P450 ENZYMES: SUBSTRATES, INHIBITORS, INDUCERS
CYP1A2 ENZYME
| CYP1A2 SUBSTRATES | CYP1A2 INHIBITORS | CPY1A2 INDUCERS |
| Caffeine | Cimetidine (Tagamet) | Barbiturates |
| Clozapine (Clozaril) | Ciprofloxacin (Cipro) | Carbamazepine (Tegretol) |
| Mirtazapine (Remeron) | Fluvoxamine | Rifampin (Rifadin) |
| Olanzapine (Zyprexa) | Zileuton (Zyflo) | Smoking |
| Ramelteon (Rozerem) | ||
| Ropinirole (Requip) | ||
| Tizanidine (Zanaflex) | ||
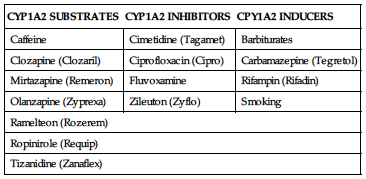
• CYP1A2 enzyme is increasingly involved in drug interactions.
• More potent inhibitors include cimetidine, ciprofloxacin, and fluvoxamine.
• Smoking is the most important inducer, but rifampin and barbiturates also can increase enzyme activity.
• Example of reaction: Tizanidine plasma concentrations increased more than 30-fold when the inhibitor fluvoxamine was given concurrently.
CYP2C9 ENZYME
| CYP2C9 SUBSTRATES | CYP2C9 INHIBITORS | CYP2C9 INDUCERS |
| Candesartan (Atacand) | Amiodarone (Cordarone) | Barbiturates |
| Celecoxib (Celebrex) | Clopidogrel (Plavix) | Carbamazepine (Tegretol) |
| Diclofenac (Voltaren) | Fluconazole (Diflucan) | Rifampin (Rifadin) |
| Glipizide (Glucotrol) | Metronidazole (Flagyl) | St. John’s wort |
| Glyburide (DiaBeta) | Sulfamethoxazole | |
| Ibuprofen (Advil, Motrin) | Valproic acid (Depakote) | |
| Irbesartan (Avapro) | ||
| Meloxicam (Mobic) | ||
| Warfarin (Coumadin) | ||
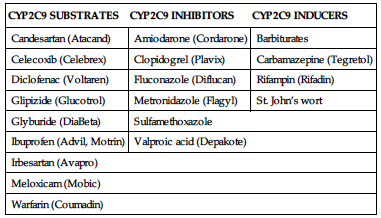
• More potent inhibitors include amiodarone, metronidazole, and sulfamethoxazole.
• All of the inducers can substantially increase enzyme activity.
• Both warfarin and oral hypoglycemics are of serious concern with regard to drug interactions. Substrates warranting attention include warfarin and oral hypoglycemics.
CYP2C19 ENZYME
| CYP2C19 SUBSTRATES | CYP2C19 INHIBITORS | CYP2C19 INDUCERS |
| Citalopram (Celexa) | Cimetidine (Tagamet) | Barbiturates |
| Diazepam (Valium) | Clopidogrel (Plavix) | Carbamazepine (Tegretol) |
| Escitalopram (Lexapro) | Esomeprazole (Nexium) | Rifampin (Rifadin) |
| Omeprazole (Prilosec) | Fluconazole (Diflucan) | St. John’s wort |
| Pantoprazole (Protonix) | Fluvoxamine | |
| Sertraline (Zoloft) | Modafinil (Provigil) | |
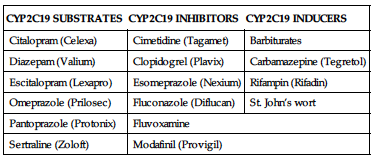
• Inhibition by itself does not frequently cause adverse effects compared with other CYP enzymes because many of the substrates do not have serious toxicity.
• Inhibition or induction of the enzyme nonetheless may result in an adverse drug interaction.
• Racial background is important in the likelihood of being deficient in this enzyme (e.g., 3%–5% of Caucasians and 12%–23% of Asians are poor metabolizers of this enzyme).
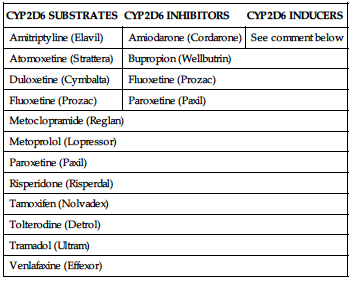
CYP2D6 ENZYME
| CYP2D6 SUBSTRATES | CYP2D6 INHIBITORS | CYP2D6 INDUCERS |
| Amitriptyline (Elavil) | Amiodarone (Cordarone) | See comment below |
| Atomoxetine (Strattera) | Bupropion (Wellbutrin) | |
| Duloxetine (Cymbalta) | Fluoxetine (Prozac) | |
| Fluoxetine (Prozac) | Paroxetine (Paxil) | |
| Metoclopramide (Reglan) | ||
| Metoprolol (Lopressor) | ||
| Paroxetine (Paxil) | ||
| Risperidone (Risperdal) | ||
| Tamoxifen (Nolvadex) | ||
| Tolterodine (Detrol) | ||
| Tramadol (Ultram) | ||
| Venlafaxine (Effexor) | ||
CYP3A4 ENZYME
| CYP3A4 SUBSTRATES | CYP3A4 INHIBITORS | CYP3A4 INDUCERS |
| Alfuzosin (Uroxatral) | Amiodarone (Cordarone) | Carbamazepine (Tegretol) |
| Alprazolam (Xanax) | Clarithromycin (Biaxin) | Efavirenz (Sustiva) |
| Budesonide (Entocort EC) | Diltiazem (Cardizem) | Phenobarbital |
| Carbamazepine (Tegretol) | Erythromycin (Ery-Tab) | Rifampin (Rifadin) |
| Cyclosporine (Neoral) | Fluconazole (Diflucan) | St. John’s wort |
| Fluticasone (Flovent) | Fluoxetine (Prozac) | |
| Lovastatin (Mevacor) | Itraconazole (Spoiranox) | |
| Repaglinide (Prandin) | Ketoconazole (Nizoral) | |
| Sildenafil (Viagra) | Verapamil (Calan, Isoptin) | |
| Simvastatin (Zocor) | ||
| Tadalafil (Cialis) | ||
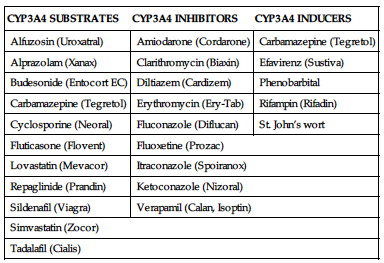
• This enzyme metabolizes about half of all medications on the market.
• Drug toxicity of CYP3A4 substrates due to inhibition of CYP3A4 is relatively common.
• This enzyme is very sensitive to induction, tending to lower plasma concentrations of substrates, resulting in reduced efficacy of the substrate.
• Most potent inhibitors include clarithromycin, itraconazole, and ketoconazole.
• Rifampin is a potent inducer and may reduce serum concentrations of substrates by as much as 90%.