
This section will focus on injuries involving the face and sensory organs as well as neurological trauma of the head, brain, and spinal cord. Injuries to the sensory organs can make oral assessment and history taking more difficult for the provider. Injuries possibly involving the spine need to be treated cautiously because rough handling of the patient during extrication or transportation could result in a worsened injury. Head injuries can be difficult to care for because the patient can be combative, have seizures, or be resistant to treatment. The section starts by looking at the anatomy and physiology of each region, along with injuries and treatment for any injuries that may occur within that region.
The face and skull are made up of several bones held together at immovable joints, often called suture lines. The following lists the major bones of the face and the cranium. “Paired” noted in the definition indicates that the bones exist as separate bones on the right and left side of the face.
In addition to the temporal bone and the frontal bone, these bones comprise the cranial vault. “Paired” noted in the definition indicates that the bones exist as separate bones on the right and left side of the skull.

The eye is a complex sensory organ. As noted in the neurological section earlier in the book, several different nerves are responsible for the sense of vision (optic nerve, CN II) and the motion of the eyeball itself (oculomotor nerve, CN III; trochlear nerve, CN IV; and abducens nerve, CN VI). The extraocular muscles of the eye are responsible for movement of the eye and looking in different directions.
The cornea is a thin layer of colorless cells that covers the anterior portion of the eye over the pupil. This is a very delicate layer, and it does not take much to cause a corneal abrasion.
The pupil is a hole in the iris through which light passes through.
The iris is the colored part of the eye that dilates and constricts to control the amount of light entering the pupil.
Located just behind the pupil and iris, the lens focuses light on the retina to form an image. The thickness of the lens is controlled by the ciliary muscles, which attach to the lens on all edges of the lens.
The retina is a photosensitive layer of specialized cells that receive light entering the eye and convert the light into an electrical signal. The area of the retina with the most light-sensitive cells is called the fovea. This area of the retina allows for the clearest vision; other areas of the retina are less sensitive and therefore produce the less detailed image of the peripheral vision.
Once the retina converts the image to an electrical signal, it travels to the optic nerve and eventually to the visual cortex in the posterior region of the brain for interpretation. The optic disk is an area of the retina that does not contain any light-sensitive cells and is often called the blind spot.
Most of the globe of the eyeball is composed of a tough fibrous tissue that is white in color, called the sclera.
The lens and supporting ciliary muscles divide the globe of the eyeball into a large posterior chamber and a much smaller anterior chamber. The anterior chamber is filled with a fluid called the aqueous humor. The posterior chamber is filled with a clear fluid called vitreous humor. If the vitreous humor is lost, it cannot be replenished by the body, and the patient may end up blind. Aqueous humor, conversely, can be replenished by the body.
The lacrimal gland, located under the upper eyelid on the lateral edge, drips tears into the eye. With each blink, the tears drift across the eye and wash away any debris. The tears then drain from the eye into the lacrimal duct on the medial corner of the eye near the nose. The tears then drain into the nose. Tears also keep the conjunctiva, the underside of each eyelid that contacts the eye, lubricated so that blinking does not scratch the eye.

The ears are responsible for hearing; however, they also are responsible for maintaining a person’s balance and orientation in space. The vestibulocochlear nerve (CN VIII) is responsible for both of these senses and has 2 branches: the auditory branch and the vestibular branch. First, the sound will be followed along its progression; then the vestibular system will be discussed.
The ear has 3 subdivisions conveniently named the outer, middle, and inner ear. Sound first contacts the pinna, which is the outermost structure of the external ear. The sound is then funneled into the ear canal, where it contacts a thin membrane called the tympanic membrane or eardrum. The tympanic membrane is the division between the outer and middle ear.
The eardrum vibrates and transmits the sound through 3 bones: the malleus, the incus, and the stapes. The bones conduct the sound in that order to the oval window in the vestibule, and with that, the sound enters the inner ear. The eustachian tube connects the inner ear with the posterior pharynx, allowing the inner ear pressure to remain equal to atmospheric pressure.
The structure of the inner ear is the cochlea. As sound travels through this snail-shaped organ, the vibrations reach the organ of Corti that has specialized hairs that are sensitive to particular frequencies. Each hair then stimulates a nerve fiber of the auditory branch of the vestibulocochlear nerve. This electrical impulse is interpreted in the auditory centers in the temporal lobe of the brain.
Also within the inner ear, unrelated to the sense of hearing, are the semicircular canals, known as the vestibular system. Three semicircular canals arranged in perpendicular axes send signals to the brain to alert it to the body’s orientation in space and its relative speeds in each direction—side to side, front to back, and vertically.

Fractures of the bones of the face occur as a result of blunt trauma, such as the case of an unrestrained driver or passenger who collides face first with the dashboard or the windshield. A patient with facial fractures has sustained forces between 30g (nose) and 100g (maxillae and orbit), which is more force than astronauts experience during takeoff (about 3g). As a result, although a facial fracture may be visually stunning, it is more likely that the patient has a significant—often lethal—brain injury.
Facial fractures can present in a variety of ways depending on the bone that was fractured; however, all of them will present with bruising at the very least and likely nearby lacerations. Facial fractures that result in a fracture to the bones of the base of the cranial vault may cause CSF to leak out. If this happens, CSF can be seen mixed with blood coming from the ears and/or the nose. To assess this, perform the halo test: Dab a little blood coming from the ear or nose on a 4x4 bandage. If there appears to be a pale yellow ring around the red blood, this indicates CSF.
In addition to likely brain injury, the patient may present with significant airway compromise caused by bleeding into the airway, swelling of the airways, and possibly foreign bodies lodged in the airway (teeth). Airway compromise is the primary concern in nasal and mandibular fractures because they are directly involved in the airway.
Mandibular fractures, in addition to the aforementioned airway compromise and bleeding, also may present with malocclusion. Malocclusion is a change in the articulation of a patient’s teeth. The patient also may complain about pain on biting. Patients may not be able to talk in cases of fracture or dislocation of the temporomandibular joint because they are no longer able to close their upper and lower jaws.
Orbital fractures are most likely to occur on the inferior or lateral portion of the orbit and significantly less likely to happen in the superior edge of the orbit, which is the frontal bone. Any fracture, but particularly inferior orbital fractures to the orbit, carries with it the possibility of entrapment of or damage to facial nerves, resulting in numbness to the face. Extraocular muscles also may become entrapped or lacerated by the fractures. This will result in the patient’s eye not being able to follow the provider’s finger.
Zygoma fractures, also called cheek fractures, result in apparent asymmetry of the face with the affected side flatter than the other. Numbness and paralysis often result in that cheek, upper lip, and teeth. Eye movement can be inhibited as well.
Maxillary fractures are perhaps the most dramatic of any facial fracture and require the most force to occur. They will present with instability of much of the face and malocclusion as a possible symptom caused by shifting of the upper jaw. Fractures involving the maxillae are referred to as LeFort fractures.

Treatment of facial fractures often involves an extended focus on establishing and maintaining a patent airway. Manually open the airway, using only the modified jaw thrust to protect the cervical spine. An ETT is highly recommended if the patient requires positive pressure ventilation because the instability of the facial structures will make obtaining a seal for BVM unlikely. Suction should be liberally used before and during intubation attempts to clear the airway of blood, vomit, and any dislodged teeth. Because of the increased likelihood of fractures to the base of the skull with facial fractures, inserting anything into the nose is contraindicated. This includes nasopharyngeal airways, nasogastric tubes, and blind nasotracheal intubation. Application of a cervical collar in this patient, either before or after intubation, may help stabilize the jaw and support facial structures. Rarely, needle cricothyrotomy may be required to establish an airway; however, if needed, it should be employed early and quickly.
Eye injuries are concerning because they often result in some degree of vision loss, even if only temporarily. As a result of the temporary vision disturbance and the patient’s contemplation of permanent visual loss, the patient often has a high degree of anxiety with an eye injury. Eyes, like any other part of the body, can be subjected to blunt and penetrating trauma and are particularly sensitive to chemicals, heat, and irritants.
For a laceration or impaled object to the eye or eyelid, do not apply direct pressure to the eye. The application of pressure to the eye can be extremely harmful to the patient. First, pressure to the eye can stimulate a vagus response leading to bradycardia. Second, if the globe is lacerated or punctured, pressure can force aqueous or vitreous humor out of the eye, and, in extreme cases, the lens, iris, or even retina can be forced out of the eye as well. Any of these can lead to permanent blindness. Although the eyelid may bleed heavily, the eye does not often bleed much.
If the impaled object is still present in the eye, the goal is stabilization of the object to prevent further injury. Placing a cup or bulky dressings around the object and covering both the patient’s eyes is recommended. Covering both the patient’s eyes causes the patient to minimize eye movement, thereby providing protection against more damage from the impaled object. When applying the dressing and covering either eye, be sure to not apply pressure to the globe of either eye. In addition, this will effectively make the patient blind, so treat the patient as if they are:
Objects on the eye surface can be more than just a nuisance. They can cause corneal abrasions or lacerations. Chemicals can lead to conjunctivitis or inflammation of the conjunctiva. Flush the affected eye with water away from the unaffected eye. Do not allow the patient to rub his or her eyes.
Because the eye is somewhat recessed within the socket (orbit), blunt eye injuries are relatively uncommon. Blunt trauma can result in rupture of the globe or hyphema, bleeding into the anterior chamber of the eye. The retina also can detach from the sclera as a result of blunt trauma. Blunt trauma in the area of the eye can cause the eye to protrude from the orbit. If the globe is exposed, place a moist sterile dressing directly in contact with the avulsed eye and cover with a dry sterile bandage that includes both eyes.
External ear injuries are generally limited to the pinna and are the same as any other area of the body. Soft-tissue injuries to the external ear often heal poorly because of the poor blood supply. The result is often a deformed pinna called cauliflower ear.
Blunt injuries to the ear typically do not result in meaningful external injury; however, it is possible that the eardrum will rupture. This is especially likely when a person is slapped in the ear, such as might happen during an assault. It also may occur if the patient is close to an explosion. Bleeding is possible, though typically it is light. If there is bleeding from the ears, never pack the canal. Instead, loosely bandage the ear to allow the blood to drain. If there is bleeding from the ear, perform a halo test to evaluate for CSF.
Head injuries can result from blunt and penetrating trauma to the skull. Head injuries can occur from falls, assaults, sports-related injuries, motor vehicle collisions, or gunshot wounds. They often can involve neurological deficits that can range from short-term anterograde amnesia to unconsciousness, brainstem herniation, and eventual death. In the previous section, it was noted that facial injuries can transmit energy to the brain, leading to injuries there as well. The types of skull fractures will be presented first; the implications on the brain will be discussed a bit later.
Basal skull fractures are fractures to the base of the skull and can result from impacts on any area of the head; however, large forces are usually required to cause basal skull fractures. Signs and symptoms of a basal skull fracture often include blood and CSF leaking from the ears, nose, or both. This can be found by performing the halo test described previously. Patients with basal skull fractures also may have periorbital ecchymosis, known as raccoon’s eyes, or ecchymosis in the area of the mastoid process called the Battle sign. Both of these take a while to form and are considered late signs not usually seen immediately following the traumatic event.
Linear skull fractures are a closed, nondisplaced fracture of the skull that often results from blunt trauma. If the underlying brain is not injured, then the fracture itself is not typically anything to worry about.
Depressed skull fractures are fractures that result from blunt trauma to the skull, resulting in multiple fractured pieces of skull in 1 area. The result is a dent or a depression of the skull. Such fractures can cause shards of skull to become embedded in the brain tissue, leading to profound neurological deficits. Concurrent basal skull fractures are possible when this much force has been imparted to the skull.
Head injuries can be open or closed. In an open head injury, brain tissue is exposed as a result of skull fracture. In a closed head injury, brain tissue has still been injured regardless of whether the skull has been fractured. But brain tissue is not exposed. Remember, with every fracture listed here, if the scalp over the top of the fracture is broken, it is considered an open fracture. This is not the same as an open head injury.
Traumatic brain injury is any injury to the brain that results in transient or permanent cognitive, intellectual, or emotional changes. A primary brain injury is the actual injury to the brain as a direct result of the insult. This injury can be through penetrating trauma such as a gunshot wound; however, it is much more likely the result of blunt trauma to the head and brain. After the head is impacted, say by the concrete sidewalk during a fall, the brain will continue to move within the cranium until it collides with the inner wall of the cranium. At this point, the brain is injured in the same area of the initial impact. This is called a coup injury. If the force was great enough, the brain may then bounce off the cranial wall and into the other side of the cranium, thus injuring the side of the brain directly opposite the point of impact. This is called a contrecoup injury.

Secondary brain injuries happen after the brain has been directly injured. These injuries include the damage to the brain tissue that results from bleeding into the brain and swelling of the brain. This also can include any infections and abscesses that can occur with open head injuries. Finally, cerebral ischemia, hypoxia, and infarct can happen when blood flow to a particular area of the brain is compromised for even just a short period of time.
Secondary brain injuries can lead to a worsened patient outcome because the skull is not capable of expanding to make room for the swelling brain after an injury. Because swelling will occur whether or not the brain has a place to go, it will first move into the potential spaces within the cranium. These include the small volume initially occupied with CSF. Once that space has been occupied, it starts to occlude the blood vessels within the cranial vault. Throughout this process, the pressures within the head are increasing. This is referred to as increasing ICP.
As this pressure increases, the brain recognizes that it is getting hypoxic as a result of the pressures building up, so, as a matter of self-preservation, it orders an increase in blood pressure. Blood pressure increases. However, not knowing what is happening in the brain, the carotid sinuses, which measure pressure, recognize an increase in pressure that they did not call for and order the heart rate to slow down. So, the heart rate slows down. This cycle of increasing blood pressure and decreasing heart rate will continue and worsen as the pressure in the skull continues to rise.
The brain does this to maintain cerebral perfusion pressure (CPP). The minimum CPP required to perfuse the brain under normal circumstances is 60 mmHg and can be calculated by subtracting the ICP (which cannot be measured in the field) from the MAP. MAP is shown on automatic blood pressure cuffs as a number in parentheses but can be calculated by doubling the diastolic number, adding to it the systolic number, and dividing by 3.
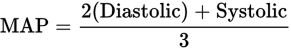
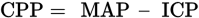
Normally, ICP is less than 15 mmHg and can be 0. Therefore, it is essential that the MAP of any patient, especially the patient with a head injury, be kept above 60 mmHg by maintaining blood pressure and providing fluids.
As the brain continues to swell, after occluding the blood vessels, now kept open only with the markedly increased blood pressure, the only other option for the brain in a closed head injury is to herniate out of the foramen magnum at the base of the skull through which the spinal column passes. To do this, it must first push out the medulla and midbrain, which includes the respiratory centers of the brain. Pressure and damage to the respiratory center results in an ataxic respiratory rate, which tends to be fast, shallow, and irregular. This type of respiration will not be effective in maintaining oxygenation or removing CO2 and will lead to a respiratory acidosis that can possibly cause the cerebral arteries to dilate, further worsening the ICP. Ataxic respirations, combined with bradycardia and hypertension, is called the Cushing triad or the Cushing reflex. This is a hallmark sign of a potentially lethal brain injury.
Signs and symptoms to look for when assessing a patient with a head injury include the Cushing triad but also include evaluation of pupil equality. As the brain swells, it will exert pressure on the oculomotor nerve, causing one pupil to be dilated and sluggish to react or completely unreactive to light. The patient may vomit without a previous complaint of nausea. The patient may have an altered mental status or have had a transient loss of consciousness prior to EMS arrival.
Concussion is a diffuse brain injury that can occur with any blow to the brain. Concussions are most common in deceleration injuries, such as those that result from sports injuries, motor vehicle crashes, and falls. A concussion is not associated with long-term debilitation. Loss of consciousness is not necessary for a person to have sustained a concussion. Patients may be amnestic to the events that caused the injury and may show either anterograde or retrograde amnesia, but a patient may not have either.
A diffuse axonal injury is characterized only once in the hospital. These injuries are differentiated from a concussion because the brain has sustained more extensive damage to the axons of the neurons, resulting in interrupted transmission of nerve signals. Axons can be sheared or torn off the nerve bodies, which is often not survivable or results in permanent deficits. Stretching of the axons, instead of shearing them, is survivable but may result in some long-term impairments depending on the area of the brain affected.
Cerebral contusions are a bruise within the cerebrum in a local area. This is worse than a concussion because this actually results in structural damage to the brain and a loss of the blood-brain barrier, resulting in a longer period of neurological deficits than with concussion.
An epidural hematoma is located outside the dura mater between the meninges and the skull. Epidural hematomas are most commonly caused by blunt trauma and linear fracture to the temporal bone and a laceration to the middle meningeal artery that underlies it. The trauma to the head that leads to the epidural hematoma usually first causes the patient to lose consciousness. The patient will then regain consciousness and have a “lucid interval” before losing consciousness again after the ICP has critically increased. Often, the patient also will display unequal pupils.
A subdural hematoma results when 1 or more of the veins that lie between the dura and the brain are torn during a traumatic event. This is very common in elderly falls and motor vehicle accidents because the distance between the brain and dura mater expands as a result of atrophy and shrinking of the cerebral tissue. Here, blood accumulates beneath the dura but still outside the brain tissue. It has the capacity to increase ICP; however, it takes a much longer time to develop than an epidural hematoma; sometimes it is not clinically apparent for days or weeks after the injury.
An intracerebral hematoma is worse than a cerebral contusion because the bleeding is heavier and affects a larger area of the cerebrum. Although the blood can be surgically removed from within the brain tissue, there is still a very high likelihood of death with this type of injury.

Bleeding into the subarachnoid space where the CSF circulates leads to a significant headache as a result of meningeal irritation. A subarachnoid hemorrhage is associated with a high mortality rate; those who survive often have significant clinical deficits. Signs and symptoms include those associated with closed head injury.
The anterior neck has several relatively superficial structures of concern when assessing neck trauma. First, along the midline is the trachea, and located superficial to the thyroid cartilage of the trachea is the highly vascular thyroid gland. Immediately lateral to the trachea lie each of the carotid arteries. They are reasonably protected with overlying muscles. Moving further laterally are the jugular veins. Also within the neck, in the area of the carotid arteries, are several cranial nerve bundles, including the vagus nerve among others.
Penetrations and lacerations to the anterior neck can be immediately life threatening. The trachea is particularly vulnerable to lacerations because of its prominent location. Lacerations to the trachea will result in heavy bleeding and difficulty breathing. Treat a lacerated trachea similar to a dislodged tracheostomy tube. Place an ETT directly through the hole in the anterior trachea, inflate the cuff, and either allow the patient to breath unaided through the tube or ventilate as needed.
If the great vessels—either the carotids or the jugulars—are lacerated, bleeding will be massive. Controlling the bleeding can be tricky because the application of pressure to the bleeding site can stimulate a vagus response. A failure to occlude both sides of the lacerated vessel can result in a massive air embolus directly into the brain if the laceration is on the superior side of the carotid or directed into the heart if the lacerated vessel is one of the jugulars. In addition to the massive bleeding, patients could present with neurological deficits as a result of a possible air embolus or simply the lack of cerebral blood flow. Apply an occlusive dressing to lacerations of the great vessels of the neck and apply enough pressure to control bleeding.
Blunt injuries to the neck most commonly will result in tracheal fractures. If the cartilaginous rings are broken, then the trachea is no longer able to remain open when the patient takes a breath. This will cause severe—possibly fatal—difficulty in breathing because the trachea collapses with each inhalation. Rapidly providing positive pressure ventilation is essential for this patient. If the tissue of the trachea also is ruptured, air may escape into the mediastinum and cause additional problems as the pressure builds up.
Thirty-three vertebrae make up the spinal column. The vertebrae surround and protect the bundle of nerves that is the spinal cord. Each vertebra is connected to a vertebra above and below it with multiple ligaments and cushioned from each with a cartilaginous pad located between the vertebral bodies. All vertebrae have the following features:

The vertebral column is divided into 5 different sections. The vertebrae are identified based on their location and number, working superior to inferior. For example, the first thoracic vertebra is named T-1.
The Cervical Vertebrae (7). Each of the other cervical vertebrae differ from the remainder of the column in that they all have a foramen on the lateral sides through which passes the vertebral arteries. They are the only vertebrae that have this feature. C-1 and C-2 differ from each of the other 5 in this section and have specific names: atlas and axis, respectively. The axis (C-2) provides the axis on which the atlas (C-1) spins when the head turns from side to side.
The Thoracic Vertebrae (12). Each thoracic vertebra is associated with a pair of ribs that articulates on the lateral facets. The spinous processes are slightly more pronounced because they have more muscle and ligaments attached than other vertebrae.
Lumbar Vertebrae (5). Lumbar vertebrae have the largest and thickest vertebral bodies because they support the weight of much of the body superior to it.
Sacrum (5). These vertebrae are fused together within the ring of the pelvis.
Coccyx (4). The vestiges of our tail, injuries to the coccyx are usually insignificant, despite being extremely painful.
The spinal cord transmits messages from the brain to the PNS and from the PNS to the brain. Sensory signals travel on the afferent (ascending to the brain) tracks, whereas motor signals travel on the efferent (exiting the brain) tracks to the muscles of the body. Spinal nerves exit the spinal column in between every vertebra and are named according to the vertebra above it. Inferior to L2, the spinal cord the nerve roots take on the appearance of a horse’s tail. This region is aptly referred to as the cauda equina and services the lower extremities.
The neck is the only area of the spine that allows for a comparatively wide range of motion. So injuries are caused by flexion, rotation with flexion, and hyperextension. Each injury type can result in different presentations.
Flexion injuries result from any incident where the head can whip forward suddenly. They can result in fractures to the atlas and axis or dislocation of these joints. Each of these can be described as either stable or unstable. Unstable injuries are more significant and can result in stretching or tearing of the spinal cord. Flexion when combined with rotation of the head, such as what may happen during a lateral impact during a motor vehicle accident or an assault or tackle in a football game, can result in even worse injuries to the C-1 and C-2 area.
Hyperextension injuries can occur anywhere in the spine, but mostly occur in the cervical spine. Hyperextension of the cervical spine can result in a hangman’s fracture. A hangman’s fracture is a fracture to C-2 that results in bilateral fracture to both pedicles. This is an unstable fracture but does not typically result in a cord injury.
Compression injuries can result from vertical compression of the spine, also known as axial loading. This often results in burst fractures of the vertebral body anywhere along the spine. It is most commonly found in the cervical and lumbar vertebrae because the cervical vertebral bodies are the smallest of all, and the lumbar already support the most weight, so any more load can result in fracture. The compression force can come from above, such as hitting the crown of the head on the roof of a car during a collision or from below as might happen when jumping from a height and landing on the feet with locked knees. Most of these fractures are stable relative to causing cord injury; however, continued movement of the fractured vertebra could force a piece of bone into the cord, lacerating it.
A primary cord injury is any cord injury resulting directly from the traumatic event. This can include complete or partial transection from penetrating trauma. Primary injury from blunt trauma is more varied. Transection of the cord can still occur with blunt trauma after the ligaments that hold the vertebrae together are torn. This leads to an unstable dislocation of the vertebrae in that area, which could lead to one sliding off the other and cutting the spinal cord. Fractures to the vertebra can force a piece of bone shrapnel into the cord, leading to partial loss of neurological function on the affected side. Injuries such as these result in permanent deficits.
Hemorrhage into the spinal canal and contusions to the spinal cord itself can lead to temporary or permanent deficits. Spinal distraction, or the stretching of the spinal cord resulting from the vertebrae being pulled apart can cause small tears in the neurons or acute swelling. Each of these may result in normal radiology studies and may be referred to as SCIWORA, which stands for a spinal cord injury without radiological abnormality.
Like any other tissue in the body, the cord can swell as a result of trauma leading to a temporary loss of neurological function distal to the injury. It is not uncommon for a patient to have normal feeling and motor after an incident but later have paresthesias or movement problems distal to a traumatic spine injury. What follows is a list of secondary cord injury syndromes with their symptoms and prognoses.
Anterior cord syndrome results from disruption of the anterior region of the cord often caused by flexion injuries. The patient will present with motor and sensory loss to the area inferior to the injury.
Central cord syndrome is associated with hyperextension injuries of the cervical spine. Patients with this type of injury will have a loss of function of the upper extremities, whereas motor function of the lower extremities tends to remain intact. Patients may have acute bowel and bladder dysfunction with this and also may have variable changes in their sensation to pain and temperature of the upper extremities. This injury is common in the elderly, particularly those with arthritis of the spine or spinal stenosis. Recovery from this often is complete but with bilateral hand weakness sometimes persisting.
Posterior cord syndrome is likely with extension injuries, though much less common. Patients with this syndrome will have a decreased sensation to light touch and proprioception. Proprioception is the person’s ability to perceive position in space without having to look at the limb.
Cauda equina syndrome is caused by lesions in the L-1 and L-2 area, including hemorrhage, transection, and penetrating injuries. In addition to low back pain, it can lead to paresthesias to the lower extremities, particularly those areas that would contact a saddle. Patients also will present with decreased rectal tone and have bowel or bladder dysfunction.
Brown-Sequard syndrome can be thought of as lateral cord syndrome, though it is never referred to this way. It results from damage to 1 side of the cord from either distraction, transection, or a penetrating injury. Damage to all nerve tracts on 1 side of the spinal cord leads to loss of motor and light touch and vibration on the side of and inferior to the injury. This also will lead to the loss of pain and temperature sensation on the side opposite the injury.
Neurogenic shock can result from any of the above injuries. It causes widespread dilation of vessels inferior to the spinal cord lesion. This, in turn, leads to hypovolemia relative to the size of the container. Patients will present pale and diaphoretic superior to the injury and flushed and dry inferior to it.
The assessment of suspected spinal cord injuries should involve careful palpation of the entire spinal column. Encountering a step-off, or an area where the spine is no longer a continuous line, indicates a possible transection of the cord or a distraction injury at least. As with extremity fractures, assess distal pulse, motor, and sensation, particularly in the lower extremities and document findings. Anytime the patient has or is suspected of having a spinal cord injury (SCI), the patient should be carefully transferred to a backboard and fully immobilized with a cervical collar and head immobilization devices. Anytime the patient is transferred or moved in any way, reevaluate pulse, motor, and sensation of the extremities.
Treatment of SCIs has 2 primary goals. Minimizing the progression of secondary spinal injuries should be the primary goal. This is accomplished by employing spinal motion restriction devices, such as the short spine board if the patient is found seated, and securing the patient to a long backboard as well, regardless of position found. Second, the patient should be treated for shock, and steps should be taken to prevent the onset of shock. Often, an SCI is not the only issue facing the patient, so completing a full secondary assessment and the treatment of any life-threatening conditions found should not be ignored.