CASE 45
Mary, a 3-year-old girl, had her spleen removed after a motor vehicle accident, in which both parents died. When she was transferred to the emergency department of a nearby hospital, it became apparent that her spleen had ruptured and the surgeon had no option but to remove it. Mary recovered well from the surgery, but her next of kin, who knows that the spleen is important in immune responses, wants to know how removal of the spleen will affect her immunologically, and so you arrange for a consultation with an immunologist.
QUESTIONS FOR GROUP DISCUSSION
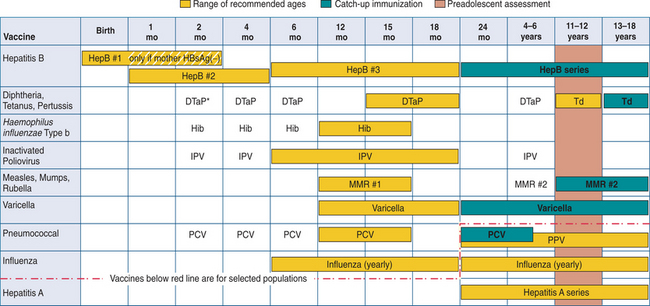
FIGURE 45-1 Childhood and adolescent immunization schedule, by vaccine and age, recommended by CDC’s Advisory Committee on Immunization Practices (ACIP), June 2004. (Abbreviations: HepB, hepatitis B; DTaP, diphteria, tetanus toxoids, and acellular pertussis; Hib, Haemophilus influenzae type b conjugate; IPV, inactivated polio; MMR, measles, mumps, and rubella; PCV, pneumococcal conjugate; Td, tetanus and diphtheria toxoids.
*DTaP (diphtheria, tetanus toxoids, and acellular pertussis) has replaced DTP/DPT (diphteria, tetanus toxoids, and whole cell pertussis) vaccine. Products containing whole cell pertussis vaccines have been discontinued. (Modified from Centers of Disease Control and Prevention. Recommended Childhood and adolescent, immunization schedule—United States, 2005. MMWR 53(51–52): Q1–Q3, 2005.)
RECOMMENDED APPROACH
Implications/Analysis of Family History
Family history is insignificant here because the asplenia was surgery related. In cases of congenital asplenia family history is significant because this disorder has an autosomal recessive mode of inheritance. The parents of these offspring can be normal, with each carrying this recessive gene. The presentation of the gene is more common in offspring of consanguineous marriages, a setting in which autosomal recessive disease is encountered more frequently than in outbred people. Chance alone predicts that most likely one in four offspring can be affected in such a family (both parents carriers), because in each pregnancy there is a one in four chance of the fetus inheriting the abnormal gene from both parents. The actual genetic defect causing asplenia in this case has not yet been identified.
Implications/Analysis of Clinical History
Mary’s growth and development have been normal. She suffered a middle ear infection (otitis media) at age 24 months, but otherwise she has had no other illnesses except for a common cold each winter. Having determined that Mary was a healthy child, your next consideration is her immunization record.
Childhood immunization is important, particularly if we are to maintain what is referred to as herd immunity (protection from spread of disease within a group because most members are immunized). However, in asplenic patients, immunization is recommended for their own protection. Mary’s medical files indicated that she had received most of the recommended pediatric vaccines and boosters. These included vaccines for DTaP (diphtheria, tetanus toxoids, and acellular pertussis), MMR (measles, mumps, rubella), hepatitis, and the inactivated poliovirus (IPV).
Of significance is the fact that Mary had already received the Hib vaccine (a conjugated capsular polysaccharide vaccine for Haemophilus influenzae type b), as well as the pneumococcal conjugate vaccine (PCV) for Streptococcus pneumoniae (PCV7/Prevnar). Haemophilus influenzae (type b) and Streptococcus pneumoniae are encapsulated bacterial pathogens that can enter the bloodstream where, in a normal patient, they would be eliminated in the spleen by innate and adaptive immune responses. In the absence of a spleen, patients who become infected with these encapsulated bacteria are at risk for fulminant pneumococcal sepsis, which is associated with high mortality.
Implications/Analysis of Laboratory Investigation
Given the fact that Mary is now without a spleen, antibody titers to various pediatric vaccines were requested to ensure that Mary was sufficiently protected. Although laboratory results indicated normal antibody titers, and even though Mary has been immunized with the pneumococcal conjugate vaccine Prevnar, there is concern that Mary is at risk for pneumococcal disease caused by pneumococcal serotypes not included in the this vaccine. The Prevnar pneumococcal conjugate vaccine (PCV7) contains only seven purified capsular polysaccharides of S. pneumoniae serotypes. These serotypes have been selected because they cause the majority of pneumococcal disease in children. Consequently, the Pneumovax 23 polysaccharide vaccine, which consists of 23 pneumococcal capsular types, was administered.
DIAGNOSIS
Mary had surgery-induced asplenia, resulting in a need for additional immunization and prophylactic antibiotics.
THERAPY
For broader protection, Mary was administered the Pneumovax 23 vaccine. Mary’s guardian should be notified that there is a low risk of encephalomyelitis with the vaccine.
Antibiotics were prescribed to be taken at a low dose daily but at higher doses when Mary has any dental work done or undergoes any invasive surgical procedure. As well, “flu shots” should be recommended in that respiratory virus infection can be lethal in both the elderly and in asplenic individuals. However, the vaccine is generally made to previous year’s agents and does not convey total resistance to current serotypes! Mary will still get a subclinical infection, but less severe than natural disease.
ETIOLOGY: STREPTOCOCCAL INFECTIONS AND IMMUNIZATION
Streptococcus pneumoniae, more commonly referred to as “pneumococcus,” is the causative agent of pneumonia, acute otitis media, meningitis, and sinusitis, particularly in young children. This infection is spread via respiratory droplets during sneezing/coughing or directly from person to person contact. As such it may be inhaled into the lungs and spread to the blood. Bacteria enter the bloodstream all the time, including when we brush our teeth or when we have a local infection, for example of the middle ear. Normally these bacteria are disposed of efficiently by the spleen. When the spleen is not present, serious or even fatal infections occur.
Clinical Presentation
A typical presentation of severe pneumococcal pneumonia would include unrelenting fever, elevated white blood cell count, and a “left shift,” indicating the presence of predominantly neutrophils, recruited to defend the body against bacterial infection. A chest radiograph would generally show infiltrates suggestive of consolidation.
Pneumococcal Polysaccharide Vaccines
The major components of the pneumococcal capsules are T cell–independent antigens. As the term implies, these antigens can activate B cells in the absence of cognate interaction with T cells. The predominant antibody isotype produced in response to T cell– independent antigens is IgM. As such the response is not long lasting and memory B cells are not generated. Therefore, protection is not long lasting. The Pneumovax 23 vaccine is a mixture of purified capsular polysaccharides from the 23 most prevalent S. pneumoniae serotypes causing infection in North America. Included in the vaccine are the seven serotypes in the Prevnar vaccine (see later). Protective antibodies are usually detectable 3 to 4 weeks after immunization. This vaccine is recommended for the elderly, the immunocompromised, and children older than the age of 2 who are congenitally asplenic or have had a splenectomy.
Responses to this vaccine have all the limitations of antibody responses to T cell–independent antigens. Furthermore, children younger than 2 years of age respond poorly to T cell–independent antigens because their immune system is immature. To overcome this limitation, a pneumococcal conjugate vaccine (Prevnar) was developed.
Pneumococcal Conjugate Vaccine
Conjugate vaccines are generally polysaccharide vaccines to which a potent T cell–dependent antigen is linked. The S. pneumoniae conjugate vaccine (Prevnar) consists of seven purified capsular polysaccharides each coupled to a carrier protein (nontoxic variant of diphtheria toxin). This conjugate vaccine triggers a T cell–dependent response that leads to the generation of IgG antibodies and memory B cells. As such, booster responses lead to enhanced antibody titers. Antibodies generated can serve as opsonins and facilitate the phagocytosis of S. pneumoniae.