1 Conquering a Pandemic That Raged from Antiquity to the Eighteenth Century
In the history of the war between pathogens and humans, there are two eras. In the first era, the subject of this chapter, humans were suffering from the misery of infectious disease but didn’t know what caused them or how to mitigate their effects. Our ancestors observed, however, that individuals who recovered from these diseases did not get the same disease again, and thus could serve as caregivers during an outbreak. We will begin by briefly describing the earliest ideas regarding the origins of this observation, which we now understand to be acquired immunity. The attempt to harness this observation for human good is the history of vaccines. We will describe how the first era of our eternal battle with infectious diseases ended with one of the major achievements of medicine, the vaccine against smallpox. We will tell the tale here of how this procedure, which ultimately eradicated the scourge of smallpox from the planet, was developed slowly by several cultures on different continents in an empirical way without any understanding of how or why it worked. The following chapters will describe the second era when we learned about the origins of infectious diseases and how to combat them.
The Earliest Ideas
Spirits, Demons, and Divine Punishment
We are an inherently curious species. So, the observation that once someone recovers from a disease like smallpox they are not afflicted again led to ideas attempting to explain what was going on. In ancient civilizations (e.g., India, Egypt, and Mesopotamia) diseases were considered to be a punishment from God for sins that a person had committed. In India, upon being afflicted with smallpox, people prayed to a specific incarnation of God called Sitala. This custom is still followed in India when someone in the family has chicken pox or measles, presumably because these diseases also result in skin rashes and pustules that look like liquid-filled raised bumps on the skin.
Not surprisingly, it was speculated in ancient times that individuals who recovered from a serious illness had sinned less than those who succumbed. The reason why one was protected from a disease after recovering from it was because the sufferer had been sufficiently punished. The reason for subsequently being afflicted with other diseases was presumably that the person must have gone on to commit other sins.
Spirits, demons, and celestial objects were also considered to cause diseases. The name “influenza” is derived from the Italian word for influence because the disease was thought to be caused by the influence of stars. Similarly, in Europe, syphilis was supposed to have been caused by an evil conjugation of planets. One implication of the idea that spirits and demons caused diseases was that one could be protected from them by practicing the right rituals. One of the authors (AC) had firsthand experience with such practices. After AC’s infant sister died of pneumonia in 1968, his educated but distraught mother visited a “Man of God.” This man provided her with an amulet that AC was made to wear to protect him from disease-causing spirits. AC does not remember when in college he stopped wearing it or whether he was admonished by his mother for this action. He has not been struck with terrible illnesses since he stopped wearing the amulet!
Spirits, demons, celestial objects, and divine punishment are not the causes of infectious diseases. The appeal of these earliest ideas regarding the origins of disease and acquired immunity is their simplicity and the peace of mind that comes from taking action to prevent disease. This is why similar ideas persist to present times in some segments of society.
Expulsion or Depletion
Physicians had also started thinking about why people were not usually infected by smallpox after recovering from illness. One type of explanation is the expulsion theory. An example is one attributed to the great Persian physician and scientist Abu Bekr Mohammed ibn Zakariya al-Razi, who lived in the ninth and tenth centuries AD. His name, al-Razi, means that he came from a city, Rey, near Tehran. During his lifetime, he achieved great fame as a physician with his evidence-based approach to examining disease and evaluating various therapies. He was the first to distinguish between smallpox and another skin disease, measles. Besides his many seminal contributions to medicine, he was also a scholar of grammar and other diverse fields. His work in medicine was influential throughout the Islamic world and beyond.
In al-Razi’s view, smallpox afflicted young people because they had too much moisture and this led to fermentation of blood. The products of this fermentation process caused pustules to form, and when they burst the liquid that was expelled was the excess moisture. Given this explanation, it was also clear why smallpox did not recur; people who recovered no longer had excess moisture.
Many other explanations of a similar vein were proposed over the years. Girolamo Fracastoro (1478–1553), proposed that seeds (or seminaria) that arose spontaneously in a person, earth, or water were the cause of diseases like smallpox. The disease was transmitted from one person to another by transfer of seeds. To explain acquired immunity to smallpox, he posited that all humans were “contaminated” with menstrual blood during birth. When seeds emerged in a person, it caused this contaminant to putrefy or decay. After recovery, one could not be afflicted by smallpox again because the putrefied menstrual blood was expelled in the smallpox pustules. Variants of this theory included ones where, instead of menstrual blood, other fluids from the birth process were considered to be the contaminants that putrefied and were expelled upon infection with smallpox seminaria. It is interesting to speculate on why the birth process had such a powerful influence on the worldview of some early physicians.
Girolamo Mercuriale (1530–1606), a contemporary of Fracastoro, pointed out several problems with the expulsion theory. If the need for expulsion of menstrual blood contamination was the cause for smallpox, why were only humans, and not other mammals, afflicted with smallpox? Why did smallpox not exist in Indigenous populations before the Europeans brought it to the Americas? Since the menstrual blood contaminant had been expelled by smallpox, why was there not protection from all diseases after recovery from smallpox? Mercuriale was logically testing the expulsion model to see if it made sense and whether it was consistent with all the data, and found it wanting.
By the way, this is a good example of how science progresses. A model is proposed to explain certain observations. The model is then found to be inadequate for describing new observations. The model is then modified to accommodate the new data, leading to newer predictions. This is exactly what we witnessed in real time when epidemiological models continually revised estimates of deaths due to COVID-19 as new data became available and lockdown measures started to take effect.
New models that were proposed in the seventeenth and eighteenth centuries to account for observations not explained by the expulsion theory continued to rely on disease-causing seeds, but proposed a different function for the seeds. This class of models was called depletion theories. One version of this type of theory, proposed by the English physician, Thomas Fuller (1654–1734), posited that individuals were born with various kinds of “ovula” (like seeds) and that each corresponded to a particular disease. When the appropriate seed was germinated, it gave rise to a specific disease. Upon recovery from the disease, this seed was depleted, and one could not subsequently be afflicted by the same disease. But the seeds for other diseases remained. This model builds on the seed idea and now easily explains why we are protected only from diseases from which we have recovered.
As new observations became available, the depletion idea also became untenable. When a scientific model cannot be modified further to account for new information, there is a crisis because the old model has to be completely abandoned. Then, in what the philosopher Thomas Kuhn referred to as a paradigm shift, a new model is put forth. In later chapters, we will describe the paradigm shifts that led to our modern understanding of infectious diseases and immunity. For now, let us turn to the history of the devastation caused by smallpox, and how it was vanquished by human ingenuity and informed public policy.
A Brief History of Smallpox
From Antiquity to the Early Eighteenth Century
Smallpox is a viral infection that was not only lethal but also horrifying for the patient. It usually began with a high fever, malaise, and muscle and headaches. That would last for 3–4 days. Then a rash and pustules would develop in the mouth, tongue, and throat. Over the next 24 hours, the rash would then progress to cover other parts of the body. Over a few days, the pustules would increase in size and eventually burst. During this second phase, about 30 percent of those infected would die. Those who survived were often left with a disfigured appearance because of severe scarring of the skin and a loss of skin pigment. Their appearance was proof that they had recovered from the disease and would not be afflicted by smallpox again. Thus, they could safely care for the sick. Fortunately, the COVID-19 disease does not leave visible scars, but this means that scientific tests are required to prove that one has been exposed to the disease and is protected for some time.
It is believed that smallpox started to afflict humans in about 10,000 BC. Concrete evidence for its existence in humans 3,000 years ago is provided by Egyptian mummies with signs of the disease. A medical book written in roughly AD 400 in India describes the classic symptoms of the disease, the appearance of pustules on the skin of patients. The first description of smallpox in Europe is in the writings of Bishop Gregory of Tours around AD 580. With the start of European exploration in the fourteenth century, smallpox was spread to Africa and Asia. By the seventeenth century, smallpox was among the top two killer diseases in Europe. In 1849, 13 percent of all deaths in the Indian city of Calcutta (where one of us was born) were due to smallpox, and between 1868 and 1907 over 4 million people in India died of the disease. Globally, it is estimated that, just in the twentieth century, smallpox caused 300 to 500 million deaths, with roughly 50 million people afflicted every year as recently as the 1950s. These numbers indicate a level of devastation greater than the enormous damage already caused by the COVID-19 pandemic.
Smallpox was brought to the Americas by the Spanish in about 1520 with devastating consequences. It is estimated that between 60 and 90 percent of the population of the New World was decimated by the virus. The extremely high mortality rate in the Americas was probably due to the simultaneous introduction of other highly infectious viruses like measles that the native population had never seen. Smallpox also influenced the outcome of wars. Infected with smallpox, the Aztec armies had no chance against the invading armies of Cortes.
Smallpox epidemics occurred regularly in American cities. Between 1636 and 1698, Boston had six epidemics. The Boston epidemic in 1721 was so severe that many fled to other colonies, thus spreading the epidemic. The epidemics in Boston and New York in the early twentieth century (1900–1903) led to the establishment of government quarantine facilities and mandatory vaccination programs.
The devastating smallpox and plague epidemics led our ancestors to make an important observation. In 430 BC, during the plague of Athens, the Greek historian Thucydides noted that those who recovered from the disease could become caregivers to the sick without consequence. Throughout history, there are many other references to individuals being protected or exempt from a disease after recovering from it. People who had recovered began to be referred to as “immune,” derived from the Latin word immunis for “exempt.”
The observation of immunity inspired our ancestors to devise procedures to try and protect the healthy from smallpox. The Chinese began practicing a procedure to protect people from smallpox as early as AD 1500. The procedure involved collecting scabs from individuals who had a mild form of the disease. The scabs were then converted to a powder. About a month later, it was administered by inhaling powder nasally through a silver tube, left nostril for females and right for males. A week after this procedure pustules formed in the mouth and skin. It was hoped that these symptoms would not be as severe as the full-blown disease or cause death, but this was not always the outcome. Importantly, people who had successfully undergone the procedure did not get the disease when epidemics occurred.
Europeans encountered a similar procedure being used in India in the seventeenth century. Here, the fluid from smallpox sores and scabs was collected, stored for a while, and ultimately mixed with cooked rice to form a paste. Several punctures were made in the skin (arm or forehead) of a healthy person with a needle. These needle punctures were then covered with the paste made with rice. This method spread from India to other parts of Asia and the Balkans.
The methods developed by the Chinese and Indians came to be called variolation. The story of how variolation was brought to Europe is interesting, and many detailed accounts are available. Our story begins by noting the establishment of the British Royal Society in 1660. It is the oldest scientific academy in continuous existence. Because the Royal Society was a prominent entity, many scientists would send their important observations to the Fellows of this society. In 1700, the Royal Society received two letters from British subjects in China describing the Chinese variolation procedure. Neither communication led to any interest among the Fellows, perhaps because of the perceived risk in infecting an otherwise healthy person with diseased material. In December 1713, similar information about variolation was received in a letter from Emmanuel Timoni, a physician who practiced in Constantinople and whose patients included the British ambassadors there. Unlike in 1700, this letter did elicit interest in the variolation procedure.
Enter Mary Wortley Montagu. She was the wife of Edward Wortley Montagu, the British Ambassador in Constantinople. Her brother died of smallpox, and she herself was badly scarred by the disease. Mary Montagu witnessed variolation in Constantinople and given her personal encounters with smallpox developed a keen interest in the procedure. She decided to have her young son variolated by Dr. Charles Maitland, who was serving the British embassy in Constantinople. When she returned to England, she tried to champion the procedure. In 1721, a major smallpox epidemic broke out in London. Fearing for the life of her younger daughter, Montagu requested Maitland to carry out the procedure on her daughter. Maitland carried out the procedure. Members of the Royal College of Physicians were there to observe the procedure and its successful aftermath.
During the 1721 smallpox epidemic in England, a child of Caroline, the Princess of Wales, fell ill. Although it turned out that the child did not have smallpox, the princess got interested in variolation. While there is controversy as to who played the most prominent role, Montagu, Maitland, and Hans Sloane, Bart (the president of the Royal College of Physicians) all played important roles in promoting variolation among the royal family in England. Thus began what was likely the first “clinical trial.” The trial was to be carried out with six condemned prisoners in Newgate Prison in England. In exchange for participating in the trial, the prisoners were to be pardoned afterward. After being variolated in August 1721, five of the prisoners got symptoms of the disease but recovered. The sixth did not get symptoms, and it was then learned that this individual had recovered from smallpox the previous year. One of the women who had been successfully variolated was then sent to care for a child who was afflicted with smallpox. In spite of living in close quarters and tending to the patient, the variolated woman did not fall sick, further validating the efficacy of the procedure. All six prisoners were freed.
Despite the success of the variolation trial with prisoners, Princess Caroline still wondered whether the procedure was safe for her children. To further convince herself that the procedure was safe, the Princess then sponsored the variolation of five orphan children. Variolation did not harm these children. In April 1722, Princess Caroline, now convinced about the safety of the procedure, had two of her daughters variolated. This popularized the procedure among the upper classes of British society. Variolation was tried in Boston around the same time as the clinical trials in England. Benjamin Franklin became a strong proponent of the procedure.
The events of 1721 and 1722 were covered extensively by the press, which helped convince the public that variolation was a safe procedure. It is impossible to overstate the importance of clinical trials for establishing the safety and efficacy of any new vaccine even today. As we will describe in chapter 7, the time required to carry out proper clinical trials is one of many reasons why developing and deploying a new vaccine takes so long. Viewed from our modern perspective of ethics and morality, selecting prisoners and orphans as the subjects of the clinical trials seems highly unethical. Now, of course, participants in clinical trials of vaccines are healthy volunteers, who participate with full knowledge of the risks.
Variolation was practiced in a way that was traumatic for the person being inoculated. The individual was bled and given very little to eat before the procedure was carried out. Variolation involved the preparation of material taken from a person who was infected. We now know that this material contained the smallpox virus. So, even if the inoculum was prepared by an experienced practitioner, serious or lethal illness could ensue. Variolation also resulted in localized outbreaks of smallpox on occasion. Variolated people were therefore housed together after the procedure to prevent spread of the disease. The danger inherent in the variolation procedure and the trauma to the person being inoculated were reasons why variolation was not widely practiced, and most people remained unprotected from smallpox infections. All of this changed with the work of Edward Jenner, who incidentally had been variolated as a child.
Edward Jenner’s Paradigm Shift
Jenner was born on May 17, 1749, in the Gloucestershire town of Berkeley in England. After completing his early education and apprenticeship to an apothecary, Jenner became an early student of John Hunter, a Scottish surgeon and doctor. Hunter and Jenner shared many interests, including studying species that hibernated and the migration of birds.
After completing his work with Hunter, Jenner returned home to Berkeley in 1773. It is believed that a milkmaid told Jenner that she did not respond to variolation because she once had cowpox, a relatively harmless disease in cows and humans. He also heard about this phenomenon from John Fewster (1738–1824), a medical colleague in Gloucestershire who noticed that a young man who had previously been infected with cowpox did not react to variolation. Jenner began to study the connection between cowpox infection and protection from smallpox. These studies took time because cowpox outbreaks in dairies and farms were infrequent. Jenner’s studies led him to believe that the origin of cowpox was a disease called “grease heel,” which caused inflammation in the skin of horses, and he thought it was transmitted to cows by farmworkers who tended both horses and cows. In cows, the disease affected the nipples and it was passed to dairymaids while milking the cows. It is legend that dairy maids have fine complexions that were envied by noblewomen. The basis of this legend may be that because their exposure to cowpox left them immune to smallpox their faces were not pockmarked.
With his mentor Hunter’s encouragement, Jenner did an experiment to test whether cowpox inoculation could protect humans from smallpox. On May 14, 1796, Jenner used the variolation procedure to inoculate a boy called James Phipps with pus from a sore of a cowpox-infected milkmaid named Sarah Nelmes. Because this event was so momentous in medical history, we also know that the name of the cow that infected Nelmes was “Blossom.” Two months later, Jenner repeated the variolation procedure on Phipps, but now he used smallpox. When no symptoms appeared, his hypothesis that cowpox inoculation could protect a person from smallpox was validated. He would repeat the procedure with a small number of individuals two years later.
Jenner’s experiment represented a paradigm shift in the human endeavor to protect people from infectious diseases. His new paradigm was that one could protect an individual from a deadly illness by inoculating with a material derived from a relatively harmless (for humans) related disease. Thus, unlike variolation, the procedure was largely safe for healthy people.

Jenner described his work to the British Royal Society, and he tried to publish a paper based on his findings in the society’s prestigious journal, Philosophical Transactions, which still exists today. In spite of the fact that Jenner was a Fellow of the Royal Society, the Royal Society rejected his paper. They felt that Jenner did not have enough evidence for his claims, and he might do irreparable damage to his reputation by publishing the work before he had definitive proof. Jenner had his findings published by the private firm of Sampson Low. Presumably, he made money from the sales of this book, which would not have happened if he had published his findings in the Philosophical Transactions.
The popularity of Jenner’s procedure began to grow. Richard Dunning, an early supporter of the procedure in England, proposed that the procedure be called vaccination because the Latin name of cowpox is Vaccinia. Pasteur later promulgated the use of this term for an inoculation procedure that protected humans from any disease. Ultimately, vaccination replaced variolation, and the latter procedure was made illegal in 1840 in England. Vaccination was made mandatory shortly thereafter.
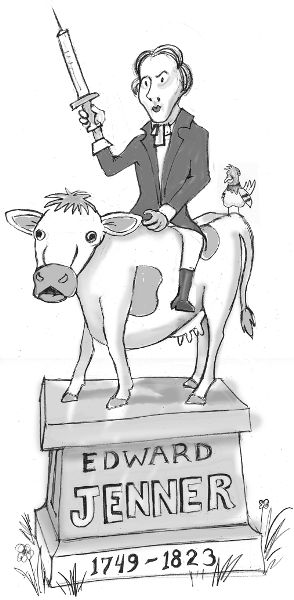
Jenner’s development of vaccination based on careful observation was a remarkable advance. It led to a safe procedure that protected millions of people from a disease that had caused frequent devastating epidemics over millennia. This huge advance in public health was recognized in Jenner’s lifetime with numerous honors from professional organizations in England and around the world. The French Emperor Napoleon was supposedly a big fan. Statues were built and poems were written to honor Jenner’s contribution to humankind. Jenner’s home is now a museum, as is the hut where Phipps was vaccinated. Remarkably, when Jenner did his work, we did not know that infectious microbes cause diseases or that we have an immune system. We will describe infectious microbes and how our immune system works in the next three chapters.
Eradication of Smallpox from the Planet
Throughout the twentieth century, Jenner’s smallpox vaccine was administered just like the variolation procedure. After applying the vaccine material, the surface of the skin was punctured repeatedly with a needle to induce a scab. The use of the smallpox vaccine spread around the globe with particularly strong efforts in the Western world. By the early twentieth century, smallpox had been eradicated in Northern Europe and only a small number of cases were reported in other European countries. In 1950, a group of health officials proposed an effort to eradicate smallpox in the Americas and largely succeeded within the decade. In 1958, the Soviet Union proposed that the World Health Organization (WHO) lead an international effort to eradicate smallpox worldwide. Efforts were mounted in almost every country using a novel strategy called ring vaccination. Following the identification of an infected person, every person who lived in the vicinity was vaccinated.
The last two countries with extensive caseloads were Ethiopia and Somalia. A stepped-up focus on these two countries finally succeeded in the eradication of smallpox from these countries in 1979. The last case of smallpox was the fatal infection of Janet Parker, a medical photographer, who contracted the virus from a laboratory that was doing research on smallpox. This resulted in the destruction of all known stocks of the virus except for two vials, one stored in the United States and the other in Russia. As the years passed by without any new smallpox cases, a raging controversy stormed through the scientific community about whether these last vials should be destroyed to literally eradicate smallpox completely from the planet. There was worry that if terrorists were to take control of these stocks and weaponize smallpox, without anyone in the world being immune, a devastating pandemic could take place. Others argued that for scientific purposes it might be necessary to draw on these stocks for some unknown future problem. This controversy was made moot in 2017, when researchers showed that it would be possible to recreate smallpox in the lab using existing methods.
What was the secret to eradicating smallpox, this centuries-old enemy of the human race? The first was the international cooperation of all countries of the world in understanding the horrific nature of smallpox infection and the importance of eradicating it from the earth. Can we now achieve a similar level of global coordination to create a more pandemic-resilient world? The other key was that the virus that causes smallpox did not infect animals. It infected only humans, and spread solely by human-to-human contact. As we will learn in a later chapter, the natural hosts for many viruses are animals, and that viruses can jump to humans when they change in a way that allows them to infect and/or reproduce in human cells. This is precisely what happened to cause the H1N1 influenza pandemic in 2009 and the COVID-19 pandemic. Eradication of a viral disease that infects animals would require the extermination of entire species of animals or finding a way to vaccinate them. Newer technologies have suggested approaches where genetically engineered insects or animals are released into the wild. These organisms are engineered to have the ability to breed with existing species and block the ability of specific pathogenic microbes to survive in their progeny. Whether this is a strategy that is worth trying or whether this may generate unexpected ecological changes is a difficult ethical issue with potentially dangerous environmental impact.
Early Opposition to Vaccination
The smallpox epidemics in Boston in the early twentieth century led the local board of health to start free vaccination programs. Much like flu shots today, one could get vaccinated for free in various locations around the city. In 1902, vaccination was made mandatory in Boston. Those who refused to be vaccinated were subject to a $5 fine or 15 days in prison. Henning Jacobson, a Swedish immigrant in Boston, refused to be vaccinated because he feared that it would make him sick. But, instead of paying the fine, he sued the state of Massachusetts on the basis that the mandatory vaccination program violated his rights. This case went all the way to the US Supreme Court, which ruled in favor of Massachusetts in 1905. The Court’s reasoning was that Jacobson’s refusal to be vaccinated endangered the health of others.
With improvements in vaccine quality, vaccination is now practiced widely. It is fair to say that vaccination has saved more lives than any other medical procedure. The sharp decrease in child mortality over the past century is primarily due to the success of vaccination programs. Polio, another disease caused by a virus, afflicted 60,000 people in the United States in 1952. Jonas Salk, and then Albert Sabin, developed vaccines that protected people from polio. Today, polio has been all but eradicated from the world.
But, the controversy over the use of vaccines still rages today in some quarters. As we will discuss later, when a significant fraction of the population is not vaccinated against specific diseases, outbreaks occur. Several parents choosing not to vaccinate their children against measles led to the recent outbreaks of this disease in California. High vaccination rates protect the public—in particular, vulnerable people like the elderly and the immunocompromised—by generating something called “herd immunity,” which we hear about so much during the COVID-19 pandemic. We will focus on these topics in later chapters.