77
Umbilical catheters and intraosseous cannulation
Umbilical catheters
Umbilical artery catheter (UAC)
Indications
- Continuous measurement of arterial blood pressure.
- Frequent blood gases or other blood samples.
- Exchange transfusion – to remove blood.
Contraindications
- Vascular compromise in the lower extremities or gluteal area.
- Necrotizing enterocolitis, peritonitis.
- Omphalitis (infection of the umbilical cord).
- Omphalocele.
Insertion (see video: Umbilical catheter insertion (arterial and venous))
Easiest on first day, possible within first 3–4 days.
- Wear gown, mask and sterile gloves, prepare sterile field.
- Prime catheter with saline.
- Clean the umbilicus and skin with chlorhexidine 2%/70% isopropyl alcohol swabs (ensure no pooling under baby).
- Place nylon tape around the base to control bleeding, then cut umbilical cord 1–2 cm from skin.
- Identify artery (Fig. 77.1). Dilate the artery with fine forceps or a dilator.
- Insert gently a 3 or 4.5 French gauge catheter to predetermined length (Table 77.1). There is gentle resistance from the muscular wall of the artery. Check that blood can be withdrawn (Fig. 77.2).
- Secure catheter (Fig. 77.2).
- Check position with X-ray (Figs 77.3 and 77.4) or ultrasound.
- Flush with heparinized saline.
- Label line as arterial or use red three-way tap.
Fig. 77.1 Two arteries and one vein in umbilicus. The arteries are small, circular and have a muscular wall; the vein is larger, thin-walled and irregular.
Table 77.1 Formula to calculate length of umbilical lines.
| Type of line | Length (cm) – add on the length of the umbilical stump |
| Umbilical artery catheter (UAC) (high position) | 3 × weight (kg) + 9 cm |
| Umbilical vein catheter (UVC) | Half the UAC length + 1 cm |
Fig. 77.2 Insertion and fixation of umbilical artery catheter. Transverse cutting of cord as shown here or cut down onto artery. Dilate with fine forceps or dilator. Magnification may be helpful. The umbilical cord is tied to a strip of tape to avoid tape on the skin. In some units, tape is placed in an H-shape on the abdominal wall and incorporates the catheter and thread suture from the cord.
Fig. 77.3 Position of catheters. For an arterial catheter (red), the high position (T6–10) is above the diaphragm, avoiding the celiac axis (T12), superior mesenteric artery (T12–L1) and renal arteries. This is the ideal position with less vascular complications. The low position (L3–4) is below the inferior mesenteric artery but above the aortic bifurcation. IVC, inferior vena cava. The position of the venous catheter is shown in blue.
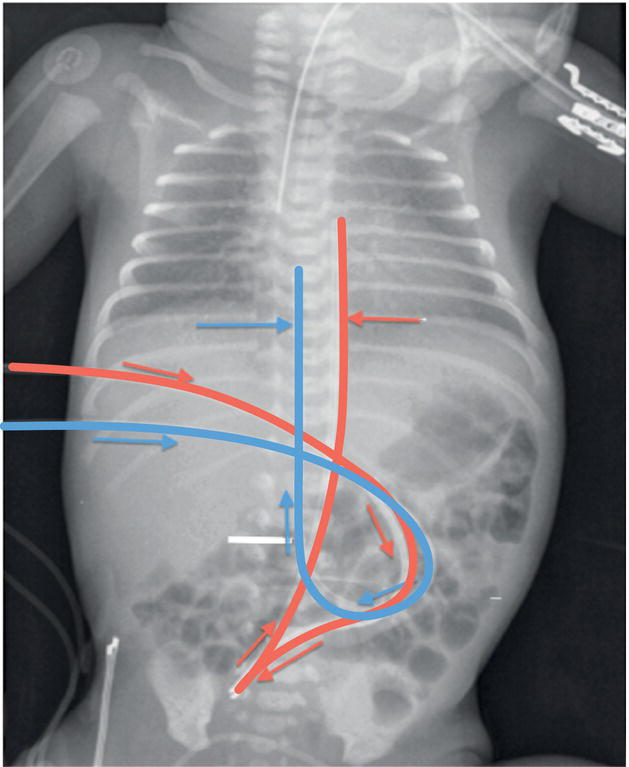
Fig. 77.4 X-ray to confirm position of the umbilical artery (red) and umbilical vein (blue) catheters, which need to be withdrawn. The artery first goes towards the groin before going towards the head just to the left of the vertebral column. Also check position of tracheal tube (satisfactory) and gavage (nasogastric) tube (missing).
Complications
- False track by catheter.
- Poor perfusion of lower limbs. If ischemic immediately REMOVE catheter.
- Blood loss if line disconnects.
- Aortic thrombosis and emboli.
- Infection (remove line as soon as no longer needed).
- Anemia from repeated excess blood volume sampling.
Umbilical vein catheter (UVC)
Indications
- Resuscitation – for urgent venous access.
- Inotropes.
- Parenteral nutrition.
- Exchange transfusion.
Contraindications
- Omphalitis.
- Omphalocele (exomphalos).
- Peritonitis.
Insertion
- Insert umbilical arterial catheter first if also required.
- Prepare sterile field and clean stump as for UAC.
- Select single- or double-lumen catheter.
- UVC can sometimes be inserted several days after birth.
- Prime catheter with saline and insert to required length (see Table 77.1).
- Check position with X-ray (Fig. 77.4) or ultrasound. Tip should lie in the inferior vena cava 1 cm below the diaphragm.
- Label clearly that it is a venous line.
Complications
- Thrombosis or emboli.
- Extravasation of fluid (e.g. PN) into liver.
- Infection.
- Pleural or pericardial effusion (if in right atrium).
- Remove as soon as no longer essential.
Intraosseous cannulation
Indication
- Emergency infusion of fluids and drugs when no venous access possible.
Preparation
- Clean the skin and prepare sterile field.
- Position infant with knee flexed and supported.
Insertion
- Proximal tibia 1–3 cm below tibial tuberosity – medial flat surface (Fig. 77.5).
- Use neonatal intraosseous needle.
- Insert needle at 10–15° from vertical towards foot (avoids growth plate).
- Use twisting motion or use drill device.
- Place dressing around base to secure needle.
- Aspirate marrow to confirm position.
- Infuse drugs using syringe.
Fig. 77.5 Intraosseous infusion into tibia.
Complications
- Fracture.
- Extravasation causing cellulitis.
- Osteomyelitis.