52
Genital disorders
Features of the normal male genitalia are listed in Table 52.1. Most abnormalities arise from abnormal embryology (Fig. 52.1).
Table 52.1 Features of normal male genitalia at term.
| Length and diameter – normal size |
| Meatus – at tip |
| Testes – palpable in scrotum |
| Scrotum – rugae |

Fig. 52.1 (a) Embryology of testicular descent. The testis migrates from the posterior abdominal wall to the scrotum. It is preceded by a tongue of peritoneum, the processus vaginalis. This is obliterated in the normal infant (b). It remains widely patent in an inguinal hernia (c). With a hydrocele, it is patent but narrow (d).
Inguinal hernia
This results from the processus vaginalis remaining patent. Much more common in males than females and usually on the right side.
Common in preterm infants, particularly those with broncho-pulmonary dysplasia as they have weak muscles and increased intra-abdominal pressure.
Presents as a swelling in the groin or scrotum on crying (Fig. 52.2). It should be repaired promptly to avoid the risk of strangulation in both term and preterm infants, unless the anesthetic risk necessitates delaying the operation.

Fig. 52.2 Inguinal hernia in a newborn infant (arrow).
(Courtesy of Dr Mike Coren.)
If the hernia becomes irreducible, the lump is firm and tender, the infant vomits or becomes unwell, then an attempt should be made to reduce it after sustained gentle compression together with opioid analgesia. If possible, surgery is delayed for 24–48 hours to allow the edema to resolve. If reduction is unsuccessful, emergency surgery is required to avoid bowel strangulation and damage to the testis.
Hydrocele
This is fluid around the testis from a processus vaginalis that is wide enough to allow peritoneal fluid to flow down it but too narrow to form an inguinal hernia. Tense, transilluminates (Fig. 52.3). Often bilateral. Most resolve spontaneously.
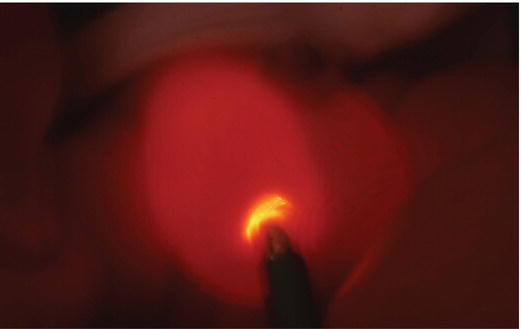
Fig. 52.3 Hydrocele on transillumination.
(Courtesy of Dr Mike Coren.)
Undescended testis
Failure of the testis to descend into the scrotum. Present in 5% of term male infants. Incidence is higher in preterm infants as testicular descent through the inguinal canal only occurs in the third trimester of pregnancy. Testicular descent may continue after birth; by 3 months of age only 1.5% are affected, but few descend thereafter.
Examination
With warm hands the contents of the inguinal canal are gently massaged towards the scrotum. If undescended, no testis is palpable in the scrotum, and the overlying scrotum is often poorly formed. The undescended testis may be palpable in the groin, but may sometimes be in the abdomen or outside the normal line of descent. A descended testis sometimes subsequently retracts upwards into the inguinal region (retractile testis).
Investigations
For bilateral undescended testes, pelvic ultrasound and karyotype may be needed to establish the infant’s gender, i.e. male and not a virilized female. The presence of testicular tissue can be confirmed by detecting testosterone production after hormonal stimulation. Sometimes laparoscopy is required to locate the testis.
Management
Surgery to place the testis in the scrotum (orchidopexy) is performed soon after 6 months of age, definitely by 2 years because:
- fertility is optimized – the testis needs to be in the scrotum to be below body temperature
- malignancy – increased risk, which for a unilateral undescended testis is reduced to nearly the same as a normal testis
- it is cosmetic and avoids psychologic upset.
Torsion of the testis
There is interruption of the blood supply to the testis and epididymis. The testis and surrounding area may be inflamed and the scrotum is dark red or black. Must be differentiated from a strangulated hernia and scrotal hematoma. Doppler ultrasound of testicular blood supply is helpful to determine testicular viability. Torsion must be relieved promptly for testis to remain viable. Occasionally present at birth, when testis is seldom viable.
Hypospadias
Common, affecting 1 in 300 boys. In the fetus, the urethra is created by flat tissue folding over from the perineum towards the tip. If this is not completed, the meatal opening may not reach the normal site at the tip of the penis (Fig. 52.4).
Fig. 52.4 Classification of hypospadias.
In hypospadias there is:
- a ventral urethral meatus – usually on the glans of the penis, but can be on the shaft or perineum (Fig. 52.5)
- a hooded foreskin – from failure to fuse
- chordee – tethering resulting in ventral curvature of the penis, most obvious on erection. This is associated with the more severe forms.
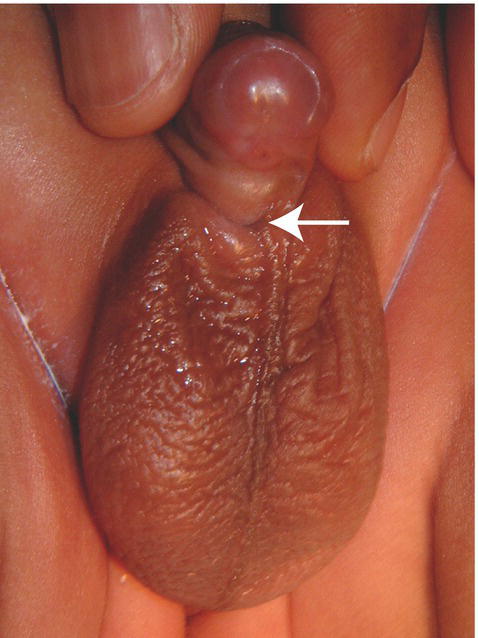
Fig. 52.5 Hypospadias. The arrow shows the urethral meatus.
Surgical correction is performed by 18 months of age so that the urethral meatus is at the tip of the penis, erection is straight and the penis looks normal. In most cases of hypospadias affecting only the glans, surgery is not required, except sometimes for cosmetic reasons.
Circumcision
At birth, the foreskin adheres to the surface of the glans penis. These adhesions subsequently separate, allowing the foreskin to become retractile. The foreskin cannot be retracted in 50% of boys at 1 year of age and in 10% at 4 years, but in only 1% by 16 years.
The advantages and disadvantages of circumcision are controversial and emotive.
Advantages are:
- hygiene – easier to keep clean
- prevents possibility of pathologic phimosis (scarring) or recurrent balanitis (infection) requiring circumcision when older
- slightly reduced incidence of urinary tract infection
- reduced risk of heterosexual HIV transmission as adults.
However, it is not a trivial operation, as healing can take up to 10 days. Complications of neonatal circumcision include:
- pain during and after the operation – adequate analgesia should be provided
- bleeding, infection, damage to glans penis, but this is uncommon.
In the US, circumcision is widely performed. In the UK, the main indication is religious, among Jews and Muslims. In countries in Sub-Saharan Africa with high HIV prevalence, the WHO recommends consideration as a component of HIV prevention.