For a person to be healthy and sustain life, several things must happen without fail. First, O2 must be able to enter the alveoli from the atmosphere, in a process called ventilation. Once in the alveoli, O2 must be able to enter the blood vessels at the same time CO2 is removed without interference, in a process called respiration. These 2 processes must happen in parallel, with the body taking in macronutrients (food) and having the ability to break down food into usable pieces through the process of digestion. These pieces then must be absorbed in the intestines and into the bloodstream and travel in the blood plasma to the destination tissues, with O2 riding attached to hemoglobin. Perfusion is O2 and nutrients getting to the destination cells and tissues. As long as all these processes continue uninterrupted, there should be no problems. However, if any of these processes is disrupted, hypoperfusion can occur and result in death if not recognized and reversed in a timely manner.
To maintain all the requirements for a fully functioning body, among other things, the body needs a functioning pump, a properly sized container, and an appropriate amount of fluid for the pump to move throughout the container. Shock can be thought of as any deviation from normal in any of these 3 requirements. Shock, and its severity, centers around blood pressure, so let’s start by explaining blood pressure.
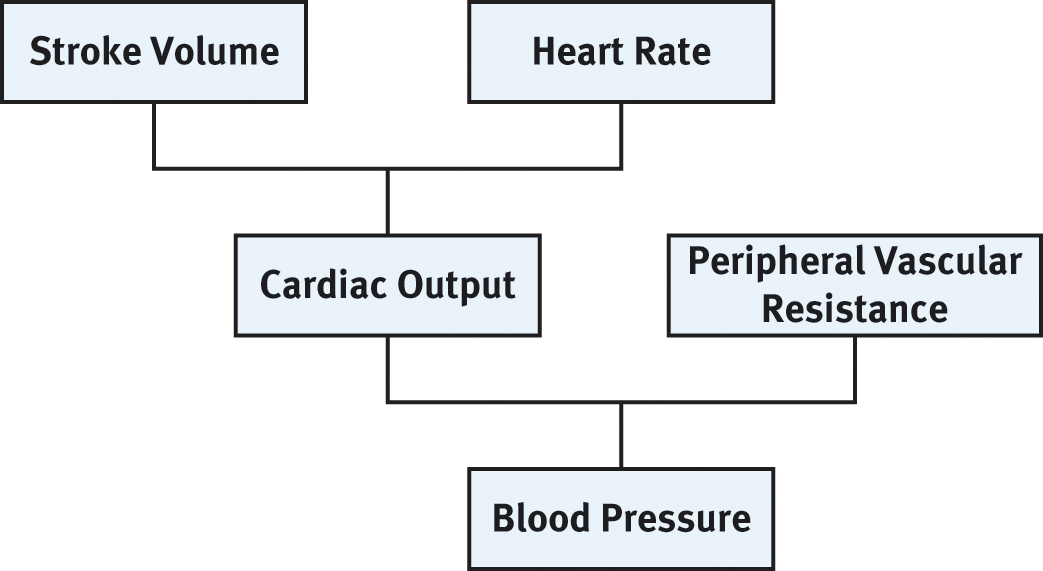
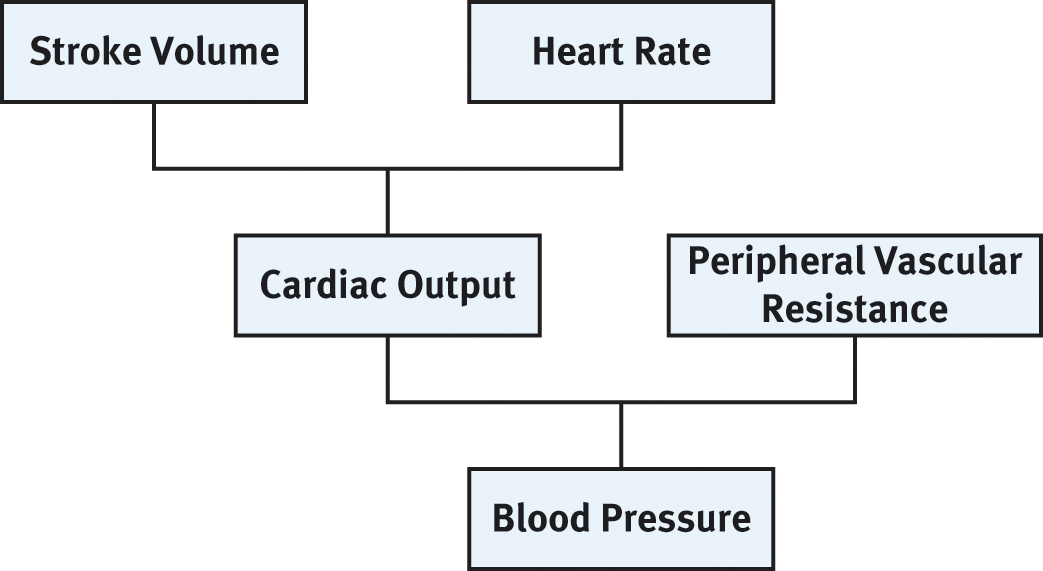
Blood pressure is dependent on cardiac output and peripheral vascular resistance. Cardiac output is the amount of blood pumped out of the heart in 1 minute; it is the product of stroke volume and heart rate. Peripheral vascular resistance is the resistance of blood flow through all the vessels of the body, excluding those in the lungs. Stroke volume is the amount of blood ejected from the left ventricle of the heart with each beat or contraction. Heart rate is the number of beats in 1 minute.
The heart must be able to adequately pump blood around the body, and, most importantly, it must have adequate strength to get blood up to the brain against gravity. By itself, pure muscle strength of the heart is not enough. There must be enough blood returning to the heart from the body to fill and stretch the chambers of the heart, which is called the preload. As blood flows into the heart chambers, the chambers stretch, thereby increasing the contraction strength of the heart. Finally, outflow of blood must not be obstructed. This afterload, or pressure against which the heart must pump, needs to be lower than the force of the heart’s contraction to overcome it. In the cases of myocardial damage, such as from a heart attack or cardiac contusion from trauma, the contractile strength of the heart is diminished, which will eventually lead to shock.
The vasculature (collection of blood vessels) must be of appropriate size for the amount of fluid contained within it. Under normal circumstances this is typically not an issue, but during severe blood loss or dehydration, the container as it is normally may be too large for the volume of blood remaining. In times of crisis, the autonomic nervous system is responsible for shutting down nonessential capillary beds, such as those found in the skin, and constricting the venous and arterial side of the vasculature. This effectively shrinks the overall size of the container to better match the volume within. Taken a step further, this measure will maintain blood pressure at least in the short term until fluid or blood can be replaced. In some instances, the vessels of the container may suddenly dilate, or get larger, resulting in the current fluid volume being too small, which can occur in cases of spinal trauma.
The blood has several responsibilities in the prevention of hypoperfusion. There must be an adequate number of red blood cells with hemoglobin capable of carrying O2. In cases of hemorrhage, insufficient red blood cells may be remaining to carry adequate O2 to the tissues. In this situation, the best efforts of fluid resuscitation and oxygenation will ultimately prove futile. In the case of anemia, there is insufficient hemoglobin to hold O2, potentially resulting in shock as well. Finally, the blood must be able to get to the end organ to deliver its O2 and nutrients. If the container remains constrained for too long, between starvation of the cells from a lack of nutrients and a buildup of waste products, cellular death and, eventually, organ death are inevitable.
A variety of things can affect the pump, the container, or fluid. Although they will all produce similar symptoms, their causes, and consequently the optimal treatment, are different. The types of shock you will encounter as a paramedic will be presented first, which is followed by a discussion of the progression and stages of shock. Finally, the end of this chapter addresses the assessment and treatment of shock in broad and general terms. In later chapters, these same causes of shock will be presented, including a discussion of more specific treatments. Here, the phrase treat for shock will be defined.
Cardiogenic shock, as the name implies, starts in the heart. This happens when the heart is no longer strong enough to move the blood around the body and through the lungs. It often results from a heart attack, or the cumulative damage from a series of heart attacks. This topic is covered in much greater detail in chapter 4.
Hypovolemic and hemorrhagic shock are 2 forms of shock that are similar but not exactly the same. Hypovolemic shock is exactly that; it is shock that results from a low circulating volume. It can be caused by excessive vomiting and diarrhea, poor fluid intake, or extravasation from burns. Hemorrhagic shock is a specific form of hypovolemic shock that occurs because of blood loss. The blood loss can be external or internal from trauma or can be from cumulative blood loss from gastrointestinal bleeding or something similar. Hemorrhagic shock carries with it the extra burden during resuscitation of replacing red blood cells. With hypovolemic shock, aggressive fluid administration often is sufficient.
Obstructive shock refers to a variety of disorders that hamper preload or elevate afterload to the point where cardiac function is disrupted. Some examples include pulmonary embolism (PE), pneumothorax, and blood return from the inferior vena cava.
Distributive shock is the collective name for several different causes of shock that all have displacement of fluid as a common thread. In each, fluid is somehow shifted from the vessels to other locations within the body. Septic shock, anaphylactic shock, neurogenic shock, and psychogenic shock are all forms of distributive shock.
Septic shock is caused by bacterial toxins infiltrating the bloodstream from a local infection or a systemic infection. The body’s reaction to this infection is to initiate a widespread inflammatory response, which causes systemic vasodilation and increased capillary permeability. In addition to being too small of a volume for the now dilated container, fluid leaks from the capillaries into the interstitial space (the potential space between the cells and outside the vasculature), further worsening hypovolemia.
Although our immune system is truly a marvel, occasionally, it short-circuits and wildly overreacts to an otherwise innocuous invader, such as bee venom or egg proteins. When this happens, it starts a complicated cascade of events that can eventually, and sometimes rapidly, lead to death. This is known as anaphylactic shock. During the progression of anaphylaxis, capillaries once again become leaky, and the vasculature dilates, leading to a state of profound hypotension. As if that were not enough, unlike in septic shock, this also happens in the airways, the lips, and the tongue, leading to difficulty breathing and asphyxiation.
Neurogenic shock is a type of shock resulting from some type of insult has occurred to the spinal cord. Sometimes it is caused by an infection, but most often, trauma is the cause. In addition to paralysis, which may be a patient’s complaint, the astute paramedic will be far more wary of systemic, uncontrolled dilation of all blood vessels inferior to the injury. Once again, the container is too large for the fluid within (though, thankfully, the capillaries are not leaky), and profound hypotension ensues. In addition, the area affected by the vasodilation will not be sweating like the area superior to it. Because the blood vessels nearest the skin of the affected area also are dilated, the skin also will appear flushed, whereas the remainder of the body will be white or grey.
Psychogenic shock is not mentioned in many texts; however, it is worth noting here. Psychogenic shock is the “see-blood-and-faint” variety of shock, and, yes, it is real. In cases where a person becomes scared or otherwise overwhelmed, such as from negative news, blood vessels dilate, if only transiently, resulting in a container too big for the fluid. Often, the person passes out briefly; once supine, the patient regains consciousness as the nervous system recovers and regains control.
Whatever the cause of the shock, all forms will progress through 3 distinct phases, culminating in certain death if not recognized early and treated with definitive steps.
During compensated shock, the body’s main concern is the preservation of a blood pressure, specifically the mean arterial pressure (MAP). To maintain brain, kidney, and coronary artery perfusion, the MAP must be >60 mmHg. The MAP can be calculated based on the following equation, where DBP is the diastolic blood pressure and SBP is the systolic blood pressure.

Using this equation, the MAP for a person whose blood pressure is 106/70 can be calculated: 70 + 1/3(106 – 70) = 82.
Consider a person who is losing blood over a period of time. As the person first starts to lose blood, the blood vessels begin to constrict, shrinking the container around the diminishing volume of circulating fluid. Baroreceptors, specialized areas within blood vessels extremely sensitive to otherwise imperceptible changes in blood pressure, signal this drop to the brain, and the autonomic nervous system responds by constricting blood vessels. The heart rate also accelerates during this phase and is 1 of the earliest findings in any shock. Remember the relationship of heart rate and blood pressure; as the heart rate increases, so does cardiac output and, therefore, blood pressure. Sweating and pale skin become apparent as the bleeding continues.
In decompensated shock, the patient’s bleeding continues. The volume of loss has begun to outstrip the body’s ability to recover on its own. The heart rate has increased to the point where it cannot go any higher, approaching 140–150 beats per minute in the adult. The capillary sphincters to all nonessential areas are closed, and the patient’s skin is now systemically mottled or pale and ashen. Capillaries are now beginning to shut down blood flow to essential areas, including the entire digestive tract and kidneys in a last ditch effort to maintain the person’s blood pressure and MAP to the heart, lungs, and brain. The hallmark of this stage is a measurably low blood pressure because the body’s self-protection mechanism has been overwhelmed. External support for the patient is now necessary and should include aggressive fluid replacement before the patient progresses into the final stage of shock.
Irreversible shock is the point at which end organ failure and cellular death have begun and will, ultimately, be unrecoverable. Kidney failure and death have begun; even if the shock is adequately treated at this stage, death is frequently unavoidable. Extended periods of hypotension lead to this stage.
This section addresses global assessment and treatment of the person in shock. More specific treatments will be addressed in later chapters. Be on the lookout for “Practical Points,” which are designed to help you link cognitive knowledge from this book with practical knowledge essential for the psychomotor exam portion of the NRPE.
Sizing up the scene begins with any dispatch information you are given and any additional information you are provided during the response. This part of the assessment gives you an opportunity to anticipate and request additional resources, such as police, fire, or additional ambulances. When arriving on the scene, evaluate your safety as you walk up to and enter the patient’s location. While you are looking for clues to your patient’s condition, be aware of any potential weapons in the vicinity of the patient. Now that you have encountered your patient, will you and your partner alone be able to carry the patient? This is another opportunity to request additional support. Finally, consider any obstructions for accessing the patient or egressing from the scene; the way you came in may not be how you exit. Hazards here could be as insidious as a welcome mat becoming a tripping hazard or as obvious as loose stair treads.
The first step is to form a general impression of your patient. This is a simple thought that will frame your thinking about the severity of the patient’s condition. It might sound like the following: “A 58-year-old female is seated on her couch in no apparent distress” or “This is a 28-year-old male lying unresponsive on a bed with vomit on the pillow and agonal respirations.”
More than just the first 5 letters of the alphabet, ABCDE guides you to what will kill your patient first: Airway, Breathing, Circulation and Consider C-Spine, Disability, and Expose.
After the life threats are addressed, you will need to assess SAMPLE and OPQRST as you would for any patient. More information on this can be found in the psychomotor portion of this book.
With shock, the same treatment can generally be used regardless of the cause or source. Needless to say, maintaining a patent's airway, maintaining an adequate breathing rate and quality, and treating cardiac arrest take priority over all sequential treatment, especially for patients in shock. For a patient in shock, you may need to initiate an advanced airway if the patient is unable to maintain it on his or her own. At the very least, administer O2 via a non-rebreathing mask or BVM if breathing quality is inadequate.
As already seen, circulation in shock can be highly compromised, for a variety of reasons. It should go without saying that if a patient is pulseless, high-quality cardiopulmonary respiration (CPR) should be initiated early and continued until a measurable return of spontaneous circulation occurs, and treatment should be continued along cardiac arrest algorithms (see chapter 4). Because shock often is a lengthy progression, you will likely encounter patients who still have a pulse, though often weak and “thready,” so maintaining and improving pulse quality and rate should be the primary goal once you are confident you have secured an airway. Starting a large-bore (≥18 gauge) intravenous line with a liter of a crystalloid solution is a great first step. Even if the patient is not currently hypotensive, the progression of shock will eventually lead to hypotension, so it is better to be ahead of the curve. The crystalloid solution could be normal saline or Ringer lactate and should be administered as a bolus of 20 mL/kg in approximately 500 mL increments. Fluid resuscitation should be titrated to the patient’s needs; however, aim for the following perfusion goals:
These 2 goals should be achieved without pulmonary edema or jugular vein distension.
In addition to O2 and intravenous fluid therapy, proper patient positioning and core body temperature maintenance are essential steps to be taken for any shock patient. In many cases, the Trendelenburg position, lying supine with the feet raised, is the recommended position for shock. This will help blood stay in the core circulation instead of in the legs. This position is not recommended for patients in shock who have suffered a traumatic head injury, a stroke, chest injuries, or abdominal injuries or who are found to have pulmonary edema (rales or crackles for lung sounds) during the initial examination; such positioning will exacerbate any of these problems for this subset of patients.
Keeping the patient warm during transport will help the body put energy into addressing the problem rather than shivering to generate heat. Layer on a few blankets and keep the back of the ambulance hotter than you may otherwise prefer. In addition, administer warm fluids whenever possible so the body does not have to work to raise the temperature of that fluid. Avoid localized heat sources such as heat packs and pads because they have the potential to cause more vasodilation and actually worsen hypotension.