ, Gupta AK, et al. Suicidal ideation in psoriasis. Int J Dermatol 1993;33:188–90.
- Gupta MA, Gupta AK. Depression and suicidal ideation in dermatology patients with acne, alopecia areata, atopic dermatitis and psoriasis. Br J Dermatol 1998;139:846–50.
- Denicoff KD, Lehman ZA, Rubinow DR, et al. Suicidal ideation in Darier's disease. J Am Acad Dermatol 1990;22:196–8.
- Cotterill JA, Cunliffe WJ. Suicide in dermatological patients. Br J Dermatol 1997;137:246–50.
- Albertini RS, Phillips KA. Thirty three cases of BDD in children and adolescents. J Am Acad Child Adolesc Psychiatry 2006;38:453–9.
- Kellett SC, Gawkroger DJ. The psychological and emotional impact of acne and the effect of treatment with isotretinoin. Br J Dermatol 1999;140:273–82.
Isotretinoin and mood changes
- Sundström A, Alfredsson L, Sjölin-Forsberg G, et al. Association of suicide attempts with acne and treatment with isotretinoin: retrospective Swedish cohort study. BMJ 2010;341:c5812.
- Marqueling A, Zane L. Depression and suicidal behaviour in acne patients treated with isotretinoin: a systematic revue. Semin Cutan Med Surg 2005;24:92–102.
- Hull P, Darcy C. Isotretinoin use and subsequent depression and suicide; presenting the evidence. Am J Clin Dermatol 2003;4:493–505.
- Serrano A, Rodriguez L. Isotretinoin and depression. Acta Dermo Sifilog 2003;94:535–8.
- Waraich P, Goldner EM, Somers JM, et al. Prevalence and incidence studies of mood disorders: a systematic review. Can J Psychiatry 2004;49:124–38.
- Jick S, Kremers H, Vasilakis C. Isotretinoin use and risk of depression, psychotic symptoms, suicide and attempted suicide. Arch Dermatol 2000;136:1231–40.
Psychiatric treatments
- National Institute for Health and Care Excellence (NICE). Depression in Adults. NICE Guideline CG90, 2009. http://www.nice.org.uk/ (last accessed August 2015).
- National Institute for Health and Care Excellence (NICE). Depression in Children and Young People. NICE Guideline CG98, 2005. http://www.nice.org.uk/ (last accessed August 2015).
- National Institute for Health and Care Excellence (NICE). Generalised Anxiety Disorder and Panic Disorder (with or without Agoraphobia) in Adults. NICE Guideline CG113, 2014. http://www.nice.org.uk/ (last accessed August 2015).
- National Institute for Health and Care Excellence (NICE). Obsessive–Compulsive Disorder: Core Interventions in the Treatment of Obsessive–Compulsive Disorder and Body Dysmorphic Disorder. NICE Guideline CG31, 2005. http://www.nice.org.uk/ (last accessed August 2015).
- National Institute for Health and Care Excellence (NICE). Post-Traumatic Stress Disorder (PTSD). NICE Guideline,CG26: 2005. http://www.nice.org.uk/ (last accessed August 2015).
- National Institute for Health and Care Excellence (NICE). Social Anxiety Disorder: Recognition, Assessment and Treatment. NICE Guideline CG159, 2013. http://www.nice.org.uk/ (last accessed August 2015).
- National Institute for Health and Care Excellence (NICE). Bipolar Disorder. The Assessment and Management of Bipolar Disorder in Adults, Children and Young People, in Primary and Secondary Care. NICE Guideline CG185, 2014. http://www.nice.org.uk/ (last accessed August 2015).
- National Institute for Health and Care Excellence (NICE). Depression in Adults with a Chronic Physical Health Problem: Treatment and Management. NICE Guideline CG91, 2009. http://www.nice.org.uk/ (last accessed August 2015).
- National Institute for Health and Care Excellence (NICE). Common Mental Health Disorders on Primary Care. NICE Pathway, December 2013. http://pathways.nice.org.uk/pathways/common-mental-health-disorders-in-primary-care (last accessed August 2015).
- Bewley A, Taylor RE, Reichenberg JS, Magid M, eds. Practical Psychodermatology. London: Wiley Blackwell, 2014.
- Barbui C, Esposito E, Cipriani A. Selective serotonin reuptake inhibitors and risk of suicide: a systematic review of observational studies. Can Med Assoc J 2009:180(3);291–7.
- Taylor D, Paton C, Kapur SR. The Maudsley Prescribing Guidelines, 12th edn. Oxford: Wiley Blackwell, 2015.
- Trivedi MH, Rush AJ, Wisniewski SR, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry 2006;163:28–40.
- Skelton M, Khokhar WA, Thacker S. Treatments for delusional disorder. Cochrane Database Syst Rev 2012; doi: 10.1002/14651858.CD009785.
- Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis: outcome and efficacy. J Clin Psychopharmacol 2008;28(5):500–8.
- Manschrek T, Khan N. Recent advances in the treatment of delusional disorder. Can J Psychiatry 2006;51(2):114–19.
- Henningsen P, Zipfel S, Herzog W. Management of functional somatic syndromes. Lancet 2007;369:944–56.
- Ruddy R, House A. Psychosocial interventions for conversion disorder [Review]. Cochrane Database Syst Rev 2007;Issue 4:CD005331.
- Rogers C. On Becoming a Person. London: Houghton Mifflin, 1961.
- Veale D, Gournay K, Dryden W, et al. Body dysmorphic disorder: a cognitive behavioural model and pilot randomised controlled trial. Behav Res Therapy 1996;34:717–29.
- Williams C. Overcoming Depression and Low Mood: A Five Areas Approach, 3rd edn. London: Hodder Arnold, 2012.
- National Institute for Health and Care Excellence (NICE). Computerised Cognitive Behaviour Therapy for Depression and Anxiety. Review of Technology Appraisal 51. London: NICE, 2006.
- Klerman G, Weissman M, Rounsaville B. Interpersonal Psychotherapy of Depression: A Brief, Focused, Specific Strategy. New York: Jason Aronson, 1994.
- Brown D, Pedder J, Bateman A. Introduction to Psychotherapy: An Outline of Psychodynamic Principles and Practice. London: Routledge, 2000.
- Abbass A, Hancock J, Henderson J, Kisely S. Short-term psychodynamic psychotherapies for common mental disorders [Review]. Cochrane Datbase Syst Rev 2007;Issue 4:CD004687.
- Fonagy P, Roth A, Higgitt A. Psychodynamic psychotherapies: evidence-based practice and clinical wisdom. Bull Menninger Clin 2005;69:1–25.
- National Institute for Health and Care Excellence (NICE). Depression. Management of Depression in Primary and Secondary Care, London: NICE, 2004.
- National Institute for Health and Care Excellence (NICE). Depression in Children and Young People. Identification and Management in Primary, Community and Secondary Care, London: NICE, 2005.
- Bazire S. Psychotropic Drug Directory. Salisbury: HealthComm UK, 2007.
- Taylor D, Paton C, Kerwin R. The Maudsley Prescribing Guidelines, 9th edn. London: Informa Healthcare, 2007.
- Mehta D, ed. British National Formulary 54. London: Pharmaceutical Press, 2007.
Alternative therapies
- Shenefelt P. Complementary psychocutaneous therapies in dermatology. Dermatol Clin 2005;23:723–34.
- Freid R. Non pharmacologic treatments in psychodermatology. In: Koo JYM, Lee CS, eds. Psychocutaneous Medicine. New York: Marcel Dekker, 2003:427–51.
- Stewart A, Thomas SE. Hypnotherapy as a treatment for atopic eczema. Br J Dermatol 1995;132:778–83.
- Shenefeld P. Hypnosis facilitated relaxation during self-guided imagery during dermatological procedures. Am J Clin Hypnosis 2003;45:225–32.
- Surman OS. Hypnosis in the treatment of warts. Arch Gen Psychiatry 1973;28:439–41.
- Ernst E, Pittler M. Complementary/alternative medicine in dermatology: evidence assessed efficacy. Am J Clin Derm 2002;3:341–8.
- Meyer S, Vogt T, Karrer S. Use of phytopharmaceutical agents in dermatology. Hautarzt 2005;56:483–99.
- Bedi MK, Shenefelt P. Herbal therapy in dermatology. Arch Dermatol 2002;138:332–42.