
Neurological emergencies include any problem that involves the brain, the spinal cord, or peripheral nerves—including all supporting circulation. This section will discuss such life-threatening problems as stroke and seizures, plus other issues of the central and peripheral nervous system.
The nervous system can be divided into the central nervous system (CNS) and the peripheral nervous system (PNS). The CNS consists of the brain and the spinal cord, whereas the PNS includes all the nerve branches emanating off the spinal cord and those arising directly from the brain itself, which are called cranial nerves. The PNS connects the CNS with the rest of the body through its vast network of nerves, and those nerves can be either somatic or autonomic. Somatic nerves include all the sensory nerves, also called afferent neurons, leading from the body to the brain, and all the motor nerves, also called efferent neurons, which carry signals from the brain to the muscles and glands of the body. The autonomic nervous system regulates the automatic, or involuntary, activities of the body, including heart rate, breathing, digestion, and pupil size, among many others. Finally, the autonomic nervous system can be further divided into the sympathetic and parasympathetic nervous systems.

The brain is covered with tough and comparatively thick connective tissue called meninges. The 3 layers from the inside (closest to the brain) to the outside (closest to the skull) are the pia mater, the arachnoid mater, and the dura mater. Together, they help protect the brain, anchor it within the skull, and contain within the layers CSF, which further cushions the brain when it moves inside the skull.
The biggest part of the brain is called the cerebrum or cerebral cortex. The surface of the cerebral cortex has many folds and bulges, called sulci (sulcus, singular) and gyri (gyrus, singular), which increase the surface area. It is divided into right and left hemispheres, or halves, and each half receives sensory information from and sends motor direction to the opposite side of the body.
The outer surface of the brain is called the cerebral cortex. The cortex is sometimes called the neocortex, a reminder that the cortex is the most recent brain region to evolve.
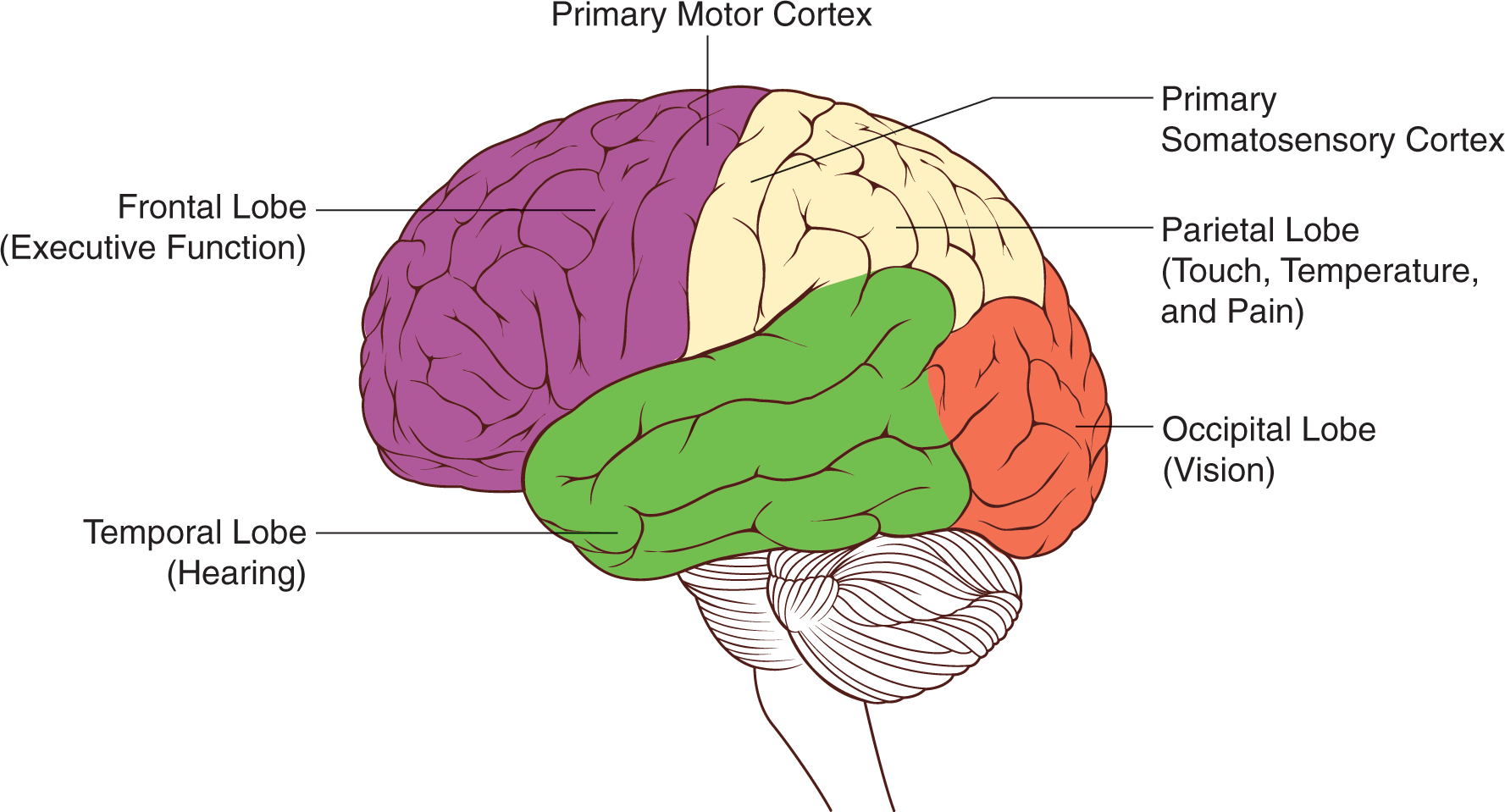
The cerebrum is divided into 2 halves, called cerebral hemispheres. The surface of the cortex is divided into 4 lobes: frontal lobe, parietal lobe, occipital lobe, and temporal lobe. These lobes are identified above as a side view of the left cerebral hemisphere.
The frontal lobe is composed of 2 basic regions: the prefrontal cortex and the motor cortex. The prefrontal cortex manages executive function by supervising and directing the operations of other brain regions. This region supervises processes associated with perception, memory, emotion, impulse control, and long-term planning. In memory, for instance, the role of the prefrontal cortex is not to store any memory traces; rather, it reminds the individual that he or she has something to remember at all. To regulate attention and alertness, the prefrontal cortex communicates with the reticular formation in the brainstem, telling an individual either to wake up or relax, depending on the situation.
Because it integrates information from different cortical regions, the prefrontal cortex is a good example of an association area: an area that integrates input from diverse brain regions. For example, multiple inputs may be necessary to solve a complex puzzle, plan ahead for the future, or reach a difficult decision. Association areas are generally contrasted with projection areas, which perform more rudimentary or simple perceptual and motor tasks. Examples of projection areas include the visual cortex, which receives visual input from the retina, and the motor cortex, which sends out motor commands to the muscles.
Damage to the prefrontal cortex impairs its overall supervisory functions. A person with a prefrontal lesion may be more impulsive, generally less in control of his or her behavior, or depressed. It is not unusual, for instance, for someone with a prefrontal lesion to make vulgar and inappropriate sexual remarks or to be apathetic.
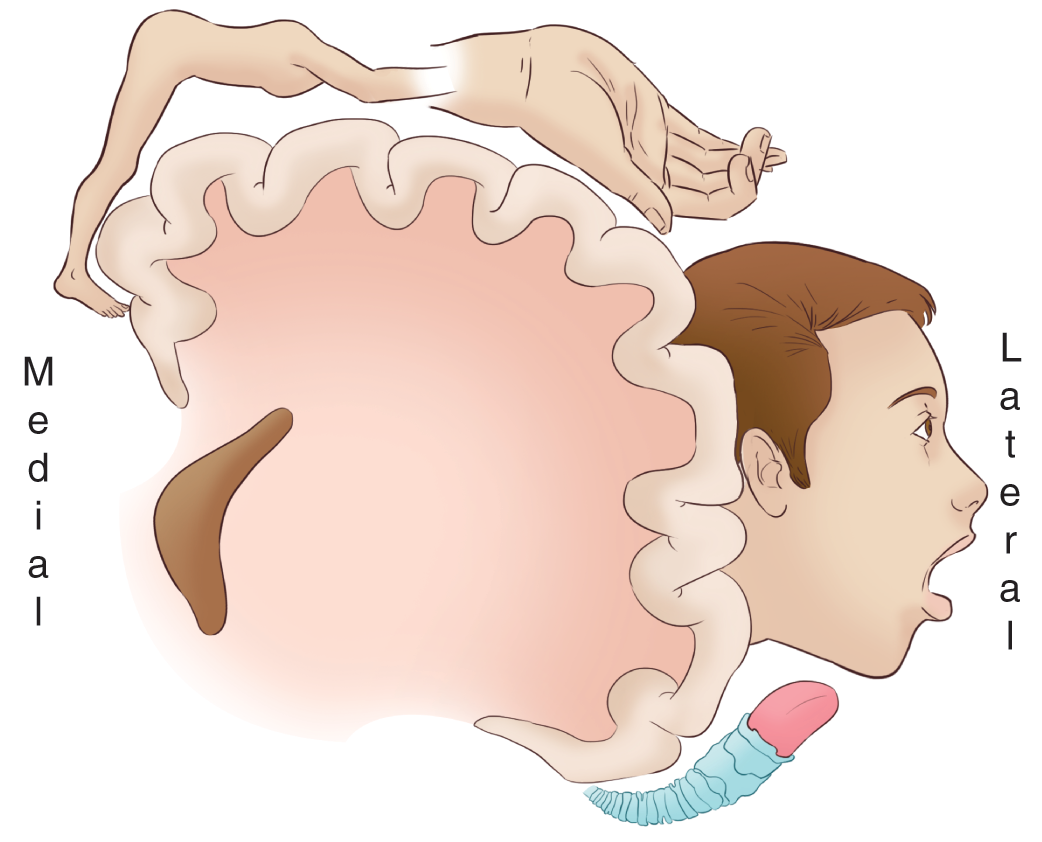
The primary motor cortex is located on the precentral gyrus (just in front of the central sulcus that divides the frontal and parietal lobes) and initiates voluntary motor movements by sending neural impulses down the spinal cord toward the muscles. As such, it is considered a projection area in the brain. The neurons in the motor cortex are arranged systematically according to the parts of the body to which they are connected. This organizational pattern can be visualized through the motor homunculus. Because certain sets of muscles require finer motor control than others, they take up additional space in the cortex relative to their size in the body.
A third important part of the frontal lobe is the Broca area, which is vitally important for speech production. The Broca area is usually found in only 1 hemisphere, the so-called dominant hemisphere. For most people—both right- and left-handed—the dominant hemisphere is the left hemisphere.
The parietal lobe is located to the rear of the frontal lobe. The somatosensory cortex is located on the postcentral gyrus (just behind the central sulcus) and is involved in somatosensory information processing. This projection area is the destination for all incoming sensory signals for touch, pressure, temperature, and pain. Despite certain differences, the somatosensory cortex and the motor cortex are very closely related. In fact, they are so interrelated they sometimes are described as a single unit: the sensorimotor cortex. The somatosensory homunculus is shown here.

The central region of the parietal lobe is associated with spatial processing and manipulation. This region makes it possible to orient oneself and other objects in 3-dimensional space, perform spatial manipulation of objects, and apply spatial orientation skills, such as those required for map reading.
The occipital lobes, at the very rear of the brain, contain the visual cortex, which is sometimes called the striate cortex. Striate means furrowed or striped, which is how the visual cortex appears when examined under a microscope. The visual cortex is one of the best-understood brain regions, owing to the large amount of research that has been done on visual processing. Areas in the occipital lobe also have been implicated in learning and motor control.
The temporal lobes are associated with a number of functions. The auditory cortex and Wernicke’s area are located in the temporal lobe. The auditory cortex is the primary site of most sound processing, including speech, music, and other sound information. The Wernicke area is associated with language reception and comprehension. The temporal lobe also functions in memory processing, emotion, and language. Studies have shown that electrical stimulation of the temporal lobes can evoke memories for past events. This makes sense because the hippocampus is located deep inside the temporal lobe. It is important to note that the lobes, although having seemingly independent functions, are not truly independent of one another. Often, a sensory modality may be represented in >1 area.
In most cases, each side of the brain communicates with the opposite side of the body. In such cases, the cerebral hemisphere communicates contralaterally. For example, the motor neurons on the left side of the brain activate movements on the right side of the body. In other cases (for instance, hearing), the cerebral hemispheres communicate with the same side of the body. In such cases, the hemispheres communicate ipsilaterally.
The dominant and nondominant hemispheres can be distinguished. The dominant hemisphere is typically defined as the one more heavily stimulated during language reception and production. In the past, hand dominance was used as a proxy for hemispheric dominance; that is, right-handed individuals were assumed to have left-dominant brains, and left-handed individuals were assumed to have right-dominant brains (because the brain communicates contralaterally with the hand). However, this correlation has not held up under scrutiny; 95% of right-handed individuals are indeed left-brain dominant, but only 18% of left-handed individuals are right-brain dominant.
The dominant hemisphere (usually the left) is primarily analytic in function, making it well suited for managing details. For instance, language, logic, and math skills are all located in the dominant hemisphere. Again, language production (the Broca area) and language comprehension (the Wernicke area) are primarily driven by the dominant hemisphere.
The nondominant hemisphere (usually the right) is associated with intuition, creativity, music cognition, and spatial processing. The nondominant hemisphere simultaneously processes the pieces of a stimulus and assembles them into a holistic image. The nondominant hemisphere serves a less prominent role in language. It is more sensitive to the emotional tone of spoken language and permits us to recognize others’ moods based on visual and auditory cues, which adds to communication. The dominant hemisphere screens incoming language to analyze its content, and the nondominant hemisphere interprets it according to its emotional tone. The roles of the dominant and nondominant hemispheres are summarized only; remember that the left hemisphere is the dominant hemisphere in most individuals, regardless of handedness.
The diencephalon is a region near the center of the cerebral cortex composed of several distinct structures: the thalamus, the hypothalamus, the posterior pituitary gland, and the pineal gland. The basal ganglia and the limbic system are closely related to the diencephalon, so those structures will be discussed here as well.

The thalamus serves as a relay station for all sensory information entering the brain from everywhere in the body, with the exception of the sense of smell. The thalamus sorts the information and relays it to the proper area of the cerebral cortex for interpretation and response.
The hypothalamus is located just inferior to the thalamus (hence its name) and is involved in maintaining homeostasis, hunger, and emotional responses. Because the hypothalamus regulates metabolism, body temperature, and water balance, it is the primary player in causing hunger, and it causes thirst through a process related to its release of antidiuretic hormone (ADH). ADH is released when receptors in the hypothalamus sense that the salt level in the blood is too concentrated, stimulating thirst and the kidneys to reabsorb more water. Finally, the hypothalamus plays a role in aggressive and sexual behaviors.
The posterior pituitary gland is the place where hypothalamic hormones enter the bloodstream, beginning the journey to their target organs. Oxytocin, also released by the hypothalamus, enters circulation via the posterior pituitary gland. The pineal gland, a small gland located posterior to the thalamus, is responsible for the body’s circadian rhythms and releasing melatonin. Melatonin is produced in greater quantities in the dark and is believed to help us go to sleep.
Lateral to each lobe of the thalamus in each hemisphere of the brain are the basal ganglia. These structures are involved in coordinating movement so that posture is maintained and other coordinated movements are smooth and fluid. Damage or destruction to the basal ganglia results in Parkinson disease (PD).
The limbic system is a group of structures closely related to the diencephalon that are primarily associated with memory. The primary components include the septal nuclei, the amygdala, and the hippocampus.
The septal nuclei contain the pleasure centers of the brain. Stimulation of the septal nuclei is intensely pleasurable, and it is believed that these nuclei are responsible for addictive behaviors.
The hippocampus plays a vital role in memory formation and learning. It converts information into long-term memories and redistributes them to portions of the cerebral cortex associated with memory. The hippocampus is connected directly to the septal nuclei through a projection called the fornix. This connection between the memory formation processing center and the pleasure and emotional centers of the brain—the septal nuclei and anterior portion of the hypothalamus—explains why long-term memories of particularly emotional events, both positive and negative, are some of the most enduring of long-term memories. Damage to the hippocampus can cause the inability to form new long-term memories and is called anterograde amnesia. Previously formed memories usually remain intact. The opposite of anterograde amnesia is retrograde amnesia, in which memories prior to a brain injury are lost.
The amygdala is the fear and anger center of the brain, which is responsible for defensive and aggressive behaviors. Damage to or lesions within the amygdala result in a particularly docile and likely hypersexual person.
The cerebellum is the area of the brain found at the base of the posterior portion of the brain and appears different from any the other structure in the brain. The cerebellum is responsible for coordinated and smooth movements and for posture and balance. The cerebellum is closely related to the vestibulocochlear nerve, also known as cranial nerve VIII, which is responsible for hearing and balance. Damage to this area affects fine motor movements and causes slurred speech and overall poor balance. Alcohol impairs the cerebellum function.
The brainstem contains 3 distinct parts: the midbrain, the pons, and the medulla oblongata (referred to simply as the medulla). It is the most inferior part of the brain and is contiguous with the spinal column. Of the 12 cranial nerves, 10 arise directly from the brainstem. The brainstem then serves as a relay center to the appropriate areas of the cerebrum, or it handles autonomic functions directly. The midbrain is associated with involuntary reflexes and visual and auditory stimuli triggers. The pons lies between the midbrain and the medulla and contains nerve tracts that connect the midbrain to the medulla, the cerebellum, and the cerebrum. It contains centers that are associated with autonomic functions, including blinking, bladder control, changing from inhalation to exhalation, swallowing, and balance. The medulla regulates vital signs, including respiratory rate and depth, heart rate, and blood pressure. Damage to the medulla will eliminate these functions.

The PNS includes all the neurons outside the brain and spinal cord. These are further broken down into either the cranial nerves or spinal nerves, based on where they originate. Cranial nerves originate from the cerebrum, the diencephalon, the midbrain, the pons, or the medulla and reach their target organs without traveling down the spinal column. Spinal nerves, on the other hand, branch off the spinal cord and emerge from the space between the vertebrae.
The 12 pairs of cranial nerves each have very specific functions. Some nerves have multiple functions, such as the vagus nerve that provides the parasympathetic innervation to all the visceral organs and motor control over most muscles in the pharynx; others have fewer functions, such as the trochlear nerve that controls exactly 1 muscle responsible for moving the eyeball toward the nose and down. Each of the 12 pairs of cranial nerves, an explanation of the functions, and methods to assess each are described in the table.
| Nerve | Sensory or Motor | Function | Assessment |
|---|---|---|---|
| I. Olfactory | Sensory | Sense of smell | Not usually assessed. |
| II. Optic | Sensory | Sense of vision | Identify something. |
| III. Oculomotor | Motor |
|
Have the patient follow your finger in the shape of a box with his or her eyes. Have the patient blink. |
| IV. Trochlear | Motor | Superior oblique—causes the eye to look down and in | Have the patient follow your finger in the shape of a box with his or her eyes. |
| V. Trigeminal | Both | Sensation to the face, forehead, eyelids, nose, nasal linings, cheeks, lips, gums, and teeth Movement of muscles of mastication (chewing) Spicy sensation in mouth |
Touch the forehead, cheeks, and mandible gently with a sharp object to test all 3 branches of the nerve. |
| VI. Abducens | Motor | Lateral rectus of the eye—causes the eye to look laterally (away from the nose) | Have the patient follow your finger in the shape of a box with his or her eyes. |
| VII. Facial | Both | Controls facial expression Responsible for taste of the anterior 2/3 on the tongue Salivation from the submandibular salivary glands Lacrimation |
Have the patient smile. |
| VIII. Vestibulocochlear (Auditory) | Sensory | Hearing from the cochlea and balance from the vestibular apparatus | Have the patient follow spoken word commands. |
| XI. Glossopharyngeal | Both | Sensation to the tongue, tonsils, pharynx, middle ear, and carotid body Taste from the posterior 1/3 of the tongue Salivation from the parotid gland Motor fibers to muscles of swallowing |
Have the patient swallow. |
| X. Vagus | Both | Parasympathetic stimulation to all visceral organs, except the adrenal glands, and from the
3rd segment of the transverse colon through the rectum Muscles related to swallowing and the palatoglossus muscle of the tongue |
Have the patient swallow. |
| XI. Accessory | Motor |
|
Have the patient shrug his or her shoulders while pushing down on them to test symmetry. |
| XII. Hypoglossal | Motor | All muscles of the tongue except the palatoglossus (vagus). | Have the patient stick out his or her tongue. |
The 31 pairs of spinal nerves emerge from each side of the spinal column. The dorsal or posterior root is the afferent nerve bundle that carries sensory information from the body to the brain. Each set of afferent nerves services a specific area of the body, referred to as a dermatome. The ventral or anterior root carries the efferent or motor nerve fibers. Each set of efferent nerves supplies a specific set of muscles, known as the myotome.
| Level | Motor Function |
|---|---|
| C1–C6 | Neck flexors |
| C1–T1 | Neck extensors |
| C3, C4, C5 | Supply diaphragm (mostly C4) |
| C5, C6 | Move shoulder, raise arm (deltoid), and flex elbow (biceps) |
| C6 | Externally rotate (supinate) the arm |
| C6, C7 | Extend elbow and wrist (triceps and wrist extensors) and pronate wrist |
| C7, C8 | Flex wrist and supply small muscles of the hand |
| T1–T6 | Intercostals and trunk above the waist |
| T7–L1 | Abdominal muscles |
| L1–L4 | Flex thigh |
| L2, L3, L4 | Extend leg at the knee and adduct thigh |
| L4, L5, S1 | Abduct thigh, flex leg at the knee, dorsiflex foot (off gas pedal), and extend toes |
| L5, S1, S2 | Extend leg at the hip, plantar flex foot (point foot), and flex toes |

Neurons are specialized cells capable of transmitting electrical impulses and then translating those electrical impulses to chemical signals. This section considers the structure of the neuron as well as how neurons communicate with other parts of the nervous system.
Each neuron has a shape that matches its function, as dictated by the other cells with which that neuron interacts. A variety of different types of neurons are in the body, but they all share some specific features.
Like all other cells (besides mature red blood cells), neurons have nuclei. The nucleus is located in the cell body, also called the soma. The soma is also the location of the endoplasmic reticulum and ribosomes. The cell has many appendages emanating directly from the soma, called dendrites, that receive incoming messages from other cells. The information received from the dendrites is transmitted through the cell body before it reaches the axon hillock, which integrates the incoming signals. The axon hillock plays an important role in action potentials, or the transmission of electrical impulses down the axon. Signals arriving from the dendrites can be either excitatory or inhibitory; the axon hillock sums these signals; if the result is excitatory enough (reaching threshold, as discussed later in this chapter), it will initiate an action potential.
The axon is a long appendage that terminates in close proximity to a target structure (a muscle, a gland, or another neuron). Most mammalian nerve fibers are insulated by myelin to prevent signal loss or the crossing of signals. Just like insulation prevents wires next to each other from accidentally discharging each other, the myelin sheath maintains the electric signal within a single neuron. In addition, myelin increases the speed of conduction in the axon. Myelin is produced by oligodendrocytes in the CNS and Schwann cells in the PNS.
At certain intervals along the axon, small breaks in the myelin sheath with exposed areas of axon membrane are called the nodes of Ranvier. As will be explored in the discussion of action potentials to follow, the nodes of Ranvier are critical for rapid signal conduction. Finally, at the end of the axon is the nerve terminal or synaptic bouton (knob). This structure is enlarged and flattened to maximize neurotransmission to the next neuron and ensure the proper release of neurotransmitters, the chemicals that transmit information between neurons.
Neurons are not physically connected to each other. Between the neurons, there is a small space into which the terminal portion of the axon releases neurotransmitters, which bind to the dendrites of the postsynaptic neuron. This space is known as the synaptic cleft; together, the nerve terminal, the synaptic cleft, and the postsynaptic membrane are known as a synapse. Neurotransmitters released from the axon terminal traverse the synaptic cleft and bind to receptors on the postsynaptic neuron.
Multiple neurons may be bundled together to form a nerve in the PNS. These nerves may be sensory, motor, or mixed, which refers to the type(s) of information they carry; mixed nerves carry both sensory and motor information. The cell bodies of neurons of the same type are clustered together into ganglia.
In the CNS, axons may be bundled together to form tracts. Unlike nerves, tracts carry only one type of information. The cell bodies of neurons in the same tract are grouped into nuclei.

After discussing the basic anatomy of the neuron, the focus turns to the physiology that underlies neuronal signaling. Neurons use all-or-nothing messages, called action potentials, to relay electrical impulses down the axon to the synaptic bouton. As will be explored in the following section, action potentials ultimately cause the release of neurotransmitters into the synaptic cleft.
All neurons exhibit a resting membrane potential. This means that there is an electrical potential difference (voltage) between the inside of the neuron and the extracellular space. Usually, this is about –70 mV, with the inside of the neuron being negative relative to the outside. Neurons use selective permeability to ions and the Na+/K+ ATPase to maintain this negative internal environment.

Like any other cell, the neuronal plasma membrane is fairly impermeable to charged species. Because the plasma membrane contains a thick nonpolar barrier (fatty acid tails), it is not energetically favorable for ions to cross this barrier. Inside the neuron, K+ is high and Na+ is low. Outside of the neuron, Na+ is high, whereas K+ is low. The negative resting potential is generated by both negatively charged proteins within the cell and the relatively greater permeability of the membrane to K+ compared with Na+. If the cell membrane is more permeable to K+ and the ion’s concentration is higher inside, K+ will diffuse down its gradient out of the cell. What does this mean in terms of charge movement? K+ is positively charged, so its movement out of the cell results in a cell interior that is negative. Put another way, if the membrane starts at 0, and a positive charge is removed, the end result is a negative charge inside the cell: 0 – (+1) = –1. Na+ cannot readily enter at rest, so the negative potential is maintained.
The Na+/K+ ATPase is important for restoring this gradient after action potentials have been fired. It transports 3 Na+ out of the cell for every 2 K+ into the cell at the expense of 2 ATP (adenosine triphosphate). ATP is necessary because both Na+ and K+ are moved against their gradients by this process; thus, this qualifies as primary active transport. Each time the pump works, it results in the cell becoming relatively more negative: only 2 positive charges are moved in for every 3 that are moved out.
Neurons can receive both excitatory and inhibitory input. Excitatory input causes depolarization (raising the membrane potential, Vm, from its resting potential) and thus makes the neuron more likely to fire an action potential. Inhibitory input causes hyperpolarization (lowering the membrane potential from its resting potential) and thus makes the neuron less likely to fire an action potential. If the axon hillock receives enough excitatory input to be depolarized to the threshold value (usually in the range of –55 to –40 mV), an action potential will be triggered.
This implies that not every stimulus necessarily generates a response. A small excitatory signal may not be sufficient to bring the axon hillock to threshold. Further, a postsynaptic neuron may receive information from several different presynaptic neurons, some of which are excitatory and some of which are inhibitory. The additive effect of multiple signals is known as summation.
The 2 types of summation are temporal and spatial. In temporal summation, multiple signals are integrated during a relatively short period of time. A number of small excitatory signals firing at nearly the same moment could bring a postsynaptic cell to threshold, enabling an action potential. In spatial summation, the additive effects are based on the number and location of the incoming signals. A large number of inhibitory signals firing directly on the soma will cause more profound hyperpolarization of the axon hillock than the depolarization caused by a few excitatory signals firing on the dendrites of a neuron.
A graph of membrane potential versus time during an action potential follows.

If the cell is brought to threshold, voltage-gated sodium channels open in the membrane. As the name implies, these ion channels open in response to the change in potential of the membrane (depolarization) and permit the passage of Na+ ions. A strong electrochemical gradient promotes the migration of sodium into the cell. From an electric standpoint, the interior of the cell is more negative than the exterior of the cell, which favors the movement of positively charged Na+ ions into the cell. From a chemical standpoint, the concentration of sodium outside the cell is higher than on the inside, which also favors the movement of sodium into the cell. As sodium passes through these ion channels, the membrane potential becomes more positive; that is, the cell rapidly depolarizes. Sodium channels not only open in response to changes in membrane potential but are also inactivated by them. When Vm approaches 35 mV, the sodium channels are inactivated and will have to be brought back near the resting potential to be deinactivated. Thus, these sodium channels can exist in 3 states: closed (before the cell reaches threshold and after inactivation has been reversed), open (from threshold to approximately 35 mV), and inactive (from approximately 35 mV to the resting potential).
The positive potential inside the cell triggers not only the voltage-gated sodium channels to inactivate but also the voltage-gated potassium channels to open. Once sodium has depolarized the cell, there is an electrochemical gradient favoring the efflux of potassium from the neuron. As positively charged potassium ions are driven out of the cell, there will be a restoration of the negative membrane potential called repolarization. The efflux of K+ causes an overshoot of the resting membrane potential, hyperpolarizing the neuron. This hyperpolarization serves an important function: it makes the neuron refractory to further action potentials. There are 2 types of refractory periods. During the absolute refractory period, no amount of stimulation can cause another action potential to occur. During the relative refractory period, there must be greater than normal stimulation to cause an action potential because the membrane is starting from a potential that is more negative than its resting value.
The Na+/K+ ATPase acts to restore not only the resting potential but also the sodium and potassium gradients that have been partially dissipated by the action potential.
So far, the movements of ions at 1 small segment of the axon have been discussed. For a signal to be conveyed to another neuron, the action potential must travel down the axon and initiate neurotransmitter release. This movement is called impulse propagation. As sodium rushes into 1 segment of the axon, it will cause depolarization in the surrounding regions of the axon. This depolarization will bring subsequent segments of the axon to threshold, opening the sodium channels in those segments. Each of these segments then continues through the rest of the action potential in a wavelike fashion until the action potential reaches the nerve terminal. After the action potential has fired in 1 segment of axon, that segment becomes momentarily refractory, as described previously. The functional consequence of this is that information can only flow in 1 direction.

The speed at which action potentials move depends on the length and cross-sectional area of the axon. Increased length of the axon results in higher resistance and slower conduction. Greater cross-sectional areas allow for faster propagation because of decreased resistance. The effect of cross-sectional area is more significant than the effect of length. To maximize the speed of transmission, mammals have myelin. Myelin is an extraordinarily good insulator that prevents the dissipation of the electric signal. The insulation is so effective that the membrane is permeable only to ion movement at the nodes of Ranvier. Thus, the signal “hops” from node to node—what is called saltatory conduction.
It is important to note that all action potentials within the same type of neuron have the same potential difference during depolarization. Increased intensity of a stimulus does not result in an increased potential difference of the action potential but rather an increased frequency of firing.
As discussed previously, neurons are not actually in direct physical contact. There is a small space between neurons called the synaptic cleft into which neurotransmitters are secreted. To clarify the terminology, the neuron preceding the synaptic cleft is called the presynaptic neuron; the neuron after the synaptic cleft is called the postsynaptic neuron. If a neuron signals to a gland or muscle, rather than another neuron, the postsynaptic cell is termed an effector. Most synapses are chemical in nature; they use small molecules referred to as neurotransmitters to send messages from cell to cell.
Prior to release, neurotransmitter molecules are stored in membrane-bound vesicles in the nerve terminal. When the action potential reaches the nerve terminal, voltage-gated calcium channels open, allowing calcium to flow into the cell. This sudden increase in intracellular calcium triggers fusion of the membrane-bound vesicles with the cell membrane at the synapse, causing exocytosis of the neurotransmitter.
Once released into the synapse, the neurotransmitter molecules diffuse across the cleft and bind to receptors on the postsynaptic membrane. This allows the message to be passed from one neuron to the next. As stated earlier, neurons may be either excitatory or inhibitory; this distinction truly comes at the level of the neurotransmitter receptors, which tend to be either ligand-gated ion channels or G protein-coupled receptors. If the receptor is a ligand-gated ion channel, the postsynaptic cell will either be depolarized or hyperpolarized. If it is a G protein-coupled receptor, it will cause either changes in the levels of cyclic AMP (cAMP; cyclic adenosine monophoshate) or an influx of calcium.
Neurotransmission must be regulated; there are almost no circumstances under which constant signaling to the postsynaptic cell would be desirable. Therefore, the neurotransmitter must be removed from the synaptic cleft. Three main mechanisms accomplish this goal. First, neurotransmitters can be broken down by enzymatic reactions. The breakdown of acetylcholine (ACh) by acetylcholinesterase (AChE) is a classic example.
Second, neurotransmitters can be brought back into the presynaptic neuron using reuptake carriers. The reuptake of serotonin is a classic example of this mechanism. Dopamine and norepinephrine also use reuptake carriers.
Third, neurotransmitters may simply diffuse out of the synaptic cleft. Nitric oxide, a gaseous signaling molecule, fits into this category.
As with any call, always begin by assuring that you arrive safely and have a safe scene for you and your partner to work. Once a secure scene has been reasonably established, form a general impression of the patient. This will help you determine early on the urgency of the situation: Is the patient seriously ill and requires rapid transportation or can some interventions be performed on scene before moving to the ambulance? Rapidly assess the ABCs and take appropriate steps to ensure a patent airway, adequate rate and depth of breathing, and adequate circulation.
When assessing the ABCs at this point, it is not essential to get numbers; merely ensuring that what they have will last to the ambulance, or until a time to fully evaluate respiratory and pulse rates, is sufficient.
Regardless of the chief complaint, every patient should be evaluated for his or her level of consciousness; however, this is especially true for neurological emergencies. Early and frequent assessment of the neurological status of any patient is essential to be able to track the progression of the issue. Several methods can be used to assess a patient’s level of consciousness: AVPU, the GCS, and degree of orientation.
AVPU is a mnemonic that will help you remember the tenets of the most basic level of consciousness:
The GCS is a comprehensive tool that assigns a numeric value to a person’s level of consciousness. During assessment of the patient, assign the patient a score in each of the categories and then add the numbers from each category. Generally, a person with a total score <8 (i.e., 7 or less for adults but <5 for children) is considered critical because the person is most likely unable to maintain a patent airway because he or she has lost his or her gag reflex; the patient should be aggressively managed and frequently reassessed.
| Category | Score | Adult (≤7) | Pediatric (<5) |
|---|---|---|---|
| Eye opening | 4 | Spontaneous | Spontaneous |
| 3 | Verbal stimulus | Verbal stimulus | |
| 2 | Painful stimulus | Painful stimulus | |
| 1 | Unresponsive | Unresponsive | |
| Best verbal response | 5 | Oriented | Smiles/coos/babbles |
| 4 | Confused | Consolable, inappropriate interactions | |
| 3 | Inappropriate words | Inconsolable, inappropriate cry | |
| 2 | Garbled | Grunting and ineffective whimpering | |
| 1 | None | None | |
| Best motor response | 6 | Obeys commands | Obeys commands |
| 5 | Localizes pain | Withdraws from touch | |
| 4 | Withdraws from pain | Withdraws from pain | |
| 3 | Decorticate posturing | Decorticate posturing | |
| 2 | Decerebrate posturing | Decerebrate posturing | |
| 1 | None | None |
As mentioned previously in this chapter, the A in AVPU means only that the patient has his or her eyes open spontaneously; essentially a 4 in the eye-opening category in the GCS. This should be coupled with the degree of orientation the patient can orally provide, which can be accomplished by determining the patient’s ability to know who he or she is, where he or she is, and describe correctly a reference of time. If the patient is correct on all 3 orientation questions, the patient is said to be alert and oriented times 3 (A&Ox3); if the patient misses 1 question, the patient is A&Ox2, and so on. Ask the patient the following 3 questions:
Frequently, with neurological problems, patients will lose orientation in reverse numerical order of the above. This is caused, at least in part, by the increasing transiency of each sequential question. Dates change all the time; sometimes even fully oriented people need a calendar to know the day of the week. Ever think it was Wednesday when it was really Tuesday? Location tends to be permanent longer unless the person is visiting somewhere such as a restaurant or a park, but if the person is at home, that is usually not overly new to the person. Finally, in most cases, the person has had his or her name, at least first name, throughout life, so that is the last degree of orientation to be lost.
Some providers and texts suggest a 4th question to ask a patient to determine his or her orientation: What happened? Having the patient successfully being able to provide details of the history of present illness or complaint can result in an assessment that the patient is A&Ox4.
It has been said that the eyes are the windows to the soul. Well, if true, then the pupils are the window to the functional status of the brain. Examine the pupils for reactivity to light, size, and shape.
As noted in the GCS, verbal responses and the quality of them is an important assessment finding in the patient with neurological deficits. First evaluate the quality of the speech according to the GCS. Is it slurred or garbled? Are the words appropriate? There are several situations in which a person can have clear speech but incorrect word choice. Agnosia is when a patient is unable to tell you the correct name for a common object because of a breakdown in communication between the visual cortex in the occipital lobe of the brain and the temporal lobe where general knowledge is stored. Apraxia is a situation where the patient may be able to name the object in question (occipital to temporal lobe communication is intact); however, the patient is completely incapable of demonstrating how to use it. In this case, nerve tracts between knowledge in the temporal lobe and the motor cortex in the frontal lobe have been damaged.
A patient may have receptive aphasia, which is a condition where the patient is unable to understand what is communicated to him or her either written or verbally. Receptive aphasia results from damage to the Wernicke area located in the left hemisphere of the brain, whether from a medical event or a traumatic event. Patients with receptive aphasia are often able to speak clearly; however, the words they use are frequently nonsensical, made up words. Sentence structure appears intact, but the sentences are completely devoid of any meaning or ability to be interpreted. They also often talk continuously, though with seemingly appropriate intonation and inflection. Frequently, these patients also are completely unaware that the speech they are saying is nonsensical because they cannot understand their own words either.
The opposite of this is expressive aphasia, which is where the patient is unable to form or select the words he or she needs to complete a thought or a sentence. The patient understands completely what is happening around him or her and is able to understand spoken and written communication. The patient’s speech is effortful but often visibly frustrating. The patient can follow commands because the speech interpretation area (Wernicke area) is intact; here, the Broca area is damaged or impaired, resulting in telegraphic speech—speech where only important words are spoken after some time of deliberate concentration on forming them. If you ask the patient to smile and he or she does, but the patient is unable to clearly succinctly state what he or she just did, the patient most likely has expressive aphasia.
Global aphasia is a complete disruption of verbal or written communication. The patient displays both expressive and receptive aphasia. He or she may blurt out incomprehensible words or syllables, but otherwise, any communication attempted cannot be interpreted. This patient is still able to think and interact with his or her environment through other senses; the patient just has no way of communicating this.
Stroke is a condition where blood flow to an area of the brain is compromised. A stroke can be either ischemic or hemorrhagic in nature. Ischemic strokes, sometimes referred to as occlusive strokes, result from a blockage to an artery that services a part of the brain or possibly the entire hemisphere. Ischemic strokes can be further differentiated into thrombic or embolic. In a thrombic stroke, the clot formed right there in that artery. In an embolic stroke, the clot formed elsewhere in the body and traveled to its current location. The most common locations for clots to form that eventually release the embolus resulting in a stroke are the heart or carotid arteries. In cases of AF, clots can form as a result of blood stasis in the atria if the AF is not found early enough or if the patient is not properly anticoagulated. A piece of this clot or the entire thing may break loose and travel into the brain. If the leaflets to the aortic valve are damaged for any reason, clots will form on the leaflets, which can then embolize into the brain. The carotid arteries may become damaged after years of high blood pressure and arterial or atherosclerotic plaque can build up inside the artery. This, too, can break apart and embolize up to the brain.
In a hemorrhagic stroke, an artery in the brain has weakened and ruptured, compromising the blood-brain barrier. This bleeding will continue, leading to increasingly worsening symptoms over time and increased ICP; eventually, the brainstem will herniate out of the skull and compress the medulla. Once the medulla becomes compressed, vital sign regulation will become erratic and fail, resulting in certain death for the patient. The progressive worsening of symptoms seen in a hemorrhagic stroke is in stark contrast to an ischemic stroke, where symptoms typically come on suddenly and remain, rather than worsen. Between bleeding into the brain tissue and the increasing pressure inside the cranial vault, the damage resulting from a hemorrhagic stroke often is irreversible and pervasive.
Depending on the location of the lesion—the occlusion or hemorrhage—stroke symptoms are widely varied and affect multiple functions. Patients will often state that they are having the worst headache of their life, and, frequently, this headache is focused on 1 side of the head. The patient also may exhibit weakness, a loss of sensation, or paralysis to the side of the body opposite the side on which the headache is located. If the lesion includes the visual cortex or the auditory cortex, visual or hearing disturbances also may be noted.
To help prehospital providers determine the severity of the stroke, various scales can be used to guide assessment of a patient who has had a stroke. The Cincinnati Prehospital Stroke Scale and the Los Angeles Prehospital Stroke Screen are good examples of such scales. If a finding is abnormal in the Cincinnati Prehospital Stroke Scale, it predicts a stroke 72% of the time. If the criteria numbered 1–6 in the Los Angeles Prehospital Stroke Screen are all “yes,” it predicts a stroke 97% of the time.
| Criteria | |||
|---|---|---|---|
| 1. Age >45 | Yes | No | Unknown |
| 2. History of seizures or epilepsy absent | Yes | No | Unknown |
| 3. Symptoms <24 hours | Yes | No | Unknown |
| 4. Patient was not wheelchair or bed bound prior. | Yes | No | Unknown |
| 5. Blood glucose level between 60 and 400 mg/dL | Yes | No | Unknown |
| 6. Notable asymmetry in any 1 of the 3 below: | Yes | No | Unknown |
| Test | Right | Left | Equal? |
| Have patient smile | Moves less | Moves less | Equal |
| Have patient squeeze your fingers as tightly as possible | Weaker/None | Weaker/None | Equal |
| With palms up and eyes closed, hold patient's arms out in front of them. Ask the patient to hold up his or her arms | Drifts/Falls | Drifts/Falls | Both held up equally |
| Assessment Point | Clinical Test | Normal | Abnormal |
|---|---|---|---|
| Facial droop | Smile and show teeth. | Smile is symmetrical. | Smile is asymmetrical. |
| Arm drift | With palms up and eyes closed, hold the patient’s arms out in front of the patient. Ask the patient to hold up his or her arms. | Arms remain in place. | One arm drifts down slowly or 1 arm falls down immediately. |
| Speech | Have the patient repeat any easy sentence. | Speech is clear and with correct words. | Speech is slurred, or the patient is completely unable to speak. |
Minimizing the long-term effects of a stroke, or cerebrovascular accident (CVA), is time dependent. Similar to saying, “Time is muscle” in a heart attack, the saying, “Time is brain” applies to a CVA. Rapid, thorough assessment, coupled with rapid transport to a facility capable of conducting a computerized tomography (CT) scan is critical. In the hospital, clots from an ischemic stroke can be physically removed in 1 of 2 ways: (1) using a surgical technique that goes into the vasculature, grabs the clot, and pulls it out of the body or (2) using “clot busting” medications called fibrinolytics. If time permits and the patient or his or her family is able to answer the necessary questions, assess the patient’s ability to receive fibrinolytics at the hospital. Fibrinolytics need to be administered within 3 hours of the onset of symptoms, so if the paramedic can have this checklist filled out after arriving at the hospital, precious time can be saved.
| Fibrinolytics Checklist | |||
|---|---|---|---|
| Yes | No | Unknown | Patient 18 years or older? |
| Yes | No | Unknown | Facial droop? |
| Yes | No | Unknown | Slurred speech? |
| Yes | No | Unknown | Arm drift? |
| Yes | No | Unknown | Was there a seizure? |
| Yes | No | Unknown | SBP >185? |
| Yes | No | Unknown | History of structural nervous system disease? (stroke, arteriovenous malformation (AVM), aneurysm) |
| Yes | No | Unknown | Head or facial trauma within 6 weeks? |
| Yes | No | Unknown | MI within 6 weeks? |
| Yes | No | Unknown | Blood clotting disorder or on anticoagulants? |
| Yes | No | Unknown | Ulcers? |
| Date/Time: | Time signs and symptoms began or time last known to be well | ||
| Value: | Blood glucose reading | ||
Seizures, regardless of type, are caused by an erratic misfiring of cerebral neurons. This excessive overstimulation of neurons can lead to several different presentations of seizures. The first and most common kind of seizure is the grand mal or tonic-clonic seizure. Next is the focal motor seizure, sometimes referred to as the partial seizure. Finally is the petit mal or absence seizure. A variety of reasons may lead a person to have a seizure, including the following:
The generalized seizure involves the entire brain and body and presents as forceful jerking movements of all the skeletal muscles. The seizure begins with the tonic phase, which is a brief tensing of all the muscles in the body. This precedes the clonic phase, which is the alternating forceful contraction of all the muscles with a relaxed phase of all the muscles. During this time, the patient is not breathing and is moving air in and out of the lungs only by virtue of the diaphragm and the intercostal muscles contracting along with the rest of the body. This is by no means effective. During the active part of the seizure, the patient also may be incontinent to both urine and feces. Many patients who have a history of seizures often are able to sense when they are about to have a seizure, called an aura, and prepare themselves by lying on the ground. Following a seizure, patients enter a postictal state, which is essentially a recovery time for the brain to reset and appears as if the patient is deeply asleep.
After the postictal phase, frequently within about 10–15 minutes, a patient will slowly regain consciousness and become fully oriented after a period of confusion. Occasionally, the patient begins to seize once again, without regaining consciousness after the previous seizure. Patients who have tonic-clonic seizures lasting >5 consecutive minutes or who do not regain consciousness after being postictal are said to be in status epilepticus. Status epilepticus is a legitimately life-threatening condition that needs to be aggressively managed.
Another form of generalized seizure that affects the entire brain is the absence seizure. This seizure does not involve tonic-clonic movements but rather a complete lack of movement. The patient afflicted with the absence seizure can stop all movement, including stopping mid-sentence, and pick up right where he or she left off without ever knowing anything happened. Often, these seizures last no more than a few seconds and are not regarded as life threatening unless they happen at a time where surrounding events can cause an injury, such as while the person is crossing a street.
Partial seizures differ from generalized seizures in that they involve only 1 part of the brain. A partial seizure may be classified as a simple partial seizure or a complex partial seizure. During a simple partial seizure, 1 area of the body will begin moving if the frontal lobe is involved, or 1 area will lose feeling if the parietal lobe is involved. This movement or loss of feeling will move in a wave-like fashion across and seemingly out of the body. For example, the patient’s right hand may start shaking; the shaking will move to the arm, then shoulder and then the head before finally going down the left arm and hand and finally leaving the body. During a complex partial seizure, the effects of the simple partial seizure are seen; however, it is accompanied by hallucinations or changes in the patient’s level of consciousness. The patient will not usually fully lose consciousness and may have a memory of the incident.
A paramedic may encounter several types of patients when called to aid a patient having a seizure: the patient may be fully alert, postictal, or still seizing. The assessment of each type of individual, however, is largely similar. Witnesses may be the greatest source of valuable information because the patient may or may not be responsive. Even if the patient is alert on when the paramedics arrive, the patient may have only a limited memory. It is important to try to first determine the type of seizure. Next, attempt to determine how long the patient was seizing and how long it has been since the patient’s last seizure. Also find out if the patient is compliant with his or her medication regimen or if he or she is known to have had seizures in the past. With the above list as a reference, try to determine what caused the seizure by ruling out other causes, particularly if seizures have not previously occurred or if none of the bystanders are familiar with the patient’s medical history.
Performing a thorough physical examination will help determine the cause in patients who are unable to talk or recall events leading up to the seizure. Although seizures may be preceded with an aura, the patient may still have suffered injuries if he or she was standing at the onset of the incident.
Treatment is not usually necessary for either absence seizures or partial seizures, beyond ensuring the patient’s safety during any seizure activity they may have in the presence of the paramedics. This discussion will therefore focus on the tonic-clonic seizure activity. If the patient is still seizing on arrival to the scene, do not restrain the patient. Allow the patient to continue the seizure without interference. Ensure that adequate space is around the patient so that he or she will not hit anything during these convulsions. Do not make any attempts to force anything into the patient’s mouth. Because the patient usually has his or her teeth clenched, this will do more harm than good. Because the patient is still seizing and attempting to start an intravenous could result in injury to the paramedic or the patient, consider administering intranasal midazolam, 0.2 mg/kg, up to 10 mg, to help the patient stop seizing. You also may consider giving 0.5 mg/kg diazepam rectally, up to 10 mg.
Once the seizure has stopped, work quickly to begin the necessary interventions in case this is merely an intermission of status epilepticus. Initiate cardiac monitoring and obtain a full set of vital signs. Remember that the patient was not effectively breathing during the seizure, so initiate high-flow O2 and consider providing BVM ventilation if necessary for long periods of apnea. Always check the blood sugar reading and administer 25 g D50 if it is <60 mg/dL. Initiate an intravenous line and provide a fluid bolus if the patient is hypotensive. If you suspect opiate drug overdose, administer 0.4–2 mg naloxone, titrated to adequate respirations. Pad around the patient if possible in case the patient begins seizing again. If the patient does seize during transport, loosen the seat belts and protect the patient from hurting himself or herself as much as possible. Be prepared to administer benzodiazepine again if seizures begin again. The intravenous options are as follows:
A common call the paramedic must be ready for is altered mental status. The mnemonic AEIOU-TIPS can help evaluate the possible reasons for a person to have an altered level of consciousness (LOC). Note that the reasons for altered mental status do not differ appreciably from those that cause seizures.
| Letter | Cause | Onset | Additional Signs and Symptoms | Treatment Options |
|---|---|---|---|---|
| A | Alcohol, acute | Hours | Slurred speech, unsteady gait | Time, fluids |
| Alcohol, chronic | Days | Slurred and garbled speech and abdominal pain | Fluids, thiamine, D50 | |
| Acidosis, metabolic | Days | Eating without taking insulin, high blood sugar, and Kussmaul respirations | Fluids; bicarbonate in extreme circumstances | |
| Acidosis, respiratory | Minutes | Decreased respiratory effort and no breathing | Restoring adequate ventilation | |
| E | Epilepsy | Seconds | Tonic-clonic activity | Diazepam or lorazepam |
| I | Insulin | Minutes | Unresponsiveness and low blood sugar | D50 or glucagon |
| O | Overdose | Minutes | Pupillary changes, needle track marks, and drug paraphernalia at scene | Naloxone for opiates; otherwise, drug dependent |
| U | Uremia (acute renal failure) | Days to weeks | Decreased urine output, failure to go to dialysis, and recent excessive exercise | Ensure adequate blood pressure, SpO2, and blood glucose level |
| T | Trauma | Seconds | Multiple systems involvement | Varies with injury; treat for shock |
| I | Infection | Days | Hot, dry skin, foul smelling urine, and a productive cough | Maintain SBP >100; treat for shock |
| P | Psychosis | Seconds | Possible drug overdose, agitated or hypoactive, and delirium | Ensure adequate blood pressure, SpO2, and blood glucose level |
| S | Stroke | Seconds | Unilateral weakness, facial droop, and slurred speech | Ensure adequate blood pressure, SpO2, and blood glucose level |
When evaluating the patient with altered mental status, focus on the time that the patient was last known to be at his or her baseline level of consciousness and how quickly the patient arrived at his or her current state. Assess the GCS level and document any changes to that level throughout transport; depending on the cause of the alteration, the patient may get better or worse as time goes on. The use of bystanders as part of the assessment technique here is essential because although the patient may be able to answer, there is no reliable way to know if what the patient is saying is accurate. Evaluate the patient for any trauma, especially of the head, but not necessarily only the head. Evaluate the patient on the basis of 1 of the previously mentioned stroke scales. Attempt to identify any overdose or poisoning agent.
There are some treatment options for each cause of an altered mental status; however, some global treatment options should be performed with any patient in this population. First, ensure adequate ABCs; secure the airway, ventilate with a BVM, and initiate CPR if needed above all else. If the ABCs are intact, consider O2 to maintain an SpO2 >94%. Check the blood sugar reading and administer 25 g D50 if it is <60 mg/dL. Initiate an intravenous line and provide a fluid bolus if the patient is hypotensive. If you suspect opiate drug overdose, administer 0.4–2 mg naloxone, titrated to adequate respirations.
Also known as fainting, syncope or a syncopal episode results from a sudden temporary drop in blood flow to the brain, resulting in a brief period of unresponsiveness. The transient lack of O2 and glucose causes the brain to shut down. Although this is the ultimate cause, the assessment goal will be to figure out why this happened in the first place. Standing up too fast from a seated or lying position, cardiac rhythm disturbance, a transient ischemic attack (TIA), a vasovagal response (i.e., straining too hard to have a bowel movement), and psychogenic shock are all possibilities that should be discussed with or evaluated on the patient.
Once blood returns to the brain in a sufficient quantity, the patient will regain consciousness, though frequently without recollection of the incident.
As with any patient, evaluate the ABCs and ensure that there is adequate ventilation, oxygenation, and circulation. Once this is assured, assess the patient for any trauma, particularly if he or she fell at all during the syncopal episode and pay close attention to the head. Finally ask the patient questions to attempt to isolate a cause from those listed above. It may not be obvious what caused the patient to pass out, and it may never be determined conclusively in the hospital.
Manage any derangement of the ABCs and any trauma the patient may have sustained. Evaluate the blood sugar level and treat with D50 as indicated for seizures and altered mental status. Continuously monitor the patient’s cardiac rhythm and treat any disturbances that may have contributed to the syncope; these include excessive PVCs, couplets or runs of VT, bradydysrhythmias, and tachydysrhythmias, among others.
The chief complaint of a headache is not one that usually strikes fear in the hearts of even the most novice paramedic. Fact is, most headache complaints are likely not life threatening or debilitating, with 2 glaring exceptions: meningitis and stroke. Strokes and the other symptoms were discussed earlier, which will help you differentiate a nominal headache from the life-altering headache of a CVA. Here, the discussion focuses on the other types of headaches, including the headache that is associated with meningitis.
Typical headaches are rarely treated in the field. If the patient is in severe pain from a migraine or a cluster headache, consider giving 30 mg ketorolac intramuscularly, 2–4 mg morphine sulfate as an intravenous piggyback, or 0.1 mg/kg fentanyl via slow intravenous piggyback for analgesia. Headaches often are accompanied by nausea, so 4 mg ondansetron would be recommended. For a meningitis headache, analgesia can be considered, but medical control should be contacted first. Initiating an intravenous line for fluid administration and being prepared in case of seizures or cardiac arrest is important in meningitis. That said, the most important treatment for a patient with meningitis may very well be to put a surgical mask on your own face if the patient does not wish to or for some reason cannot wear a mask. Although patient-to-provider transmission is rare, it is not a gamble worth taking. If the physician at the hospital believes that the provider was exposed, the physician will prescribe prophylactic antibiotics to the provider.
Dementia refers to any number of disorders that result in chronic deterioration of the brain. These diseases can occur as quickly as weeks, such as in Wernicke encephalopathy, or over decades, such as Huntington disease. The degradation of the brain can affect memory, personality, and language skills. Patients can become aggressive when they were previously docile, or vice versa. Because none of these conditions are particularly acute, they do not usually represent a serious emergency. When presented with a patient that is afflicted with one of these diseases, it is important to ascertain the patient’s baseline level of consciousness and degree of orientation. The patient may appear to have an altered mental status to the provider, even though this may simply be the new normal. If a caregiver or family member indicates to you that a person with dementia of any kind is not acting as he or she normally does, it is important to find out what the patient’s baseline is; this change may represent a progression of the disease, or there may be another underlying reason for an altered mental status.
The following nervous system disorders are disorders with which the paramedic should have a basic understanding; however, prehospital treatment is limited in scope and primarily supportive. Supportive treatment largely works to relieve symptoms. For example, if the patient is anxious, it may be worthwhile to give an anxiolytic, such as lorazepam; if the patient is in pain, consider ketorolac or fentanyl. The goal here is to ensure that the patient is comfortable because most of these disorders are chronic and require complex, continuous management beyond what a paramedic can accomplish.
Multiple sclerosis (MS) is an autoimmune disorder in which the body’s immune system arbitrarily attacks the myelin sheath surrounding the axons of the neurons, particularly those within the CNS. This results in scarring and a decline in functioning of the body part those neurons innervated. Patients often complain of numbness in their extremities and visual disturbances as the initial presenting sign. Over time, an increasing number of neurons are compromised, leading to widespread functional declines across nearly all body systems: muscle weakness and paresthesias, perceiving light touch as painful, bowel and bladder dysfunction, cognitive changes including speech and comprehension changes, and depression, just to name a few.
Guillain-Barré syndrome is a demyelinating disease like MS, where the immune system attacks the myelin sheath; however, the progression of Guillain-Barré syndrome is much more rapid. Unlike MS, it is a reversible disease, and a high percentage of patients make a full recovery. Although it is not fully understood, more than 2/3 of the people diagnosed with Guillain-Barré syndrome have recently had a respiratory illness, such as the flu or a bout with diarrhea. Agents believed to cause Guillain-Barré syndrome include the bacteria Campylobacter jejuni and the influenza virus. The disease presents itself as weakness and tingling sensation in the legs that moves up the body, quickly moving to the abdomen, chest, and arms. The progression from normal to profound systemic weakness requiring a ventilator for breathing can take but a few hours. Treatment is largely supportive but be prepared to initiate aggressive interventions, including intubation, ventilation, and fluid infusions. Unlike complications arising in MS, where the patient knows that he or she has the disease, patients with this condition do not know because of the nature of its sudden onset.
Lou Gehrig’s Disease, also known as amyotrophic lateral sclerosis (ALS), is a devastating and ultimately fatal disease. Little is understood even about what causes it in the first place, and there is no known cure. The best treatment is supportive, even after diagnosis. This disease attacks the voluntary motor nerves, causing them to die and the muscles they once innervated to atrophy. Disease progression will result in eventual failure of the muscles of speech and breathing. Patients will die within 3–5 years of the initial diagnosis.
PD is associated with a decrease in the production of dopamine in the brain, often caused by damage to the area of the brain responsible for its production. The damage could be caused by a concussion or other injury or simply the result of overuse. Dopamine is a neurotransmitter that is necessary for muscles to contract in a smooth, coordinated fashion. The disease progresses over time, starting off with minor tremors that are often isolated to 1 side. Patients then start walking stooped over as their muscles of posture begin to be affected. Next, the patient starts to display highly uncoordinated exaggerated movements, where the muscles seem to go from fully relaxed to fully contracted with a loss of subtle fine motor control. In the later stages, patients are at risk for aspiration and pneumonia because of poor swallowing and gag reflexes. Patients also are at risk for injury from falls.
Peripheral neuropathy is a global term for a group of conditions that damage the peripheral, or spinal, nerves. Trauma, tumors, bacterial or environmental toxins, metabolic disorders such as diabetes, and autoimmune diseases are all possible causes for peripheral neuropathy. The most common form of peripheral neuropathy is diabetic neuropathy. Patients complain of a burning and tingling sensation; as the disease process continues, the patient may lose all feeling in the area. In the case of diabetic neuropathy, the feet and fingers are most generally affected.