
We established earlier that you could die of starvation within weeks and within days from dehydration. Now let’s talk about the things that can kill you in minutes. Disasters cause injuries. It’s a fact of life. In normal times our medical system can perform miracles. The survival rate of gunshot wounds is upwards of 98 percent if the victim makes it to a trauma doctor in time. Unfortunately, in a disaster those hospitals and doctors may be unavailable or overwhelmed. You may have to deal with injuries that you would normally go to the emergency room for.
The thing to know about medicine is that an untrained person can allow damage to get worse by not acting, but a semi-trained individual can DO a lot of damage by acting outside of their training. Medicinal knowledge is not learned through reading or through watching YouTube. This is an area that you need to get training from a qualified source. Luckily, it is inexpensive to get basic first aid training. A basic first aid and community CPR class can be taken in a day. You can get more advanced first responder training in a week. The classes are available if you know where to look.
That being said, no book on basic preparedness would be complete if it did not cover basic first aid.
First aid involves immediate action to reduce the severity of an injury or to provide lifesaving assistance to stabilize a patient until more advanced medical care is available.
An example of reducing the severity of an injury is applying ice and immobilization to a sprain so it does not swell or become further damaged. A splint on a broken bone is another example.
Lifesaving assistance may be cardiopulmonary resuscitation (CPR) on a heart attack victim, or applying a direct pressure bandage on someone with a severely bleeding wound.
As with most other aspects of basic preparedness, first aid can be summarized as fixing what is important now. First aid training focuses on the ABC’s: airway, breathing, and circulation. If compromised, the ABC’s will kill a person the fastest.
A blocked airway prevents oxygen from entering the lungs. A blocked airway will cause death in minutes. It is also easy to diagnose, so like our earlier planning discussion on threat likelihood and impact, airway issues are covered in all basic first aid courses and should be dealt with first.
Unconscious Patients
With an unconscious patient, the priority is clearing the airway of obstruction and keeping it clear. Common problems with the airway of unconscious patients are blockage of the pharynx by the tongue, a foreign body, or vomit.
Most often this is done by manually positioning the unconscious person. The most commonly taught technique is the “head tilt, chin lift” method, although other methods such as the “modified jaw thrust” can be used, especially where spinal injury is suspected.
Head Tilt, Chin Lift
This technique is used to open the airway of an unconscious patient. It is practiced by tilting the head backwards. Apply pressure to the forehead while simultaneously lifting the chin. The maneuver is used on any patient where cervical spine injury is not a concern and is taught on most first aid courses as the standard way of clearing an airway.

Head Tilt, Chin Lift.
BruceBlaus via Wikimedia Commons.
The jaw thrust method is an alternative to the head tilt, chin lift technique. It is used when spinal damage is suspected, if the patient is wearing a cervical collar, or is restrained on a long spine board.
The maneuver is used on a patient lying on their back and is performed by placing the index and middle fingers to physically push the rear of the jaw up while the rescuer’s thumbs push down on the chin to open the mouth. When the jaw is moved forward, it pulls the tongue forward and prevents it from obstructing the entrance to the throat.
Recovery Position
An unconscious, but breathing, patient can be placed in the recovery position to prevent suffocation through obstruction of the airway. This prevents suffocation by foreign objects and prevents the tongue from falling back and blocking the throat. It also prevents liquid suffocation by items such as vomit or blood. Vomiting (known medically as emesis) in unconscious patients is a common cause of death and it is often (but not exclusively) found in victims of drug or alcohol overdose.

Recovery Position.
Photo courtesy of iStock.com/Highwaystarz Photography.
In conscious patients, choking often causes airway blockage and they will often signal using the universal sign for choking. You may also see other signs like gasping, the inability to speak or cough, and a blue tinge around the lips.
Abdominal Thrusts (Heimlich Maneuver)
In this maneuver, a rescuer stands behind a patient and uses his hands to press sharply inward and upward right under the ribcage in order to exert pressure on the diaphragm. This abdominal thrusting compresses the lungs and exerts pressure on any object lodged in the throat and hopefully will expel the object.
Most first aid certification groups teach a tiered approach to the abdominal thrust method and alternate thrusts with back blows and show how to transition from abdominal thrusts on a conscious victim to rendering aid on an unconscious patient.

Universal sign for choking.
Photo courtesy of iStock.com/zegers06.

Heimlich maneuver.
Photo courtesy of iStock.com/clearstockconcepts.
Breathing
Once the airway is open attention needs to be given to find out if the victim is breathing normally. Most people take between twelve and twenty breaths a minute.
If a patient is unconscious and the airway is clear, but they are not breathing, then CPR is likely to be needed if you are trained.
If the patient is conscious but not breathing, they will most likely become unconscious very soon. Look for things such as asthma or trauma to help diagnose the issue, but treatment and diagnosis of conditions like pulmonary edema (fluid causing pressure on the lungs) or hemothorax (penetrating wound in the chest which causes a buildup of blood to place pressure on the lungs). These conditions are beyond the scope of first aid and should be prepared for by taking a first responder medical course or other more advanced training.
Circulation
Once air is entering the blood and is placed into the blood by the lungs, the oxygen-rich blood must be able to circulate throughout the body. The most common way to check for this is to feel for a carotid pulse.

Checking for a carotid pulse.
By Rama via Wikimedia Commons.
Checking a Carotid Pulse
To check your pulse over the patient’s carotid artery, place your index and middle fingers on your neck to the side of your windpipe. Do not use your thumb because it has a detectible pulse and you may get your heartbeat confused with your patient’s.
When you feel your pulse, look at your watch and count the number of beats in six seconds and multiply that by ten to get beats per minute.
If the patient does not have a pulse, then they have no circulation as their heart is not pumping blood. CPR is needed at that point.
Cardiopulmonary Resuscitation (CPR)
There are several organizations that provide inexpensive training and certification in CPR. The American Red Cross and the American Heart Association are the two most common. I have held certification from both, and find them to be very similar. Any person that wants to increase their preparedness level should seek out certification as the likelihood of needing to know CPR is much higher than having to deal with rogue asteroids, zombies, or other types of disasters.
For illustrative purposes, the basics of CPR are as follows:
Call
Check the victim for unresponsiveness as you don’t want to call an ambulance or perform CPR on someone sleeping. A simple shake and a loud “Hey! Are you okay?” works well. If the patient is not responsive and not breathing normally, have someone call 911. In most locations, the emergency dispatcher can assist you with verbal CPR instructions if necessary.
Pump
If your patient is not breathing normally, coughing, or moving, you can cause the heart to pump by performing chest compressions. Push down hard and fast on the center of the chest thirty times. Your compressions should be faster than one per second so that you work at a rate of 100–120 compressions per minute. The chest should compress between two and two-and-a-half inches.

Everyone should be CPR Certified.
US Army Corps of Engineers Sacramento District via Wikimedia Commons.

Once you are sure the scene is safe, check the victim for responsiveness.
Photo courtesy of iStock.com/JanekWD.

Chest compressions.
By Rama via Wikimedia Commons.
Blow
After thirty compressions, tilt the head back and lift the chin. Pinch their nose shut and cover their mouth with yours and blow until you see the chest rise. Give two breaths. Each breath should take one full second. Watch to see if their chest rises as you blow.
You will learn different memorization tools in a certification class depending on the organization. The Red Cross uses Check, Call, Care, but the basic principles are the same.
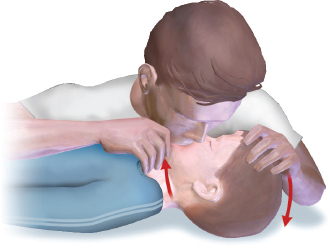
Rescue breathing.
By BruceBlaus via Wikimedia Commons.

Automatic External Defbrilators (AED) are becoming commonplace.
Photo courtesy of iStock.com/Jin_Youngin.
Defibrillation is becoming more common. The heart has a normal rhythm to its beat. This allows the heart to pump blood efficiently. When the heart goes into fibrillation, instead of having rhythmic electrical impulses activating heart muscles, chaotic electrical impulses cause the heart to shudder and not pump. A defibrillator identifies those chaotic pulses and then gives a calculated charge of electricity to shock the heart back into its normal rhythm. Studies show that rapid use of an Automatic External Defibrillator (AED) can save the lives of those in cardiac arrest 38 percent of the time.
Blood Loss
Circulation can also be impacted by trauma. If you have ever tried to blow up an inflatable toy with a hole in it you understand the problem. It does not matter if the heart and lungs are working perfectly if there is a wound that is draining blood from the system. This aspect of first aid is very important. As a matter of fact, in some instances, such as the military, dealing with extreme blood loss comes before dealing with the ABC’s as traumatic injuries such as a severed artery can kill a person before they would die of a stopped heart.
Direct Pressure
The main way to treat blood loss is with direct pressure. If you have to deal with a large open wound, take an absorbent bandage and place it directly over the wound. Put pressure on the bandage and hold it so that the dressing stops the bleeding. Once the bleeding slows, you can wrap gauze or other bandaging material around the injured body part and tie a square knot over the wound so that it holds the original dressing in place.
If the original bandage becomes soaked, do not remove it as doing so will damage any clotted blood and will restart the bleeding. Place a new bandage over the used dressing.
Tourniquet
A tourniquet is a constricting or compressing device made from a wide band, used to control otherwise uncontrollable blood loss to an extremity. A tourniquet is placed around an arm or leg just above the wound. As the band is tightened, it compresses the flesh of the limb and closes off all the blood vessels below the tourniquet.

Direct pressure.
By Mike6271 via Wikimedia Commons.

Commercial CAT tourniquet as developed for our military.
By INDNAM via Wikimedia Commons.
While this device is extremely effective at stopping extreme blood loss, it also prevents blood from flowing to any tissue below it. This can lead to tissue death and possible amputation. A combat application tourniquet is a common item in tram kits and IFAKs as it allows people to put a tourniquet on themselves if needed. A belt can make an improvised tourniquet.
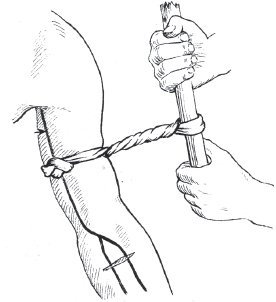
An improvised tourniquet.
By Pearson Scott Foresman via Wikimedia Commons.
Improvised Tourniquet
To make a tourniquet out of a belt or other thick strap, wrap the material around the limb and tie it loosely. Then insert a stick or small rod (screwdriver, etc.) between the strap and the body part. Twist the rod so that it bites into the tourniquet strap and tightens it around the limb. Once it is sufficiently tight enough to restrict blood flow, use a string or rope to tie the rod against the limb so it does not unravel.
No matter the type, note the time the tourniquet was applied. It is commonly taught to write the application time on the victim’s forehead using their blood.
Hemostatic Agents
Hemostatic agents are materials that stop bleeding. QuikClot is a common brand. These materials come in two common types for use in IFAKs, loose powder or impregnated in gauze bandage. Some of these agents, QuikClot for example, work chemically, while others such as ChitoSAM works biologically to bond with blood (similar to natural clotting). Earlier hemostatic agents gave off heat when used and caused burns, however, newer products such as Celox, QuickClot, and ChitoSAM do not do so.
Other Injuries
Burns
Heat is the most common cause of burn injuries, but chemicals, radiation, electricity, and excessive sunlight can also cause them. Burns are classified into degrees of seriousness, and are not only extremely painful, but can be deadly when deep or over a large portion of the body.
There Are Three Types of Burns
• First-degree burns damage only the outer layer of skin
• Second-degree burns damage the outer layer and the layer underneath
• Third-degree burns damage or destroy the deepest layer of skin and tissues underneath
• Fourth-degree burns are third-degree burns that penetrate to tendons and bone

First-degree burns are the least serious.
By Bejinhan vua Wikimedia Commons.
First-degree burns are often treated with home care soaking the wound in cool water for five minutes or more and taking an aspirin. Do not ice a first-degree burn as this can cause tissue damage.
Second-degree burns blister and are more serious. Use cool water for fifteen minutes or longer to ease pain, do not pop blisters, and do not use folk remedies such as spreading butter on the wound as it increases the risk of infection.
Third-degree burns require medical care. They don’t always hurt as the nerves can be destroyed. Scarring can occur.
Broken Bones
Broken bones are extremely painful and come in many forms, but these are the most common:
• Open fractures occur when a piece of bone punctures the skin and is exposed.
• Closed fractures remain inside the body and do not cause an open wound.

Second-degree burns come with blisters—this one was the result of a kitchen fire.
Photo by the author.

Third-degree burns require medical care.
By Craig0927 via Wikimedia Commons.
• Displaced breaks occur when the bone does not remain in place—this will show in a lump in the skin or displaced limb.
• Non-displaced breaks occur when the bone breaks but remains in place so that the bone fragments remain lined up.
Broken bones heal by themselves in time; most medical treatment involves ensuring the bone heals straight. First aid is limited to treating wounds caused by open fractures, and immobilization of the joints above and below the broken bone.
Do not try to realign or reset displaced fractures, or return open fractures beneath the skin without specialized training.
Cold Injuries
Cold injuries can be deadly; hypothermia is when heat loss is greater than the body’s ability to produce heat. Additionally, frostbite is the freezing of body parts. Hypothermia can be deadly, and frostbite can cause the death and eventual loss of fingers, toes, or any exposed body part.
To Prevent Hypothermia, the Army Developed the Acronym COLD
• Keep it Clean
• Avoid Overheating
• Wear it Loose and in Layers
• Keep it Dry

Improvised splinting.
Flickr: Joe Loong.
• Vigorous shivering
• Confusion
• Sleepiness
• Slurred speech
• Shallow breathing
• Weak pulse
• Low blood pressure
• Change in behavior
• Poor control over body movements/slow reactions.
First aid for hypothermia involves re-warming the body by exercise or body heat. Using external heat sources should only be attempted if the patient stops shivering and care is taken to prevent burns.
Frostbite is better prevented than treated. Wear gloves, and do not come in contact with liquids or bare metal. Take care during times of long-term exposure to the cold.
Re-warming of frostbitten extremities should be done slowly and should not be attempted if there is a possibility of refreezing.
Symptoms of Frostbite Include
• Numbness in affected area.
• Tingling, blistered, swollen, or tender areas.
• Pale, yellowish, waxy-looking skin (grayish in dark-skinned individuals).
• Frozen tissue that feels wooden to the touch.
• Significant pain after re-warming.

An example of frostbite.
By Dr. S. Falz via Wikimedia Commons.
Heat injuries are often overlooked, but can quickly cause death if not caught and treated.
The two main heat injuries are:
• Heat exhaustion, which can occur after exposure to high temperatures and is often accompanied by dehydration. It can be caused by water depletion or salt depletion.
• Heat stroke, a condition caused by body overheating, usually as a result of prolonged exposure to or physical exertion in high temperatures. This most serious form of heat injury, heat stroke can occur if your body temperature rises to 104 F. It can result in death if untreated.
Heat Exhaustion Symptoms
• Dizziness
• Headache
• Nausea
• Weakness
• Clumsy/unsteady walk
• Muscle cramps
Treatment for heat exhaustion is simple. You should move the patient to the shade, loosen their clothing, and have them sip water at the rate of two quarts an hour. If condition worsens, then more advanced treatment is necessary.
Heat Stroke Symptoms
• Profuse sweating
• Convulsions and chills
• Vomiting
• Confusion, mumbling—ask mental status check questions to see if brain is working correctly
• Combative
• Unconsciousness
If a person has heat stroke rapid cooling is essential. The faster the body is cooled, the less damage to the brain and organs occurs.
Remove all outer clothing, immerse in cold water or iced sheets, and fan the patient. Observe for changing mental status.
It can take months to recover from heat injuries. Once someone succumbs to heat exhaustion, they are more susceptible for months after the initial injury. Prevention is the key.
Impalement
Impalement occurs when an object penetrates the body and remains in place. It is something that cannot be treated by laymen, as removing an impaled object can cause more damage. Impaled objects have been known to sever and hold blood vessels closed. Removal can cause rapid death by blood loss.
Basic first aid is to stabilize the object without completely covering the object, control bleeding, and treat for shock.

Protect the object to keep it from moving.
Photo courtesy of Max Pixel, http://maxpixel.freegreatpicture.com.
Poisoning
Vomiting is no longer recommended for treatment of poisoning. It has not been shown to help, and can cause additional damage.

Keep the Poison Control number near your phone.
Photo by the author.
For swallowed poisons, recommended first aid is to remove any poison still in the mouth, read the poison’s label if available, and follow the guidance as you call for aid from emergency medical or Poison Control.
For poison in the eye or skin, remove any contaminated coverings and flush for twenty minutes under lukewarm water.
For inhaled poisons, quick removal to fresh air is the best aid possible by the layperson.
Seizure
There is a lot of misinformation about seizure treatment. The aid giver should never attempt to restrain someone having a seizure, nor should they attempt to place something in the person’s mouth. Aid should be limited to staying close by and removing objects in the area that could cause injury to the person.
Remain calm and understand that a seizure does not last longer than a few moments. Comfort the patient when the seizure stops and encourage onlookers to give the person space.
Stroke
Besides rapid diagnosis, there is not much a person can do to treat a stroke outside of a hospital. Rapid treatment by a medical professional is essential to preventing permanent brain loss.
Stroke Identification Can Be Done Using the Acronym FAST
• Face. Does the face droop on one side while trying to smile?
• Arms. Is one arm lower when trying to raise both arms?
• Speech. Can a simple sentence be repeated? Is speech slurred or strange?
• Time. During a stroke every minute counts. Get the patient to a hospital ASAP.
Other Signs of a Stroke
• Weakness or numbness on one side of the body
• Dimness or blurred vision
• Sudden severe headache
• Unexplained dizziness