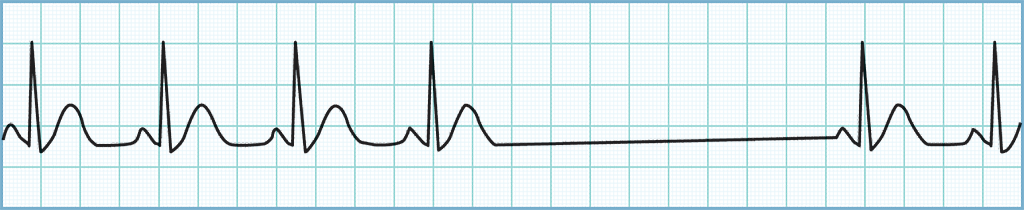
| Origination Point: SA Node | Differential Causes | |
|---|---|---|
| P Wave |
|
|
| Shape | Upright | |
| P rate | <60 | |
| P wave for every QRS? | Yes | |
| QRS complex for every P wave? | Yes | |
| PRI | ||
| Duration | <0.20 second | |
| QRS Complex | ||
| Shape | Normal | |
| Duration | 0.08–0.12 second | |
| R-R Interval | ||
| Regularity | Regular | |
| Rate | <60 | |

|
||
|
Treatment Options. The treatment for sinus bradycardia is largely dependent on the hemodynamic stability of the patient and the root cause for the bradycardia. If the patient is stable and has not displayed any change in mentation while in this rhythm, aggressive treatment likely is not indicated.
|
||