78
Central venous catheters and exchange transfusions
Central venous catheters (CVC)
In neonatal practice, central catheters are usually peripherally inserted, but sometimes a surgically placed subclavian or internal jugular catheter is required for long-term management, or if venous access is very difficult.
Peripherally inserted central catheters (PICC lines)
Indications
- Parenteral nutrition.
- Inotropes (due to vasoconstriction).
- Hyperosmolar infusions, e.g. glucose >12.5%.
- Prolonged administration of antibiotics.
Site
- Common veins – brachial, saphenous, sometimes scalp.
Insertion (Figs 78.1–78.3)
- Prepare infant – optimize position, minimize discomfort (see Chapter 63), temperature control, monitoring.
- Measure length of insertion from cannulation site to inferior or superior vena cava as appropriate.
- Prepare equipment – gauze, polyurethane catheter, cannula or needle for insertion, T-piece and connection, dressing, saline flush.
- Sterile procedure – wear gown and mask and two sets of gloves – remove outer gloves once the area is cleaned and sterile.
Quality improvement care bundles to reduce central line-associated bloodstream infection (CLABSI) have markedly reduced late-onset sepsis rates. Achieved through practical training and improving procedures to optimize infection control, root cause analysis of positive blood cultures, feedback and use of results to further improve guidelines.
Fig. 78.1 An example of placing a peripherally inserted central catheter (PICC line). Needle is inserted into vein. The central line is threaded through the cannula. Non-toothed forceps may be used.
Fig. 78.2 The cannula is removed and then split, leaving the long line in place.
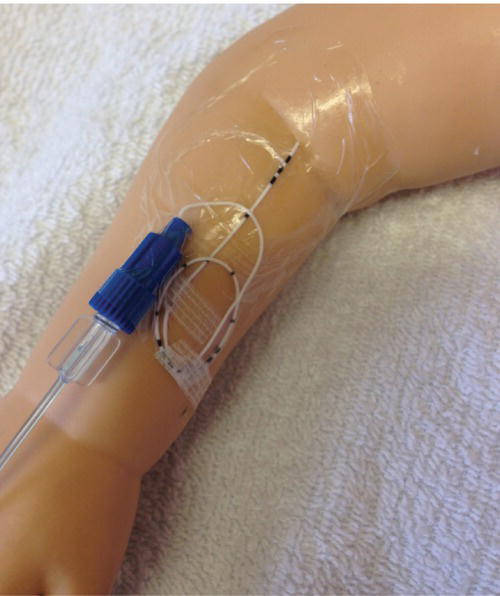
Fig. 78.3 Securing the line using sterile strips followed by clear adhesive dressing, incorporating loops of the central line. Ensure that insertion site is visible, that the infant is comfortable and that the dressing is not constricting the line or arm.
Line tip position and management
- Ideal position of the tip is in the inferior or superior vena cava outside the right atrium.
- Position of the long line should be checked by X-ray or ultrasound (Fig. 78.4) to ensure it is not in the right atrium. If position in doubt, inject sterile intravenous contrast and X-ray.
- If line inserted in upper arm, perform X-ray with arm abducted.
- If line inserted in lower limb, ensure it has passed superior to the lumbar venous plexus.
- Line management – usually last several weeks. They must be handled aseptically.
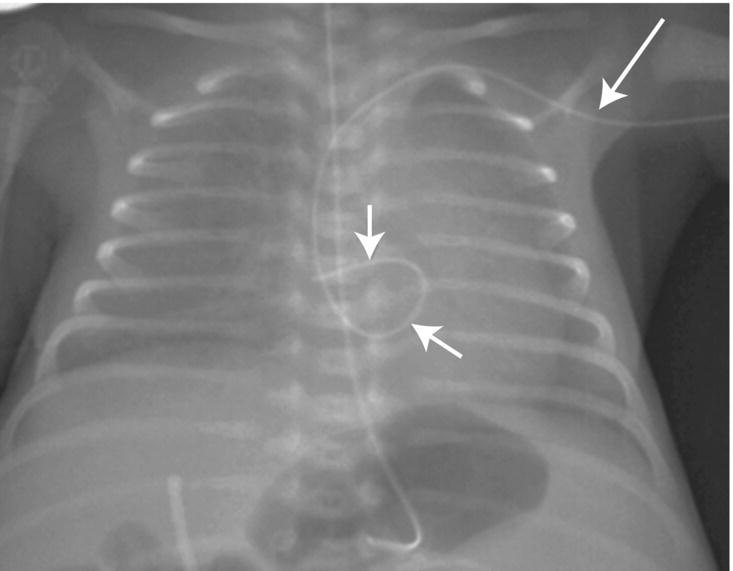
Fig. 78.4 X-ray demonstrating the importance of confirming catheter position. Central line may be radiopaque or need contrast flushed into it. The central venous catheter inserted into a vein in the left arm (arrow) is in the right atrium (arrows) and must be withdrawn.
Complications
- Infection.
- Thrombus and emboli.
- Extravasation – pleural effusion, pericardial effusion (tamponade), tissue edema.
- Superior vena caval obstruction.
- Blockage.
- Leakage at connection sites.
- Line breaking off on removal.
Surgically tunneled subclavian or jugular line
Indications
- Long-term central access.
- Peripheral insertion not successful.
Insertion
- Usually by a pediatric surgeon or interventional radiologist under general anesthetic in operating theater.
- Tunneled under skin.
- Tip position in superior vena cava.
Complications
- Pneumothorax.
- Surgical scar.
- Superior vena caval obstruction.
- Blockage or extravasation.
- Infection.
Exchange transfusion
Indications
- Severe hyperbilirubinemia – exchange with fresh blood, 2 × blood volume (i.e. 2 × 90 mL/kg).
- Severe polycythemia (hematocrit >0.75 or symptomatic) – exchange with normal saline to reduce hematocrit to 0.55 (usually ~ 20 mL/kg).
Exchange transfusion is performed infrequently for hyperbilirubinemia since the introduction of routine anti-D antibody to rhesus-negative mothers, better phototherapy and intravenous immunoglobulin for severe jaundice.
Technique (see video: Haemolytic disease of the newborn)
- Use fresh, CMV-negative, irradiated, whole blood or plasma reduced red cells (not packed red cells), ideally with hematocrit 0.5–0.6.
- Prepare sterile field. Ensure operator will not be disturbed during procedure.
Blood withdrawn via umbilical or peripheral arterial line; infused via umbilical or peripheral vein
- Infuse blood at a constant rate through the vein via a blood warmer.
- Withdraw blood from arterial line in aliquots (5 mL extremely preterm, 20 mL term).
Via umbilical venous catheter (Fig. 78.5)
- Alternate between withdrawing and infusing aliquots (5–20 mL) of blood. Use a closed system, designed for exchange transfusion, to reduce the risk of error.
Fig. 78.5 An example of exchange transfusion via umbilical vein with 10 ml aliquots. 1. Withdraw 10 mL of baby’s blood into syringe. 2. Inject baby’s blood into waste bag. 3. Draw 10 mL of donor blood into syringe. 4. Inject 10 mL of blood into baby. Repeat to replace calculated blood volume.
Monitoring
- Heart rate, blood pressure, temperature throughout.
- Volume infused and withdrawn (separate observer).
- Glucose, electrolytes, calcium, acid–base.
- Allow time for equilibration – perform over several hours for double volume exchange.
- No feeds during procedure.
Complications
- Technical problems (e.g. loss of access).
- Air embolization or thrombosis.
- Volume overload or depletion.
- Electrolyte imbalance – hyperkalemia, hypocalcemia, acidosis or alkalosis.
- Hypoglycemia.
- Infection.
- Hypothermia.
- Mortality – possibly up to 1%.