Cancer is a serious health issue for Irish men. About one in every three Irish men will develop cancer at some stage in their lives and about one in six men will die from it. The word ‘cancer’ is often perceived as a frightening one, yet cancer is not the hopeless diagnosis it once was. Many cancers can now be prevented through the combination of a healthy lifestyle and regular check-ups. Those cancers that can be detected early can be treated before it is too late. Unfortunately, research has shown that Irish men tend to ignore warning symptoms and present late to their doctor for check-ups and medical advice. Through a combination of fear, denial, embarrassment and lack of time, men often ignore their own health, to their cost. The national cancer registry has shown that rates of common cancers in Irish men are set to increase by over 50 per cent by 2020. The four most common cancers in men are:
Cancer is a serious health issue for Irish men. About one in every three Irish men will develop cancer at some stage in their lives and about one in six men will die from it. The word ‘cancer’ is often perceived as a frightening one, yet cancer is not the hopeless diagnosis it once was. Many cancers can now be prevented through the combination of a healthy lifestyle and regular check-ups. Those cancers that can be detected early can be treated before it is too late. Unfortunately, research has shown that Irish men tend to ignore warning symptoms and present late to their doctor for check-ups and medical advice. Through a combination of fear, denial, embarrassment and lack of time, men often ignore their own health, to their cost. The national cancer registry has shown that rates of common cancers in Irish men are set to increase by over 50 per cent by 2020. The four most common cancers in men are:
- Skin cancer
- Prostate cancer (discussed in Chapter 8)
- Colon cancer
- Lung cancer
What Is Cancer?
The basic unit in the body is the cell and we all have billions of cells in our bodies. Normally, cells divide to make more cells when the body needs to either repair existing cells or replace those that have worn out or died. This process of cell growth, repair, death and renewal is normally finely tuned and regulated. It is a continual process and helps to keep our bodies in good shape.
The main feature that all cancers have in common is a lack of regulated or proper cell growth. The inbuilt system of checks and balances breaks down. So when a cancer cell begins to grow, it multiplies out of control. If cells keep dividing when new cells are not needed, a mass of tissue forms. This mass of extra tissue is called a ‘growth’ or ‘tumour’.
Benign and Malignant Tumours
Tumours can be benign or malignant. What’s the difference? Benign tumours are not cancer and are rarely a threat to life. Cells from benign tumours do not spread to other parts of the body. They can usually be removed surgically or treated with drugs and/or radiation to reduce their size and, in most cases, they do not recur. Malignant tumours are cancer. There are more than 100 different types. Cancer cells can invade and damage tissues and organs near the tumour as well as spreading to form new malignant tumours in other parts of the body. This spread of cancer is called metastasis (pronounced me-tas-tis-iss). The word cancer itself comes from the Latin word for crab. This is because historically the swollen blood vessels around the area of a tumour were thought to resemble a crab’s limbs.
What Causes Cancer?
As we have said, cancer occurs when the fine-tuning mechanism in the body that controls and regulates cell growth and cell death is altered. In addition, the body’s natural immune system, which is normally able to kill off many cancer cells, malfunctions. The result of these two events is uncontrolled cell growth and these cells can then invade other parts of the body.
This can occur because of genetic factors or environmental factors or a combination of both. Many people are genetically programmed to develop cancer. In other words, if there is a strong history of cancer in the family then you may be more at risk of developing that type of cancer yourself. Bowel cancer is a good example of this. Environmental factors include exposure to a wide variety of substances that are known to increase the risk of getting cancer. These substances are known as carcinogens.
Known Risk Factors for Cancer
A risk factor is anything that increases a person’s chance of getting a disease such as cancer. Different cancers have different risk factors. Several risk factors make a person more likely to develop cancer:
- Cigarette smoking and tobacco use. Smokers worldwide account for about 85 per cent of cases of lung cancer in men. Smoking is also a major cause of oesophageal, mouth, throat, bladder and pancreatic cancer. There are over fifty different carcinogens in tobacco smoke.
- Obesity
- A high-saturated-fat ‘Western diet’. Lots of red meat and little fresh fruit and vegetables lead to an increased risk of both colon and prostate cancer.
- Lack of exercise
- Exposure to workplace carcinogens such as asbestos, arsenic, benzene and vinyl chloride
- Drinking large amounts of alcohol leads to an increased risk of mouth, throat, oesophageal and liver cancer.
- Genetic factors are important in some cancers, such as colon, stomach and prostate cancer.
- Exposure to radon gas. This is a natural radioactive gas which seeps from the ground into the home. Levels of radon are quite high in various parts of Ireland and it is strongly associated with lung cancer.
- Food additives such as nitrates in processed foods, which are converted in the body to carcinogenic nitrosamines
- Barbequing food may produce carcinogenic chemicals such as polycyclic aromatic hydrocarbons that may promote intestinal cancer.
- Medical treatment that suppresses the immune system, allowing for successful organ transplantation, can also result in cancer because of this suppression of the immune system.
- Radiation
- sunlight exposes the body to ultraviolet radiation. Ultraviolet radiation over a prolonged period of time can damage DNA and cause cancer. This is why excess sunbathing or sunburn can cause skin cancer.
- other forms of ionising radiation such as nuclear energy (think of the Chernobyl tragedy), medical x-rays and the natural gamma radiation in cosmic rays
- Infections
- virus infections associated with cancer would include the HIV virus, which weakens and destroys the body’s natural defence system, thereby opening the door to many cancers.
- hepatitis B and C viruses can lead to liver cancer.
- the human papillomavirus, which is sexually transmitted by men to women, can cause cervical cancer in women.
- Helicobacter pylori, a bacterial infection, if untreated is associated with an increased risk of stomach cancer.
Length of Exposure
Of course the likelihood of developing cancer from a carcinogen increases in relation to the intensity and length of exposure to that carcinogen. For example, someone who continues to eat a diet high in saturated animal fat and low in fresh fruit and vegetables is at higher risk of bowel and prostate cancer than a man who may have had a poor diet but has now made some positive changes. Smoking one cigarette once clearly has a negligible risk of lung cancer compared to smoking twenty cigarettes a day for thirty years.
Radon
Radon is the second leading cause of lung cancer after cigarette smoking. The World Health Organization has classified radon as a Class 1 carcinogen. When breathed into the lungs this radioactive gas damages lung tissues, which can lead to lung cancer. Radon is a naturally occurring gas that comes from the radioactive decay of uranium in our rocks and soils. It has no odour, colour or taste and so can not be detected by humans. There are parts of Ireland where radon gas levels are very high, including the south east. Radon dissolves and is harmless in the open air but in enclosed spaces like houses it can build up to dangerous levels. All new houses now have to be fitted with a radon barrier but any house built prior to 1998 does not have to have a radon barrier fitted. Therefore it is important to check radon levels in your own house. This can be done quite simply by getting a radon counter, which is available from the Radiological Protection Institute of Ireland in Dublin (RPII) (www.rpii.ie). The counter is left in your house for a period of time and then sent back to them for analysis. If the radon levels are high, then remedial measures can be taken to correct this. According to the RPII, radon accounts for about two-thirds of the total radiation to which the average Irish person is exposed. The lifetime risk of lung cancer for a 70-year-old man who has been exposed to high levels of radon is one in fifty.
General Warning Signs of Cancer – Catch it Early
While cancer is best prevented, early detection is vital to maximise the chance of cure. This means, as a man, you must be aware of potential early warning signs of cancer and take appropriate action. While many men with some of the listed symptoms won’t actually have cancer or other serious illnesses, it’s important not to take chances with your health. If in doubt, check it out! There really are no advantages to delaying seeking medical advice. On the contrary, early detection can literally sometimes be the difference between life and death.
- Any change in your bowel habit such as bleeding from the back passage, constipation or diarrhoea, or a feeling of incomplete emptying may indicate early bowel cancer.
- A change in your waterworks pattern, including urinating more often, the stream stopping and starting, peeing at night and with a sense of urgency, may indicate prostate problems.
- A sore that doesn’t heal can suggest mouth or skin cancer.
- Any obvious change in a mole or a wart, such as an increase in size, change in colour or bleeding, may indicate skin cancer.
- Unusual bleeding from any site of the body:
- blood in the stool may indicate colon cancer.
- blood in the urine may indicate bladder cancer or kidney cancer.
- spitting or coughing up blood may indicate lung cancer.
- A lump or swelling in the testicles may indicate testicular cancer.
- Persistent heartburn, indigestion, difficulty swallowing or feeling something getting stuck may indicate cancer of the food pipe (oesophagus) or stomach.
- A persistent cough or chronic hoarseness may be a sign of throat or lung cancer.
- Any nagging pain in the bones or elsewhere without apparent reason
- Unexplained weight loss or loss of appetite
- Persistent sweating
- Low-grade fever
- Unexplained bruising
- Persistent headaches
- Unusual fatigue
Treatment Options for Cancer
Surgical removal of the tumour is usually the best treatment option if it is possible. Other options include chemotherapy or radiotherapy, which may be used on their own or in combination. The potential for the use of these treatments depends on many factors, including the type and location of the tumour, as well as whether and where else in the body the tumour has spread to. If radiotherapy or chemotherapy is used to treat a cancer along with surgery then this is called adjuvant chemotherapy or adjuvant radiotherapy.
Chemotherapy is medication that attacks cancer cells. Some forms can be given orally while others are given by injection into the blood vessels. There are different chemotherapy ‘cocktails’ used for different tumours. One of the main side effects of this treatment is a weakening of the immune system.
Radiotherapy is a treatment that uses beams of radiation to attack cancer cells. This is usually external to the body but recently, for prostate and breast cancers, radiation capsules are sometimes being placed inside the body to irradiate the tumour from the inside out.
Lung Cancer
Lung cancer usually starts in the lining of the tubes that bring air into the lungs. Lung cancers are believed to develop slowly over a period of many years.
What Are the Symptoms of Lung Cancer?
Lung cancer usually does not show symptoms when it first develops, but symptoms often appear when the tumour begins growing. Each individual may experience symptoms differently.
A persistent cough is the most common symptom of lung cancer. Other symptoms include:
- Hoarseness
- Blood-streaked sputum or phlegm (spit)
- Constant chest pain
- Feeling short of breath
- Wheezing
- Recurring lung infections, such as pneumonia or bronchitis
- Unexplained fever
- Low sodium levels, leading to confusion
Like all cancers, lung cancer can cause general symptoms such as loss of energy, fatigue, weight loss, loss of appetite, non-specific aches and pains, headaches and fractures. Direct pressure effects on large blood vessels or certain nerves near the lung can cause swelling of the neck and face or cause pain and weakness in the shoulder, arm or hand. Of course, some or all of these symptoms can be caused by many other conditions so make sure you consult your doctor for advice.
What Are the Main Risk Factors for Lung Cancer?
By far and away the most common cause of lung cancer is cigarette smoke. Heavy smokers are twenty-five times more likely to get lung cancer than non-smokers. The risk of lung cancer also applies to light smokers, who are ten times more likely to get lung cancer than non-smokers. Passive smoking, in other words breathing in someone else’s smoke, is also an increased risk factor for lung cancer.
Rarer causes of lung cancer include exposure to environmental carcinogens such as asbestos, arsenic or radon gas. The effects of exposure to these carcinogens can be much more lethal in smokers.
Smoking marijuana can result in even more tar getting to the lungs than cigarettes and is a recognised cause of lung cancer. As marijuana is an illegal substance, it is not possible to control whether it contains other harmful substances such as pesticides or other additives. Marijuana joints tend to be inhaled very deeply and smoked all the way to the end, where the tar content is the highest.
Chronic inflammation of the lungs such as from tuberculosis, some types of pneumonia and air pollution can also be potential risk factors for lung cancer.
Prevention of Lung Cancer
Lung cancer kills more men than any other cancer worldwide. The vast majority of all lung cancer cases in men are related to smoking. Avoid cigarette smoke, including second-hand smoke. If you smoke cigarettes, stop.
Avoid exposure to environmental pollutants such as asbestos, arsenic, radon and air pollution. Eat well; a diet rich in natural antioxidants such as plenty of fresh fruit and vegetables may have some protective benefits. Make sure you get at least five portions of fresh fruit and vegetables a day. Keep your alcohol consumption within safe limits.
How Is Lung Cancer Diagnosed?
In addition to a complete medical history and a physical examination, procedures used to diagnose lung cancer may include the following:
- A chest x-ray – to look for any mass or spot on the lungs
- Bronchoscopy – this is where a thin flexible tube with a good light source is put into the main tubes of the lungs. This test helps to evaluate and diagnose lung problems, assess blockages and obtain samples of tissue and/or fluid.
- A CAT scan is sometimes used; this can show detailed images of any part of the body and is much more detailed than an x-ray.
- Sputum cytology – the study of phlegm (spit) cells under a microscope.
- Needle biopsy – this is where a sample of the mass is removed and evaluated under a microscope. This can help determine which type of lung cancer you have.
- Other types of scan such as MRI scans, bone scans or PET scans may be needed to determine if the cancer has spread from where it started into other areas of the body.
Treatment for Lung Cancer
Surgery, radiation therapy and chemotherapy may all be used in the treatment of lung cancer. Surgical removal is the treatment of choice if this is possible. Sometimes this can be done successfully. However, if there are multiple tumours or if the tumour is too close to the big blood vessels in the lungs, then non-surgical options need to be considered, including radiotherapy and/or chemotherapy. Some types of lung cancer are more susceptible to chemotherapy than others. This is a decision that your cancer specialist will help you with, taking account not only of your individual medical history, but also your own preferences and wishes.
Colon Cancer
Colon cancer (also known as bowel cancer or colorectal cancer) is the second most common cancer in Irish men. About 1,800 cases are diagnosed in Ireland each year and the average lifetime risk for men is about 3 per cent. Colon cancer is both preventable and curable. It can be prevented by removing pre-cancerous colon polyps (see below). It can be cured if it is found early and surgically removed before it spreads to other parts of the body. However, colon cancer remains a major cause of death and disease in Irish men. The rates of colon cancer are predicted to increase by 50 per cent by the year 2020. Early detection of colon cancer can improve the chances of a cure and overall survival.
What Is the Colon?
The colon is a long, muscular hollow tube about 6 feet long and is the part of the digestive system where waste material is stored. It receives undigested food from the small intestine. It removes water from the undigested food, stores it and then finally eliminates it from the body through bowel movements. The rectum is the end of the colon beside the anus or back passage.
What Are the Risk Factors for Colon Cancer?
Factors that have been shown to increase a man’s risk of colon cancer include a diet high in fat, polyps in the colon, a family history of colorectal cancer and medical conditions such as ulcerative colitis.
Diet and Colon Cancer
Diets high in saturated fat are believed to increase the risks of colon cancer. In countries with high rates of bowel cancer, the fat intake by the population is much higher than in countries with low cancer rates. Breakdown products of fat metabolism are thought to lead to the formation of cancer-causing chemicals (carcinogens). Diets high in vegetables and high-fibre foods such as wholegrain breads and cereals may rid the bowel of these carcinogens and help reduce the risk of cancer.
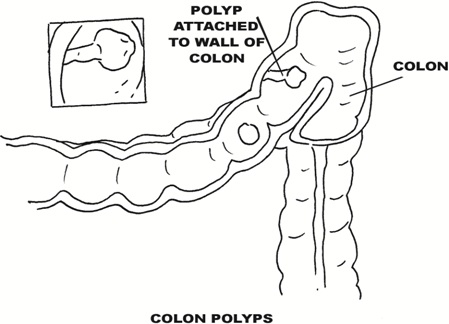
Colon Polyps and Colon Cancer
Polyp is the name given to small mushroom-like growths that can appear on the lining of the colon. Colon polyps are initially benign but over years can acquire additional chromosome damage to become cancerous. Some polyps can be pre-cancerous but can be present for many years before they turn into cancer. Doctors believe that most colon cancers develop in colon polyps. Therefore, removing benign colon polyps can prevent colorectal cancer. This can be easily done during a colonoscopy (see pages 121–122).
Know Your Genes – The Genetics of Colon Cancer
Your genetic makeup is an important colon cancer risk factor. The lifetime risk of developing colon cancer is thought to be about 3 per cent. But, if a first degree relative (parent, sibling or child) has bowel cancer then your lifetime risk increases to 9 per cent. However, despite this hereditary risk, most colon cancers still occur in patients who have no family history of colon cancer.
Men who have hereditary colon cancer syndrome tend to develop large numbers of colon polyps at a young age, and are at a very high risk of developing colon cancer early in life. Such a person can develop hundreds or thousands of colon polyps, starting during the teenage years, and is almost certain to develop colon cancer from these polyps by the age of 40. They are also at risk of developing cancers in other organs. Treatment involves removal of the colon at an early age.
Other men start to develop many colonic polyps, which eventually become cancerous, from the age of 30 onwards. Hence it is important to know your family history and get yourself properly checked out.
Ulcerative Colitis and Colon Cancer
Chronic ulcerative colitis is a condition that causes inflammation of the lining of the colon. Colon cancer is a recognised complication of chronic ulcerative colitis and is related to the location and the extent of the disease. Therefore, if you suffer from this condition, regular colonoscopies are recommended to look for pre-cancerous changes.
Other Risk Factors for Colon Cancer
Cigarette smoking has been associated with an increased risk of colon cancer. Patients with diabetes are more likely to be diagnosed with colon cancer. Obesity is associated with an increased risk, as is having a beer belly. Excess alcohol (more than 4 units per day), particularly beer consumption, is an associated risk factor for colon cancer.
What Are the Symptoms of Colon Cancer?
Bowel symptoms may include some or all of the following:
- A persistent change in bowel habit, such as constipation, diarrhoea or alternating constipation and diarrhoea
- Bleeding from the back passage
- Narrow stools
- A feeling of incomplete emptying of the bowel when going to the toilet
- A straining feeling or discomfort in the back passage
- Abdominal pain, cramps or bloating
Colon cancer can be present for several years before symptoms develop. Other symptoms of colon cancer can include fatigue, nausea, weakness, loss of appetite and weight loss. Symptoms vary according to where in the large bowel the tumour is located. The right side of the colon is spacious, and cancers in this area can get big before they cause any abdominal symptoms. These cancers tend to cause iron deficiency anaemia due to the slow loss of blood over a long period of time. Iron deficiency anaemia causes fatigue, weakness and shortness of breath.
The left side of the colon is narrower than the right side and cancers here are more likely to cause partial or complete bowel blockage or obstruction. Cancers causing partial bowel obstruction can cause symptoms of constipation, narrowed stools, diarrhoea, abdominal pains, cramps and bloating. Bright red blood in the stool may also indicate a growth near the end of the left side of the colon or rectum.
If you have these symptoms you should see your doctor without delay. However, other conditions, such as irritable bowel syndrome (spastic colon), ulcerative colitis, Crohn’s disease, diverticulosis, and peptic ulcer disease, can all have symptoms that mimic colon cancer.
Early diagnosis of bowel cancer is very important because the percentage chance of cure is directly related to how far advanced the condition is when it is diagnosed. So, if bowel cancer is still located within the bowel wall, the chances of cure may be as high as 100 per cent. Tragically, many Irish men fail to report early warning symptoms of bowel cancer and may put up with these symptoms for many months before seeking help. Delay of this sort can spell disaster.
What Tests Can Be Done to Detect Colon Cancer?
There are a number of tests available to detect colon cancer. These include colonoscopies, enemas, blood tests, digital rectal examination and stool occult blood testing, and genetic testing. The diagnosis is confirmed by the pathological analysis of a sample of the colon. Other tests, including scans, are used if the cancer has spread to other parts of the body, particularly the liver or bones.
Colonoscopy
The best test is usually a colonoscopy. This is where a long, thin, flexible tube, about the thickness of a finger, is put into the back passage. It has a camera at one end and a good light source that allows the bowel lining to be thoroughly examined. Any suspicious areas or growths such as polyps can be biopsied (removed) and sent for further analysis.
Screening Colonoscopy
Regular screening reduces the risk of dying from colon cancer. A screening colonoscopy test is recommended for Irish men at average risk generally every few years from the age of 50 upwards. Men with a higher risk of developing colon cancer may need to start this at an earlier age. This includes men who have a first degree relative with either colon cancer or polyps. These men may need to start screening colonoscopies from the age of 40 or sometimes earlier. Therefore it is important to be aware of your family history, as a family history of colon polyps or colon cancer merits close attention to your colon.
Barium Enema
Sometimes an alternative test called a barium enema is done. This involves putting a white, chalky liquid containing barium into the back passage and taking x-ray pictures of the colon afterwards. Tumours and other abnormalities can appear as dark shadows on the x-rays.
Blood Tests
Blood tests can help in the diagnosis. For example, low iron (anaemia) in someone with suspicious symptoms (described above) will point in the direction of further tests. Sometimes, the doctor may obtain a blood test for carcinoembryonic antigen (CEA). CEA is a substance produced by some cancer cells. It is sometimes found in high levels in patients with colon cancer, especially when the disease has spread.
Digital Rectal Examination and Stool Occult Blood Testing
As part of an annual check-up with your own doctor, a digital rectal examination to check your prostate can at the same time examine the lower rectum and detect any low-lying rectal tumours. This is done by inserting a gloved and lubricated index finger into the back passage area. This can be followed by an FOB (faecal occult blood) test, whereby a sample of faeces is sent away to a laboratory to be analysed for the presence of tiny speckles of blood. This can be an important screening test for colon cancers and polyps. Tumours of the colon and rectum tend to bleed slowly into the faeces and the small amount of blood mixed into the faeces is usually not visible to the naked eye. A small amount of faecal sample is smeared on a special card for occult blood testing. Usually three consecutive faecal cards are collected. However, be aware many other conditions can cause occult blood in the faeces. It is also important to realise that if your faeces samples have tested negative for occult blood this does not necessarily mean the absence of colon cancer. Having said that, a man who tests positive for faecal occult blood is thought to have at least a 30 per cent chance of having a colon polyp and a 3 per cent chance of having colon cancer.
Genetic Counselling and Testing
Blood tests are now available to test for hereditary colon cancer syndrome. Families with many cases of colon cancer, especially at a young age, can be referred for genetic counselling followed possibly by genetic testing. The advantages of this process include identifying family members with a high risk of developing colon cancer so as to begin colonoscopies early, as well as alleviating concern for members who test negative for the defect.
Treatment of Colon Cancer
Surgical removal of the affected part of the colon is usually the treatment of choice. After the operation, a colostomy bag would be attached to the skin surface of the stomach wall to collect the faeces. This can be temporary or permanent, depending on where the cancer is located. Treatment often also requires chemotherapy or radiotherapy, depending on the type of tumour and where it has spread to. Sometimes chemotherapy is done even before surgery to reduce the size of the tumour. The long-term prognosis is related to how far the cancer has spread before it is diagnosed, with men having tumours confined within the wall of the colon doing best.
How Can Bowel Cancer Be Prevented?
The best way to prevent bowel cancer is to eat a diet rich in fibre and fresh fruit and vegetables and low in animal fat. This means less red meat, less processed or cured meats such as bacon, sausages and ham, less fatty processed foods such as cakes, biscuits and chocolate, and less alcohol.
Fibre is the insoluble, non-digestible part of plant material present in fruits, vegetables and wholegrain breads and cereals. It is thought that lots of fibre in your diet leads to the creation of bulky stools that can rid the intestines of potential carcinogens. In addition, fibre speeds up the passage of faecal material through the colon, which allows less time for a potential carcinogen to react with the colon lining.
Apart from a healthy diet and lifestyle, the most effective way to prevent colon cancer is early detection and removal of pre-cancerous colon polyps. Of course, even in cases where cancer has already developed, early detection still significantly improves the chances of a cure by surgically removing the cancer before the disease spreads to other organs.
Regular physical exercise appears to be beneficial in terms of reducing the risk of colorectal cancer. Statins, which are used to treat high cholesterol, have recently been shown to possibly have a protective effect against bowel cancer. Taking supplements of folic acid may have some protective effect on colon cancer. Other agents being evaluated as possibly helping to prevent colon cancer include calcium, selenium and Vitamins A, C and E. More studies are needed before these agents can be recommended for widespread use by the public to prevent colon cancer. Taking low-dose aspirin can also have some protective benefit against bowel cancer. However, the flip side of this is that regular aspirin can slightly increase your risk of bleeding. Discuss the potential benefits of low-dose aspirin with your family doctor.
Unfortunately, colon cancers can be well advanced before they are detected. Being aware of the early warning signs of bowel cancer is important, so you can seek immediate help if need be.
Stomach Cancer
Stomach cancer remains one of the most common forms of cancer. However, the worldwide incidence of stomach cancer has declined rapidly over recent decades. Part of the decline may be due to awareness and treatment of helicobacter infection (see below). The increased use of refrigerators in recent decades has improved the storage of food and means that fresh food and vegetables (a valuable source of antioxidants important for cancer prevention) are more easily available. It has also led to a reduction in bacterial and fungal contamination, as well as salt-based preservation of food.
Symptoms to suggest stomach cancer include vague discomfort in the abdomen, loss of appetite, indigestion, heartburn or ulcer-like symptoms, a sense of fullness after eating a small meal, nausea, vomiting and abdominal swelling. Unfortunately, stomach cancer usually has no symptoms until the later stages. The optimal treatment of stomach cancer is the subject of ongoing research and usually involves some combination of surgery, chemotherapy and radiotherapy.
Causes of Stomach Cancer
The exact cause of stomach cancer is unknown. However, cigarette smoking and alcohol abuse increase the risk of stomach cancer. Dietary factors implicated in stomach cancer include a high-salt, processed-food diet with little fresh fruit and vegetables. Processed foods often contain nitrates, which can then be converted in the body to nitrosamines – potentially potent carcinogens. Stomach cancer is twice as common in men as in women. Infection of the stomach with the bacteria Helicobacter pylori is an important risk factor for stomach cancer.
Prevention of Stomach Cancer
As well as general advice regarding not smoking and not abusing alcohol, it is important to eat a good diet: one rich in fresh fruit, vegetables and beans, and with plenty of wholegrain breads and pasta. Processed foods and smoked foods should be avoided. As a man you should consider getting yourself tested for the presence of Helicobacter pylori.
What Is Helicobacter Pylori (H. Pylori)?
H. pylori is a spiral-shaped bacterium found in the stomach, which (along with acid secretion) can damage the stomach and part of the bowel known as the duodenum. It is the leading cause of ulcers. It was discovered by an Australian medical student in 1991 – quite a breakthrough as up until then nothing was thought to be able to live in the strongly acidic environment of the stomach. It is not known what causes certain people to develop H. pylori. In recent years it has been shown to be a risk factor for stomach cancer and is now classified as a carcinogen. Therefore it is worth getting tested for it and treated. Most people will never have symptoms or problems related to H. pylori infection. When symptoms are present, they may include a multitude of stomach-related symptoms, including heartburn, bloating and wind, as well as tummy discomfort, which may be relieved by eating. Always consult your doctor to have your symptoms evaluated.
The presence of Helicobacter pylori can be diagnosed either by a blood test or by having a gastroscopy, in which a thin flexible tube with a light source is inserted into the stomach to view its inner lining. A sample of tissue can be removed and an on-the-spot test, known as the urease test, can be done to diagnose the presence of Helicobacter. Urease is an enzyme made by the H. pylori bug. Another option is the hydrogen breath test where you blow into a hydrogen-based machine. H. pylori can be successfully treated and eradicated in most cases with a short course of antibiotics combined with a tablet to turn off the acid tap in the stomach. These tests can also be done to ensure proof of cure after treatment to make sure the bug is gone.
Skin Cancer
Skin cancer is a common cancer in Irish men and is on the increase. Unlike many other types of cancer however, only a small minority of those affected by skin cancer will actually die of the condition.
What Are the Different Types of Skin Cancer?
There are three main types of skin cancer. The most common types of skin cancers are basal cell (BCC) and squamous cell (SCC) skin cancers. These can be disfiguring but are unlikely to spread to other parts of the body and so are rarely fatal. The least common form of skin cancer is also the most dangerous and is called malignant melanoma.
Basal Cell Cancer
This is the most common type of skin cancer and accounts for about 75 per cent of all cases. It often looks like a small, raised pearl-like bump or nodule on a sun-exposed area of skin on the head, face, neck or back of the hands. It can easily be mistaken for a sore that doesn’t heal. This highly treatable cancer tends to start in the top layer of skin and grows very slowly. It commonly occurs among persons with light-coloured eyes, hair and complexion. Untreated, it can eventually spread down through the skin, which is why it has the alternative medical term of a ‘rodent ulcer’.
Squamous Cell Cancer
This is the second most common form of skin cancer and accounts for about 20 per cent of cases. It often looks like a raised crusted lesion on the sun-exposed areas of skin. Symptoms may include any spot or sore on the skin that changes or fails to heal, as well as localised scaliness, oozing, bleeding, itching, tenderness or pain at the site of the spot. Squamous cell carcinoma, although more aggressive than basal cell carcinoma, is highly treatable. It may appear as nodules or red, scaly patches of skin, and may be found on the face, ears, lips and mouth. Squamous cell carcinoma, if untreated, can spread to other parts of the body. This type of skin cancer is usually found in fair-skinned people.
Malignant Melanoma
Malignant melanoma is the least common but most dangerous form of skin cancer. It affects about 500 people each year in Ireland and its incidence is on the rise. Risk factors for developing malignant melanoma include a history of melanoma in the family. Those with certain skin types are at increased risk of melanoma, particularly those who are fair-skinned with blue eyes, and men who develop lobster-type skin after a few days in the sun. Having a lot of moles on your skin is termed dysplastic naevus syndrome and is associated with an increased lifetime risk of developing melanoma. Some people are born with very large moles on their bodies that are at increased risk of turning into melanoma over the long term.
Malignant melanoma starts in the melanocyte cells that produce pigment in the skin. It usually begins as a mole that then turns cancerous. This cancer may spread quickly.
Diagnosis
The warning signs for melanoma are either the arrival of a new mole or a change in an existing mole. The most useful signs in a mole are:
- An increase in size
- A change in shape
- A change in colour
- Bleeding, crusting, itching or altered sensation
Also look out for the ABCD of mole changes, which are a red alert for possible melanoma:
- Asymmetry – one half of the mole different from the other
- Border – an irregular edge to the mole
- Colour – colour variation within the mole, i.e. light and dark brown areas
- Diameter – generally moles greater than 6 millimetres in diameter (the end of a pencil)
Any new or existing mole with these changes must be fully removed. As with many other cancers, early detection greatly increases the chance of long-term cure as the survival rate from melanoma is directly related to the depth and thickness of the mole at the time of removal. If you are concerned or unsure about any mark or mole on your skin, discuss this with your family doctor.
What Are the Risk Factors for Skin Cancer?
- Skin cancer is more common in fair-skinned people, especially those with blond or red hair and those who have light-coloured eyes.
- A family history of melanoma.
- Sun exposure – the main risk factor is ultraviolet light and sunburn. In particular, blistering sunburns in childhood and adolescence significantly increase the risk of developing malignant melanoma. Overexposure to ultraviolet radiation from the sun can cause skin cancer. Sun exposure between 10 a.m. and 4 p.m. is most intense and therefore most harmful.
- Sunbed use is associated with skin cancer, including melanoma.
- Many ordinary moles on the skin (more than fifty).
- Funny-shaped moles (known as dysplastic naevi).
- Chronic non-healing wounds, especially burns.
- Those who work outdoors, such as construction workers and farmers, have increased risk.
Know Your Skin, Know Your Moles
It is important to examine your skin on a regular basis and become familiar with moles, freckles and other skin blemishes. This will allow you to better identify changes at an early stage. Be alert to changes in the number, size, shape and colour of pigmented areas. Finding suspicious moles or skin cancer early is the key to treating skin cancer successfully. Some moles are not easy to watch, particularly those on the back, so you may need your partner’s help here. Getting your moles looked at as part of a check-up with your doctor is also a good idea. Sometimes taking a photo of a mole allows you to see if it is changing over time.
Treatment of Skin Cancer
Most skin cancers are treated by simply removing the lesion. This is then analysed in the pathology laboratory under the microscope to confirm the diagnosis. Sometimes small non-melanoma skin cancers can be successfully treated by freezing the cancer off or by radiation treatment.
For melanoma, subsequent treatment will depend on how far the condition has spread prior to diagnosis. Interferon, a drug that alters the immune system, is sometimes used to treat patients with melanoma.
Prevention of Skin Cancer
The best way to prevent skin cancer is to be sun aware and protect your skin:
- Avoid sunburn and avoid excessive sun exposure. Minimise exposure to the midday sun (10 a.m. to 4 p.m.), when the sun is highest in the sky.
- Apply sunscreen all over your body and regularly use a broad-spectrum sunscreen with an SPF of 15 or higher, even on cloudy days, on all areas of your body that are exposed to the sun. This protects against both UVA and UVB rays.
- Reapply sunscreen every 2 hours, even on cloudy days. Reapply after swimming or perspiring.
- Avoid exposure to UV radiation from sunlamps or tanning parlours.
- Wear protective clothing. Hats should provide shade for both the face and back of the neck. Wearing sunglasses will reduce the amount of rays reaching the eye by filtering most of the rays. This helps to protect the eyelids as well as the lens.
- Remember, sand and pavements reflect UV rays even under an umbrella. Snow is a particularly good reflector of UV rays. Reflective surfaces can reflect up to 85 per cent of the damaging sun rays. Don’t forget your sunscreen on your skiing holiday.
Testicular Cancer
Testicular cancer is a young man’s disease. It is the most common form of cancer in men between the ages of 15 and 34. Testicular cancer is the exception to the rule that most cancer occurs in middle-aged or older men. It is more common in white men, for reasons that are unknown.
The incidence of testicular cancer has been increasing in recent years. However it is one of the most curable forms of cancer, provided it is diagnosed early, which is why awareness of it is so important. Practising regular testicular self-examination (see Chapter 12) allows testicular problems, including testicular cancer, to be diagnosed early and cured. Tragically, many men still remain unaware of the importance of this simple and potentially life-saving measure. And many men who are aware still delay unnecessarily before seeking medical help.
Testicular cancer is a ‘germ cell cancer’ as the cells which become cancerous are those involved with making sperm. Testicular cancers are divided into two main types, depending on the type of cell causing the cancer: seminomas, which occur in about half of all cases, and non-seminomas, which make up the rest and are mainly teratomas, but include some other rare types. It is important to know which kind of cell the cancer started from because these types of cancer may be treated differently.
Symptoms of Testicular Cancer
The following are the most common symptoms of testicular cancer. However, each individual may experience symptoms differently. The symptoms of testicular cancer may resemble other conditions or medical problems. The most common symptoms include:
- A lump in either testicle, usually painless
- Enlargement of a testicle
- A feeling of heaviness in the scrotum
- A dull ache in the lower abdomen or groin
- A sudden collection of fluid in the scrotum
- Pain or discomfort in a testicle or the scrotum
- Enlargement or tenderness of the breasts
What Causes Testicular Cancer?
The exact cause of testicular cancer is not known. In many cases testicular cancer develops for no apparent reason. However, there are a number of risk factors that can increase the risk of getting the disease:
- Age – most testicular cancers occur in young men between the ages of 15 and 40.
- A history of an undescended testicle(s). This increases the risk of testicular cancer in later life, which is why an undescended testis should always be ‘brought down’ into the scrotum. This allows any later changes in it to be detected at an early stage.
- Family history of testicular cancer
- A personal history of cancer in the other testicle
- Race/ethnicity – the rate of testicular cancer is higher in white men than in other population groups, which suggests that some genetic or environmental factor is involved.
- HIV infection
- Men whose mothers took a hormone called DES (diethylstilbestrol) during pregnancy to prevent miscarriage.
Can Testicular Cancer Be Prevented?
Currently, we don’t know if or how testicular cancer can be prevented because there is no known cause of the disease; many of the suggested risk factors are those that cannot be changed and many men who get testicular cancer do not have the suggested risk factors.
How Is Testicular Cancer Diagnosed?
The key is to notice any lump or abnormality in the testes and get this checked out by your doctor. However, it is important to remember that most lumps or abnormalities detected are not cancer. If you are suspicious about a testicular swelling then further tests may include the following:
- Ultrasound – a simple and painless diagnostic scan where gel is put on the scrotum and a probe is used to look at the testes. This test can help tell if the lump is likely to be a tumour or a benign fluid-filled cyst.
- Blood tests – certain blood proteins, known as tumour markers, can be raised in men with testicular cancer. Blood tests that measure these tumour markers can be used to help confirm the diagnosis and also as a means of monitoring treatment.
- Biopsy – a procedure in which a sample of testicular tissue is removed with a needle or during surgery for detailed analysis to determine if cancer or other abnormal cells are present.
If you are confirmed to have testicular cancer then further tests, including scans, are carried out to see if it has spread elsewhere in the body. This helps to determine the best treatment plan.
Treatment for Testicular Cancer
There are several kinds of treatment for testicular cancer. The treatment advised for each case depends on various factors, such as the type of cancer (seminoma or non-seminoma), how far it has spread and your general health.
Surgical removal of the affected testicle is advised in almost all cases. This alone may be curative if the cancer is at an early stage and has not spread. Radiotherapy, to destroy cancer cells or slow the rate of growth, may be done after surgery for men with seminoma tumours to prevent recurrence. Chemotherapy using anti-cancer drugs to destroy cancer cells throughout the body has greatly improved the cure rates of both seminomas and non-seminoma testicular tumours.
What Is the Prognosis?
The prognosis is usually good. Most testicular cancers are diagnosed at an early stage, and after treatment over 90 per cent of men are completely cured. Even if the testicular cancer has spread to other parts of the body there is still a good chance of being cured. After treatment you will be monitored regularly for a number of years to make sure the cancer hasn’t come back. This will involve blood tests to measure the tumour markers and sometimes scans as well.
If you have one testis removed, it should not affect your sex life. You should still have normal erections and produce sperm and hormones from the other testis, and so can still father children. However, if you have chemotherapy or radiotherapy, this may affect fertility. You should discuss this with your specialist.
Bladder Cancer
The bladder is a triangular-shaped, hollow organ located in the lower abdomen. The role of the bladder is to store urine; its walls relax and expand to store urine, and contract and flatten to empty urine through the urethra. Bladder cancer occurs when there are abnormal, cancerous cells growing in the bladder. Bladder cancer affects men two to three times more frequently than women.
What Are the Risk Factors for Bladder Cancer?
While the exact causes of bladder cancer are not known, there are well-established risk factors, which include the following:
Cigarette Smoking
By far and away the most important cause of bladder cancer is cigarette smoke. Smoking causes about half of the deaths from bladder cancer among men. There are over fifty different carcinogens in tobacco smoke. When these are inhaled through the lungs into the bloodstream these carcinogens eventually end up in the bladder before being excreted through the urine. The disease occurs in smokers twice as often as non-smokers.
Occupational Exposure
Certain occupations and work environments that expose workers to dyes and some organic chemicals appear to increase the risk of developing bladder cancer. Workers in the rubber, chemical, leather, textile, metal and printing industries are exposed to substances such as aniline dye and aromatic amines that may increase their risk of bladder cancer. Other at-risk occupations include hairdressers, machinists, painters and truck drivers.
Chronic Bladder Irritation
Chronic bladder infections or bladder stones may be linked to certain types of bladder cancer. Infection with certain parasites found in tropical regions of the world can increase the risk of bladder cancer.
Other Risk Factors
The risk of developing bladder cancer increases as a man gets older. It is more common in white men and those with a family history of bladder cancer.
What Are the Symptoms of Bladder Cancer?
Every man may experience symptoms differently and, in the early stages, bladder cancer can be asymptomatic. Symptoms may include blood in the urine; this may be visible to the naked eye, in that the urine looks discoloured, or it may be picked up on examination of the urine by your doctor. Other symptoms include pain or discomfort on urination, frequently feeling the urgent need to urinate, frequent urination and pelvic or flank pain. These symptoms of bladder cancer may resemble other medical conditions or problems and it is important to consult your doctor for advice.
How Is Bladder Cancer Diagnosed?
In addition to a complete medical history and physical examination, diagnostic procedures for bladder cancer may include the following:
Laboratory Tests
Tests can be carried out on the urine to check for the presence of blood, chemicals and bacteria. The urine may be examined microscopically or grown in culture to check for infection. Cancerous cells may be detected using the microscope. Blood tests can also be carried out.
Cystoscopy
This is an examination in which a thin flexible tube and viewing device is inserted through the urethra to examine the bladder and urinary tract for structural abnormalities or obstructions, such as tumours or stones. Samples of the bladder tissue (a biopsy) may be removed through the cystoscope for examination under a microscope in the laboratory.
Intravenous Pyelogram (IVP)
This is a series of x-rays of the kidney, ureters and bladder performed after the injection of a contrast dye into the veins. This test is used to detect tumours, abnormalities, kidney stones or any obstructions, and to assess renal blood flow. It may also be used to rule out other diseases or check for spread (metastasis) of the bladder cancer to other areas of the urinary tract.
What Is the Treatment for Bladder Cancer?
About 70–80 per cent of individuals with bladder cancer have superficial and non-invasive tumours. Treatment of these tumours is often very effective and results in an excellent prognosis. Less often, bladder tumours become more invasive and can spread to other organs. Depending on the extent, bladder cancers may be managed with a single therapy or a combination of treatments, including surgery, radiation therapy and chemotherapy.
How Do You Prevent Bladder Cancer?
While there is no known way to prevent bladder cancer, you can reduce your chances of developing the disease. The best way to do this is to quit smoking and avoid any potential exposure to known bladder carcinogens, such as benzene. As with the prevention of other cancers, it is thought that a diet rich in fresh fruit and vegetables and low in saturated fat is helpful. Drinking plenty of fluids and keeping your urine clear at all times allows toxins to be cleared from the body. Drinking lots of fluids may also limit the time that cancer-causing substances present in urine will remain in contact with bladder cells.
Breast Cancer in Men
Breast cancer in men is uncommon. Less than 1 per cent of all breast cancers occur in men. Although men of all ages can be affected with the disease, the average age at diagnosis is between 60 and 70.
What Are the Risk Factors for Breast Cancer in Men?
Risk factors may include a family history of breast cancer in female relatives. Other factors may include radiation exposure and medical conditions associated with high oestrogen states, such as cirrhosis of the liver.
What Are the Symptoms of Breast Cancer in Men and How Is it Treated?
Every man may experience symptoms differently. Symptoms may include breast lumps, nipple inversion, a nipple discharge (sometimes bloody) or atypical pain or a pulling sensation in the breast. Keep in mind that these symptoms of breast cancer may resemble many other medical conditions. It is important to consult your doctor for advice. Overall survival rates are similar to that of women with breast cancer.
The main treatment is surgical removal, and other treatment options include radiation therapy and chemotherapy.
Liver Cancer
Liver cancer is a rare cancer in men and usually involves a cancer elsewhere in the body spreading to the liver. The main cause of cancer originating in the liver itself is the hepatitis B virus infection, which is why vaccination against hepatitis B is so important for individuals at risk of contracting it. This virus spreads through contact with infected blood. Other infections that can cause liver cancer include hepatitis C, which is also spread via infected blood and other body fluids. Cirrhosis, usually but not always caused by excess alcohol, can also cause liver cancer. Some foodstuffs such as aflatoxin mould on peanuts, for example, can cause liver cancer.
Symptoms of Liver Cancer
Symptoms of liver cancer include yellow jaundice, loss of appetite, weight loss and pain or swelling in the upper abdomen.
Prevention of Liver Cancer
The best way to prevent liver cancer is to avoid hepatitis B or C infection. The most common form of hepatitis (hepatitis A) is not a risk factor for liver cancer. Hepatitis B and C are spread by contact with contaminated body fluids, most commonly blood or saliva. Practising safe sex, including the use of condoms, and avoiding sharing needles are important. There is a vaccine available to prevent hepatitis B. Unfortunately there is no vaccine available yet for the hepatitis C infection. You can also help prevent liver cancer by avoiding drinking excess alcohol, thereby preventing liver cirrhosis.
Treatment of Liver Cancer
Specific treatment for cancer will be determined by your doctors in consultation with you. Factors to be taken into consideration will include:
- The extent of the cancer – how far it has spread
- Your overall health, age and other medical conditions
- Your tolerance for specific medications, procedures or therapies
- Your ideas, concerns and expectations
- Your opinions or preferences
Key Points

- Cancer is common among Irish men. The ‘big four’ cancers in Irish men are skin, prostate, colon and lung cancers. Testicular cancer is the most common cancer in young men.
- The number of new cancer cases in Irish men may double between 2000 and 2020. Many cancers can be prevented by leading a healthy lifestyle and by being aware of potential warning symptoms and signs. Knowledge is power!
- The good news is that cancer survival is improved by earlier detection and improved treatment.
- Know the ABC of cancer in men:
- Awareness of the symptoms
- Be alert to the causes – maximise your chances of preventing cancer
- Catch it in time – maximise the chance of cure
 Cancer is a serious health issue for Irish men. About one in every three Irish men will develop cancer at some stage in their lives and about one in six men will die from it. The word ‘cancer’ is often perceived as a frightening one, yet cancer is not the hopeless diagnosis it once was. Many cancers can now be prevented through the combination of a healthy lifestyle and regular check-ups. Those cancers that can be detected early can be treated before it is too late. Unfortunately, research has shown that Irish men tend to ignore warning symptoms and present late to their doctor for check-ups and medical advice. Through a combination of fear, denial, embarrassment and lack of time, men often ignore their own health, to their cost. The national cancer registry has shown that rates of common cancers in Irish men are set to increase by over 50 per cent by 2020. The four most common cancers in men are:
Cancer is a serious health issue for Irish men. About one in every three Irish men will develop cancer at some stage in their lives and about one in six men will die from it. The word ‘cancer’ is often perceived as a frightening one, yet cancer is not the hopeless diagnosis it once was. Many cancers can now be prevented through the combination of a healthy lifestyle and regular check-ups. Those cancers that can be detected early can be treated before it is too late. Unfortunately, research has shown that Irish men tend to ignore warning symptoms and present late to their doctor for check-ups and medical advice. Through a combination of fear, denial, embarrassment and lack of time, men often ignore their own health, to their cost. The national cancer registry has shown that rates of common cancers in Irish men are set to increase by over 50 per cent by 2020. The four most common cancers in men are: