Bone disease
Donncha O'Gradaigh, Richard Conway
Anatomy and Physiology of Bone
Bone is a specialized connective tissue serving three major functions:
• mechanical – supplying structure and muscle attachment for movement
• metabolic – providing the body's primary store of calcium and phosphate
Bone structure
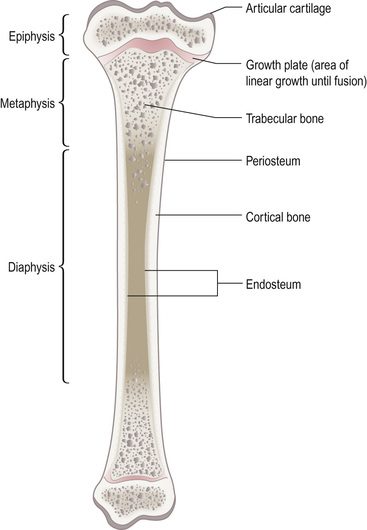
Bone is comprised of cells and a matrix of organic protein and inorganic mineral. Long bones (femur, tibia, humerus) and flat bones (skull, scapula) have different embryological templates, with varying proportions of cortical and trabecular bone.
• Cortical (compact or lamellar) bone forms the shaft of long bones and the outer shell of flat bones. Formed of concentric rings of bone, it is particularly adapted to withstand bending strain.
• Trabecular (cancellous) bone is found at the ends of long bones and inside flat bones. Comprised of a network of interconnecting rods and plates of bone, it offers resistance to compressive loads. It is also the main site of bone turnover for mineral homeostasis.
• Woven bone lacks an organized structure. It appears in the first few years of life, at sites of fracture repair and in high-turnover bone disorders such as Paget's disease.
Matrix components
• Type I collagen is the main protein, forming parallel lamellae of differing density (which impairs spreading of cracks). In cortical bone, concentric lamellae form around a central blood supply (Haversian system), which communicates via transverse (Volkmann's) canals.
• Non-collagen proteins include osteopontin, osteocalcin and fibronectin.
• Bone mineral largely consists of calcium and phosphate in the form of hydroxyapatite.
Bone cells
Osteoblasts
Derived from local mesenchymal stem cells, these cells synthesize matrix (osteoid) and regulate its mineralization. After bone formation, the majority of osteoblasts are removed by apoptosis (see p. 105), others remaining at the bone/marrow interface as lining cells or within the bone as osteocytes. Osteoblasts regulate bone resorption through the balance in expression of the stimulatory receptor activator of nuclear factor kappa B ligand (RANKL) and its antagonist, osteoprotegerin (OPG). Osteoblasts are rich in alkaline phosphatase and express receptors for parathyroid hormone (PTH), oestrogen, glucocorticoids, vitamin D, inflammatory cytokines and the transforming growth factor-beta (TGF-β) family, all of which may therefore influence bone remodelling.
Osteocytes
These small cells, derived from osteoblasts, are embedded in bone and interconnected with each other and with bone lining cells through cytoplasmic processes. They respond to mechanical strain by undergoing apoptosis or through altered cell signalling, which in turn activates bone formation with or without prior resorption. As osteocytes also express RANKL and OPG, the relative importance of osteocytes and osteoblasts in bone resorption function continues to be explored.
Osteoclasts
These cells have the unique capacity to resorb bone and are derived from haemopoietic precursors of the macrophage lineage. In response to RANKL, macrophage colony stimulating factor (M-CSF) and local adhesion factors (integrins), osteoclasts attach to bone, creating a ruffled border that forms a number of extracellular lysosomal compartments. Hydrogen ions are actively secreted into these spaces and the acid environment removes the mineral phase before specialized cysteine proteases (e.g. cathepsin K) resorb the collagen matrix.
Bone growth and remodelling
Longitudinal growth occurs at the epiphyseal growth plate, a cartilage structure between the epiphysis and metaphysis (Fig. 19.1). Cartilage production is tightly regulated, with subsequent mineralization and growth finally arrested at 18–21 years, when the epiphysis and metaphysis fuse.
In adults, bone is regularly remodelled to ensure repair of microdamage and turnover of calcium and phosphate for homeostasis. This remodelling cycle is carried out by the basic multicellular unit (BMU; Fig. 19.2 ). Signals initiating resorption include osteocyte apoptosis and altered signalling (sclerostin, prostaglandins, RANKL and other molecules), resulting in localized retraction of bone-lining cells and binding of multinucleate osteoclasts to the bone surface, followed by bone resorption. Bone formation involves reciprocal effects of wnt versus dickkopf (Dkk) and sclerostin on the LRP5/6-β-catenin pathway. The switch from resorption to formation may rely on osteocyte signalling or on release of signals from the bone matrix, such as TGF-β. Bone remodelling is said to be coupled when formation follows resorption, but may be unbalanced when the amount of bone removed is not replaced with an equal amount.
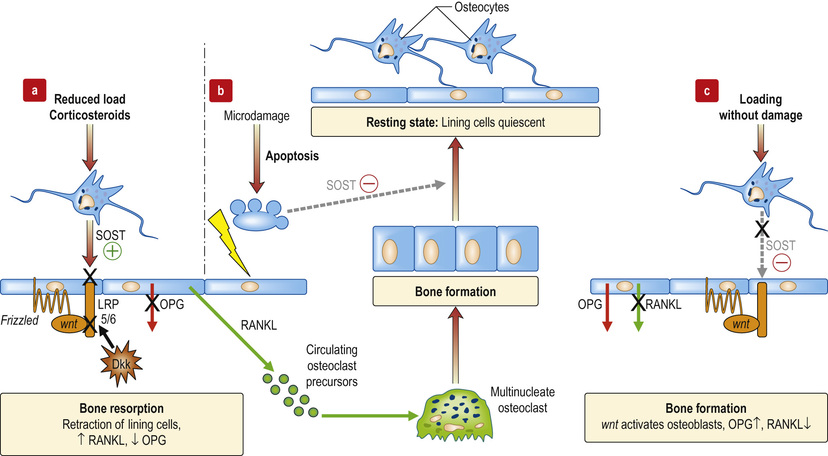
Examples of bone remodelling include:
• Myeloma cells have dual lytic effects, with enhanced expression of RANKL and expression of Dkk
• In rheumatioid arthritis, RANKL and Dkk are increased
• In spondyloarthritis (characterized by new bone formation alongside erosion) Dkk is inhibited, with the increased wnt activity also increasing OPG relative to RANKL
• Corticosteroids may increase osteocyte SOST expression, and stimulate expression of Dkk.
Calcium homeostasis and its regulation
Calcium homeostasis is regulated by the effects of PTH and 1,25-dihydroxyvitamin D (1,25(OH)2D3) on gut, kidney and bone. Calcium-sensing receptors are present in the parathyroid glands, kidney and brain.
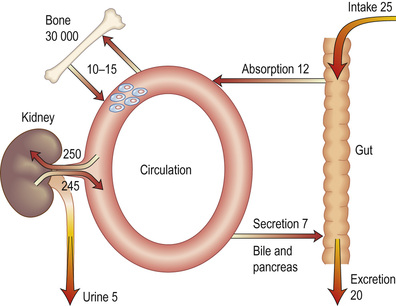
Calcium absorption and distribution
Daily calcium consumption (Fig. 19.3), primarily from dairy foods, is 20–25 mmol (800–1000 mg). The combined effect of calcium and vitamin D deficiency contributes to the bone fragility seen in some older persons. Intestinal absorption of calcium is reduced by vitamin D deficiency and in malabsorption states (see p. 204).
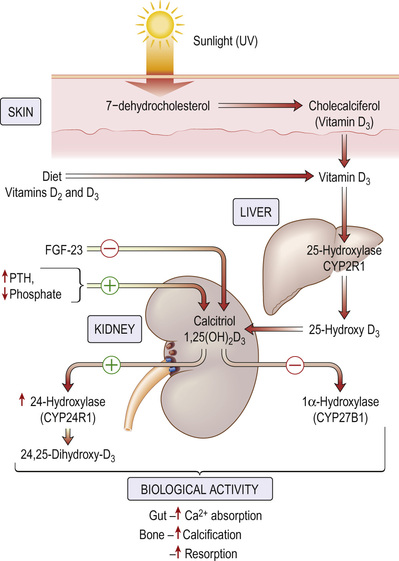
Vitamin D metabolism
The primary source of vitamin D (Fig. 19.4) in humans is photoactivation in the skin of 7-dehydrocholesterol to cholecalciferol, which is then converted first in the liver to 25-hydroxyvitamin D (25(OH)D3) and subsequently in the kidney (by the enzyme 1α-hydroxylase) to 1,25(OH)2D3. (This step can occur in lymphomatous and sarcoid tissue, resulting in hypercalcaemia.) Regulation of the latter step is by PTH, phosphate and feedback inhibition by 1,25(OH)2D3.
Parathyroid hormone
Parathyroid hormone (PTH), an 84-amino-acid hormone, is secreted from the chief cells of the parathyroid gland, which have calcium-sensing and vitamin D receptors. PTH increases renal phosphate excretion and increases plasma calcium by:
• increasing osteoclastic activity in bone (a rapid response)
• increasing intestinal absorption of calcium (a slower response)
• increasing 1α-hydroxylation of vitamin D (the rate-limiting step)
Hypomagnesaemia can suppress the normal PTH response to hypocalcaemia.
Calcitonin
Calcitonin is produced by thyroid C cells. Although calcitonin inhibits osteoclastic bone resorption and increases the renal excretion of calcium and phosphate, neither excess calcitonin (seen in medullary carcinoma of the thyroid) nor its deficiency following thyroidectomy has significant skeletal effects in humans.
Clinical Approach to the Patient with Bone Disease
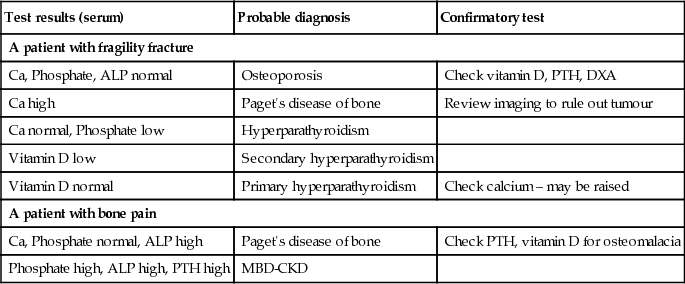
Investigation of bone and calcium disorders
(See Box 19.1.)
Total plasma calcium
Normal range 2.2–2.6 mmol/L. About 40% is ionized and physiologically active; the remainder is complexed or protein-bound. As ionized calcium is difficult to measure, normal practice is to measure total calcium, correcting the value to allow for protein binding according to the following formula: add or subtract 0.02 mmol/L for each gram per litre of a simultaneous albumin level below or above 40 g/L. For critical measurements, samples should be taken in the fasting state and without a tourniquet (the latter may increase local plasma calcium concentration).
Plasma phosphate
Normal range 0.8–1.4 mmol/L. Phosphate is essential to most biological systems. High levels are found in chronic kidney disease (CKD) and hypoparathyroidism, while low levels are associated with primary hyperparathyroidism, hypophosphataemic rickets and osteomalacia, and other disorders associated with reduced renal tubular phosphate reabsorption.
Plasma PTH
Normal range 10–65 ng/mL. The PTH assay measures the intact hormone. In hypercalcaemia not due to hyperparathyroidism, serum PTH levels are suppressed. Lithium toxicity may be associated with raised PTH levels; in familial hypocalciuric hypercalcaemia (FHH), serum PTH may be normal or marginally elevated.
Serum 25-hydroxyvitamin D
Vitamin D status is best assessed using serum 25-(OH)D3, as 1,25(OH)2D3 has a short half-life and does not accurately reflect true vitamin D status. Vitamin D deficiency is defined as <25 nmol/L (10 ng/mL) and vitamin D insufficiency as <75 nmol/L (30 ng/mL). Rickets and osteomalacia occur with prolonged vitamin D deficiency.
The significance of vitamin D insufficiency is uncertain but it has been linked to a wide range of conditions, including ischaemic heart disease, multiple sclerosis and a variety of cancers. Recent evidence suggests that racial differences are present in the assessment of vitamin D status. Black Americans have consistently lower levels of 25-(OH)D3 than white Americans but also lower levels of vitamin D-binding protein, resulting in equivalent bioavailable 25-(OH)D3.
24-hour urinary calcium
Normal range 2.5–6.25 (female) and 7.5 (male) mmol/24 h. This is increased where renal tubular reabsorption of calcium is decreased, and in hypercalcaemia. One exception is FHH, where the genetic defect leads to inappropriately reduced calcium excretion. Measurement of 24-hour urinary calcium excretion should be performed in the assessment of hypercalcaemic patients.
Biochemical markers of bone formation and resorption
The clinical use of these biochemical markers is limited by large biovariability and measurement variance. Serial measurements at the same time of day in individual patients are useful in assessing response to treatment of metabolic bone diseases.
• Bone-specific alkaline phosphatase. Circulating alkaline phosphatase is derived from bone, liver and placenta. The bone-specific isoenzyme can be measured as a marker of formation, although there is some overlap with the liver isoenzyme. Elevated serum levels occur during bone growth: for example, in adolescents, fracture repair, and high-bone-turnover states.
• Type 1 collagen pro-peptides. These are by-products of collagen synthesis. Serum levels of both the carboxyterminal (P1CP) and aminoterminal (P1NP) pro-peptides reflect bone formation.
• Serum osteocalcin. This is another bone formation marker.
• Serum or urine levels of N-terminal (NTX) and C-terminal (CTX) cross-linked telopeptides. These reflect bone resorption. They may change rapidly in response to anti-resorptive drugs or in disease states, and have been used to assess fracture risk.
Diagnostic imaging
• Plain radiographs. These identify fractures, tumours and infections. Other specific features may be seen (see following sections).
• Radionucleotide imaging. The uptake of a 99mtechnetium-labelled bisphosphonate in bone reflects bone turnover and blood flow. Increased uptake is therefore seen in fractures, tumour and metastatic deposits, infection and Paget's disease of bone.
• Magnetic resonance imaging (MRI). This is the most sensitive and specific test for the diagnosis of osteomyelitis. It is also useful in the detection of stress fractures, which may not be demonstrated on plain radiographs. A technique to suppress the high signal associated with bone marrow (such as STIR sequences; see p. 651) allows highly sensitive recognition of ‘bone marrow oedema’, a non-specific feature of a number of bone disorders, including osteonecrosis.
• Bone biopsy (Fig. 19.5). A core of bone is removed, including both cortices of the iliac crest, using a trephine. The non-decalcified specimen is examined for static and dynamic (bone turnover) indices. An oral tetracycline is given to the patient prior to the biopsy, for 2 days on two occasions 10 days apart, allowing assessment of the rate of bone turnover and mineralization. Biopsy is most commonly used in the assessment of suspected renal bone disease and osteomalacia.
• Bone densitometry measurements (see p. 712).
Osteoporosis
Osteoporosis is defined as ‘a disease characterized by low bone mass and micro-architectural deterioration of bone tissue, leading to enhanced bone fragility and an increase in fracture risk’.
Using bone densitometry at the hip or spine measured by dual X-ray absorptiometry (DXA), the World Health Organization (WHO) also defines osteoporosis as a bone density of 2.5 standard deviations (SDs) below the young healthy adult mean value (T-score ≤−2.5) or lower. Values between −1 and −2.5 SDs below the young adult mean are termed ‘osteopenia’. The rationale for this definition is the inverse relationship between bone mineral density (BMD) and fracture risk in postmenopausal women and older men. However, this definition should not be applied to younger populations.
Fractures due to osteoporosis are a major cause of morbidity and mortality in elderly populations, with osteoporotic fractures of the spine causing acute pain or deformity and postural back pain. One in two women and one in five men aged 50 years will have an osteoporotic fracture during their remaining lifetime. Caucasian and Asian races are particularly at risk. As the risk of fracture increases exponentially with age, changing population demographics will increase the burden of disease.
 Pathogenesis
Pathogenesis
Osteoporosis results from increased bone breakdown by osteoclasts and decreased bone formation by osteoblasts, leading to loss of bone mass.
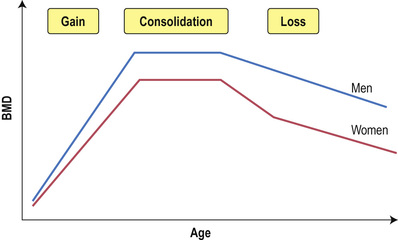
Bone mass decreases with age (Fig. 19.6) but will depend on the ‘peak’ mass attained in adult life and on the rate of loss in later life. Genetic factors are the single most significant influence on peak bone mass. Multiple genes are involved, including collagen type 1A1, vitamin D receptor and oestrogen receptor genes. Nutritional factors, sex hormone status and physical activity also affect peak mass. Not all causes of osteoporosis affect bone remodelling and architecture in the same way.
Oestrogen deficiency results in increased numbers of remodelling units, premature arrest of osteoblastic synthetic activity and perforation of trabeculae, with a loss of resistance to fracture that is not fully reflected in the bone density measurement.
Glucocorticoids induce a high-turnover state initially, with increased fracture risk evident within 3 months of starting therapy. More prolonged use leads to a reduced-turnover state but with a net loss due to reduced synthesis (through increased inhibition of the wnt-LRP5/6 axis).
Ageing results in increased turnover at the bone/vascular interface within cortical bone, resulting in a weak structure for the stresses occurring in this area of long bones (trabecularization of cortical bone).
 Risk factors
Risk factors
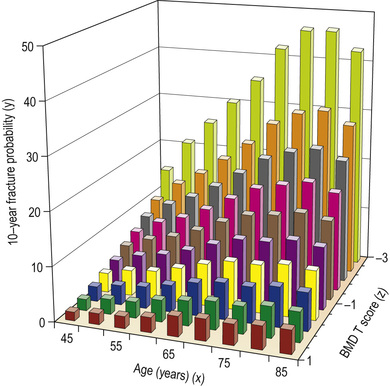
Risk factors for fracture may exert their effect through reducing BMD, or they may increase risk over that attributable to BMD, meaning that they are BMD-independent (Box 19.2). Oestrogen deficiency is a major factor in the pathogenesis of accelerated bone loss due to a normal or premature menopause or amenorrhoea in anorexia and in athletes. In the elderly, vitamin D insufficiency and consequent hyperparathyroidism reduce BMD. However, previous fracture, increasing age, glucocorticoid therapy, smoking and falls increase the risk of fracture at any given BMD. For instance, 10% of women who are 65 years old and have a T-score of −2 at the hip would be expected to sustain a fracture over the next 10 years; if similar women had a Colles' fracture, smoked and had prolonged exposure to steroids, their risk would be closer to 26% in the same period.
Treatment depends on the type of risk factors: if they are recognized as ‘BMD-dependent’, they respond to bone-directed treatment; if classed as ‘BMD-independent’, they require additional intervention (e.g. reduction of falls risk).
 Clinical features
Clinical features
Fracture is the only cause of symptoms in osteoporosis. Vertebral crush fracture is suggested by the sudden onset of severe pain in the spine, often radiating around to the front. However, only about 1 in 3 vertebral fractures is symptomatic. Pain from mechanical derangement, increasing kyphosis, height loss and abdominal protuberance follow crushed vertebrae. Colles' fractures typically follow a fall on an outstretched arm. Fractures of the proximal femur usually occur in older individuals falling on their side or back.
Other causes of low-trauma fractures must not be overlooked, including metastatic disease and myeloma.
 Investigations
Investigations
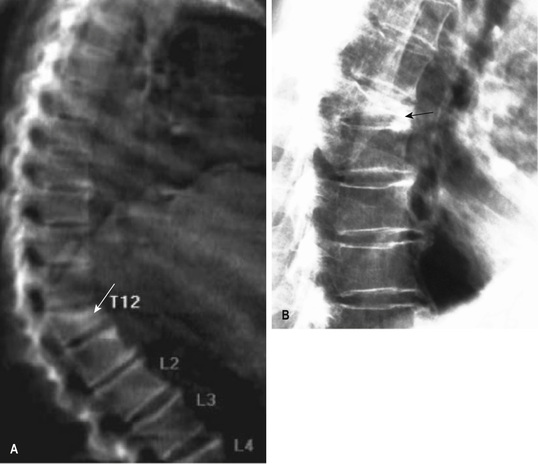
Plain radiographs (Fig. 19.7) usually show a fracture and may reveal previously asymptomatic vertebral deformities. Such clinically silent fractures may also be detected during DXA scanning with an additional analysis (called lateral vertebral assessment, carried out with a much lower radiation dose than conventional imaging).
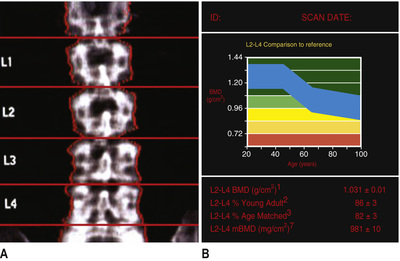
Bone density
DXA measures areal bone density (mineral per surface area rather than a true volumetric density), usually of the lumbar spine and proximal femur. It is precise and accurate, uses low doses of radiation and is the ‘gold standard’ in diagnosis of osteoporosis (Fig. 19.8). Because of osteophytes, spinal deformity and vertebral fractures, spinal values may be artefactually elevated and should be interpreted with caution in the elderly.
Associated disease and risk factors
Investigations to exclude other diseases or identify contributory factors associated with osteoporosis should be performed and are particularly necessary in men, in whom secondary causes are more common (Box 19.2).
Selection of individuals for treatment: risk assessment
The purpose of treatment in osteoporosis is to reduce the risk of fractures (Box 19.3). Thus, assessment of absolute fracture risk should be made in every case. All patients with a history of fragility fracture should be reviewed for treatment. In those aged over 75 years, DXA is often not necessary prior to treatment, but in those under 75 years of age, DXA is useful in guiding treatment decisions (Box 19.4 and Fig. 19.9 ). Although age and BMD measurements in the spine and proximal femur are the most useful data for assessing fracture risk, it is vital to recognize that the majority of fragility fractures occur in women with a T-score better than −2.5. Therefore, factors that are known to increase fracture risk independently of BMD should be taken into account when assessing an individual's risk of fracture, for example, using risk calculators such as FRAX®. The threshold for recommending treatment will be determined by the cost-effectiveness of treatment in a particular healthcare setting and by clinical judgement.
 Prevention and management
Prevention and management
• Symptomatic management. New vertebral fractures may require bed rest for 1–2 weeks with strong analgesia, muscle relaxants (e.g. diazepam 2 mg 3 times daily) and gradual physiotherapy to restore confident mobilization (see p. 659). Non-spinal fractures should be treated by conventional orthopaedic means.
• Calcium and vitamin D. Daily intakes of 800–1200 mg of calcium and 400–800 IU of vitamin D are recommended throughout life for optimum bone health. Dietary intake of calcium, and vitamin D from sunshine and diet, are preferable. For those not meeting calcium intake targets, or those with low serum 25-(OH)D3 levels, supplements are recommended, e.g. colecalciferol 20 µg and calcium 2 g daily.
• Lifestyle measures. Weight-bearing exercise for 30 min 3 times a week may increase BMD, while gentle exercise in the elderly may reduce the risk of falls and improve the protective responses to falling. Smoking and excess alcohol use should be avoided.
• Reduction of falls. Physiotherapy and assessment of home safety are helpful. Hip protectors do reduce fractures in the elderly in residential care when worn correctly, but compliance is poor.
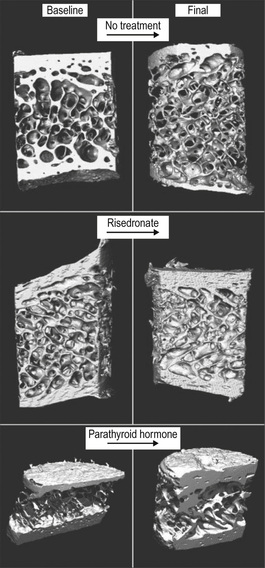
Pharmacological intervention
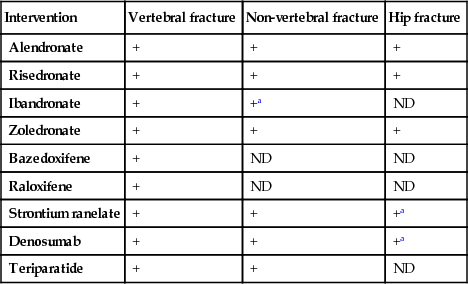
Most interventions (see Fig. 19.5 ) act by inhibiting bone resorption (anti-resorptives), the exception being PTH peptides, which stimulate bone formation. The impression from bone turnover markers that strontium ranelate may have both anti-resorptive and stimulatory effects remains poorly understood.
The evidence base for the anti-fracture efficacy of interventions varies. Some interventions have been shown to reduce fracture at vertebral and non-vertebral sites, including the hip, whereas others have not been demonstrated to be effective at all sites (Box 19.5). Since a fracture at one site increases the risk of subsequent fracture at any site, treatments with efficacy at all major fracture sites (particularly spine and hip) are preferable. Hence, the bisphosphonates and denosumab are generally regarded as first-line options in the majority of postmenopausal women with osteoporosis.
Bisphosphonates
Synthetic analogues of bone pyrophosphate, bisphosphonates adhere to hydroxyapatite and inhibit osteoclasts. Alendronate and risedronate are given as once-weekly doses, zoledronate as a once-yearly infusion, and ibandronate usually as a once-monthly oral therapy (a 3-monthly intravenous injection is rarely used).
Oral bisphosphonates should be taken fasting, with a large drink of water, while standing or sitting upright. The patient should then remain upright and avoid food and drink for at least 30 minutes.
Bisphosphonates are generally well tolerated but may be associated with upper gastrointestinal side-effects such as oesophagitis, particularly if the dosing instructions are not closely followed. Bisphosphonates should be used with careful monitoring in patients who have chronic kidney disease (stage 4 or 5). Osteonecrosis of the jaw is rarely seen following high-dose intravenous bisphosphonates in patients who have malignant disease. It is associated with poor dental hygiene. As prolonged suppression of bone turnover is linked with atypical femoral fractures, it is currently advised to reassess bisphosphonate treatment after 5 years. Only those with vertebral fractures and a T-score at the neck of femur of <−2.5 at this 5-year scan appear to have a reduced risk of fracture with continued treatment.
Denosumab
Denosumab is a fully human monoclonal antibody to RANKL and is administered as a single subcutaneous injection every 6 months. It is an anti-resorptive agent that increases BMD and reduces fractures at the spine, hip and other non-vertebral sites. Fracture risk reduction at the spine is equivalent to that with most bisphosphonates, and risk reduction at the hip is superior (with the exception of zoledronic acid). Adverse effects are infrequent: most commonly dysuria, rarely cellulitis. Osteonecrosis of the jaw and atypical femoral fractures have also occurred but estimating the true frequency of these rare adverse events is not possible with current data.
Strontium ranelate
This is used only when no alternative exists because of its adverse cardiovascular effects. It has weak anti-resorptive activity whilst maintaining bone formation. It reduces the risk of vertebral fractures in postmenopausal women with osteoporosis, and the risk of hip and other non-vertebral fractures in high-risk subgroups (women with previous fracture and T-scores at the hip of −2.4 or less). Nausea, diarrhoea and headaches are infrequent side-effects.
Selective oestrogen-receptor modulators
Selective oestrogen-receptor modulators (SERMs) include raloxifene and bazedoxifene. They have no stimulatory effect on the endometrium but activate oestrogen receptors in bone. Both prevent BMD loss at the spine and hip in postmenopausal women, but have been found to reduce only vertebral fracture rates. Leg cramps and flushing may occur and the risk of thromboembolic complications is also increased to a degree similar to that seen with hormone replacement therapy (HRT; see pp. 1296–1297 and Box 29.1). The use of SERMs is associated with a small increase in the risk of stroke.
Recombinant human parathyroid hormone
Recombinant human PTH peptide 1–34 (teriparatide) and recombinant human PTH 1–84 are anabolic agents that stimulate bone formation. Teriparatide reduces vertebral and non-vertebral fractures in postmenopausal women with established osteoporosis, although data on hip fracture are not available. It is given by daily subcutaneous injection for 24 months. Recombinant human PTH 1–84 is also administered by once-daily subcutaneous injection but has been shown to reduce only vertebral fractures. An anti-resorptive drug, such as denosumab, should be given on completion of PTH peptide therapy to maintain the increase in BMD. Non-osteoporotic bone diseases, such as osteomalacia, should be excluded prior to treatment. PTH peptide therapy is indicated mainly in severe cases of vertebral osteoporosis or in women who fail to respond to other therapies. Teriparatide may cause mild transient hypercalcaemia but routine monitoring is not required. Nausea and headache may occur. Recombinant human PTH 1–84 is associated with a higher incidence of hypercalcaemia and hypercalciuria, and routine monitoring is advised. Neither agent should be used in people with skeletal metastases or osteosarcoma.
Hormone replacement therapy
Because of its adverse effects on breast cancer and cardiovascular disease risk, HRT is not indicated for osteoporosis except in early postmenopausal women who also have significant perimenopausal symptoms.
Calcitriol (1,25-(OH)2D3) and calcitonin
These may reduce vertebral fracture rate, although the data are inconsistent.
Combination therapies
Combination therapies, either with two anti-resorptive agents, or an anti-resorptive and an anabolic agent, often produce larger increases in BMD than monotherapy but have not been shown to result in greater fracture reduction.
Surgery
This is required to stabilize vertebral fractures. Percutaneous vertebroplasty and balloon kyphoplasty are discussed on page 659. Hip fractures are dealt with by hip replacements or stabilization with pins.
Treatment of specific conditions
Glucocorticoid-induced osteoporosis
Individuals requiring continuous oral glucocorticoid therapy for 3 months or more (at any dose) should be assessed for coexisting risk factors (age, previous fracture, hormone status). Postmenopausal women, men aged over 50 years and any individuals who have sustained a fragility fracture should receive treatment without waiting for DXA scanning. DXA results and fracture risk assessment guide treatment for other patients (see Box 19.4 ). For these individuals, bisphosphonates and teriparatide are the approved agents. Denosumab is likely to be equally effective; though it is not yet formally approved for this indication, its mode of delivery may be advantageous in some settings.
Osteoporosis in men
Alendronate, risedronate and denosumab increase BMD and reduce vertebral fractures in men with osteoporosis. Teriparatide is also approved for use in this setting. In men with osteoporosis who have clinical and biochemical evidence of hypogonadism, testosterone replacement is also used.
Osteonecrosis
This is also known as aseptic, avascular or ischaemic necrosis of bone. There are a multitude of risk factors but over 80% of cases are attributed to glucocorticoid treatment or alcohol excess. Less frequent causes include sickle cell disease, systemic lupus erythematosus (SLE), deep-sea diving (Caisson's disease), endocrine disorders (e.g. Cushing's, diabetes mellitus), trauma, human immunodeficiency virus (HIV) infection and irradiation.
Osteonecrosis usually presents with joint pain, the shoulder or hip being most commonly affected, but can be asymptomatic, particularly on the opposite side in the same person. It may only be recognized when it results in collapse of the articular bone.
MRI best confirms the diagnosis by showing bone marrow oedema. If advanced, it can be seen on plain X-rays.
Management is mainly symptomatic. Surgical options include drilling through the bone cortex (decompression), vascularized bone grafts, or rotation of the affected bone away from the load-bearing area; however, joint replacement is often required. Bisphosphonates may reduce pain, and progression has been reduced with statin therapy in steroid-associated osteonecrosis.
Paget's Disease of Bone
Paget's disease of bone is a focal disorder of bone remodelling. Increased osteoclastic bone resorption is followed by a compensatory increase in new bone formation, increased local bone blood flow and fibrous tissue in adjacent bone marrow. Ultimately, formation exceeds resorption but the new woven bone is weaker than normal bone, which leads to deformity and increased fracture risk. Paget's disease does not spread, but can become symptomatic at previously silent sites.
Epidemiological studies are difficult because most affected individuals are asymptomatic. Paget's disease is most often seen in Europe and particularly in northern England. It affects men and women (2:3) over the age of 40 years. The incidence approximately doubles per decade thereafter, with up to 10% of individuals radiologically affected by the age of 90. For unknown reasons, the incidence and severity of Paget's disease have decreased in recent years.
 Aetiology and pathogenesis
Aetiology and pathogenesis
Genetic factors are implicated in Paget's disease. A positive family history is noted in about 15%. Mutations in SQSTM1, which encodes the osteoclast mediator protein p62, have been reported in up to 10% of cases. Intracellular inclusions in the osteoclasts in pagetic lesions are believed to be paramyxovirus nucleocapsid (e.g. canine distemper virus, measles or respiratory syncytial virus). However, similar inclusions are seen in other bone disorders, and theories of a viral aetiology in Paget's remain contentious. Altered expression of c-fos (an oncogene) is one suggested mechanism linking viral infection with the pathogenic changes in osteoclasts, which are more numerous and contain an increased number of nuclei (up to 100).
 Clinical features (see Fig. 19.10A)
Clinical features (see Fig. 19.10A)
Between 60% and 80% of people with radiologically identified Paget's disease are asymptomatic. Diagnosis often follows the finding of an asymptomatic elevation of serum alkaline phosphatase, or a plain X-ray performed for other indications. The disease may involve one bone (monostotic, in 15%) or many (polyostotic). The most common sites, in order of frequency, are pelvis, femur, lumbar spine, skull and tibia (see Fig. 19.10C ). Small bones of the feet and hands are rarely involved.
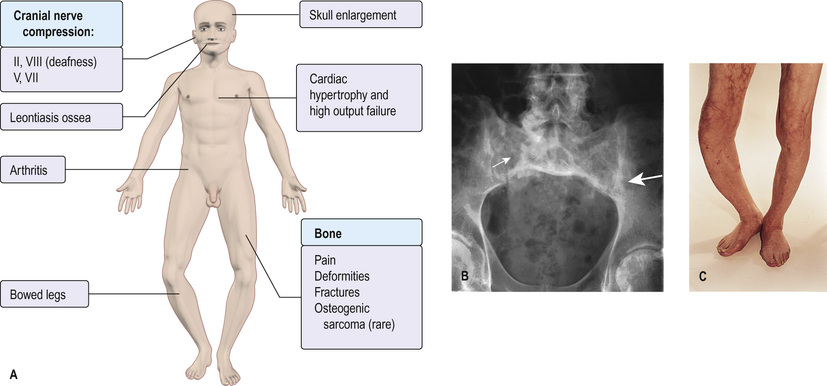
Symptoms and complications include:
• joint pain when an involved bone is close to a joint, leading to cartilage damage and osteoarthritis
• deformities, in particular bowed tibia and skull changes
• neurological complications – nerve compression (deafness from VIIIth cranial nerve involvement; cranial nerves II, V and VII may also be involved); spinal stenosis; hydrocephalus due to blockage of the aqueduct of Sylvius
• high-output cardiac failure and myocardial hypertrophy due to increased bone blood flow
• hypercalcaemia – rarely seen outside the setting of fracture
• osteosarcoma – occurs in fewer than 1% of cases of Paget's and may be heralded by an increase in bone pain or swelling in a previous pagetic bone area.
 Investigations
Investigations
• Increased serum alkaline phosphatase with normal serum calcium and phosphate reflects increased bone turnover. Levels may be normal with limited or monostotic Paget's disease. Levels are reduced with treatment and increased during relapse.
• Vitamin D should be measured, as deficiency is frequent in the age group affected by Paget's disease and should be corrected (see p. 718) to avoid hypocalcaemia following bisphosphonate treatment
• X-ray features (Fig. 19.10B) vary from predominantly lytic lesions (osteoporosis circumscripta in the skull is characteristic), through a mixed phase, to a mainly sclerotic phase of bone expansion, cortical thickening and coarsening of the trabecular pattern.
• Isotope bone scans are useful to determine the extent of skeletal involvement, but are unable to distinguish between Paget's disease and sclerotic metastatic carcinoma (especially breast and prostate).
 Management
Management
Bisphosphonates are the mainstay of treatment. New bone formed after treatment is lamellar, not woven (reflecting normalization of bone turnover rather than a direct effect on osteoblasts). Treatment is interrupted and repeat courses are guided by symptoms and by recurrence in elevation of alkaline phosphatase. In addition to treatment of symptomatic patients, treatment of asymptomatic lesions is appropriate if there is a significant risk of potential complications, such as fracture in weight-bearing long bones or the spine, nerve entrapment or deafness with skull involvement, and before orthopaedic procedures in involved bone (to reduce vascularity).
Intravenous bisphosphonates
Zoledronate is the most commonly used agent for Paget's disease, administered as a single infusion over 15 min. Pamidronate is an alternative but takes longer to infuse and is less potent; some patients develop drug resistance for unknown reasons. Both drugs can be associated with a first-dose reaction characterized by ‘flu-like’ symptoms, including transient pyrexia over 24–48 hours, which can be ameliorated with paracetamol.
Oral bisphosphonates
Oral bisphosphonates are used at doses higher than those for osteoporosis (e.g. 30 mg risedronate daily for 2 months, or 40 mg alendronate daily for 6 months) and are less effective than intravenous zoledronic acid.
Surgery
Joint replacement or osteotomy is sometimes necessary to correct deformity or pain due to associated degenerative joint disease. Neurosurgery may be needed where there is spinal disease. Osteosarcoma usually requires amputation, though wide excision and limb salvage can be successful at distal sites.
Rickets and Osteomalacia
Osteomalacia is defective mineralization of newly formed bone matrix or osteoid. Rickets is defective mineralization at the epiphyseal growth plate and is found in association with osteomalacia in children.
 Aetiology
Aetiology
Many factors can result in defective mineralization of the osteoid. For normal mineralization, adequate levels of vitamin D, calcium and phosphate, adequate activity of alkaline phosphatase, a normal pH at the osteoid surface and normal osteoid composition are all necessary (Box 19.6).
The most common cause of osteomalacia is hypophosphataemia due to hyperparathyroidism secondary to vitamin D deficiency. The most common cause of vitamin D deficiency worldwide is dietary deficiency. Bread, milk and cereals in high-income countries are now fortified with vitamin D. This has led to a much-reduced incidence of osteomalacia and rickets.
Vitamin D is produced in the skin through the action of sunlight on 7-dehydrocholesterol (see Fig. 19.4 ). Lack of sun exposure can lead to vitamin D deficiency, especially in individuals living in temperate regions who keep large parts of the skin covered throughout the year.
Vitamin D is a fat-soluble vitamin, so gastrointestinal disease can result in malabsorption. Gastrectomy, cystic fibrosis, coeliac disease, Crohn's disease and primary biliary cirrhosis are well-recognized causes.
Due to the intimate involvement of the kidney in phosphate balance, a number of causes of osteomalacia are mediated by the kidney (see p. 779). Primary renal phosphate wasting occurs in tumour-induced osteomalacia, multiple myeloma and Fanconi syndrome. Proximal (type 2) renal tubular acidosis can cause osteomalacia due to both renal phosphate wasting and abnormal osteoid pH secondary to metabolic acidosis.
 Clinical features
Clinical features
Osteomalacia may be asymptomatic and identified incidentally on routine investigations following a fragility fracture. When symptomatic, it characteristically causes muscle weakness and widespread bone pain. Muscle weakness is due to a multifactorial proximal myopathy, with low vitamin D, hypophosphataemia and high PTH levels all contributing. It results in a characteristic waddling gait with difficulty climbing stairs and getting out of a chair. Generalized bone pain and tenderness are thought to be caused by hydration of the demineralized matrix, resulting in periosteal distension. The pain is typically a dull ache that is worse on weight-bearing and walking. It can be reproduced by pressure on the sternum or tibia. Insufficiency fractures can occur when the quality of the bone is insufficient to handle the stress of weight-bearing.
At birth, neonatal rickets may present as craniotabes (a thin, deformed skull). In the first few years of life, there may be widened epiphyses at the wrists and beading at the costochondral junctions, producing the ‘rickety rosary’, or a groove in the rib cage (Harrison's sulcus). In older children, lower limb deformities are seen. A myopathy may also occur. Hypocalcaemic tetany may occur in severe cases.
 Investigations
Investigations
• Serum alkaline phosphatase is elevated in 90% of cases.
• Low serum calcium, low phosphate and elevated PTH are each present in approximately half of the cases.
• Serum 25-(OH)D3 is low, usually less than 25 nmol/L (10 ng/mL).
• Serum FGF-23 is elevated in many people with tumour-induced osteomalacia and in hypophosphataemic rickets.
• Plain radiographs demonstrate decreased bone mineralization. The characteristic finding in osteomalacia is Looser's pseudofractures. These are narrow radiolucent lines with sclerotic borders running perpendicular to the cortex. They can be found at any site but are most commonly seen in the femur and pelvis.
• Tetracycline-labelled bone biopsy is the gold standard diagnostic test. This is not practical in most clinical settings and is used mainly in research studies.
 Management
Management
Vitamin D replacement is the cornerstone of treatment. Treatment involves two stages: an initial loading stage to replenish body stores of vitamin D, and a subsequent maintenance phase to avoid repeat deficiency. All patients should also receive supplementary calcium of 1000–1200 mg/day. In nutritional deficiency, recommended initial replacement is with vitamin D 50 000 units per week orally. The initial replacement dose should be continued for 8 weeks. Vitamin D is also available as an intramuscular injection; two doses of 300 000 units are usually enough to replenish body stores. Adequacy of vitamin D replacement should be evaluated by re-assaying vitamin D levels, or PTH levels if initially abnormal. This should be followed by regular supplementation with 800–1000 units of vitamin D per day.
Doses for children are lower and are age-dependent. People with gastrointestinal disease and vitamin D deficiency due to malabsorption need higher doses of 10 000–50 000 units per day of vitamin D.
Tumour-induced osteomalacia is best treated by removal of the causative neoplasm, which is usually occult and frequently benign. This leads to rapid resolution of symptoms.
Bone Infections
 Acute and chronic osteomyelitis
Acute and chronic osteomyelitis
Osteomyelitis predominantly occurs in children and chronicity is common. In children, it commonly arises due to haematogenous spread to the vascular metaphysis. In high-income countries, it occurs in around 8 per 100 000 children per year, but it is considerably more common in low-income countries, with boys affected twice as often as girls. Malnutrition, debilitating disease and decreased immunity play a role in the pathogenesis. Without prompt recognition, it has devastating consequences.
Staphylococcus is the organism responsible for 90% of cases of acute osteomyelitis. Other organisms include Haemophilus influenzae and Salmonella; infection with the latter may occur as a complication of sickle cell anaemia. The classic presentation is with fever and localized bone pain with overlying tenderness and erythema, although it is rare in adults and often hard to diagnose, requiring a bone biopsy.
 Diagnosis
Diagnosis
– Plain X-ray is not sensitive in early infection but osteopenia may be present.
– MRI is highly sensitive, showing marrow oedema in 3 days.
– Bone scans are also helpful.
• Blood cultures are often positive with staphylococcal infection.
• Bone biopsy and culture identifies the organism and sensitivities.
 Management
Management
Treatment of osteomyelitis centres on immobilization and antibiotic therapy with intravenous teicoplanin or intravenous flucloxacillin 1–2 g every 6 hours and oral sodium fusidate. Switch to oral antibiotics after 2 weeks and continue for a further 4 weeks. Surgical drainage and removal of dead bone (sequestrum) may be necessary but recurrence is common.
Delayed treatment leads to chronic osteomyelitis. In chronic osteomyelitis, sinus formation is usual. Subacute osteomyelitis is associated with a chronic abscess within the bone (Brodie's abscess). Symptoms may be limited to local pain.
 Tuberculous osteomyelitis
Tuberculous osteomyelitis
This is usually due to haematogenous spread from a reactivated primary focus in the lungs or gastrointestinal tract. The disease starts in intra-articular bone. The spine is commonly involved (Pott's disease), with damage to the bodies of two neighbouring vertebrae leading to vertebral collapse and acute angulation of the spine (gibbus). Later, an abscess forms (‘cold abscess’). Pus can track along tissue planes and discharge at a point far from the affected vertebrae. Symptoms consist of local pain and later swelling if pus has collected. Systemic symptoms of malaise, fever and night sweats occur.
Management is as for pulmonary tuberculosis but extended to 9 months (see pp. 1110–1113), together with initial immobilization.
Neoplastic Disease Of Bone
Bone pain may be due to multiple myeloma, lymphoma, a primary tumour of bone or secondary deposits. The pain is typically unremitting and worse at night, and there are other clinical clues such as weight loss or ill-health.
Malignant tumours of bone are shown in Box 19.7. The most common tumours are metastases from the bronchus, breast and prostate. Metastases from kidney and thyroid are less common. Primary bone tumours are rare and usually seen only in children and young adults.
Symptoms are usually related to the anatomical position of the tumour, with local bone pain. Systemic symptoms (e.g. malaise and pyrexia) and aches and pains occur and are occasionally related to hypercalcaemia. The diagnosis of metastases can often be made from the history and examination, particularly if the primary tumour has already been diagnosed. Symptoms from bony metastases may, however, be the first presenting feature.
 Investigations
Investigations
• Skeletal isotope scans show bony metastases as ‘hot’ areas before radiological changes occur.
• X-rays may show metastases as osteolytic areas with bony destruction. Osteosclerotic metastases are characteristic of prostatic carcinoma.
• MRI is used extensively, particularly for vertebral lesions.
• CT and computed tomography-positron emission tomography (CT-PET) are useful.
• Serum alkaline phosphatase (from bone) is usually raised.
• Hypercalcaemia occurs in 10–20% of patients who have metastatic malignancies, or is due to ectopic parathormone or PTH-related protein secretion.
• Prostate-specific antigen (PSA) and serum acid phosphatase are raised in the presence of prostatic metastases.
 Management
Management
Treatment is usually with analgesics and anti-inflammatory drugs. Local radiotherapy to bone metastases relieves pain and reduces the risk of pathological fracture. Some tumours respond to chemotherapy; others are hormone-dependent and respond to hormonal therapy. Bisphosphonates (see p. 714) can help symptomatically. Occasionally, pathological fractures require internal fixation.
Other Bone Disorders
 Osteopetrosis (marble bone disease)
Osteopetrosis (marble bone disease)
This condition may be inherited in either an autosomal dominant or a typically severe, autosomal recessive pattern. Another recessive form associated with renal tubular acidosis is due to carbonic anhydrase II deficiency.
The severe form is caused by a mutation in the gene encoding a chloride channel necessary for osteoclast activity. Bone density is increased throughout the skeleton but bones tend to fracture easily. Encroachment on the marrow space leads to a leucoerythroblastic anaemia. There is mental retardation and early death. In the mild form, there may be only X-ray changes, but fractures and infection can occur. The acid phosphatase level may be raised. Stem cell transplantation has been successful.
 Scheuermann's disease
Scheuermann's disease
This disease predominantly occurs in adolescent boys. The main feature is a progressive dorsal kyphosis of the thoracic spine. Pain may or may not be present. The cause is unknown. A genetic predisposition, exacerbated by excessive exercise prior to epiphyseal fusion, is one suggested explanation. Older patients with kyphosis may be referred with suspected osteoporotic fractures but found to have long-standing kyphosis due to Scheuermann's. Management is focused on postural exercises and avoidance of precipitants. Surgery may be undertaken to correct kyphosis in severe cases.
Significant websites
http://nof.org National Osteoporosis Foundation – useful clinicians' guide.
http://www.iscd.org International Society for Clinical Densitometry – guidelines on DXA scanning.
http://www.nos.org.uk/ UK National Osteoporosis Society – useful information and reviews of ongoing research.