INTRODUCTION
Fanny Burney was no stranger to pain. Best known for her novel Evelina, published in 1778, Fanny suffered from mastitis after the birth of her son, Alex, in December 1794. The pain was so intense ‘as to make life—even my happy life—scarce my wish to preserve!’ she wrote. Little did she know then that seventeen years later she would have to bear a mastectomy without pain relief. Her description of the operation, undertaken in Paris, is a moving testimony to the awful suffering patients endured in operations without anaesthesia. The first indication of the problem was a ‘small pain’ in her breast. Reluctant to seek medical advice, she was eventually persuaded by her husband, M. d’Arblay, to consult M. Dubois, the surgeon who had treated her for the breast abscess. Dubois’ opinion was that ‘a small operation would be necessary to avert evil consequences.’ ‘My dread & repugnance, from a thousand reasons besides the pain, almost shook all my faculties, &, for some time, I was rather confounded & stupefied than affrighted,’ Fanny recalled. As ‘the pains became quicker & more violent’ she sought a second opinion. M. Larrey, recently awarded a baronetcy for his services to Napoleons armed forces, prescribed a new regime of therapies which brought some improvement. However, his concern was strong enough to ask for a further opinion from the anatomist Dr Ribe and, as a last resort, Dr Moreau, a physician. But to no avail. After a final consultation between the doctors, Fanny was summoned to attend them. Seeing Larrey shrinking behind the sofa she realized ‘all hope was over … I now saw it was inevitable, and abstained from any further effort. … I was formally condemned to an operation.’ The doctors were unequivocal about the severity of the forthcoming operation: ‘vous souffrirez beaucoup’, warned Dubois. Ribe charged Fanny to cry and scream during surgery; any attempt to restrain herself could have serious consequences, he warned. But Dubois and Larrey refused to give Fanny more than four hours notice of the operation. They wanted to limit her anxiety, they said. When operations were performed at home, patients’ families often attended, but M. d’Arblay was too agitated; the doctors refused to have him present. To keep Fanny’s fears in check, a closet in the house was secretly filled with dressings, bandages, and compresses. Fanny made her will and appointed two women to attend her during the procedure. On the morning of 30 September 1811 Fanny received a letter from Larrey giving her two hours notice of the operation. ‘I will not be ready until 1 o’clock,’ she protested; in the event Dubois was delayed until 3 o’clock. Fanny waited; ‘the sight of the immense quantity of bandages, compresses, spunges, Lint —made me a little sick,’ she wrote. Finally ‘7 Men in black’ entered the salon. Dubois took charge, ordering a bedstead, old mattresses, and sheets to be placed in the centre of the room. Fanny later recalled, ‘every thing convinced me danger was hovering about me, & that this experiment could alone save me from its jaws.’ So she climbed on the bed and Dubois placed a thin handkerchief over her face. Its transparency permitted her to see the seven men and nurse gather round the bed, but when she saw ‘the glitter of polished Steel’ she closed her eyes, unable to watch ‘the terrible incision’. The experience was ‘a terror that surpasses all description, & the most torturing pain’, she wrote.
When the dreadful steel was plunged into the breast—cutting through veins—arteries—flesh—nerves—I needed no injunctions not to restrain my cries. I began a scream that lasted unintermittingly during the whole time of the incision—& I almost marvel that it rings not in my Ears still! so excruciating was the agony. … I then felt the Knife [rack]ling against the breast bone—scraping it!. I bore it with all the courage I could exert, & never moved, nor stopt them, nor resisted, nor remonstrated, nor spoke. When all was done, & they lifted me up that I might be put to bed. I then saw my good Dr Larry, pale nearly as myself, his face streaked with blood, & his expression depicting grief, apprehension, & almost horrour.
Fanny recovered but it was six months before she could begin to record her ordeal. ‘I dare not revise, nor read, the recollection is still so painful,’ she wrote to her elder sister Esther.1
Fanny’s account tells us clearly that operations were the last resort of surgeons and patients. Pain was not the only problem; the perils of blood loss and infection made all surgery life-threatening. Exposing a patient to such risks could only be justified when all other courses had been explored. When the diarist Samuel Pepys agreed to have his bladder stone removed in 1658, it was the only escape from ‘a condition of constant and dangerous and most painful sickness and low condition and poverty’.2 He knew he was fortunate to survive the operation: he preserved the stone in a special case and celebrated ‘operation day’ for the remainder of his life. And though anatomical knowledge and surgical techniques expanded considerably during the eighteenth and early nineteenth centuries, surgery remained a risky business. Major operations included amputation, hernia, ovariotomy, lithotomy (removal of bladder stones), trepan (cutting a hole in the skull to remove injured or diseased parts without disturbing the dura surrounding the brain), and many smaller procedures such as removing polyps or repairing fistula in the rectum. But most surgeons performed few operations. Records from Amsterdam suggest that on average, fewer than four lithotomies a year were performed between 1725 and 1821; a mortality rate of around 20 per cent indicates the risks involved. At large and prestigious London hospitals only a handful of major operations took place each month. University College hospital surgeon Robert Liston performed only two or three operations each month. Surgeon to the Royal Naval hospital in Plymouth, Stephen Hammick, undertook fewer than two amputations a month during his twenty-year career.
Because the risks of surgery were so high, an elaborate etiquette of medical consultations had developed. This was partly to ensure that patients were given every chance of alternative therapies: it also reassured surgeons that their decision to operate was sound. Larrey was not alone in reacting emotionally to Fanny’s operation. Walking to the operating room was like ‘going to a hanging’, John Abernethy, surgeon at St Bartholomew’s Hospital, told a friend: on occasion he was known to shed tears or vomit after a particularly terrible operation. Charles Bell spoke to his brother of ‘anxious feelings’ and ‘indescribable anxiety’. His fellow surgeon at the Middlesex Hospital, James Arnott, described Bell’s demeanour as ‘the reluctance of one who has to face an unavoidable evil’.3
The problem of surgical pain had occupied surgeons over many centuries and led to various experiments. At the end of the eighteenth century, the London surgeon James Moore designed a heavy steel clamp which compressed the limb before amputation. His hope was that the pressure on the nerves might succeed in diminishing pain. But patients complained that the sensations this mechanism caused were as painful as the operation itself. In London in 1813 James Wardrop bled a particularly nervous young woman until she lost consciousness in order to remove a tumour from her head. The procedure was successful—Wardrop taught medical students the technique—but most surgeons considered it dangerous. They believed that an operation placed severe stress on the body’s systems and understood pain as a vital stimulant which worked to protect the body during this risky time. Sometimes patients lost consciousness during operations because of the intense pain and blood loss—the condition was known as syncope. But to intentionally depress the body was believed to add to the inherent risks. The same argument limited the use of alcohol and opiates. Patients were often given a small dose either in advance or during an operation, but doping them to the point of unconsciousness was considered too risky. Nor did either drug succeed in calming the patient’s mind, which for most surgeons was the key problem as the mind was the source of fears, anxieties, and emotions.
Had Fanny’s doctors possessed a reliable method of pain relief we can be in no doubt that they would have offered it, and she would have taken it. Practitioners had always sought to relieve pain but within the classical medicine, developed in Greece in the fourth century bc, which dominated Western medicine until well into the nineteenth century, understandings of pain were very different from those we have today. In the classical view of the body, health and disease were understood to be determined by the balance of humours (fluids)—blood, phlegm, choler (yellow bile), and melancholy (black bile). These fulfilled specific life-giving functions within the body. Each person had a different and unique balance of these fluids which determined both constitution and personality. Physical appearance and temperament were explained by the predominant humour. A natural dominance of blood, say, produced a person with a red face and hasty temper; those with a natural excess of phlegm were pale-skinned and cool-natured. Amongst Chaucer’s pilgrims in the Canterbury Tales we find the sanguine Franklin who revels in meat and wine, and the thin, choleric Reeve.
Health was enjoyed when the humours maintained their natural equilibrium and patients often sought advice from medical practitioners on appropriate regimes for achieving this. Imbalance in one of the vital fluids produced sickness and could be remedied by lifestyle—diet and exercise—or by therapies that restored the body to its natural balance. Excessive quantities of yellow bile produced inflammation; too much blood resulted in fever. Noxious or excess fluids could be drawn from the body through vomiting, bloodletting, or emetics. Humoralism encapsulated the whole person. No differentiation was made between physical or psychological symptoms; a physician would take as much account of the patient’s state of mind as of a fever or rash. Medical consultations focused upon the individual patient. Specific diseases were described within medical theory, but both practitioners and patients believed strongly that health and sickness were individual experiences, distinct to particular bodies. Pain was believed to be a product of imbalance within the system and therapies like bloodletting were used in an attempt to draw the pain out of the body. It was taken to be a general indicator of ill-health and disease, rather than a specific entity which could be treated locally.
From the mid-seventeenth century onwards, the body’s nervous system became a focus for new research into the physiology of nerves and muscles. The Swiss physician Albrecht von Haller distinguished between nerves (endowed with sensibility, an innate capacity to communicate sensations) and muscles (endowed with irritability, a kind of nervous power that resided in the muscles). Robert Whytt in Edinburgh confirmed that sensibility was located in the nerves and explained reflex as being caused by an unconscious sentient principle located in the spinal cord and brain which stimulated the muscles and caused movement. His work put a new stress on cerebral functions which was to prove crucial to understanding the later process of anaesthesia.
By the later eighteenth century, physicians like William Cullen, Professor at Edinburgh University, were convinced that the nervous system was pivotal to understanding health and sickness. ‘Almost the whole of the diseases of the human body might be called nervous,’ proclaimed Cullen.4 Sensibility was understood to vary by degrees in different people, according to the natural capacity of their nerves to receive and transmit sensations, and the irritability of their muscles. Imbalance of irritability, or excitement as it was called, became the new way of interpreting sickness. A certain degree of ‘excitement’ in the body was necessary for healthy functions; too little or too much put the body out of balance. Following the patterns of opposites established in humoral medicine, practitioners explained their treatment of sickness as a rebalancing of these dynamics. Depressants—bloodletting, emetics—restored health to patients suffering from excessive excitement. Stimulants like opiates or alcohol and ‘shock’ therapy using electricity returned excitement to a depleted body. Some patients lapped up these new ideas: ‘I have no Fever at present, I have head-Ache, and Indigestion, & I have lately been convinc’d that I have Nerves,’ wrote one sufferer.5
The new vogue for sensibility coloured the literature of the day, especially that of Laurence Sterne and Samuel Richardson. The prolific cast of characters filling the pages of The Life and Opinions of Tristram Shandy (1759–67) are absorbed by their engagement with the outside world. The view that feelings, rather than reason, should inform morals and social structures began to be expressed by philosophers and politicians. Scottish philosopher David Hume’s moral, political, and literary essays, published in 1742, stressed how developing fine sensibilities lay at the root of self-improvement. Man’s judgement, he wrote, ‘may be compared to a clock or watch, where the most ordinary machine is sufficient to tell the hours; but the most elaborate alone can point out the minutes and seconds, and distinguish the smallest differences of time’. A well-developed judgement meant that an individual ‘feels too sensibly, how much all the rest of mankind fall short of the notions which he has entertained’.6 As sensibility emerged as a yardstick of civilization, man’s flesh and bones grew increasingly vulnerable to painful sensations.
From the mid-eighteenth century onwards, British use of opiates rose dramatically, suggesting a growing sensibility to pain. Doctors engaged with pain in a new way. For centuries, death had been viewed as a spiritual experience and the pains of the last hours or days of life were to be born in the expectation of divine redemption through eternal life. Patients’ physical needs were cared for, but attention focused on confession and priestly absolution. As opiate use grew, so did the attendance of doctors at the bedsides of the dying. Opiates were part of a package of care; doctors also held patient’s hands and uttered soothing words. Religion was not pushed away from the bedside; in fact medicine became its enabler. Pain relief gave patients a chance to resolve earthly matters without physical distractions. The Welsh physician John Jones’s The Mysteries of Opium Reveal’d (1701) made no bones about its positive effects: ‘causes a brisk, gay and good Humour … Serenity, Alacrity, and Expediteness in Dispatching and Managing Business … Ovation of the Spirits, Courage, Contempt of Danger. takes away Grief, Fear, Anxieties, Peevishness, Fretfulness … charms the Mind with Satisfaction, Acquiescence, Contentation, Equanimity, &c.’ Commitment to the Divinely ordained suffering of childbirth also began to erode. Though not widely promoted—probably for fear of opposition, either real or imagined—some doctors began to use opiates in labour. But addiction to opiates was common. Toothache and neuralgia first prompted the Romantic poet Samuel Taylor Coleridge to take opium; he soon became dependent on its life-enhancing effects. Opium addiction cost him his marriage, severed his relationship with fellow poet William Wordsworth, and eventually contributed to his death. Thomas de Quincy’s no-holds barred account of addiction, The Confessions of an English Opium Eater (1821), became a best-seller. Part of the attraction, of course, was opium’s power of restoring youth and possibilities to the aging. It is impossible to determine whether the increased use of opiates was a cause or effect of a decreased social tolerance of pain. Nevertheless these fundamental schisms in old ideas of pain as functional and integral to healing spread through Europe. The Napoleonic wars give easy evidence of the strong political and military divide between France and England at the beginning of the nineteenth century, but the two nations shared a growing intolerance to pain: imports of opiates to France rose by 50 per cent between 1803 and 1807.
For Enlightenment optimists, medicine was crucial in the quest for perfectibility. Knowledge of disease and new therapies appeared to be powerful tools in the brave new world. The new gas chemistry, spearheaded in Britain by the political radical Joseph Priestley, promised revolutionary treatments. A mouse was the first to breathe the new kind of air, isolated by Priestley in 1774 and later called oxygen. Breathing the new air himself, Priestley noticed the effects on his chest: it felt ‘particularly light and easy for some time afterwards’.7 The dangers posed to health by ‘bad air’ from natural environments such as marshes or stagnant water had been stressed by Hippocrates centuries earlier. By the eighteenth century, air quality was high on the medical agenda. The army physician John Pringle considered outbreaks of fever epidemics and scurvy in soldiers’ camps to be linked to the putrid air of the nearby marshes. Using Priestley’s new breathable airs to cure disease was an obvious route to take. It fell to Thomas Beddoes to test out this ‘pneumatic medicine’ which was to establish how gases had the power to transform bodily states.
Son of a well-to-do Shropshire tanner, Thomas Beddoes went to Oxford and then studied medicine in London and Edinburgh. He took up a chemistry post at Oxford and embraced the new French chemistry pioneered by Antoine Lavoisier that paralleled Priestley’s work in researching the ‘different kinds of air’. Fervent about the rights of man and the freedom to think independently, Beddoes developed close links with members of the Lunar Society of Birmingham including Joseph Priestley, Erasmus Darwin, Josiah Wedgewood, and James Watt. But after the French Revolution, when Britain went to war with France, known radicals were targeted by mobs. In 1791 during the Birmingham Riots, Priestley watched the destruction of his house, garden, and laboratory. Instruments were destroyed, books and manuscripts burnt: ‘I afterwards heard that much pains were taken, but without effect, to get fire from my large electrical machine, which stood in the library,’ he wrote.8 Beddoes’ own enlightened ideals were out of step for Oxford; he quit his post. Moving to Bristol in 1793, then a stronghold for political radicals, he sought to fulfil his dream that the new gases like oxygen could cure diseases like tuberculosis. Less than a year later Beddoes married Anna Edgeworth, daughter of Lunar friend Richard Lovell Edgeworth. The match surprised friends: Anna’s cheerfulness, gaiety, and wit were the antithesis of Beddoes’ fiery outspokenness. Nevertheless she engaged wholeheartedly with Beddoes’ political and pamphleteering activities. Just as the Lunar circle had supported Priestley’s researches with funding and equipment, so they mustered arms to launch Beddoes’ dreams. On 21 March 1799 a notice in the Bristol Gazette announced a new medical institution that would treat incurable diseases like consumption, asthma, palsy, dropsy, and venereal conditions. It promised methods that were not painful, nor hazardous. The Pneumatic Institute was funded by subscriptions (mainly the Lunar circle) and offered free treatment. It became a honeypot to the Romantic poets Robert Southey and Samuel Taylor Coleridge, and radicals like Davies Giddy (later President of the Royal Society).
Pragmatically, Beddoes hoped to develop his methods by testing them on poor patients. Beddoes’ rationale was developed through his own experience of respiring oxygen for several months: he lost weight, became flushed in the face, and suffered nosebleeds—typical characteristics of consumption. It seemed to him that excessive oxygen had caused the symptoms of consumption. Scurvy, he believed, was caused by too little oxygen. Rebalancing the components of the air in a body by respiring a particular gas seemed a logical way of restoring health. He recruited a young, untrained chemist to help run the Institute—Humphry Davy, later to become the most famous chemist of his generation. Beddoes was an ‘uncommonly short and fat, [man] with little elegance of manners, and nothing characteristic externally of genius or science’, Davy wrote to his mother after meeting his new employer.9 Nevertheless the two men shared a conviction that chemistry was the source of life’s powers and forces—Davy’s earlier research into the nature of heat and light was built on that principle. One of the gases Davy researched as part of Beddoes’ quest to discover a cure for a ‘catalogue of diseases’ was nitrous oxide.
Isolated by Joseph Priestley in the 1770s and called ‘dephlogisticated nitrous air’, nitrous oxide had been investigated by New York chemistry professor Samuel Mitchill: the ‘gaseous oxyd of azote’ was lethal if inhaled, suggested Mitchill. Davy’s plan to investigate its composition, properties, and mode of operation on living beings was nothing less than audacious. After a succession of chemical experiments Davy turned to animals. How would nitrous oxide affect the nervous system; what were the differences between warmand cold-blooded creatures? Through the process of respiration, he believed the gas would enter the blood and travel through the body. One lizard placed in a jar of nitrous oxide lay on his back with his paws resting on his belly ‘seemingly dead’, yet recovered when placed in shallow water. Davy observed that this lifeless state was preceded by a period of intense activity in the creature. This sequence of stimulation followed by depression was also seen in rabbits, mice, fish, flies, snails, and earthworms. Reassured that nitrous oxide did not cause instant death, Davy breathed it himself: ‘I was aware of the danger,’ he wrote, anticipating that he might feel painful or depressing sensations. On the first occasion he felt intoxicated and his pulse increased. The next day he breathed again and this time he experienced the gas’s ‘extraordinary powers of action’. He felt a gentle pressure on his muscles and a ‘highly pleasurable thrilling’ extended across his chest and extremities, he said. Under its influence a world of subdued hues was cast into dazzling technicolour. His hearing became more acute, ‘the thrilling increased, the sense of muscular power became greater, and at last an irresistible propensity to action was indulged in’, he recorded. From this point Davy was utterly absorbed by nitrous oxide. He breathed different quantities for different lengths of time and at different times of the day, on each occasion noting the effects on his pulse, sleeping, and senses. He tried it after consuming a bottle of wine, before eating, and after eating. Sometimes he breathed the gas three or four times on the same day. He noticed it relieved minor aches and pains. On the most memorable occasions he experienced ‘sublime emotions connected with highly vivid ideas’.10 Friends and visitors to the Institute were urged to participate in this new world. Rather than revolutionizing medical treatments, nitrous oxide revolutionized individual sensibilities by producing: ‘a delirium of pleasurable sensations’, enthused Robert Southey after breathing the gas.11
The sensations of nitrous oxide fanned the self-interest of Enlightenment figures but capturing the experience in words proved almost impossible. How can such ‘new and particular sensations’ be expressed in the confines of existing vocabulary, mused word-lover James Thomson, later to write the thesaurus. Even sceptics like Josiah Wedgwood were captivated by its powers: he experienced the ‘most singular sensations’ which made him feel ‘lighter than the atmosphere’, as if he were about to ‘mount to the top of the room’, he wrote.12 Some found themselves on the fringes of addiction: ‘I went on breathing with great vehemence, not from a difficulty of inspiration, but from an eager avidity for more air,’ affirmed J. Tobin. Stephen Hammick refused to let Davy take the bag away, so pleasurable was the feeling.13 Just seeing the bag caused Davy to desire the gas.
Opium addiction was a problem of the times and addicts found it brought dreadful depressions in its wake. Nitrous oxide left no such dark legacy but recollections of ‘more unmingled pleasure than I had ever before experienced’, wrote opium user Samuel Taylor Coleridge.14 That a chemical had the power to intensify engagement with the natural world harmonized with Enlightenment philosophies. But the nitrous oxide experiments brought no therapeutic breakthroughs. The conservative outcry against the French Revolution and all things French tarred gas chemistry and other radical pursuits such as mesmerism—later tried as a method of surgical pain relief—as subversive and dangerous. Davy sensed this shift and in the last few pages of his work on nitrous oxide, written in June 1800, he noted disconsolately that the common theory of excitability ‘is most probably founded on a false generalisation’ as variations of diseased action may be ‘infinite and specific in different organs’ and thus beyond the power of agents which acted on the whole system.15
The Pneumatic Institute was of its moment. Davy left to follow his star at the Royal Institution; a typhus epidemic hit Bristol, and Beddoes became caught up in treating its victims. Afterwards Beddoes restructured the Institute into a Preventive Institution to help the sick poor. Gas chemistry, the hoped-for panacea, lost its appeal in the cool light of a conservative dawn.
Davy’s work plays an important role within the history of anaesthesia. He proved that gases could change bodily states. But we should not be surprised that Davy did not leap upon nitrous oxide as a potential anaesthetic: he was a product of eighteenth-century bodily understandings. The possibility of suspending sensation without endangering life could not be imagined within the 1790s’ configurations of the nervous system: the associations and interdependence between sensibility and irritability were too complex to disentangle. Pain was thought integral to the body’s functions, and essential to healing. Davy thought it possible that sensation could outlive all other powers of the body: his greatest fear was of being buried alive and he exacted a promise from his brother that upon Davy’s death, there would be a ten-day period of grace before burial. There is no doubt that Davy would have applied the powers of nitrous oxide to surgery had he thought this plausible. His suggestion that the gas might play a role in surgical operations where there was minimal blood loss was made on the basis of its stimulatory characteristics. It would be equivalent to small quantities of opiates or alcohol found to be helpful in reviving patients debilitated from the stress of an operation. But although physiology offered no solution to the problem of pain, the philosophies underpinning its role in society had begun to shift.
In Christian theology, pain entered the world after Eve’s disobedience in the Garden of Eden and remained central to humanity. Over the centuries, mankind sought to alleviate physical suffering yet also accepted its inevitability. But during the eighteenth century there was a key shift in both social and medical attitudes to pain. A new attention to feeling and alleviation of painful sensations crept in on the back of Enlightenment philosophies and spread through Europe. The radical realignment placed sensibility as the crux of moral behaviour and drove a raft of reforms focusing on particularly vulnerable groups: slaves, animals, prisoners, and children. It was underpinned by the new physiology which viewed the nervous system as the body’s primary interface with the outside world. In England, the 1780s marked the beginning of the campaign by William Wilberforce and his associates to abolish the Slave Trade: in the Austrian Empire, Joseph II, brother of Marie-Antoinette, abolished serfdom and the death penalty. Sensibility equated to civilization: ‘Am I not a man and a brother?’ asked the black slave depicted on the yellow jasper medallion manufactured by Josiah Wedgwood for the Society for the Suppression of the Slave Trade. The new awareness that all races experienced pain (though some less than others) also extended to animals. England was notorious for its violent and bloody sports. Bull, dog, and bearbaiting, cock-fighting, and boxing had entertained generations on feast and fair days since medieval times. Some observers like the seventeenth-century diarist John Evelyn disliked the ‘barbarous cruelties’ of such sports. Once when passing the main London bear-garden, Paris Garden in Bankside, Southwark, Evelyn saw a bull toss a dog so high in the air it landed on the lap of a lady sitting in a box above the arena. The Puritans attempted to stop bearbaiting, though in his History of England, Thomas Babington Macaulay suggested that this was not on account of the pain caused to the bear, but rather the pleasure given to the spectator.
The moral philosophy upon which the shift against cruelty to animals was built may seem natural to us: that animals, as well as humans, have an innate capacity to experience pain. Thus, every body, be it of man, mammal, or insect, operated within the same dynamic framework of anatomy and physiology and was vulnerable to suffering from unpleasant physical sensations. But it challenged long-held views about man’s superiority on the basis of his reason, speech, and soul. The Church of England clergyman Humphry Primatt was one of the first to express views about animals: ‘pain is pain, whether it be inflicted on man or on beast; and the creature that suffers it, whether man or beast, being sensible of the misery of it while it lasts, suffers evil,’ he wrote in A Dissertation on the Duty of Mercy and the Sin of Cruelty to Brute Animals (1776). Primatt supported his arguments with many references to the Bible: neither colour nor species justified the enslavement or tyranny of other living beings. Sensibility was common to all. Animals, noted Primatt, are ‘no less sensible of pain than a man. He has similar nerves and organs of sensation.’ Primatt’s views spread.
The Dorset clergyman John Toogood appended part of Primatt’s text to his sermon published in the 1790s. Promoted as a ‘Shrovetide gift to his parishioners’, Toogood was no doubt trying to refocus the long history of animal baiting on feast days. Primatt’s arguments underpinned later debates on animals and pain. The moral question about animals, wrote the philosopher Jeremy Bentham in his Introduction to the Principles of Morals and Legislation (1789), ‘is not, Can they reason?, nor Can they talk? but, Can they suffer? Why should the law refuse its protection to any sensitive being? The time will come when humanity will extend its mantle over everything which breathes.’ For Bentham, sensation was the key to determining both moral behaviour and legislation:
Nature has placed mankind under the governance of two sovereign masters, pain and pleasure. It is for them alone to point out what we ought to do, as well as to determine what we shall do. On the one hand the standard of right and wrong, on the other the chain of causes and effects, are fastened to their throne. They govern us in all we do, in all we say, in all we think.
Child of the Enlightenment, Bentham drew on the philosophies of John Locke and David Hume amongst many others. He also acknowledged his debt to Joseph Priestley with whom he had corresponded on chemical experiments: ‘Priestley was the first … who taught my lips to pronounce this sacred truth:—That the greatest happiness of the greatest number is the foundation of morals and legislation.’ Bentham’s felicific calculus became a powerful influence on nineteenth-century conceptions of liberty and the state developed by the philosopher John Stuart Mill among others.
From the 1800s new research into the brain’s anatomy and physiology started to reshape old understandings of sensation. Work by the British physician Charles Bell and French physiologist Francois Magendie in the 1810s established that different parts of the brain were responsible for specific functions and showed how sensations and movement were carried by different nerves. Another Frenchman, Marie Jean-Pierre Flourens, performed a series of experiments on pigeons in 1824 which demonstrated the specificity of functions. When a pigeon lost both cerebral hemispheres it became blind; losing only one hemisphere caused blindness in the opposite eye. The idea that bodily functions could be specifically located within the brain, and that processes like respiration and circulation could operate independently, later became the basis for the science developed around the anaesthetic process. But at this point, the knowledge that sensations were controlled by nerve centres in the brain, rather than the spinal cord, caused some surgeons to think differently about the pain of surgery.
‘There is not an individual who does not shudder at the idea of an operation, however skilful the surgeon or urgent the case, knowing the great pain that the patient must endure,’ wrote Henry Hill Hickman, a Shropshire surgeon, who published his ideas on suspended animation in 1824.16 Suspended animation was thought to be a form of asphyxia, a shortage of oxygen. Although it was recognized as a state very close to death, since the late eighteenth century doctors had used resuscitation techniques to restore life in such circumstances. Prompted by a heartfelt desire to relieve both the anticipation and actual suffering of a severe operation, Hickman tested out his hypothesis that the ‘torpid state’ produced by inhaling carbon dioxide gas offered a useful interlude of insensibility. Puppies, rabbits, and mice were placed in the gas until respiration ceased; Hickman removed legs, ears, or tails, and dressed wounds; the animals gradually recovered consciousness. He took careful note of bleeding and the speed of healing but the most impressive fact was the apparent absence of suffering whilst he was using the knife. Hickman had no links to the medical bigwigs of the day but he did know Thomas Andrew Knight, Fellow of the Royal Society, who lived nearby in Downton Castle. Knight was renowned locally for his prize-winning Merino-Ryland crossbred sheep, and further afield for his expertise in plant and vegetable physiology. Hickman wrote to Knight describing his experiments and then printed a small pamphlet. We may expect this to have caused a stir. In fact Hickman’s proposals fell on stony ground. Hickman persisted. In 1828 he travelled to France and urged King Charles X to consider his work. It was discussed at the Académie Royale de Médicine, and Fanny Burney’s surgeon, Larrey, thought it of interest. But nothing came of it. Eventually Hickman returned to England and died in 1830, aged only 31. Not only did Hickman’s ideas challenge the essential purpose of pain, but suspending consciousness and respiration by inhaling a lethal gas seemed to skate too close to death.
Carbon dioxide had been identified in the 1750s through Joseph Black’s research into different kinds of air. Miners were familiar with the ‘bad’ air at the bottom of shafts and one of the best-known natural occurrences of carbon dioxide was on the outskirts of Naples, near Lake Agano, once the crater of a volcano. ‘On its bare and melancholy shores we found the celebrated Grotto del Cane,’ noted L. Simond, who visited the area in 1818.17 The Grotto received its name from the unfortunate dogs placed into the cave to demonstrate for visitors the effects of the gas. To those not au fait with new understandings of physiology it seemed as if magic. One visitor wrote that the dog
presently loses all motion, falls down as dead or in a swoon; the limbs convulsed and trembling, till at last no more signs of life appear than a very weak and almost insensible beating of the heart and arteries, which if the animal be left a little longer, quickly ceases too … But if it is taken out in time, and laid in the open air, it soon comes to life again.18
The Grotto was still listed in the 1893 edition of Baedeker’s Italian guidebook.
Carbon dioxide aroused geographical and scientific interest but for fun and frolics nitrous oxide’s alter ego—laughing gas—proved a better bet. The Adelphi Theatre in the Strand—’home of melodrama and screaming farce’, claimed one London directory—staged Monsieur Henry’s show in the 1820s. The playbill promised instruction through ‘novel and interesting experiments on gas’ and ‘peals of laughter’ provoked by the ‘wonderful effects’ of the gas.19 It was a curious mishmash of chemistry and farce. Christian Schoenbein, a German-Swiss chemist who later discovered gun-cotton and ozone, described how the curtain rose to reveal a semi-circle of large rubber bladders with glinting metal taps. M. Henry gave a short description of the gas and its properties: ‘in a way which would have done credit to a professor of chemistry’, noted Schoenbein. Then the fun began. The first volunteer was booed off the stage by the audience, as was the second. M. Henry asked for cooperation. The next volunteer sat in a chair and inhaled the gas. When the bladder was removed, he continued to sit holding his nose, causing roars of laughter; then he leapt and bounded around the stage. But the audience’s interest waned: ‘All nonsense and humbug!’, they began to cry. M. Henry asked the sceptic who began the revolt to come and try the gas. After emptying the largest bladder of gas he ‘beat around’ M. Henry ‘like a madman’ and assaulted him. Schoebein had tried laughing gas himself whilst staying with one of his friends who was an amateur chemist. After making large quantities of the gas, they invited friends to join them in the garden and inhale. One visitor, sceptical about the gas’s powers, breathed a lot: ‘he began to dance and devastate the adjoining flower-bed in his ecstasy,’ remembered Schoebein. It was, he thought, a strong contender to replace champagne at the end of dinner parties.20 Singing about laughing gas could be as entertaining as breathing it. Published around 1830, ‘Laughing Gas, a new comic song, sung with unbounded Applause’, by Mr W. Smith of the Royal Surrey Theatre, extolled the tribulations of ‘Poor Jeremy Jones’ who ‘swallowed a bladder of laughing gas’, in eleven verses. Nor were such pastimes unique to the British temperament.
Across the Atlantic, advertisements promised crowds more laughter than they had had in the previous six months if they visited the Grand Exhibition ‘of the effects produced by inhaling Nitrous Oxid, Exhilarating or Laughing Gas!’, demonstrated by Gardner Quincy Colton. No longer able to afford to continue at medical school, Colton lectured on popular scientific subjects. His shows attracted thousands of visitors and the one held on 10 December 1844 in Hartford proved particularly interesting. One of the young men who breathed the gas came strongly under its influence: running and jumping he bruised his legs so badly on a wooden bench they began to bleed. Observing these antics was Horace Wells, a local dentist. Wells asked Colton to help him try an experiment: Wells breathed nitrous oxide and had a tooth removed. Colton taught him how to make the gas and went on his way. Using a bladder and a wooden tube, Wells succeeded in giving nitrous oxide to a handful of patients during tooth extractions. He was convinced he had discovered a major technique and set up a demonstration on a man having a tooth extracted at Boston’s elite Massachusetts General Hospital. Disaster. In front of a large audience the man complained he felt pain: ‘the whole was denounced as an imposition and no-one was inclined to assist me in further experiments,’ said Wells. On reflection he realized that nerves had got the better of him; the gasbag had been removed too soon. Wells was given no second chance. The intense disappointment of failure ‘brought on an illness from which I did not recover for many months’, he later recalled.21 Wells is a tragic hero: he missed out on the discovery of nitrous oxide anaesthesia by a whisker. By the time he was credited for his work it was too late: he had committed suicide.
We may imagine that after Wells’s failure with nitrous oxide, ether anaesthesia was waiting in the wings. In fact there was no such view. Many surgeons believed pain relief was an unachievable quest: ‘a chimera that we can no longer pursue in our times’, asserted New York surgeon Valentine Mott.22 He, and many others, ignored the potential of mesmerism. An early form of hypnosis, mesmerism was introduced by Anton Mesmer in the 1790s. It was, he explained, ‘a fluid universally diffused … the medium of a mutual influence between the heavenly bodies’.23 Like laughing gas, mesmerism was popularized at fairs and exhibitions. It was also tried in surgery. The French surgeon Jules Cloquet successfully performed a mastectomy using ‘hypnotic analgesia’ in 1829. More successes followed, promoted in England in the 1830s by John Elliotson, Professor of Medicine at University College Hospital, and publicized in the Zoist. But mesmerism could not be explained by contemporary science: it was tainted by its mysterious history. Most doctors considered it a sham: ‘the girls who are magnetised deceive and cheat. They pretend to read with the back of their head, and prophecy all sorts of stuff,’ complained the President of the Royal College of Surgeons, Benjamin Brodie.24 A few doctors pursued mesmeric anaesthesia but not many managed to make it work. James Esdaile, a Scottish surgeon working in India, reported over a thousand successful operations carried out in the mid-1840s on patients rendered insensible to the pain through mesmerism: introducing mesmerism to the London hospitals was his vision. It remained unfulfilled.
Only twelve months after Wells failed to prove nitrous oxide’s anaesthetic powers at Massachusetts General Hospital, fellow dentist William Thomas Green Morton succeeded in establishing ether and began anaesthesia as we know it today. What made Morton succeed? Partly personality and partly chemistry accounted for his success. Morton was not alone in experimenting with ether. In the southern state of Georgia, a country doctor in a small agricultural community, Crawford Long, had operated under ether in the early 1840s. In Jefferson, as elsewhere, local youths entertained themselves with laughing gas. But Long could not manufacture it: he offered them ether instead. First synthesized in the sixteenth century by Valerius Cordus and sold by chemists as ‘sweet vitriol’, ether was used as a stimulant and anti-spasmodic; it could be inhaled or swallowed. Ether frolics became a local novelty. When James Venables, one of the young ether sniffers, needed a minor operation for the removal of a cyst but was terrified of pain, Long thought of using ether. ‘Breathe ether, then I’ll cut off the cyst,’ he advised Venables. Success. Venables only believed what had happened when Long showed him the cyst. Long continued the practice on one or two patients a year. But he never reported his results because he could not satisfy himself as to whether the anaesthetic effects had been produced by the ether, or the patient’s imagination. Nor was there much praise for Long’s innovation locally: most of the community were devout Christians who believed it was against God’s will to avoid physical pain. Ether breathing was as much a moral as physical risk.
Morton’s success was driven by business ambitions, rather than sympathy for patients. By the 1840s, dental technology was capable of producing good sets of artificial teeth that looked vastly superior to earlier designs. Yet a good fit relied on extracting all the decayed stumps and roots of original teeth from the jaw, and often patients could not bear the pain.
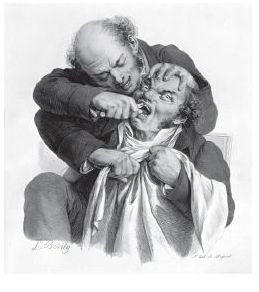
Figure 1 Many patients, partcularly females could not endure the pain of tooth extractions. Coloured litho c.1826.
Some patients tried to fortify themselves by having a glass or two of wine; some ran away in the middle of the extractions. It was this untapped market that stimulated Morton’s researches: the surefire way to boost dental profits was to solve the problem of pain. He quizzed his landlord and fellow dentist, Charles T. Jackson, on the characteristics of ether: Jackson used ether as ‘toothache drops’. Morton borrowed Jackson’s chemistry textbooks to bone up on ether: ‘there was nothing new or particularly dangerous in the inhaling of ether,’ he reassured himself.25 After establishing that sulphuric ether was the most effective form of the chemical, Morton tried it on animals, then he inhaled ether from a handkerchief and lost consciousness. On coming round, ‘I felt a numbness in my limbs, with a sensation like nightmare. Gradually, I regained power over my limbs, and full consciousness … I had been insensible between seven and eight minutes,’ he said.26 On 30 September 1846 fortune struck. A young man, Eben Frost, called on Morton in the evening in great pain, desperate to have a tooth extracted. ‘Could it be done using mesmerism to avoid pain?’, he asked Morton. ‘I have something better,’ promised Morton. From all accounts it was a success: Frost declared himself ‘perfectly well and enraptured with the novelty and successful result of the experiment’.27 Morton was spurred on: he persuaded Chief Surgeon John Collins Warren at Massachusetts General Hospital to let him demonstrate the remarkable powers of his discovery; he also visited Commissioner of Patents R. H. Eddy, keen to secure his legal rights.
On the morning of Friday 16 October Morton arrived at Massachusetts General Hospital, accompanied by Eben Frost, living proof of the discovery. They arrived late: Morton had been delayed by the last-minute adjustments to his apparatus. But whereas the drama of the situation had terrified Wells, Morton’s showmanship won through. Edward Abbott, 20 years old, was sitting in a chair, waiting to have a tumour on the left side of jaw removed. Morton took him by the hand, told him that the new preparation would ease some, if not all of the pain, pointed out Eben Frost and asked, ‘Are you afraid?’ ‘No,’ replied Abbott, ‘I feel confident that you will do precisely as you tell me.’ Once Abbott became insensible, Morton signalled to Warren to begin the operation. Warren, greatly surprised that Abbott did not start or cry during the incision, removed the tumour. During the last part Abbott moved his limbs and cried out a little, Warren was dubious about the success until he quizzed Abbott on his experience. Abbott was adamant that he had not felt pain: the incision, he said, was like a ‘blunt instrument passed roughly across his neck’.
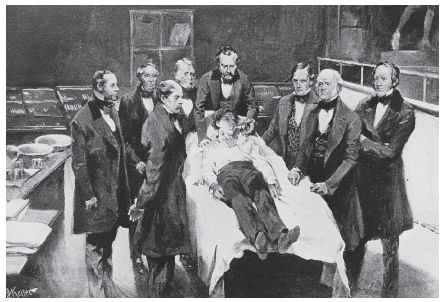
Figure 2 William Morton’s demonstration of ether at Massachusetts General Hospital on 16 October 1846, painted fifty years or so after the event. The artist depicts Abbott lying down rather than sitting in a chair.
The following day a further successful operation was performed without the patient suffering pain. To be sure, luck was on Morton’s side. Ether produced anaesthetic effects more reliably than nitrous oxide—had Wells chosen ether things may have been different—and there was no suggestion that any of Morton’s patients suffered breathing difficulties during inhalations. Warren and the other surgeons endorsed Morton’s discovery, and the Boston community began to buzz with excitement. But very soon clouds appeared in the sky.
When Jackson learnt of Morton’s plan to patent ether he convinced Eddy he should also share in any financial return from ether as it was he who gave Morton the idea. A compromise was reached and Jackson and Morton submitted a patent application to the US Patent Office on 27 October 1846. Then war broke out. Boston dentists published a manifesto protesting against Morton’s actions; hospital surgeons stopped using the preparation, partly because Morton would not reveal its identity, and partly because of the patent protections. Morton backtracked. He gave surgeons at the hospital an inhaler and agreed to reveal the identity of his preparation, providing they kept it secret: it was given the name ‘Letheon’. On 7 November 1846 surgeons began using ether again and a couple of days later at the Boston Society of Medical Improvement, Henry J. Bigelow, a surgeon at the hospital, gave a paper on the new phenomenon. It was controversial, he said, for Morton to be patenting ‘an agent capable of mitigating human suffering’ and tried to explain the reasons. Its use should be restricted in case of hazards, and dentists were accustomed to working with secret processes. There was no doubt, he concluded, that the new preparation ‘promised to be one of the most important discoveries of the age’.28 Morton’s attempt to patent his discovery and reap financial profit was not unusual within dentistry. Dental practitioners regularly sought to patent new mechanical inventions and Morton had a history of shady business ventures. Suffering pain during operations had been a tribulation of humankind for centuries: Morton could have visualized himself as the world’s benefactor but probably even he did not envisage the way in which anaesthesia would be taken up. His vision was of the material return from his discovery.
On 12 November 1846 Jackson and Morton were issued with the Letter Patent No. 4848 but this compounded rather than resolved the difficulties. Wells, encouraged by friends, attempted to set the record straight and in a letter to the editor of the Hartford Courant wrote:
If Drs Jackson and Morton claim something else, I reply that it is the same in principle, if not in name, and they can not use anything which will produce more satisfactory results, and I made these results known to both these individuals, more than a year since. After making the above statement of facts, I leave it for the public to decide to whom belongs the honor of discovery.29
Jackson sent an account of ether to the Académie des Sciences in Paris, claiming ownership of the discovery. The wrangle over priority of discovery lasted many years. Neither Morton, Jackson, or Wells ever received any kind of financial benefit for their part in the discovery of anaesthesia. Wells committed suicide in 1848; Morton died in 1868, still waging war with Jackson over their part in the discovery of anaesthesia.
But in December 1846 this was all to come. Boston surgeons were gaining confidence in ether but its future remained precarious. Many practical and intellectual controversies would have to be resolved before anaesthesia became routine in surgery. First, ether had to woo Europe.