11
Congenital infection
The term ‘congenital infection’ applies to infections acquired in utero (Fig. 11.1) whereas ‘neonatal infection’ is acquired shortly before or at delivery or postnatally (see Chapter 40).
Fig. 11.1 Congenital and neonatal infections. (CMV – cytomegalovirus; VZV – varicellazoster virus; HSV – herpes simplex virus; HPV – human papilloma virus; HTLV-1 – human T-cell leukemia virus 1.)
Most congenital infections are viral, but other significant causes include toxoplasmosis and (in terms of world-wide prevalence) syphilis.
Maternal infection is usually primary, i.e. it is a first infection, when there is lack of maternal immunity. Risk of infection from recurrent maternal infection (e.g. with CMV or HSV) is usually markedly lower than from a primary infection. Maternal infection may be asymptomatic or associated with mild symptoms. Diagnoses may be made antenatally or postnatally (Table 11.1). The placenta may play an important role in diagnosing congenital infection.
Clinical features
Congenital infections may precipitate pregnancy loss or preterm delivery. The clinical features of the symptomatic infant are shown in Fig. 11.2.
Fig. 11.2 The symptomatic infant.
Congenital cytomegalovirus (CMV) infection
- Commonest congenital infection in the US and UK (0.5–1/1000 live births).
- 1–2% of mothers seroconvert during pregnancy.
- Overall mother-to-infant transmission rate is 40%.
- May be reactivated during pregnancy
- May be transmitted postnatally in breast milk or blood transfusions.
Infected infants
- 5–10% severely affected (Fig. 11.2). Poor prognosis for abnormalities detectable on prenatal ultrasound/in utero MRI. These include significant intrauterine growth restriction (IUGR), central nervous system abnormalities (including ventriculomegaly), renal abnormality and oligohydramnios. In infants, on postnatal CT or MRI scan, they include microcephaly and periventricular calcification (Fig. 11.4),
- 80–90% asymptomatic at birth, but 10–15% of them are at risk of sensorineural hearing loss.
- Most common infectious cause of sensorineural hearing loss.

Fig. 11.3 Blueberry muffin rash in rubella and sometimes CMV.
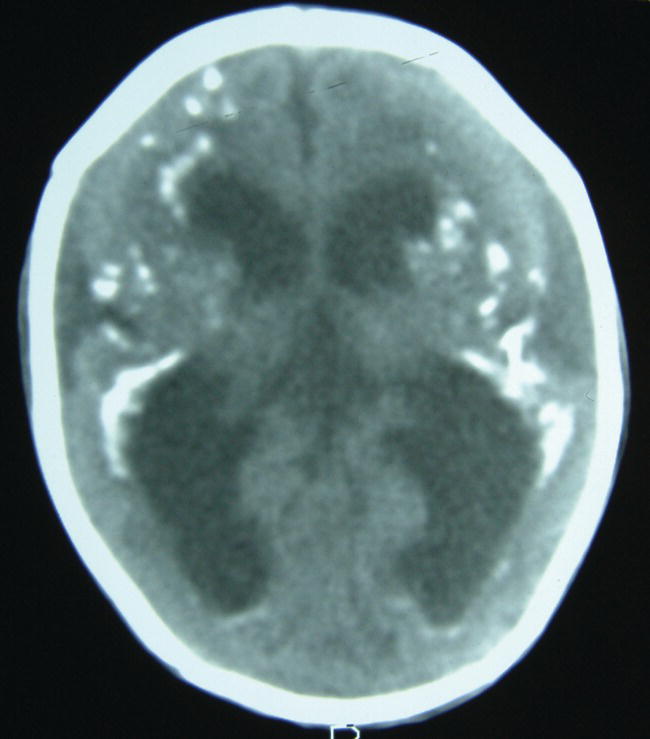
Fig. 11.4 Postnatal CT scan of the brain showing intracranial calcification from congenital CMV infection. The calcification may be identified on antenatal ultrasound.
Diagnosis
- Viral DNA (by PCR amplification) from amniotic fluid, fetal blood, or infant’s blood, urine, CSF or saliva collected at less than 3 weeks of age.
Treatment
For infants with CNS involvement, antiviral therapy with oral valganciclovir for 6 months has been shown to improve hearing and neuroevelopmental outcome in a randomized controlled trial.
Other points
- No vaccine yet for seronegative mothers.
- Infected infants may excrete CMV in urine for many months.
- All infected infants should be followed regularly for late-onset sensorineural hearing loss until school age.
Congenital toxoplasmosis
- Usually after primary maternal infection in pregnancy.
- Seronegative mothers are most at risk from poorly cooked meat. Small risk from handling feces of recently infected cats or ingesting contaminated soil from unwashed vegetables.
- The transmission rate and treatment are shown in Table 11.2 though this is controversial. The earlier in pregnancy the mother is infected the more severely the fetus is affected.
- The clinical features of the symptomatic infant are shown in Fig. 11.2. Subclinical disease includes retinitis (Fig. 11.5), epilepsy and learning difficulties.
- Treatment of infants with congenital infection – pyrimethamine and sulfadiazine plus folinic acid for prolonged duration.
Table 11.2 Transmission rate and treatment of toxoplasmosis.
| Trimester | |||
| Transmission | rate (%) | Clinical features | Treatment |
| First | 15 | 35% die before birth, 40% severely affected | Preventative – maternal spiramycin if <18 weeks |
| Second | 40 | 90% subclinical disease at birth; clinical manifestations may present years later | If severely affected – with antibiotics (pyrimethamine and sulfadiazine) and folinic acid |

Fig. 11.5 Retinitis from toxoplasmosis. This may present many years later.
Rubella
- Prevented by maternal vaccination. Now very rare in immunized populations.
- The earlier in pregnancy the mother is infected the more severely the fetus is affected.
- Clinical features are shown in Fig. 11.2.
- There is no effective treatment.
Congenital syphilis
In the US, a marked increase in incidence occurred in the 1980s, especially among drug users, but it has since declined. In the UK it is extremely rare. Antenatal screening on maternal blood is performed routinely. If active infection is diagnosed or suspected, the mother should be treated. Treatment more than 4 weeks before delivery prevents congenital infection.
- Transmission rate during primary infection in pregnancy is 100%.
- Without treatment there is 40% abortion/stillbirth/perinatal death.
- Prenatally, is associated with severe IUGR in developing countries.
- Clinical features are shown in Fig. 11.2. Those specific to congenital syphilis include a characteristic rash and desquamation on the soles of the feet (Fig. 11.6) and hands (Fig. 11.7) and bone lesions (Fig. 11.8).
- Treatment antenatally and/or postnatally is with penicillin. Effectiveness of treatment is monitored serologically.
- If the mother has not received adequate treatment or if there is physical, laboratory or radiographic evidence of disease, treat. If there is any doubt, treat directly.

Fig. 11.6 Characteristic rash and desquamation on the feet in congenital syphilis.
(Courtesy of Dr Hermione Lyall.)

Fig. 11.7 Characteristic rash and desquamation on hands in congenital syphilis.
(Courtesy of Dr Hermione Lyall.)

Fig. 11.8 X-rays in congenital syphilis showing bilateral metaphyseal lucency of the long bones and destruction of the medial proximal metaphysis of the left tibia.
Varicella: chickenpox, varicella zoster virus (VZV) infection
Primary maternal infection in pregnancy is uncommon as more than 90% of mothers are immune.
Early in pregnancy
- Intrauterine infection is rare (2% risk).
- Can lead to eye and CNS damage, skin scarring (Fig. 11.9) and limb hypoplasia.
- 1% risk of herpes zoster (shingles) in infancy.

Fig. 11.9 Skin scarring from maternal VZV infection early in pregnancy. This is rare.
Late in pregnancy
Infants born to mothers who develop chickenpox between 5 days before or 5 days after delivery should be given varicella zoster immune globulin (VZIG). This reduces but does not eliminate the risk of neonatal varicella zoster virus (VZV).
They should be closely monitored, and should be started on aciclovir (intravenous) if any signs of infection develop.
Parvovirus B19
- 50% of pregnant women are susceptible to infection.
- Transmission rate is 20–30%.
- In most cases there is a normal outcome of pregnancy but rarely infection in pregnancy leads to severe fetal anemia (aplastic anemia), causing hydrops fetalis (edema and ascites from heart failure). Anemia is associated with an abnormally elevated middle cerebral artery velocity on Doppler ultrasound. Can lead to intrauterine death, but if identified and treated by intrauterine transfusion prognosis is usually good.