The human heart is an organ that is about the size of a closed fist and it is located in the chest behind the breast bone, in the middle and to the left. The heart is an amazing organ. It is basically a muscular pump designed to pump blood, firstly to the lungs where it gets oxygen, and then all around the body to the organs and muscles that need the oxygenated blood.
The human heart is an organ that is about the size of a closed fist and it is located in the chest behind the breast bone, in the middle and to the left. The heart is an amazing organ. It is basically a muscular pump designed to pump blood, firstly to the lungs where it gets oxygen, and then all around the body to the organs and muscles that need the oxygenated blood.
Vital Statistics
The heart beats and pumps on average seventy times per minute or over one hundred thousand times per day. This equates to over two and a half billion cycles over seventy years, and all this without maintenance. It is a truly remarkable pump and without comparison in engineering terms.
However, this heart muscle can become damaged. This damage mainly occurs if the small blood vessels supplying blood and oxygen to the heart itself become narrowed or blocked. Your heart is a muscle and like any other muscle in the body it needs oxygen, good nutrition and plenty of exercise to stay at its best. The plumbing of the heart muscle is provided by small arteries called the coronary arteries, which are wrapped around the heart muscle itself. There are three of these: the LCA (left coronary artery), the RCA (right coronary artery) and the circumflex artery. Narrowing of these arteries results in heart disease and sudden blockage can cause heart attack. The LCA is known as the ‘widow-makers’ artery’ as blockage of this artery can result in sudden death.
Heart Disease – The Silent Killer
Perhaps the biggest problem with heart disease is that you may not know you have it. Narrowing of the coronary arteries can occur over many years without necessarily causing any symptoms. Indeed, men who get heart-related chest pain (called angina) may be the lucky ones in that they get an early warning that something is not right. The first symptom or sign of heart disease may be a heart attack or even sudden death. There is no doubt that early detection, and preferably prevention, of heart disease is much better than cure.
Risk Factors for Heart Disease
As an Irish male you are already at an increased risk of heart disease. Indeed, Irish men have some of the highest rates of heart disease in the world. This is largely because of the following risk factors:
- Our genetic makeup – there is no doubt that a family history is important for many conditions, including heart disease. Know your family history well and take appropriate action.
- Smoking – cigarette smoking approximately doubles your risk of heart attack. If you smoke, stop. The good news is that your risk of heart attack drops rapidly if you do stop.
- High blood pressure
- High cholesterol levels
- A ‘Western diet’ – typically a diet high in saturated fat
- Age – none of us can turn back the clock, but the risk of heart attack increases after the age of 40.
- Lack of exercise – the sedentary ‘couch potato’ lifestyle
- Diabetes
- High levels of stress/distress
- Heavy alcohol intake
- Obesity
Symptoms of Heart Disease
The main symptoms of heart disease are chest pain and tightness. As a muscle, the heart needs a good oxygen supply to keep pumping effectively. When there is narrowing of the coronary arteries there is less oxygen going to the heart muscle. This heart muscle can then develop cramp, just like any other muscle in the body. This heart cramp is known medically as angina. Initially, angina tends to come on when the heart is under extra pressure, for example, when exercising, such as climbing stairs or walking in cold weather, or when we are under stress. In other words, any situation where the heart has to work harder and therefore needs more oxygen can cause angina. Angina typically causes central-chest tightness and discomfort, often radiating upwards towards the jaw and sometimes down the left arm. It is often described as being like a tightness or pressure on the chest. An attack of angina is generally eased by rest.
Other symptoms of heart disease can include feeling short of breath when exercising, not being able to do as much as previously and getting tired easily. However, many people with heart disease have no symptoms at all until they have a heart attack.
Heart Attack
This is the biggest killer in Irish men. It is also known as myocardial infarction or coronary thrombosis. What happens is that one of the coronary arteries becomes completely blocked, causing severe cramp in the heart and causing the affected area of muscle to die if its blood supply is not restored relatively quickly. This can lead to serious irregularities of the heartbeat and the heart can stop completely. If the heart is not restarted within 3 minutes, either by resuscitation (CPR) or by the use of an external defibrillator, then irreversible brain and heart damage will occur.
Symptoms of a Heart Attack
Symptoms of a heart attack include a central crushing chest pain (like an elephant sitting on your chest), often radiating upwards to the neck and down either arm, more commonly the left arm, or down into your tummy area. This is often associated with profuse sweating, dizziness, shortness of breath, a sense of nausea or vomiting, and feeling acutely unwell. These symptoms are often compounded by an acute sense of fear or stress, which causes a massive adrenaline release to make the heart try to work even harder and harder, which makes the pain worse and worse. Clearly symptoms such as these need immediate medical attention. Early detection and treatment of heart attack can be life-saving. Clot-busting drugs have become available in recent years that can literally dissolve the blockage in your artery if given quickly enough.
Tests on Your Heart
For the Irish man all of this means you should be aware of your risk factors for heart disease and also understand the symptoms of heart disease and be able to take appropriate action. This means a regular check-up with your doctor, focusing on preventative health issues. A good chat with your doctor, along with some tests, will help give you a better understanding of your risks. Tests include examining your weight (body mass index), waist circumference, pulse and blood pressure, along with a cardiac examination and some blood tests, such as examining your lipid profile (for cholesterol and blood fat) and blood glucose levels (for risk or tendency to diabetes).
ECG Test
If your doctor suspects heart disease he may suggest some additional tests, which may include an ECG (electrocardiogram). This is an office-based test in which a number of stickers are placed on the chest wall and the electrical rhythm in the heart is recorded. This ECG test can be very useful in determining any strain on the heart or any heart irregularities. Many of these ECGs can now be analysed by computer.
An exercise ECG (stress test) can also be carried out. This is where you are put onto a treadmill and hooked up to an ECG while you exercise, walking at a slow pace initially and gradually building up until you are jogging. The heart rhythm and rate are recorded. If there are narrowings in the coronary arteries this will cause additional strain on the heart muscle as you exercise, which may show up on the ECG test. However, these tests are not black and white, and some cases of heart disease may remain undetected, even if these tests are normal.
Echocardiogram
An echocardiogram (echo) is an ultrasound scan of the heart muscle used to look at how well the heart muscle and heart valves are working. It can be a very useful test when heart problems are suspected. Sometimes an echo can detect congenital abnormalities such as thickening of the heart muscle wall, which can be associated with an increased risk of sudden cardiac death. An example of such a condition is HOCM (hypertrophic obstructive cardiomyopathy).
Angiogram
An angiogram is another test that can be done to look at the coronary arteries. In this test a thin flexible tube known as a catheter is guided from a leg artery up into the coronary arteries in the heart. Dye is then injected into the catheter and repeated x-ray pictures are taken as the dye flows through the heart. This allows any narrowing or tiny blockages in the blood vessels to show up.
More recent advanced scanning technology can also allow detailed images of the heart to be taken, which can give a good indication of blockages and damaged arteries.
Treatments for Heart Disease
Angioplasty
This is an effective procedure used to widen narrowed arteries in the heart. Once an angiogram has located the narrowed part of the coronary artery, a thin expandable balloon can be guided over a wire to the affected area. This balloon tip can then be inflated and so expands the artery by stretching the artery open. This can significantly reduce the blockage in the artery. Major complications from this procedure are uncommon. However, sometimes the artery narrows again in the six months after angioplasty. This is known as ‘restenosis’ and may need further treatment.
Stent Procedure
This is where a small tube is left in the narrowed artery after angioplasty. This is like a support structure for the artery. It keeps the narrowed part of the artery open and thereby improves the blood supply to the heart muscle. This has been a major advance in the treatment of heart disease. Newer stents have been devised that are coated with drugs to thin the blood and can help prevent reclosure at the stent site.
Heart Bypass Surgery
This is a type of heart surgery known as coronary artery bypass grafting (CABG) by which blood is re-routed around blocked arteries by creating bypasses around them with veins taken from other parts of the body, usually the legs. This procedure is less often performed now due to the newer innovations in the treatment of narrowed or blocked arteries, such as angioplasty and stents, as well as better medical management of heart-related problems.
What Can I Do to Prevent Heart Disease?
Prevention is better than cure and we know that heart disease is a largely preventable condition. You can’t change your age or your genetic makeup and family history. However, you can make dramatic improvements to your heart health and add years to your life expectancy and quality of life by taking action and making positive changes. And it is never too late to make those positive changes, even if you have several risk factors for heart disease and even if you have heart disease already.
- If you smoke, stop smoking! Smoking twenty cigarettes a day doubles your risk of heart attack because smoking makes the blood thicker, enabling it to clot more easily. Smoking cigarettes also causes carbon monoxide, which blocks oxygen from getting to the muscles, to enter the bloodstream. Smoking destroys Vitamin C, which helps protect the heart, and, most importantly, it causes damage to the lining of the blood vessels, thus facilitating clotting and blockages.
- Have a regular check-up and make sure your blood pressure is well controlled at 120/80.
- Keep your total cholesterol level under 5, your LDL (bad) cholesterol level under 3 and your HDL (good) cholesterol level over 1 (see Chapter 6 for an explanation of the different types of cholesterol).
- Eat a heart-healthy diet, focusing on fruit and vegetables, wholegrains, plenty of fibre, oats, oily fish, and eating plenty of foods rich in antioxidants (mainly fruit and vegetables, seeds and pulses). Reduce your dietary salt intake and minimise your saturated fat intake.
- Develop an active lifestyle and exercise regularly – at least 210 minutes a week (30 minutes a day).
- Monitor your stress levels – look at your work–life balance, learn to de-stress and give yourself enough down time.
- Moderate your alcohol intake – less is more. For most people, who are otherwise not addicted or allergic to alcohol, 1 or 2 units of alcohol per day may have a cardio-protective effect. This is partly due to the benefits of alcohol on HDL cholesterol as well helping the blood to clot. However, more than two drinks per day increases your risk of heart disease. Be aware of your safe limits.
What about Supplements to Prevent Heart Disease?
Folic acid and the B vitamins can lower homocysteine levels, which tend to be high in Celtic males. Homocysteine is an amino acid implicated in the hardening of the arteries and high levels are a factor in heart disease. Folic acid, either taken through diet or in supplementary form, lowers homocysteine levels and can be a useful addition in the fight against heart disease and stroke. In addition, niacin (Vitamin B3) is very helpful at raising HDL (good) cholesterol levels. This is discussed further in Chapter 6.
Omega-3 fish oil, particularly that found in cold water fish (such as salmon, tuna and sardines) or else in supplement form, is beneficial for the heart. Again this is discussed in Chapter 6.
Coenzyme Q is produced by the human body and is necessary for the basic working of cells. It is thought that coenzyme Q levels can be low in patients with some chronic diseases, such as heart conditions and high blood pressure. Some prescription drugs, such as statins for cholesterol, may also lower coenzyme Q levels. Therefore a coenzyme Q supplement may reduce some of the potential side effects of statin treatment for raised cholesterol and may also help to lower blood pressure. This area is the subject of ongoing research.
What About Aspirin?
Aspirin can prevent clotting occurring at the site of narrowed arteries by thinning the blood. Because platelets (the cells in the blood that are involved in blood clotting) are made on a continuous basis by the bone marrow, aspirin must be taken on a regular basis, either daily or every second day, to have its maximum effect.
If you have already suffered a heart attack or have established heart disease then taking low-dose aspirin has an important role in preventing further heart attack or further heart damage. Low doses of aspirin (between 75mg and 300mg per day) will produce this vital benefit. For many men who do not already have heart disease, taking a low-dose aspirin daily or on alternate days may have health benefits in terms of reducing your risk of heart attack. This blood-thinning ability of aspirin is generally better in men over fifty.
Because aspirin is a blood thinner it can help men who have peripheral artery disease (PAD) or damage to the circulation in their legs. Aspirin can also help prevent the most common type of stroke, i.e. that form of stroke caused by a blood clot in the brain. However, because aspirin thins the blood it does increase the risk of the rarer hemorrhagic stroke, which is brain damage caused by a bleed into the brain itself. Aspirin may also have some benefit in terms of preventing colon (bowel) cancer. This is an area of ongoing research.
However, despite the fact that it is widely available as an overthe-counter medicine, this does not mean that aspirin is always safe. In some people it can cause serious side effects; the most common is bleeding, especially bleeding after injury. Because of this you should always stop your aspirin at least a week before elective surgery. Bleeding from the stomach lining can cause stomach or duodenal ulcers. Aspirin can also affect the kidneys, particularly in elderly people. Some people can have allergies to aspirin and must avoid it.
There are pros and cons to taking aspirin, just like every other drug. Ultimately the decision will rest with you, in consultation with your doctor.
Blood Pressure – The Silent Killer
What Is Blood Pressure?
Blood pressure is simply the pressure of blood in the tubes as it is brought around the body. It is measured in millimetres of mercury (mmHg) and is quoted as two separate figures, e.g. 120/80. The upper figure is known as the systolic blood pressure. This is the pressure of blood in the tubes when the heart beats and contracts, causing blood to be squeezed and pumped from the heart to all parts of the body. The second figure is known as the diastolic figure or resting blood pressure. This is the pressure in the tubes when the heart relaxes after beating. This cycle of beat, relax, beat, relax repeats itself continuously. Normal blood pressure varies over a 24-hour period. Exercise will cause blood pressure to temporarily go up, as higher pressure is needed to vigorously pump blood into exercising muscles that need more oxygen. When we are under stress the ‘flight or fight’ response kicks in, whereby hormones such as cortisol and adrenaline are released from the adrenal glands (small glands that sit on top of the kidneys). The net effect of these hormones is to cause blood pressure to go up. Conversely, when we are sleeping at night-time blood pressure is usually lower as our bodies rest and relax.
What Is High Blood Pressure?
High blood pressure is when your blood pressure reading is higher than what is considered acceptable for good health. It may be indicated by a raised systolic blood pressure reading, a raised diastolic blood pressure reading, or both. As blood pressure readings can vary throughout the day, a once-off raised reading is not of any major significance. However, repeated raised blood pressure readings, ideally averaged over a 24-hour period using a 24-hour blood pressure monitor, can easily indicate high blood pressure.
How Common Is It?
High blood pressure is very common and is one of the leading risk factors for heart disease and stroke in the Western world. It can affect up to one in every four middle-aged Irish men and about one in every two Irish men aged over 65.
High blood pressure is one of those medical conditions that follows a rule known as ‘the rule of halves’. This means that about half of all people with high blood pressure remain undiagnosed and do not know they have it. This includes a lot of Irish men who haven’t been to the doctor for years because they ‘feel fine’. About half of those diagnosed are not treated and only about half of those who get treatment have their treatment properly controlled according to best practice guidelines. Therefore, as few as one in eight people with high blood pressure have their condition properly diagnosed, treated and controlled. There are many complex reasons why this rule of halves exists; these include the reluctance amongst Irish men to go to the doctor, the lack of emphasis on prevention in healthcare and the resistance of many men to taking medication when they don’t feel sick.
How Do I Know If I Have High Blood Pressure?
High blood pressure is often known as a silent disease because there may be no symptoms whatsoever. A person with high blood pressure feels well, looks well and rarely has any symptoms. Indeed, unless a man goes for a check-up and has his blood pressure checked, he may never know he has high blood pressure until it is too late.
If your blood pressure reading is up then several readings on different occasions are needed to confirm that your blood pressure is indeed elevated. Some men suffer from what is known as the ‘white-coat effect’, whereby anxiety due to unease or insecurity when going to the doctor can cause the blood pressure to temporarily go up. Taking readings on different occasions can sometimes help overcome this white-coat effect. However, the most accurate way to diagnose high blood pressure now is to use a 24-hour blood pressure monitor. This is where a cuff attached to a small computerised monitor is wrapped around your arm and you carry on with your normal business for 24 hours, after which the cuff is removed and the data is printed out on a computer. This monitor checks your blood pressure at 30-minute intervals over the entire 24-hour period. A detailed graph can then be printed out showing your overall average blood pressure as well as your average day-time and night-time readings and what percentage of each are above normal.
What Causes High Blood Pressure?
The exact cause of high blood pressure is unknown. There is often no single cause and it is thought to be due to a combination of many different factors. High blood pressure often runs in families. It is not due to being nervous or highly strung. Firstly, the ageing process itself can cause the blood vessels to become less elastic and flexible and more hard or rigid. This loss of elasticity in the blood vessel walls can cause the pressure of blood going through them to go up. It is not ageing per se but rather ageing of the blood vessels that causes this hardening and resultant increase in pressure. This hardening of the blood vessels is often caused by cigarette smoking and the high-saturated-fat, high-salt diet so prevalent in the Western world.
Cigarette smoking can damage the lining of the blood vessels, causing them to narrow over time. This will make the pressure of blood going through these narrow tubes go up, as the heart has to pump harder to push the blood through a narrow space.
High cholesterol and blood fat (triglycerides) levels, caused either by a high-saturated-fat diet or by genetic factors, can lead to the formation of cholesterol plaques on the inside of the blood vessels, which causes the tubes to narrow. This is a condition known as atherosclerosis.
A diet rich in salt can also cause blood pressure to go up as sodium causes fluid retention and also affects the complex hormonal pathways that regulate blood pressure.
Obesity or carrying excess weight is also associated with an increased risk of high blood pressure. A simple analogy is that, for every extra pound of fat, there is approximately an extra mile of tiny blood vessels supplying blood to that pound of fat. So suppose you are 3 stone overweight, that means every time your heart beats it has to pump blood an extra 42 miles. In that context it is easy to see how pressure goes up, as the heart has to work harder to bring oxygen to that extra fat. While this analogy is not totally accurate, it gets the message across.
Genetic factors are obviously important in the development of high blood pressure. If there is a history of high blood pressure in your family, you need to pay extra attention to your own risk of developing high blood pressure in the future.
High blood pressure is also very common in people with diabetes, as diabetes can lead to hardening of the arteries. Stress is also recognised as a potential cause of raised blood pressure. The fight or flight response is a normal reaction in the body to feeling under stress. However, if you are under chronic long-term stress, then the long-term effect of hormones like cortisol and adrenaline on the system can result in high blood pressure. More rarely, raised blood pressure can be caused by hormonal conditions like Cushing’s syndrome and other disorders of the adrenal glands.
What Are the Complications of Raised Blood Pressure?
For many years raised blood pressure may cause no symptoms. Occasionally, raised blood pressure can be associated with headaches and nose bleeds, but usually only when the blood pressure is very high. However, high blood pressure makes the heart and arteries work harder, causing damage over the years. This can lead to a heart attack or stroke at an early age. Fortunately, treatment can reverse most of these effects.
However, raised blood pressure can have devastating consequences by putting extra strain on the system over a long period of time. These complications can include blindness, kidney damage, heart attacks and mini-strokes, as well as full-blown strokes. These complications can come on suddenly with devastating effects.
High blood pressure is, along with cigarette smoking, the most important risk factor for the development of heart disease and stroke. Other risk factors for the development of heart disease and stroke include family history, raised cholesterol and blood fat levels, obesity, lack of exercise, excess alcohol and a diet high in saturated fat and salt. The important thing to note about these risk factors is that they are synergistic rather than additive. This means that they multiply together rather than add together. In other words, if you have three of these risk factors your risk of heart attack or stoke may be many times higher than if you just have two.
Benefits of Treating Raised Blood Pressure
Obviously prevention is better than cure. The aim in detecting and treating raised blood pressure is to bring the pressure back down to normal so as to prevent any long-term strain on the heart or blood vessels, thereby helping to prevent heart disease and stroke. If you have been prescribed medication for high blood pressure, you will usually have to take it for the rest of your life. If you stop the medication your blood pressure will tend to go up again. The good news is that this medication can prevent early ageing of the blood vessels and prevent any additional strain on the heart. There is good evidence that lowering your blood pressure, if it is raised, can significantly reduce your relative risk of both heart attack and stroke.
Can I Stop My Blood Pressure Tablets Once My Blood Pressure Is Back Down to Normal?
No, unfortunately. The decision to treat raised blood pressure is an important one as the treatment is usually lifelong. This is because, if you stop taking the blood pressure tablets, then your blood pressure will usually start to climb up again. Therefore it is very important that the diagnosis is made correctly and that the decision to treat it is a shared one between you and your doctor. By fully understanding the implications of the decision to treat high blood pressure in terms of the benefits of doing so as well as the risks and consequences of not treating your high blood pressure, you are then in a better position to weigh up the benefits of long-term treatment.
What About Changing My Lifestyle?
Certainly a heart-healthy lifestyle is conducive to good heart health and will help your blood pressure. If your blood pressure is only mildly elevated, then it may make sense to try a heart-healthy lifestyle for a period of three to six months, to see if your blood pressure benefits. If you are successful, you may avoid having to take long-term pressure treatment. A heart-healthy lifestyle would naturally include the following:
- Stopping smoking
- If you are overweight, losing weight – studies have shown that by losing 10 per cent of your body weight (if you are overweight) you can reduce your blood pressure by ten mmHg
- Watching your alcohol intake – keep within the recommended limits for men of 21 units per week. Remember, less is more
- Regular exercise
- Eating a heart-healthy diet:
- eat plenty of fresh fruit and vegetables
- use fat-free or low-fat milk and dairy products
- switch to wholegrain cereal
- eat oily fish at least once or twice a week
- eat poultry and nuts
- eat foods that are rich in potassium, calcium and magnesium
- cut out trans-fats, saturated fat and cholesterol and reduce your total fat intake
- reduce red meat consumption to once a week or less
- cut out sweets and sources of added sugar
- minimise your salt intake – this in effect means avoiding processed foods, which tend to be high in salt.
Stroke
A stroke can also be called a brain attack. It is like a heart attack except that it is the brain that is affected. The blood supply to the brain is interrupted and cut off. This causes nerve cells in that part of the brain to die, which affects the body functions controlled by those brain cells. This is the often devastating consequence of stroke. Stroke is a common cause of death among Irish men.
What Causes a Stroke?
Strokes have two underlying causes: either a blockage of a brain artery or a bleed from an artery in the brain. Most strokes are caused by a blockage in one of the brain arteries as a result of the same risk factors and processes that cause heart disease, i.e. smoking, high cholesterol, high blood pressure, etc. Less commonly, strokes are caused by a rupture in a brain blood vessel, which causes bleeding into the brain tissue itself. This is often caused by high blood pressure or a brain aneurysm. An aneurysm is a weak area or bubble on a blood vessel that can be like a time bomb waiting to go off. Some people are born with aneurysms and sometimes they develop as a result of high blood pressure or hardening of the arteries.
What Are the Symptoms of Stroke?
As the name suggests, stroke is like a bolt of lightening, and can bring on sudden death. Symptoms include weakness or paralysis down one side of the body (face, arms or legs), numbness or loss of sensation in the face or limbs, and loss of bladder control, speech or vision. Other symptoms can include weakness, difficulty swallowing, face drooping to one side, dizziness, loss of balance, severe headache, difficulty speaking or understanding simple statements, and loss of vision, especially in one eye. There is potential for a certain amount of recovery in the first few weeks after a stroke, which is why expert rehabilitation with a range of different health professionals is so important.
What Type of Man Is at Risk of Stroke?
- Older men – two-thirds of strokes occur in people aged over 65.
- Those with a history of heart disease, previous stroke or mini-stroke
- Men with risk factors such as high blood pressure, high cholesterol, obesity and lack of exercise, smokers and heavy drinkers
- Those with an irregular heartbeat, called atrial fibrillation, which increases the chances of clots in the system
- Men with a high red blood cell count, as thicker blood is more likely to clot
- Men with a family history of stroke
Prevention of Stroke
Just like heart disease, you can reduce your chances of getting a stroke by making certain changes in your lifestyle, especially by not smoking and controlling high blood pressure. If you have high cholesterol, lowering your cholesterol levels may also reduce your risk. Your doctor may tell you to change your lifestyle as well as prescribing medication to lower your blood pressure or cholesterol. Aspirin or warfarin is often used to prevent clotting and reduce the risk of stroke.
Mini-Strokes
These are also known as transient ischemic attacks or TIAs, brought on when an artery in the brain becomes temporarily blocked. This can cause symptoms similar to a stroke but the symptoms disappear without any permanent damage within 24 hours. This is the key difference between a TIA and a stroke. However a TIA is a warning sign that you are at much greater risk of a stroke in the future. Therefore it is an early warning sign that you need to sit up and take notice of your health, and work with your doctor to do all that can be done to prevent a stroke later on.
Abdominal Aortic Aneurysms (AAA)
The aorta is the main blood vessel that comes from the heart and brings blood to the body. When it leaves the heart it initially goes upwards and then curves down through the tummy area to bring blood to the lower body and legs. Damage to the wall and lining of the aorta can cause it to weaken and bulge like a small bubble, creating an aneurysm. When an aneurysm develops on the aorta in the abdominal area it is known as an abdominal aortic aneurysm (AAA). This condition is more common in men, particularly middle-aged and elderly men.
What Causes AAA?
Cigarette smoking greatly increases the chance of getting an AAA and raised cholesterol and blood pressure levels, along with obesity, are also risk factors. Also, if there is a family history of the condition then your chances of getting it are much increased. The ageing process itself, particularly ageing of the blood vessels, can also play an important role.
Diagnosis
Most men with an AAA have no symptoms. Sometimes it can cause bellyache or backache. It may be possible to feel a large aneurysm in the tummy area as a pulsating or throbbing swelling. The most reliable and accurate way to diagnose an AAA is by a simple ultrasound scan. So if you have any of the risk factors, discuss the benefits of a screening ultrasound scan for an AAA. If one is detected then you will need to see a vascular specialist to determine whether it needs to be surgically repaired. Once an aneurysm has formed it will not go away on its own, so most aneurysms eventually need surgery. The main complication of an aneurysm is that it can eventually rupture or burst, with often fatal consequences. In this respect, an aneurysm can be a time bomb.
Treatment Options
A watch-and-wait approach with regular follow-up assessments is often advised for small aneurysms with no symptoms. In general terms, the risk of an AAA rupturing or bursting is related to its size. Small aneurysms (less than 5 centimetres in diameter) have a very low risk of rupture, whereas larger aneurysms have an increased risk. However, if it enlarges beyond 5 centimetres, surgery is required. The surgical repair of an AAA is generally a big operation with a risk of serious complications. The weakened aorta is replaced with a polyester tube or graft and stitched into place. This graft is permanent and will last for many years.
Recently, new breakthroughs in minimally invasive surgery can allow the aneurysm to be fixed from the inside out by making small incisions in the groin; thus, major incisions in the chest wall can often be avoided. Aortic aneurysms that have ruptured can be repaired with emergency surgery but the mortality rate from a ruptured aneurysm is high.
Peripheral Arterial Disease (PAD)
Atherosclerosis is a disease process in which arteries that bring blood to various parts of the body become damaged, resulting in narrowed arteries and potential blockages. When atherosclerosis affects the heart it makes the coronary arteries narrow, causing angina and heart attack; when it affects the brain it can cause TIAs (mini strokes) and stroke; when it affects the aorta it can cause an aneurysm (AAA); and when atherosclerosis affects the legs it causes Peripheral Arterial Disease (PAD). This can result in progressive narrowing of the arteries in the legs, leading to potential blockages and eventually possible gangrene, which would lead to amputation.
PAD does not get as much attention as heart disease or stroke and yet it is a very common and often under-diagnosed medical condition. It is thought to affect about one in every four Irish men over the age of seventy-five.
What Are the Risk Factors for PAD?
The risk factors for PAD are the same ones that damage the circulation elsewhere in the body, including the risk factors for heart disease and stroke. They include:
- Cigarette smoking
- Diabetes
- High cholesterol levels
- High blood pressure
- Obesity
- Lack of exercise
- Stress
- Family history
What Are the Symptoms?
Like other forms of atherosclerosis, PAD can be a silent condition with no symptoms for many years. The earliest symptom tends to be pain or cramping in the leg, which comes on with exercise. Classically, this pain or cramp disappears within a few minutes of resting. The symptom pattern is very variable. With more severe blockages, pain can also occur in the foot when resting, particularly at night-time.
How Is PAD Diagnosed?
Your doctor can examine your legs and assess the pulses in your feet. He can also look for other evidence of PAD such as loss of hair on the toes, skin changes (with the skin becoming pale and shiny) and loss of colour in the leg when it is elevated.
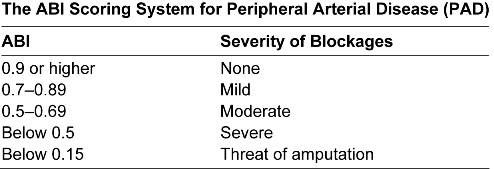
A simple test called the Ankle Brachial Pressure Index (ABI) can determine not only whether PAD is present but can also give a good estimate of its severity. The ABI test is simply a ratio of the blood pressure in your arm measured in the normal way, compared to the blood pressure in your leg measured using an ultrasound probe. The table below shows the scoring system that is used.
More detailed tests can be done for cases that may benefit from surgical intervention. These include scans and angiography, where dye is injected into the arteries to assess the extent of the blockages.
How Is PAD Treated?
Obviously, the first line of treatment is to eliminate any known risk factors. This includes stopping smoking, optimising your blood pressure, cholesterol and blood sugar levels, taking plenty of aerobic exercise, keeping your weight down and minimising stress. A good exercise programme can have amazing benefits on muscles because it can allow new blood vessels to form and sometimes create new little ring roads around blocked arteries. Exercise can also allow muscles to use oxygen more effectively, which makes them more efficient.
Medication has a limited role to play in patients with PAD. Plavix and aspirin are often used for people with established PAD because of their blood thinning and anti-clotting abilities. Alternative treatments that have been used include garlic and Ginkgo biloba, which are thought to have some circulation-enhancing benefits.
In more severe cases, blocked arteries can be unblocked by angioplasty and sometimes severe blockages are by-passed. Unfortunately, reblockage of the affected arteries can occur. As with many other conditions, prevention is better than cure. However, with meticulous attention to the risk factors, combined with a healthy lifestyle and vigorous exercise programme, the symptoms of PAD can often be kept under control and improved over time.
Key Points

- Heart disease and stroke are the number one causes of death and premature illness in Irish men.
- High blood pressure is very common in Irish men and is a major risk factor for heart disease and stroke.
- High blood pressure often has no symptoms; it is ‘the silent killer’.
- Atherosclerosis is a disease process that damages the circulation and can affect the heart, brain, aorta and legs, causing heart disease, stroke, aneurysms and blocked arteries.
- We can’t change our genes but many of the risk factors for atherosclerosis can be controlled – these include cigarette smoking, high blood pressure, diabetes, high cholesterol, stress, obesity and lack of exercise.
- Narrowing of the blood vessels in the legs (PAD) and aneurysm of the aorta (AAA) are both common in ageing men.
- Know your numbers – you should get your blood pressure and cholesterol checked regularly.
- High blood pressure, high cholesterol and many of the risk factors for heart disease, stroke and atherosclerosis can be very successfully treated, but only if you are aware that you have them.
- Prevention is better than cure.
 The human heart is an organ that is about the size of a closed fist and it is located in the chest behind the breast bone, in the middle and to the left. The heart is an amazing organ. It is basically a muscular pump designed to pump blood, firstly to the lungs where it gets oxygen, and then all around the body to the organs and muscles that need the oxygenated blood.
The human heart is an organ that is about the size of a closed fist and it is located in the chest behind the breast bone, in the middle and to the left. The heart is an amazing organ. It is basically a muscular pump designed to pump blood, firstly to the lungs where it gets oxygen, and then all around the body to the organs and muscles that need the oxygenated blood.