74
Transport of the sick newborn infant
The need for neonatal transport is increasing with centralization of specialist services. Infants must be moved to the right place, by the right team, by the right mode of transport.
Infrastructure
- Specialized trained teams.
- Dedicated equipment (Fig. 74.1).
- A ‘transport hotline’ – providing efficient referral process, advice and bed locator (if available).
- Contracts and protocols for transport – ambulance, helicopter, fixed-wing airplane.
- Insurance liabilities to cover adverse events.
- Outreach training for less specialized units.
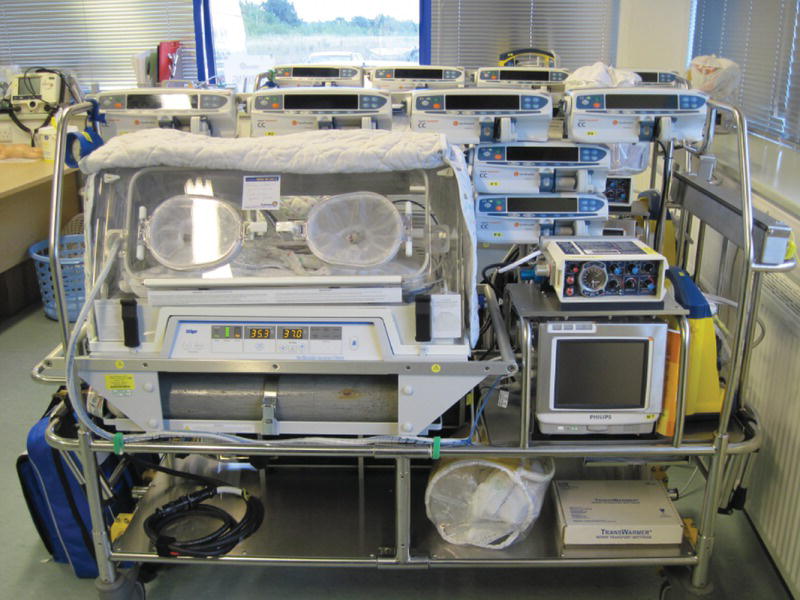
Fig. 74.1 Dedicated, specialized equipment.
Why transfer?
- Uplift in care level, e.g. extreme prematurity, unstable term infants.
- For subspecialty care – cardiology, surgery, etc.
- Transport back to referral hospital after specialist care.
Equipment
- Transport incubator or lightweight Baby Pod.
- Airways – mask, oro- and nasopharyngeal tracheal tubes.
- Respiratory support – ventilator, CPAP, air, oxygen, nitric oxide.
- Full ICU monitoring.
- IV access – cannulae, syringes, infusion pumps.
- Hand-held blood testing – glucose, electrolytes, hemoglobin, blood gases.
- Power source – available in ambulance, aircraft or hospital. Battery for transfers between power supply.
Equipment is heavy – needs handling skills and special equipment to assist.
Documentation
- Use standardized clinical assessment and treatment records.
- Necessary for debriefing, audit, legal records.
The ACCEPT principle is a comprehensive system to ensure that all aspects of the transfer process are managed optimally:
A – Assessment
- Determine the appropriate destination for the identified specialist care needs.
C – Taking Control of the situation and Communication with all teams involved
These include transport team, receiving unit and subspecialists. Ideally done through central coordinating center using call conferencing facilities.
Initial communication:
- Record all clinical details necessary to plan the retrieval.
- Give appropriate advice for stabilization and ongoing care:
- – ensure that vital signs, laboratory tests and blood gases are up-to-date and appropriate
- – request respiratory support, vascular access, infection treatment, specialist care for cardiac or surgery to be initiated if necessary.
- Ask referring hospital to prepare:
- – full documentation of pregnancy, birth and postnatal course; radiographs; laboratory results; vitamin K status
- – names of baby and parents and contact details
- – maternal blood for cross-match.
- Record exact location of patient, city, hospital, ward.
- Estimate arrival time and inform referring hospital.
- Provide ongoing contact number for clinical advice from specialist if needed.
E – Evaluation of the infant to be moved.
On arrival of transport team:
- Ensure detailed handover of patient’s condition.
- Review current treatment and management.
Before transport, the infant should have:
- normal temperature (except during therapeutic hypothermia)
- secure airway and breathing
- IV access – two lines preferably if critically ill
- gavage (naso-/orogastric) tube
- optimized blood pressure, circulation, urine output – consider arterial access
- optimized blood results – glucose, electrolytes, complete blood count (CBC), blood gases, etc.
- immediate treatment given, e.g. antibiotics, transfusion, prostaglandin (Prostin), anticonvulsants as appropriate.
- further specialized treatment started if required, e.g. active or passive cooling.
P – Preparation by transport team
Prepare emergency medications, including fluid boluses, and emergency equipment, e.g. airways, endotracheal tubes. IV lines that may be needed en route.
P – Packaging
- The infant’s clinical status needs to be rechecked after transfer to the transport incubator, ensuring that all transport equipment is functioning, i.e. ventilator, monitors, infusion pumps.
- Check that all lines, endotracheal tubes, catheters, etc. are secure.
- Make baby as comfortable as possible.
- Secure infant in the transport incubator with harnesses. The incubator, monitors and infusion pumps must be well secured to the transport trolley.
T – Transfer
- Transport trolley must be secured in ambulance (Fig. 74.2).
- Continuous monitoring, record vital signs regularly as in ICU.
- Avoid all unnecessary interventions.

Fig. 74.2 Securing trolley in ambulance.
On arrival at receiving hospital:
- Hand over to receiving staff.
- Ensure stable transfer to ICU monitoring and therapy.
- Complete documentation.

Fig. 74.3 Helicopter transfer in Northern Canada.

Fig. 74.4 Long distance repatriation of twins by fixed wing airplane.