Section 1: Preparatory
EMS Systems
Matching
|
1. Medical director 2. Paramedic 3. EMT 4. HIPAA 5. Patient advocacy 6. Online medical direction 7. Offline medical direction |
a. An individual who has extensive training in advanced life support, including endotracheal intubation, emergency pharmacology, cardiac monitoring, and advanced assessment and treatment skills. b. Federal legislation passed in 1996 that limits availability of patients’ health care information. c. The physician who authorizes or delegates to the EMT, the authority to provide medical care. d. Protection of patient rights. e. Individual who has training in basic life support, including AED, use of definitive airway adjuncts, and assisting patients with certain medications. f. Physician instructions given directly over the phone or radio. g. Protocols/standing orders. |
1. Medical director: (c) The physician who authorizes or delegates to the EMT, the authority to provide medical care.
2. Paramedic: (a) An individual who has extensive training in advanced life support, including endotracheal intubation, emergency pharmacology, cardiac monitoring, and advanced assessment and treatment skills.
3. EMT: (e) Individual who has training in basic life support, including AED, use of definitive airway adjuncts, and assisting patients with certain medications.
4. HIPAA: (b) Federal legislation passed in 1996 that limits availability of patients’ health care information.
5. Patient advocacy: (d) Protection of patient rights.
6. Online medical direction: (f) Physician instructions given directly over the phone or radio.
7. Offline medical direction: (g) Protocols/standing orders.
Quality improvement (QI) is a system of internal/external reviews and audits of all aspects of an EMS system. QI is important to an EMS system to identify aspects needing improvement; this ensures that the public receives the highest quality of prehospital care. List the roles EMTs play in QI.
• Neat, legible, and accurate documentation
• Attending continuing medical education (CME) that includes run review and call audits
• Gathering feedback from patients and hospital staff
• Conducting preventive maintenance
• Maintaining mastery of skills performance
Workforce Safety and Wellness
Matching
|
1. Posttraumatic stress disorder (PTSD) 2. Infection control 3. Bargaining 4. Denial 5. Acceptance 6. Depression 7. Anger |
a. (“Not me.”): Defense mechanism creating a buffer between shock of dying and dealing with the illness/injury. b. (“Why me?”): EMTs may be the target of aggression. c. (“OK, but first let me …”): Agreement that, in the patient’s mind, will postpone death for a short time. d. (“OK, I am not afraid.”): Does not mean the patient will be happy about dying. The family will usually require more support during this stage than the patient. e. (“OK, but I haven’t …”): Characterized by sadness and despair. The patient is usually silent and retreats into his own world. f. Delayed stress reaction. g. Procedures to reduce transmission of infection among patients and health care personnel. |
1. Posttraumatic stress disorder: (f) Delayed stress reaction.
2. Infection control: (g) Procedures to reduce transmission of infection among patients and health care personnel.
3. Bargaining: (c) (“OK, but first let me …”): Agreement that, in the patient’s mind, will postpone death for a short time.
4. Denial: (a) (“Not me.”): Defense mechanism creating a buffer between shock of dying and dealing with the illness/injury.
5. Acceptance: (d) (“OK, I am not afraid.”): Does not mean the patient will be happy about dying. The family will usually require more support during this stage than the patient.
6. Depression: (e) (“OK, but I haven’t …”): Characterized by sadness and despair. The patient is usually silent and retreats into his own world.
7. Anger: (b) (“Why me?”): EMTs may be the target of aggression.
Medical, Legal, and Ethical Issues
Matching
|
1. Abandonment 2. Duty to act 3. Expressed consent 4. Implied consent 5. Negligence 6. Standard of care 7. Scope of practice |
a. Care that an EMT is able to provide. b. Legal responsibility to provide care. c. Unilateral termination of care. d. Specific authorization to provide care expressed by the patient. e. Legal assumption that treatment was desired. f. Failure to provide the standard of care. g. Accepted level of care. |
1. Abandonment: (c) Unilateral termination of care.
2. Duty to act: (b) Legal responsibility to provide care.
3. Expressed consent: (d) Specific authorization to provide care expressed by the patient.
4. Implied consent: (e) Legal assumption that treatment was desired.
5. Negligence: (f) Failure to provide the standard of care.
6. Standard of care: (g) Accepted level of care.
7. Scope of practice: (a) Care that an EMT is able to provide.
Define abandonment.
Abandonment is leaving a patient, for whom you have an established duty to act, without the consent of the patient or arranging for transfer of patient care to another medical provider trained to the same level (or higher) as you. Once you have an established duty to act, you cannot leave, for any reason (short of protecting your own life), without that consent or transfer of patient care.
Define negligence.
Negligence is a failure to provide the level of care for which you are responsible. Four elements must have occurred for the legal determination of “negligence” to be reached:
1. There must have been a duty to act;
2. There must have been a breach of that duty, in whole or in part;
3. There must have been some injury or loss;
and
4. There must be a reasonable connection between the breach of duty and the injury or loss.
Define dependent lividity.
After a person has died and circulation stops, the blood begins to pool in the dependent areas (areas on the bottom part of the body in the position of death). This is called dependent lividity and starts within a few minutes after death, beginning in the extremities and progressing to the rest of the body.
Lividity appears as a discoloration, resembling a blotchy black-and-blue or reddish mark. As time passes, the discoloration becomes more widespread and pronounced. It is caused when red blood cells in the blood vessels settle down to the lower areas of the body. This color change is less striking in skin with dark pigmentation. Lividity is also called livor mortis.
Define rigor mortis.
Over the first few hours after death, chemical changes occur in the cells of the body. Muscle cells contract and stay contracted, causing a rigidity known as rigor mortis. This stiffening of the body begins with small muscles, including those of the fingers, neck, and jaw, and progresses to the extremities and pelvis.
As still more time passes (12 hours or longer), the protein in the muscles degrades, causing the stiffening to relax and the body to become limp.
Explain the reasons for withholding resuscitation.
You may withhold or stop resuscitation if any of the following are present:
• Injuries incompatible with life (decapitation)
• Advance directive (do not resuscitate, medical orders for life-sustaining treatment, etc.) stating resuscitation should be withheld
• Dependent lividity, rigor mortis
List some do not resuscitate (DNR) caveats.
• Do not resuscitate (DNR) means, for the patient in cardiac or respiratory arrest, no chest compressions, ventilation, defibrillation, endotracheal intubation, or medications.
• If the patient is not in cardiac or respiratory arrest, full treatment for all injuries, pain, difficult or insufficient breathing, hemorrhage, and/or other medical conditions must be provided.
• Relief of choking caused by a foreign body is usually appropriate, although if breathing has stopped, ventilation should not be assisted.
• Cardiopulmonary resuscitation (CPR) must be initiated if no out-of-hospital or facility DNR is presented. If a DNR order is presented after CPR has been started, stop CPR.
One of the EMT roles and responsibilities is patient advocacy. This means that, as the emergency care provider, the EMT is responsible for what?
Protecting the patient’s rights
Communications and Documentation
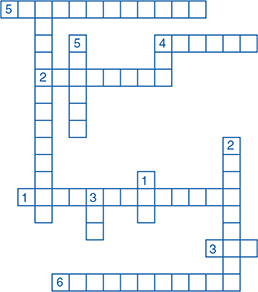
Across
1. Transmission of information to another person—verbally or through body language.
2. A base station that receives messages and signals on one frequency and automatically retransmits them on a second frequency.
3. Small computer terminals inside ambulances that directly receive data from the dispatch center.
4. The use of a radio signal and a voice or digital message transmitted to “beepers.”
5. Encouraging the patient to talk more or provide more information.
6. Type of question that allows the patient to answer in very short responses.
Down
1. Federal agency that has jurisdiction over interstate communications.
2. Type of question that allows the patient to answer in detail.
3. Radio frequencies between 300 and 3000 MHz.
4. A document that ensures continuity of patient care.
5. Ability to transmit and receive simultaneously.
Direct telephone or radio contact with a physician to obtain guidance in emergency care is called?
Online medical direction
The Human Body
Identify the 2 gases that are exchanged during breathing.
Oxygen (O2) and carbon dioxide (CO2)
The human body consists of how many bones?
There are 206 bones in the human body.
Describe the regulation of ventilation.
Although breathing can be altered voluntarily, it is primarily controlled involuntarily by the autonomic nervous system. A large part of the regulation is related to maintaining normal gas exchange and normal blood gas levels. Receptors within the body constantly measure the amount of oxygen (O2), carbon dioxide (CO2), and hydrogen ions (pH) and signal the brain to adjust the rate and depth of respiration. Centers responsible for ventilatory control are the chemoreceptors, lung receptors, and specialized centers in the brainstem.
What is the function of chemoreceptors?
Chemoreceptors are specialized receptors that monitor the number of hydrogen ions (pH), and the carbon dioxide and oxygen levels in the arterial blood. There are 2 different types of chemoreceptors: central and peripheral.
Define hypoxic drive.
A person’s ventilation is normally controlled by the strong stimulus provided by the amount of CO2 in the arterial blood. This is referred to as a hypercapnic drive or hypercarbic drive. However, some patients with chronic obstructive pulmonary disease (COPD), such as emphysema or chronic bronchitis, have a tendency to retain CO2 in their arterial blood from poor gas exchange. Because the CO2 level is chronically elevated, the central chemoreceptors become desensitized to fluctuations that typically would stimulate a change in the rate or depth of ventilation. Because of the desensitization of the central chemoreceptors, the peripheral chemoreceptors become the primary stimulus to control ventilation. Thus, hypoxia, rather than CO2, becomes the stimulus for the person to breathe; this is referred to as a hypoxic drive.
Name 3 receptors that are located in the lungs.
Three different types of receptors are found within the lungs: irritant receptors, stretch receptors, and J-receptors.
The irritant receptors are found in the airways and are sensitive to irritating gases, aerosols, and particles. Irritant receptors will cause a cough, bronchoconstriction, and an increase in the rate of ventilation.
The stretch receptors are located within the smooth muscle of the airways. These are responsible for measuring the size and volume of the lungs. To prevent overinflation when stimulated by high tidal volumes, these receptors decrease the rate and volume of ventilation when stretched.
J-receptors are located in the capillaries surrounding the alveoli and are sensitive to increases in pressure within the capillary. When activated, these receptors stimulate rapid, shallow respiration.
What are the normal breathing rates for adults, children, and infants?
Adult: 12-20 times per minute
Child: 24-30 times per minute
Infant: 30-60 times per minute
Name the 10 systems of the body.
1. Integumentary
2. Skeletal
3. Muscular
4. Nervous
5. Endocrine
6. Cardiovascular
7. Lymphatic
8. Respiratory
9. Digestive
10. Reproductive
What are the functions of the skeletal system?
Functions of the skeletal system:
• Protect organs
• Support body
• Allow movement
• Produce blood cells
• Store minerals
What are the functions of the lymphatic system?
Functions of the lymphatic system:
• Remove foreign substances
• Combat disease
• Maintain fluid balance
• Absorb fat
What are the functions of the digestive system?
Functions of the digestive system:
• Perform mechanical and chemical process of digestion
• Absorption of nutrients
• Elimination of wastes
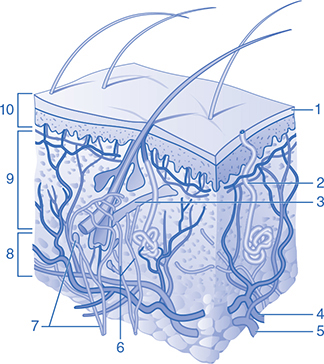
1. Name the upper chambers of the heart and their functions.
2. Name the lower chambers of the heart and their functions.
1. Right atrium: Receives oxygen-poor blood from the veins of the body.
Left atrium: Receives oxygen-rich blood from the lungs via the pulmonary veins.
2. Right ventricle: Pumps oxygen-poor blood to the lungs.
Left ventricle: Pumps oxygen-rich blood to the body.
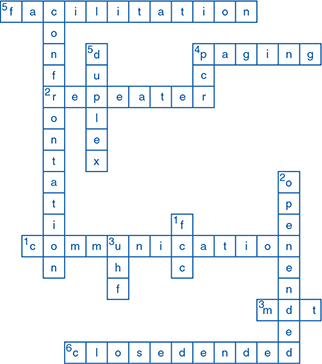
1. Stratum corneum
2. Sweat gland
3. Arrector pili muscle
4. Arteriole
5. Venule
6. Motor nerve
7. Sensory nerve
8. Hypodermis
9. Dermis
10. Epidermis
1. Superior vena cava
2. Right atrium
3. Tricuspid valve
4. Right ventricle
5. Papillary muscle
6. Aorta
7. Pulmonary artery
8. Left atrium
9. Tricuspid valve
10. Septum
Define cardiac output.
Cardiac output = (stroke volume) × (heart rate)
• Defined as the amount of blood pumped by the heart in 1 minute (stroke volume × heart rate = cardiac output)
• Expressed in liters per minute
• An increase in stroke volume or heart rate = increased cardiac output
• A decrease in stroke volume or heart rate = decreased cardiac output
Define blood pressure.
Blood pressure is defined as cardiac output × peripheral vascular resistance (afterload).
• Increased afterload = increased blood pressure
• Decreased afterload = decreased blood pressure

1. Trachea
2. Nasopharynx
3. Oropharynx
4. Larynx
5. Lung
6. Bronchus
7. Alveoli
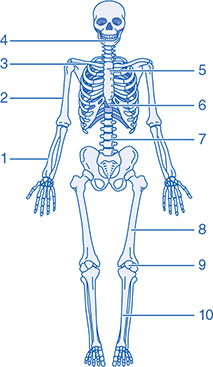
1. Radius
2. Humerus
3. Clavicle
4. Mandible
5. Manubrium
6. Xiphoid process
7. Lumbar
8. Femur
9. Patella
10. Tibia
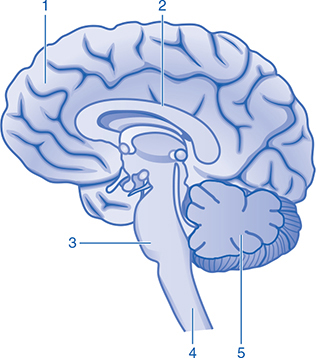
1. Cerebrum
2. Corpus callosum
3. Pons
4. Spinal cord
5. Cerebellum
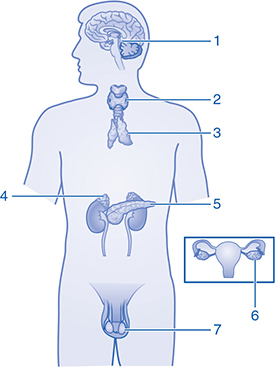
1. Pituitary gland
2. Thyroid
3. Thymus
4. Adrenal gland
5. Pancreas
6. Ovaries
7. Testis
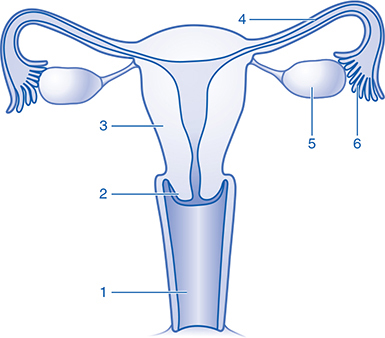
1. Vagina
2. Cervix
3. Uterus
4. Fallopian tube
5. Ovary
6. Fimbria
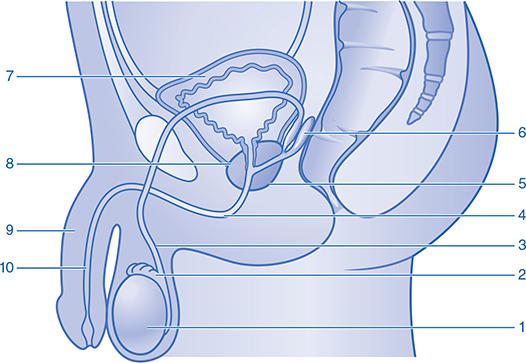
1. Testis
2. Epididymis
3. Vas deferens
4. Urethra
5. Prostate
6. Seminal vesicle
7. Bladder
8. Prostate
9. Penis
10. Urethra
Directional terminology. Define the following terms:
• Torso
• Midline
• Medial
• Lateral
• Proximal
• Distal
• Superior
• Inferior
• Torso: trunk of the body
• Midline: imaginary line running vertically from the nose through the umbilicus (belly button)
• Medial: toward the midline
• Lateral: away from the midline
• Proximal: closer to the trunk
• Distal: away from the trunk
• Superior: above
• Inferior: below
Directional terminology. Define the following terms:
• Midaxillary line
• Anterior
• Posterior
• Midclavicular line
• Bilateral
• Dorsal
• Ventral
• Palmar
• Plantar
• Prone
• Supine
• Fowler position
• Trendelenburg position
• Midaxillary line: imaginary line running vertically from the middle of the armpit to the ankle
• Anterior: toward the front
• Posterior: toward the rear
• Midclavicular line: imaginary line drawn vertically from the middle of the clavicle to the pelvis
• Bilateral: pertaining to both sides
• Dorsal: toward the back
• Ventral: toward the front
• Palmar: relating to the palm
• Plantar: relating to the sole of the foot
• Prone: lying face down
• Supine: lying face up
• Fowler position: sitting up
• Trendelenburg position: feet up, head down position (also known as the shock position)
What does whole blood contain?
• Red blood cells
• White blood cells
• Platelets
• Plasma
• Clotting factors
1. What are 2 types of metabolism?
2. What is the primary fuel for metabolism within a cell?
3. What is the primary catalyst for metabolism within a cell?
4. What is the breakdown of molecules such as glucose within the cells when oxygen is present?
5. What is the breakdown of molecules such as glucose within the cells when oxygen is not present?
6. An energy source required by the cell to release more energy and a necessity for cells to carry out certain functions such as contraction of muscles.
7. What provides for alternating movement of sodium out of and potassium into the cells, which is required for cells to perform their special functions?
8. What is needed for the sodium/potassium pump to work?
9. The delivery of oxygen, glucose, etc., to the cells and elimination of waste products from the cells.
10. It is important to ensure that the concentration of oxygen a patient is breathing is at least _____%.
11. A contraction of the vocal cords that causes them to close and prevents air from passing into the trachea.
12. The concept that the volume of a gas is inversely proportionate to the pressure.
13. The amount of air moved in and out of the lungs in 1 minute.
14. The volume of air breathed in with each breath.
1. Aerobic and anaerobic metabolism
2. Glucose
3. Oxygen (O2)
4. Aerobic metabolism
5. Anaerobic metabolism
6. Adenosine triphosphate (ATP)
7. The sodium/potassium pump
8. Adenosine triphosphate (ATP) and cellular energy
9. Perfusion
10. 21
11. Laryngeal spasm
12. Boyle’s law
13. Minute ventilation or minute volume
14. Tidal volume (Vt)
Life Span Development
1. A child from birth to 1 month of age
2. A child from 1 month to 1 year of age
3. An instantaneous and involuntary movement resulting from a stimulus
4. Soft spots on a baby’s skull that allow the head to pass through the birth canal during delivery and to expand during development
5. A child from 1 to 3 years of age
6. A child from 3 to 6 years of age
7. A child from 6 to 12 years of age
8. Involuntary bed-wetting at night
1. Neonate
2. Infant
3. Reflex
4. Fontanels
5. Toddler
6. Preschooler
7. School-age child
8. Nocturnal enuresis