
Fractures, sprains, and strains are a common reason for a patient to need an ambulance. Often, these are in the context of more serious, multisystem trauma. This section will discuss the musculoskeletal system and assessment and treatment of musculoskeletal injuries, focusing on those of the appendicular skeleton.
Skeletal muscles are under voluntary control, which means that the patient controls all aspects of muscle movement. These muscles also are referred to as striated because under a microscope, they appear to have stripes. Skeletal muscle includes all the muscles attached to the skeleton, and they provide much of the bulk surrounding the skeleton.
Skeletal muscle is responsible for moving bones that are capable of movement, but skeletal muscle also is responsible for facial expressions, blinking, tongue movement, maintenance of posture, and swallowing. Skeletal muscle has a high metabolic rate and requires a constant flow of O2. Consequently, skeletal muscles have a rich blood supply and often bleed profusely when injured.
Skeletal muscles that are attached to 2 bones have an insertion and an origin. The insertion is the end of the muscle attached to the bone that moves the most during contraction. The origin is the end of the muscle attached to the bone that moves the least during contraction. For example, the origin of the biceps muscle in the upper arm is the scapula, and the insertion is located on the radius in the forearm. When the biceps contracts, the forearm is flexed upward.
There are 2 types of skeletons: the exoskeleton and the endoskeleton. The exoskeleton encases a whole organism and is usually found in arthropods, such as crustaceans and insects. Vertebrates, including humans, have an endoskeleton. The endoskeleton is internal but is not able to protect soft-tissue structures as well as exoskeletons. However, exoskeletons must be shed and regrown to accommodate growth. The endoskeleton is much better able to accommodate the growth of a larger organism.
The components of our skeletal system are divided into axial and appendicular skeletons. The axial skeleton consists of the skull, the vertebral column, the rib cage, and the hyoid bone (a small bone in the anterior neck used for swallowing); it provides the basic central framework for the body. The appendicular skeleton consists of the bones of the limbs (humerus, radius and ulna, carpals, metacarpals, and phalanges in the upper limb; and femur, tibia and fibula, tarsals, metatarsals, and phalanges in the lower limb), the pectoral girdle (scapula and clavicle), and the pelvis. Both skeleton types are covered by other structures (muscle, connective tissue, and vasculature).

The skeleton is created from 2 major components: bone and cartilage.
Bone is a connective tissue derived from embryonic mesoderm. Bone is much harder than cartilage, but it is relatively lightweight.
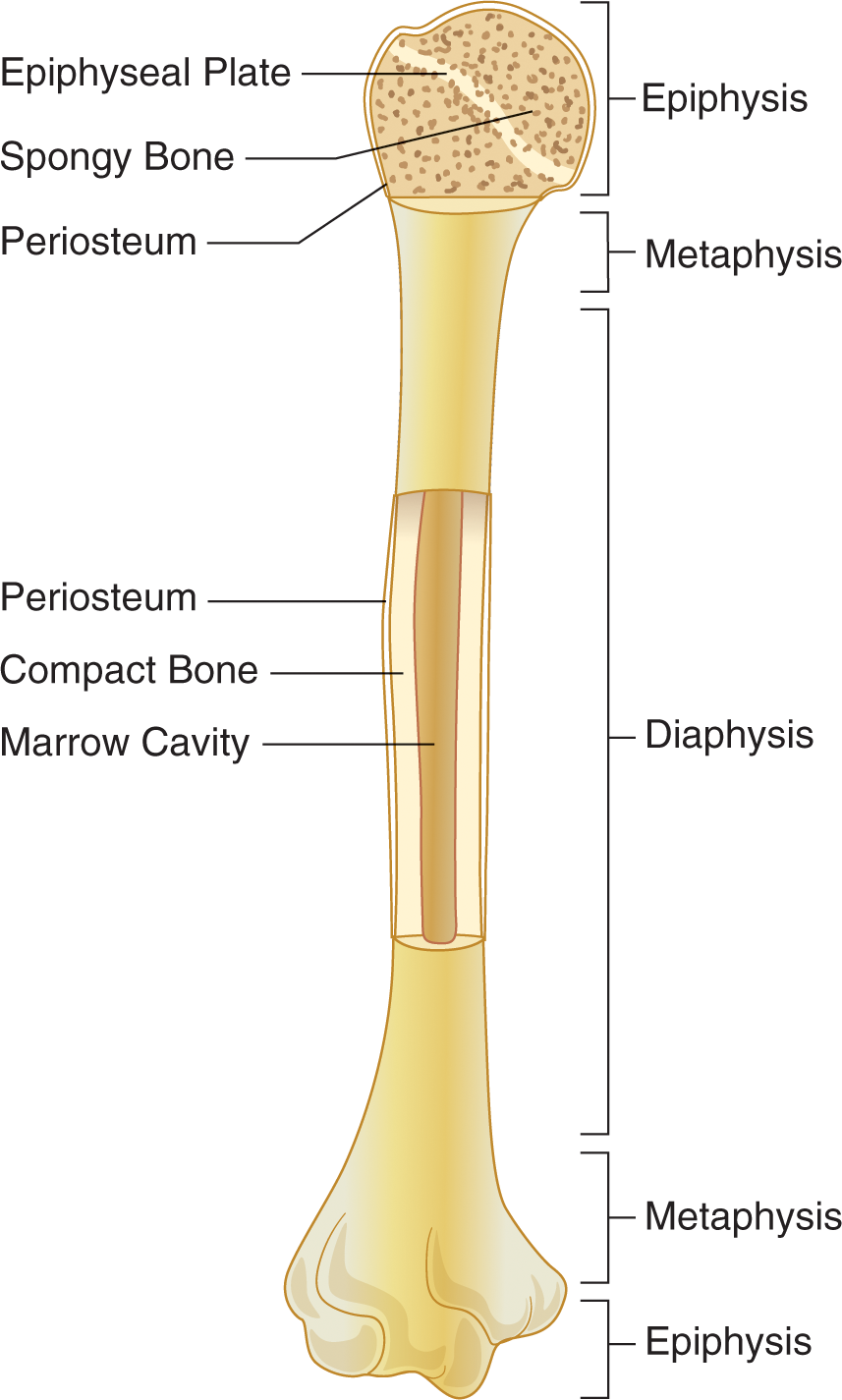
Bone’s characteristic strength comes specifically from compact bone. It lives up to its name because it is both dense and strong. The other type of bone structure is spongy or cancellous bone. The lattice structure of spongy bone is visible under microscopy and consists of bony spicules (points) known as trabeculae. The cavities between trabeculae are filled with bone marrow, which may be either red or yellow. Red marrow is filled with hematopoietic stem cells, which are responsible for generating all the cells in our blood; yellow marrow is composed primarily of fat and is relatively inactive.
Bones in the appendicular skeleton are typically long bones, which are characterized by cylindrical shafts called diaphyses that swell at each end to form metaphyses and terminate in epiphyses. The outermost portions of bone are composed of compact bone, whereas the internal core is composed of spongy bone. Long-bone diaphyses and metaphyses are full of bone marrow. The epiphyses, on the other hand, use their spongy cores for more effective dispersion of force and pressure at the joints. At the internal edge of the epiphysis is an epiphyseal (growth) plate, which is a cartilaginous structure and the site of longitudinal growth. Prior to adulthood, the epiphyseal plate is filled with mitotic cells that contribute to growth; during puberty, these epiphyseal plates close, halting vertical growth. Finally, a fibrous sheath called the periosteum surrounds the long bone to protect it as well as serve as a site for muscle attachment. Some periosteum cells are capable of differentiating into bone-forming cells; a healthy periosteum is necessary for bone growth and repair.
Structures in the musculoskeletal system are held together with dense connective tissue. Tendons attach muscle to bone, and ligaments hold bones together at joints.
Cartilage is softer and more flexible than bone. Cartilage consists of a firm but elastic matrix called chondrin that is secreted by cells called chondrocytes. Fetal skeletons are mostly composed of cartilage. This is advantageous because fetuses must grow and develop in a confined environment and then must traverse the birth canal. Adults have cartilage only in body parts that need a little extra flexibility or cushioning (external ear, nose, walls of the larynx and trachea, intervertebral discs, and joints). Cartilage also differs from bone in that it is avascular (without blood and lymphatic vessels) and is not innervated.
Most of the bones of the body are created by the hardening of cartilage into bone. This process is known as endochondral ossification and is responsible for the formation of most of the long bones of the body. Bones also may be formed through intramembranous ossification, in which undifferentiated embryonic connective tissue (mesenchymal tissue) is transformed into—and replaced by—bone. This occurs in bones of the skull.
Like bone and cartilage, joints are made of connective tissue and come in 2 major varieties: immovable and movable. Immovable joints consist of bones that are fused together to form sutures or similar fibrous joints. These joints are found primarily in the head, where they anchor bones of the skull together.
Movable joints include hinge joints (such as the elbow or knee), ball-and-socket joints (like the shoulder or hip), and others. They permit bones to shift relative to one another. Movable joints are strengthened by ligaments, which are pieces of fibrous tissue that connect bones to each another, and consist of a synovial capsule, which encloses the actual joint cavity (articular cavity). A layer of soft tissue called the synovium secretes synovial fluid, which lubricates the movement of structures in the joint space. The articular cartilage contributes to the joint by coating the articular surfaces of the bones so that impact is restricted to the lubricated joint cartilage, rather than to the bones.


A fracture is a break or crack anywhere in the bone. The break does not have to be completely through the bone. Fractures can be classified based the following means.
The 6 types of fractures are as follows:
Fractures are can be defined based on completeness:

Nondisplaced fractures remain in alignment at the fracture site. This is most common in linear fractures but can happen during any fracture if the extremity is replaced into a neutral position. In a displaced fracture, the bone ends no longer align. These are the following types of displaced fractures:
One final way to classify fractures is by whether they are open or closed. In closed fractures, the skin over the fracture area is intact. In open fractures, the skin over the fracture site is lacerated, from either external trauma or the bone ends lacerating the skin from inside. Open fractures also carry with them the added considerations of increased incidence of infection and increased bleeding. Any time the skin is broken, the likelihood of infection increases. Bleeding will increase markedly, however, because when the bone ends are exposed, the tamponading effect of a closed fracture is lost. Bones often are highly vascularized, especially in the marrow. With that in mind, when bone ends protrude through the skin, bleeding worsens.
Pain often is localized to the fracture site. In fact, pain often can be pinpointed to that area, not throughout the limb.
Deformity often will occur as an unnatural bend in the area of the fracture. If the fracture remains aligned, this may not be seen.
If the fracture becomes an overriding fracture and the muscles surrounding the fracture contract, shortening may occur, in which the affected limb may appear shorter than the other limb, if a comparison can be made. This is commonly seen in femur fractures.
Localized bleeding and tissue damage will result in swelling in the area of the fracture. Compartment syndrome is a concern when swelling is present. Bruising also may become apparent.
Crepitus is the feeling of the bone ends rubbing together. Sometimes it can even be heard. This should not be deliberately generated once it is found because it can cause more injury.
Patients with an extremity fracture often will not be able to move the limb distal to the injury, which can be caused by muscle entrapment in the fracture, lacerations to the muscle in the area of the fracture, or motor nerve damage. Frequently, pain with motion is enough to prevent deliberate movement. There also is the possibility of distal numbness if there is damage or entrapment of the sensory nerve in the area of the fracture. Distal pulses may not be palpable because of blood vessel entrapment, a laceration at the fracture site, or swelling that pinches off the vessel.
A dislocation is any displacement of the articulating surfaces of a joint. A dislocation may or may not be associated with a fracture in the same extremity. A dislocation often involves damage to the tendons surrounding the joint as well. The dislocated bone will lock into the new position because of the stretch and spasm of the muscles. Dislocations of the knee cap, elbow, and shoulder are among the more common. Dislocations to the hip joint are very common after an operation for a total hip replacement because the tendons have been manipulated during the operation.
A subluxation is a partial dislocation. In a subluxation, the articulating surfaces are no longer properly aligned. Because some of the tendons and ligaments are still intact in the joint and the joint is not locked into place as it is in a dislocation, the patient may have some capability of movement in that joint.
A sprain occurs when ligaments are stretched or torn. This can result from the joint being unnaturally twisted or a transient dislocation or subluxation that spontaneously resolves. Sprains commonly occur in the knee, ankle, and wrist.
When a muscle or tendon is stretched beyond its normal length, a strain is the result. This can occur during periods of excessive use or when the muscle is put into use in a violent manner, such as when a basketball player cuts from running in 1 direction to the other suddenly. Muscle strains are usually described as aches that worsen with use of the injured muscle.
Sudden swelling immediately following a sudden burst of pain, called edema, is common, particularly in sprains. This is often located directly superficial to the injured ligaments. The swelling can be significant to occlude blood flow distal to the injury. Always check for a distal pulse, motor, and sensation and document any deficits.
Pain for both sprains and dislocations is usually severe and in many cases worse than that of fractures. With an isolated closed fracture, pain is usually related to the amount of soft-tissue injury; in a dislocation or sprain, muscle spasms in the area contribute to ongoing, often worsening pain.
More common with sprains, discoloration and bruising often appear within 24 hours or so of the injury.
Treatment for any musculoskeletal injury begins with ensuring that the patient’s ABCs are intact. Consider cervical spine immobilization if the patient could possibly have sustained a spinal injury as well. Orthopedic injuries and the pain they cause can be distracting injuries; this means that the patient may not even notice that they have neck or back pain because the pain from the fracture or dislocation is so severe. Any other life-threatening injuries or the presence of shock should, in most cases, be treated before any focus is placed on the orthopedic injury. For the purposes of this section, let’s assume that there is an isolated injury to an extremity.
Evaluate the injured extremity for pain, deformity, discoloration, and swelling. If there is swelling, carefully mark the edges of the swollen area if they are well defined so that later when the area is assessed in the hospital, doctors and nurses are able to see if the swelling has worsened during the time that EMS was with the patient.
Next, check for pulse, motor, and sensation distal to the injury:
A helpful mnemonic for the treatment of fractures and dislocations is RICE. Because it is not practical to describe treatment of every possible fracture or dislocation a patient may sustain, RICE stands for the following:
Fractures and dislocations each need to be immobilized using a splint. To adequately splint a fracture, the joint above and below the fracture must be immobilized. To thoroughly splint a dislocation, the bones above and below the dislocated joint must be immobilized. The splint can be a pillow, a padded board, a vacuum splint, or any other object or tool that limits the motion of the fracture or dislocation. The following steps outline the proper splinting procedure after the injury has been assessed for the presence of pulse, motor, and sensation.
The long backboard can be a sufficient splint for any fractured extremity. Splinting should not supersede treatment of life-threatening injuries.
Once the extremity is splinted, applying a cold pack over the injury can be beneficial. It can help limit pain and control localized inflammation. It also can reduce swelling over time. Hot packs should be avoided for most injuries, particularly in the acute phase; however, heat may be helpful after the first 48 hours of an injury.
Analgesia should be administered to any patient in clinically significant pain. Clinically significant pain is pain that is so bad that it is having an effect on vital signs, which is particularly seen as an increased pulse rate. If the patient is tolerating the pain well, analgesia should not be given prophylactically. Patients should be given 1 mcg/kg up to 100 mcg fentanyl or 2–4 mg morphine sulfate for significant pain.
Injuries to the upper extremity and certain types of shoulder dislocations are best splinted with a sling and swath. The sling can be made from a triangular bandage and should support the entire forearm from elbow to wrist. The ends are then tied around the neck of the patient with the knot padded to minimize pressure on the soft tissues of the neck area. The swath is a band made from another triangular bandage tied around the body of the patient to prevent movement of the extremity in the sling and provide added support. Both should be tied such that they provide support and take the responsibility of holding the arm away from the patient, but they should not impede breathing.
A traction splint is applied to the lower extremity when there is a suspected mid-shaft femur fracture. The traction applied pulls the contracted upper leg muscles into a neutral position. Often, this is enough to relieve the pain from the femur fracture. This also can help minimize bleeding in the area resulting from the fracture.
Pelvic fractures require a significant amount of force and are consequently fairly rare. They also are associated with a high mortality rate because of the concurrent damage to the structures underlying the pelvic bones. In addition, the pelvis can hold a lot of blood, which is difficult to assess. For these reasons, a pelvic fracture requires the paramedic to maintain a high index of suspicion for greater problems than just the orthopedic injury.
Pelvic fractures can result from lateral compression from falls or T-bone type accidents or from anterior-posterior (AP) compression from a head-on motor vehicle collision or a fall landing on the buttocks. In a lateral fracture, the ring of the pelvis tends to be compressed, reducing the overall diameter of the pelvis. Although this usually causes significant internal trauma, the bleeding gets tamponaded more quickly because of the reduced volume in the pelvis. In an AP compression fracture, often called an open book fracture, the pelvis widens, worsening any bleeding that may be occurring within the pelvis. It is called an open book fracture because in this type of fracture, the symphysis pubis spreads open like a book might when it is set on its spine. Remember also that because the pelvis is a ring, if the pelvic ring is broken in 1 location, it must be broken in a 2nd location as well.
Both vertical shear and straddle injuries involve an upward force directly on the pelvis. Vertical shear injuries result when a person lands on his or her feet with locked knees, transmitting the force of the fall all the way up through the legs to the pelvis. This can result in tearing of the ligaments of the pelvis and essentially splits the pelvis apart in the area of the symphysis pubis anteriorly and the sacrum posteriorly. Straddle injuries to the pelvis occur when a person lands almost exclusively on the perineum. The most common fracture that results is to the rami of the ischium. Injuries of this type usually result in more significant injuries to the perineum and the genitourinary system. Bleeding from this area can be substantial.
Because of the high likelihood of internal injuries with pelvic fractures, the primary focus is to anticipate and treat for shock. Remove the patient’s clothing and immobilize the patient on a long backboard. Initiate cardiac monitoring and at least 1 large-bore intravenous line with fluid running to maintain a systolic blood pressure >90. Once the patient has been immobilized and shock prevention measures have been initiated, attention should focus on stabilizing the pelvis. Although the long backboard itself can be a sufficient splint for most situations, the application of a pelvic binder is recommended.
A pelvic binder is a specialized splint that wraps around the pelvis. When properly secured, it will squeeze the open book fracture closed. It provides uniform circumferential pressure to stabilize the pelvis. This type of splint is far superior to a board splint or the backboard alone. This will reduce pain for the patient as well as possibly reduce the bleeding associated with the fracture.
A hip fracture actually involves fractures of the proximal femur. The fracture can be an intertrochanteric fracture, which is a fracture of the proximal end of the shaft of the femur, or, more commonly, it will be a fracture of the neck of the femur, which is the area of the femur which articulates with the acetabulum of the pelvis. Both of these fractures can occur in patients of any age but are a much more common result of a fall in the elderly, especially those with osteoporosis. A femoral neck fracture is one of the most common sites of a pathologic fracture in the patient with osteoporosis. Pathologic fractures occur as a result of normal activity, not from any discernible traumatic event. In the case of a femoral neck fracture in a patient with osteoporosis, simply standing and adding weight to the femur again can be enough to break it.
Patients with a hip fracture will have the leg of the affected side shorter than the other. That leg will be rotated externally (laterally) as well. This shortening and rotation is a hallmark sign of a displaced hip fracture. Nondisplaced hip fractures are less common and may not show the classic shortening and rotation. Assess the extremity for distal pulse, motor, and sensation as previously noted. Splint the fracture with either a board splint long enough to immobilize the entire leg all the way up to the armpit or simply place the patient on a long backboard. After immobilizing the patient with either option, reassess the extremity for distal pulse motor and sensation. Blood loss is usually minimal; however, initiating an intravenous line and providing pain management is appropriate.
Femur fractures often result from a high-speed impact directly to the upper leg, such as during a motorcycle accident, a motor vehicle accident, or a sports injury. Femur fractures can be associated with severe bleeding, which often is exclusively internal and can be up to 1,500 mL of blood lost into the thigh. The leg will most likely shorten as the muscles spasm and contract, generating extreme pain. Application of a traction splint to the affected leg, provided there are no other injuries in that leg, provides both pain relief and immobilization of the leg. Other treatment should include establishment of at least 1 large-bore intravenous line to treat or prevent shock. Analgesics are recommended especially if the traction splint has not fully addressed the pain.
Most of these disorders are more chronic in nature rather than acute and are seldom seen in the field. In addition, they may not require aggressive treatment from the paramedic. Unless otherwise indicated, treatment for patients with the following ailments includes ruling out acute trauma and making the patient comfortable for transport to the hospital of their choice.
Strictly speaking, arthritis is an inflammation of any joint, which, over time, will result in destruction to the joint. This will cause significant chronic pain for the patient. Osteoarthritis is believed to be from general wear and tear of the joint that occurs with aging. Rheumatoid arthritis is an autoimmune disease where the body’s defenses attack the joints, leading to swelling and damage. Rheumatoid arthritis can occur at any age. Finally, gout is a form of arthritis that results from the body’s inability to eliminate uric acid. Uric acid salts crystallize in the joints, which can cause chronic pain that increases across time. Patients with gout will be on a medication called allopurinol, which is commonly used as a diuretic to help the kidneys remove uric acid more efficiently.
Spinal stenosis is a narrowing of the spinal canal. It is a chronic condition that worsens across time. Eventually, it will cause back pain that leads to numbness inferior to the level of the stenosis. The stenosis is not typically throughout the spine but rather at 1 or only a couple locations.
Long-term repetitive motions will lead to inflammation and pain in the affected area. Tendinitis results when 1 or more of the tendons in a joint become inflamed. Bursitis is inflammation of the bursa sac present in the joint that cushions the joint. Inflammation of the carpal tendon in the hand leads to the most common form of overuse syndrome, called carpal tunnel syndrome. The inflammation of the tendon located at the proximal portion of the palm of the hand causes compression of the underlying median nerve and blood vessels. A patient with carpal tunnel syndrome will present with numbness and tingling of the lateral hand, the thumb, and the index and middle fingers.