2
Gestalt: Rash/inflammatory
- Epidermal changes
- Parakeratosis, 99
- Spongiosis, 102
- Papulosquamous (psoriasiform), 106
- Interface (vacuolar), 112
- Interface (lichenoid), 117
- Inflammation: Specific patterns and cell type
- Epidermal eosinophils, 123
- Perivascular, 127
- Band-like dermal/papillary dermal infiltrate, 131
- Diffuse/nodular, 137
- Subcutaneous, 144
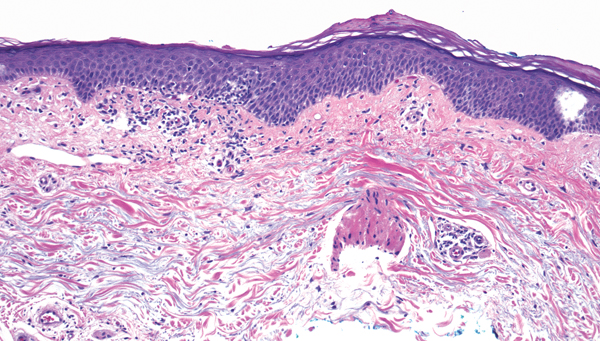
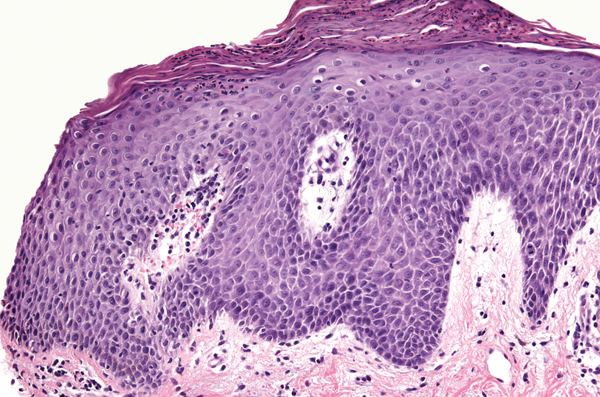
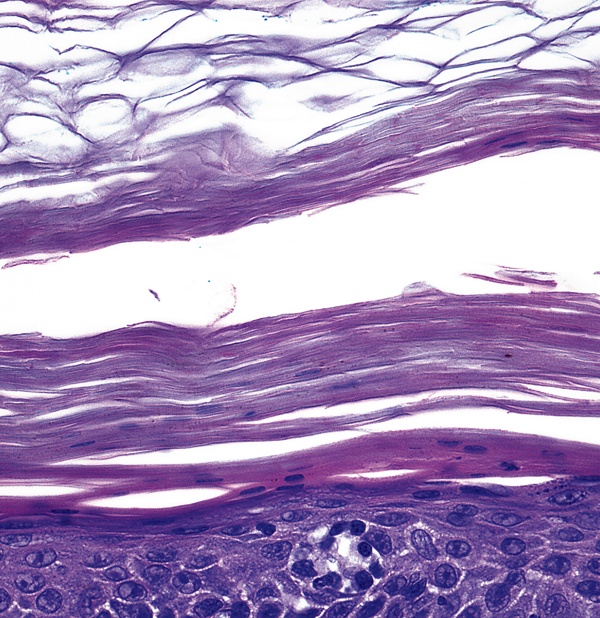
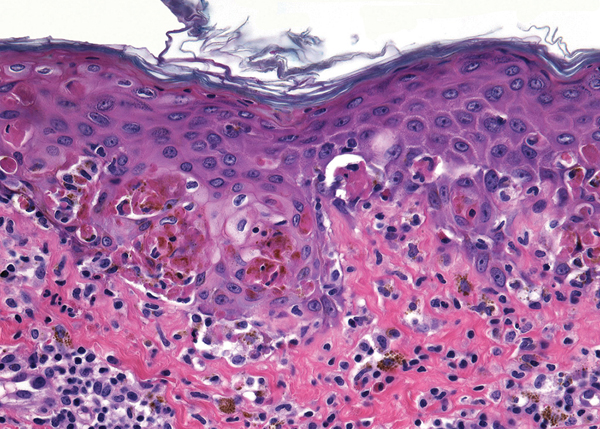
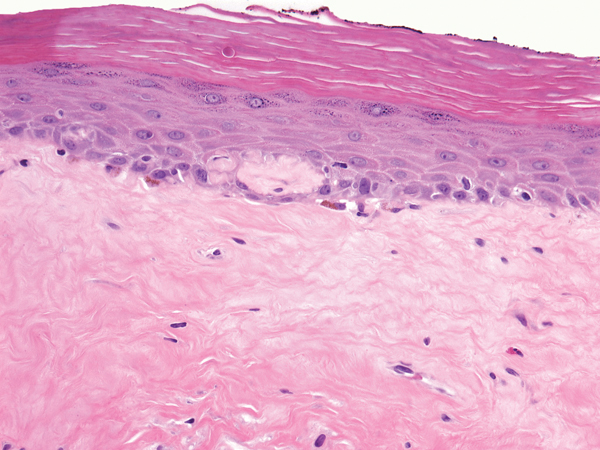
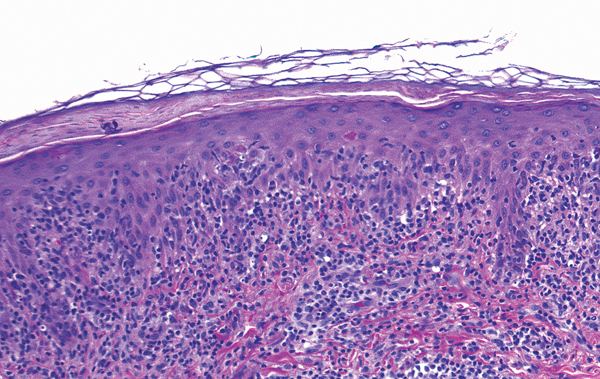
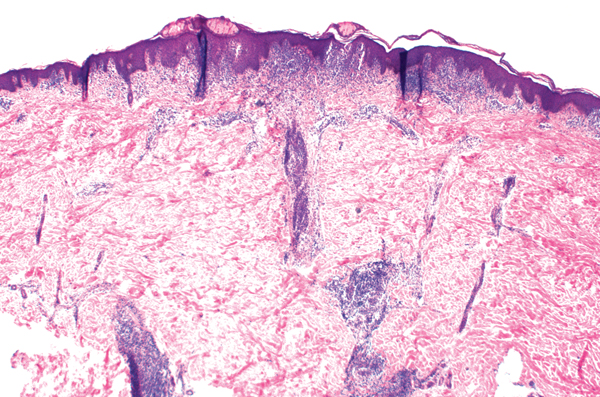
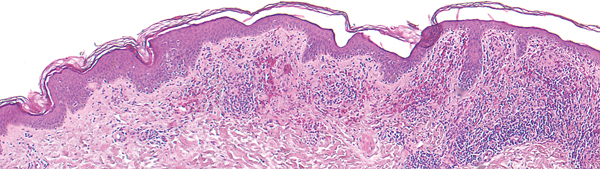
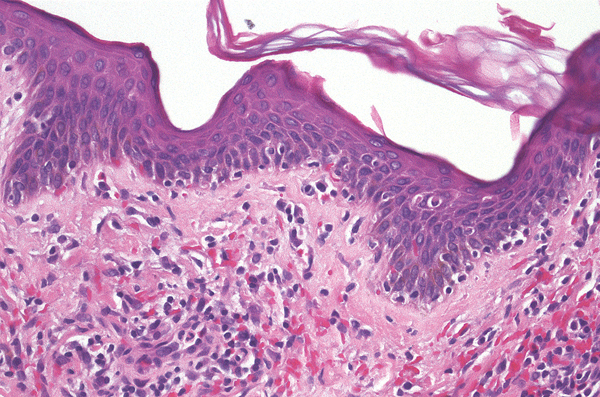
Spongiotic dermatitis
- “Wet” parakeratosis (parakeratosis with serum)
- Increased space between keratinocytes
- Vesicles may be present
- Exocytosis of lymphocytes
Perivascular inflammation
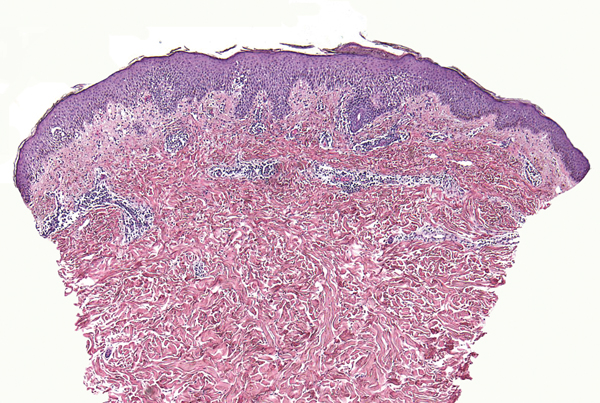
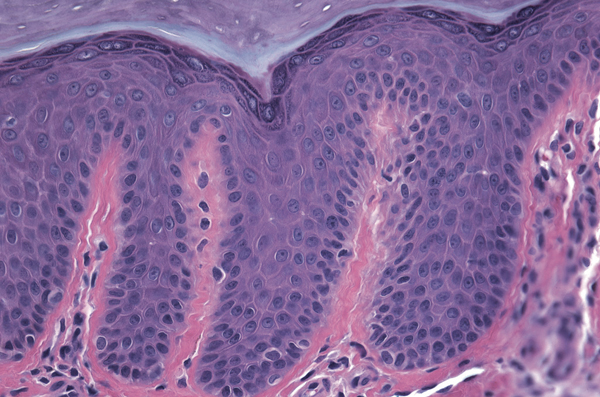
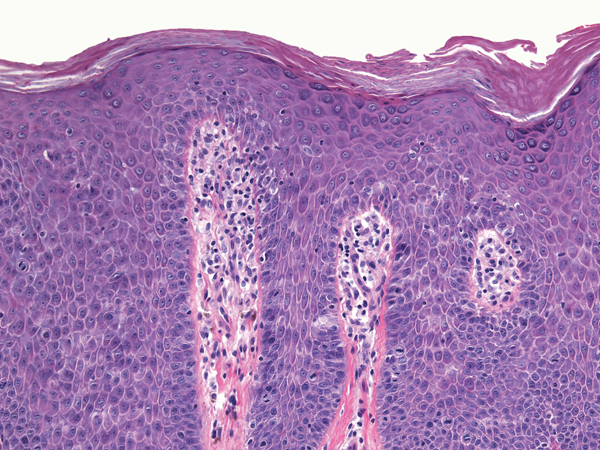
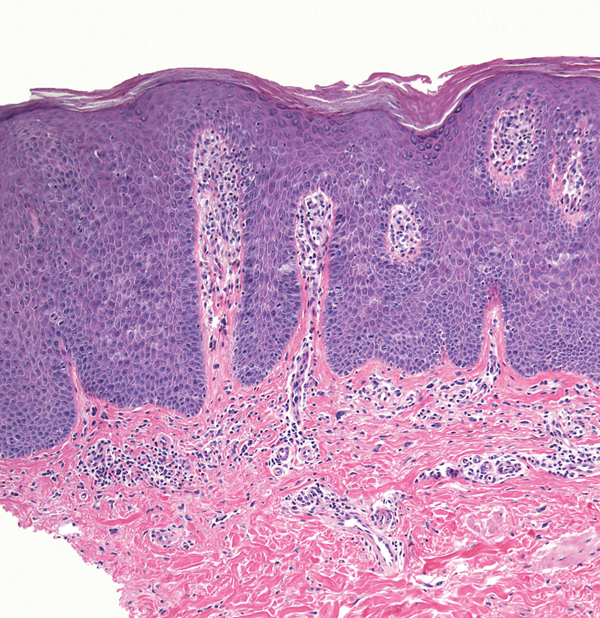
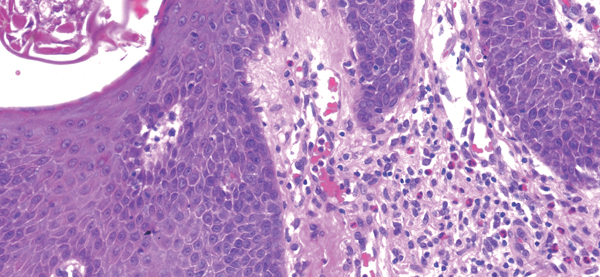
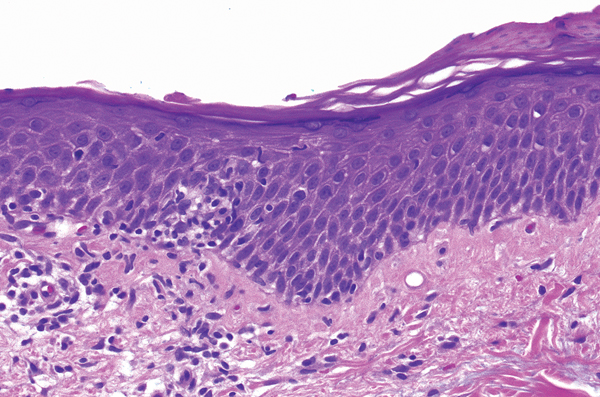
Psoriasis
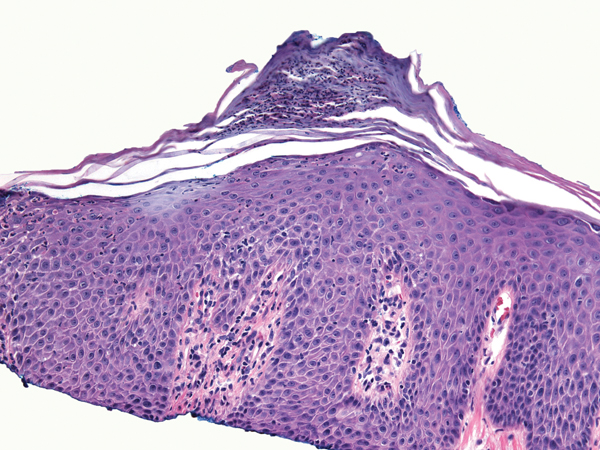
- Dry parakeratosis with neutrophils
- Regular acanthosis
- Hypogranulosis
- Neutrophils may be present in the stratum spinosum
- Prominent vessels in papillary dermis
- Perivascular inflammation
Key differences
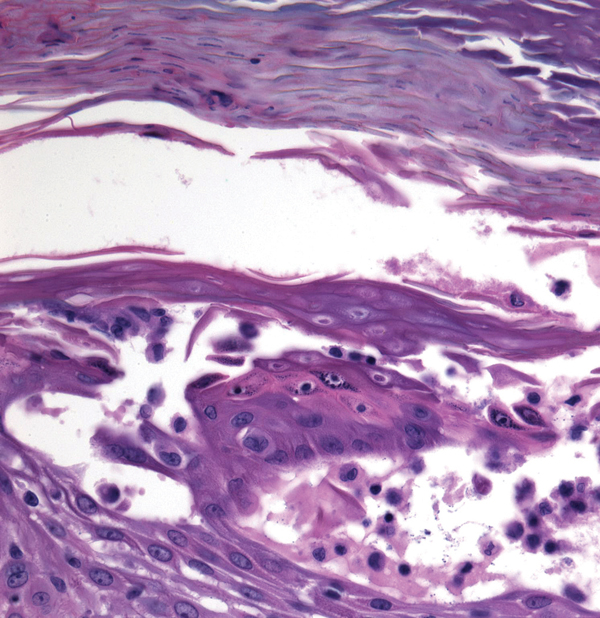
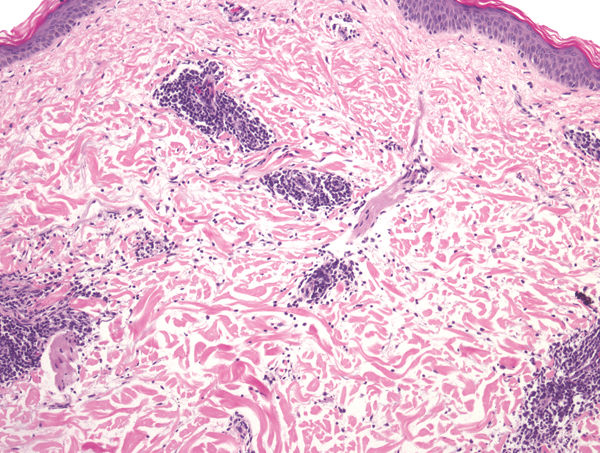
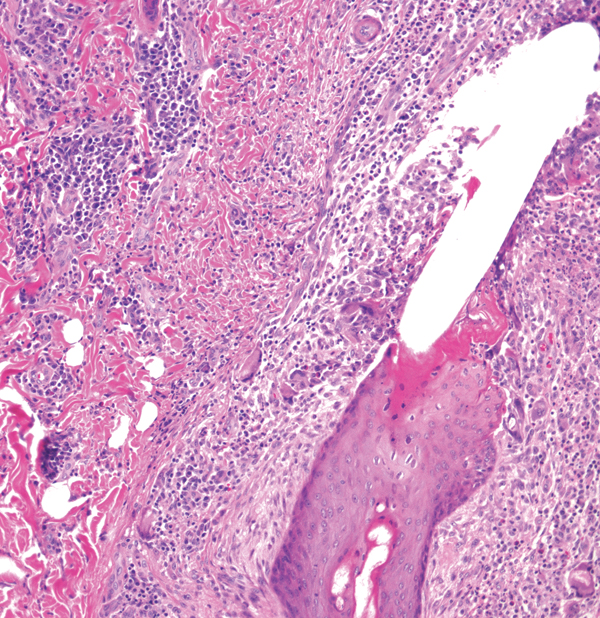
(a)
(b)
- Spongiotic dermatitis: wet parakeratosis, increased space between keratinocytes, preserved granular layer
- Psoriasis: dry parakeratosis with neutrophils, regular acanthosis, hypogranulosis, prominent papillary dermal blood vessels
Allergic contact dermatitis

- Spongiosis
- Vesicles within epidermis may be prominent
Arthropod assault
- Eosinophilic spongiosis
- Wedge-shaped pattern of inflammation on low power view
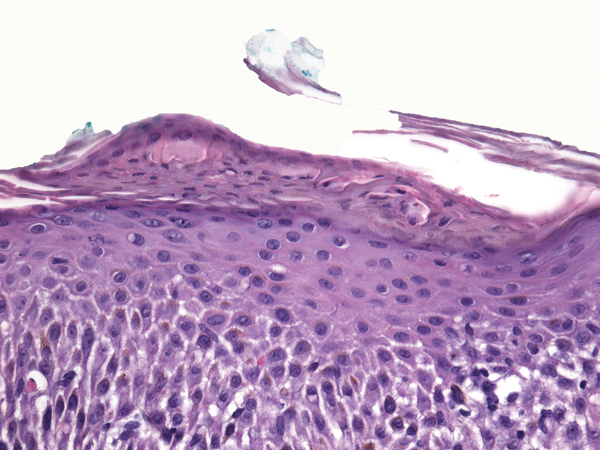
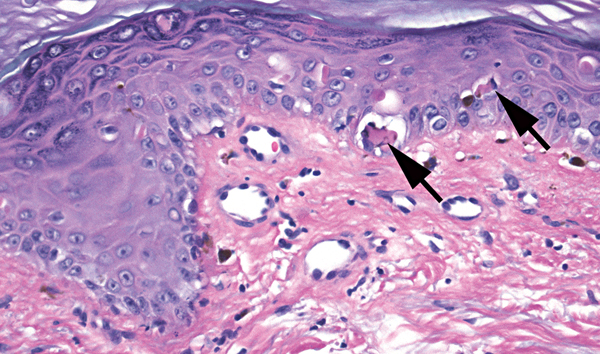
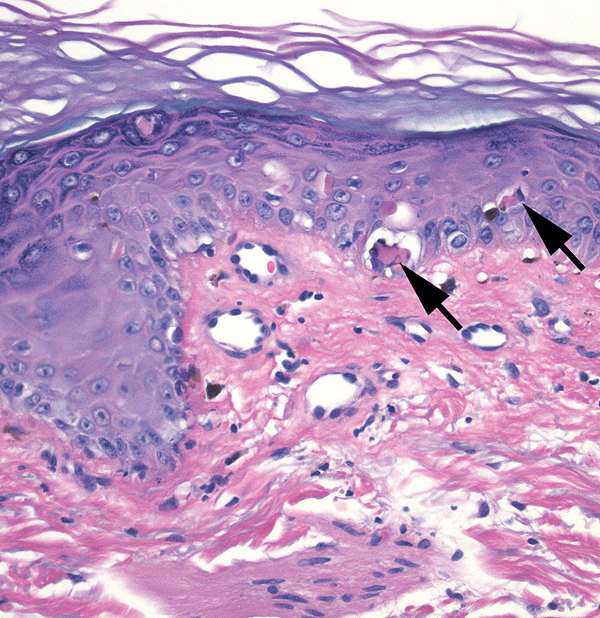
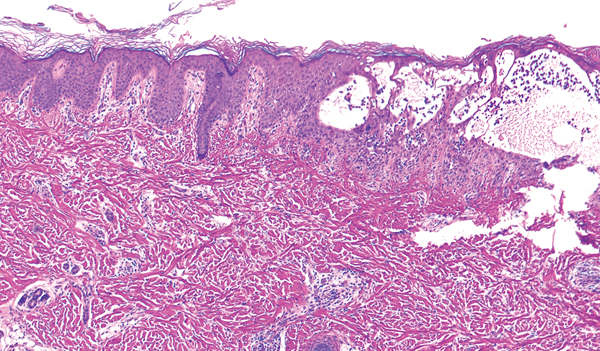
Pityriasis rosea
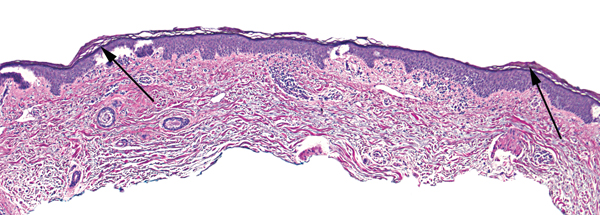

- Vesicles within epidermis may be prominent
- Mild epidermal spongiosis (short arrow)
- Mounds of parakeratosis (long arrows)
- Superficial perivascular infiltrate of lymphocytes
Extravasated erythrocytes
Note Guttate psoriasis is in the differential; guttate psoriasis is favored if there are neutrophils in the mounds of parakeratosis.
Key differences
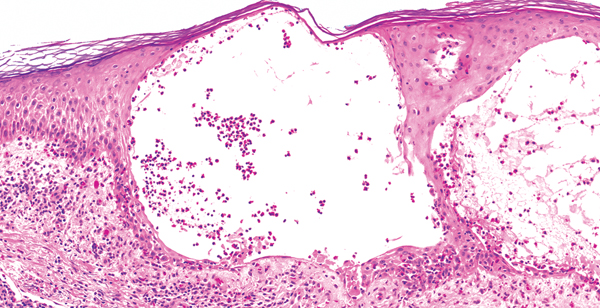
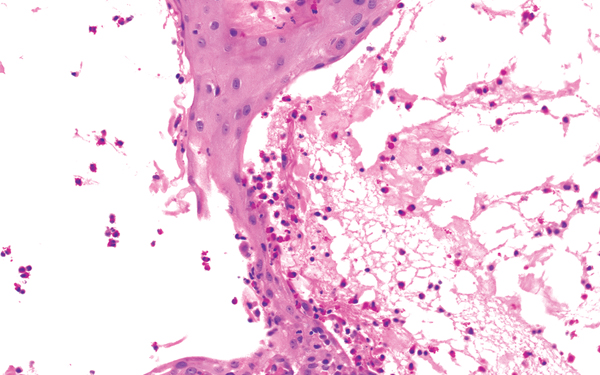
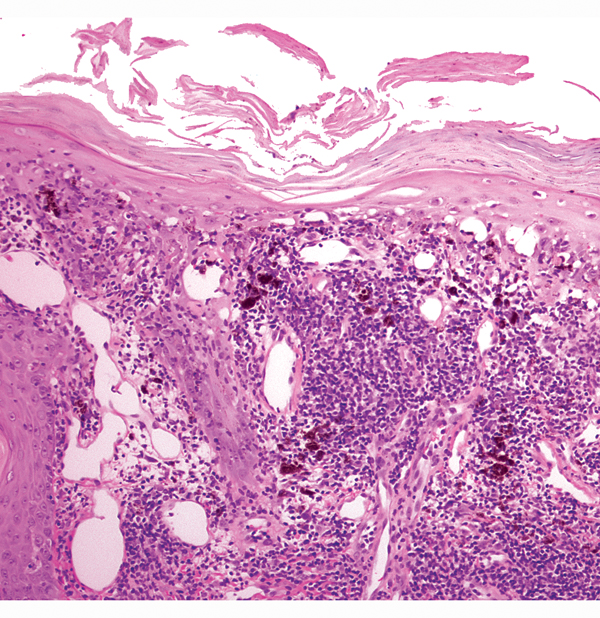
(a)
(b)
(c)
(d)
(e)
(f)
- Acute spongiosis with vesicles (allergic contact dermatitis): parakeratosis, intraepidermal vesicles, intercellular edema
- Acute to subacute spongiosis: parakeratosis with serum (“wet” parakeratosis), intercellular edema
- Chronic spongiosis: parakeratosis, granular layer preserved, acanthosis, subtle intercellular edema (see page 106)
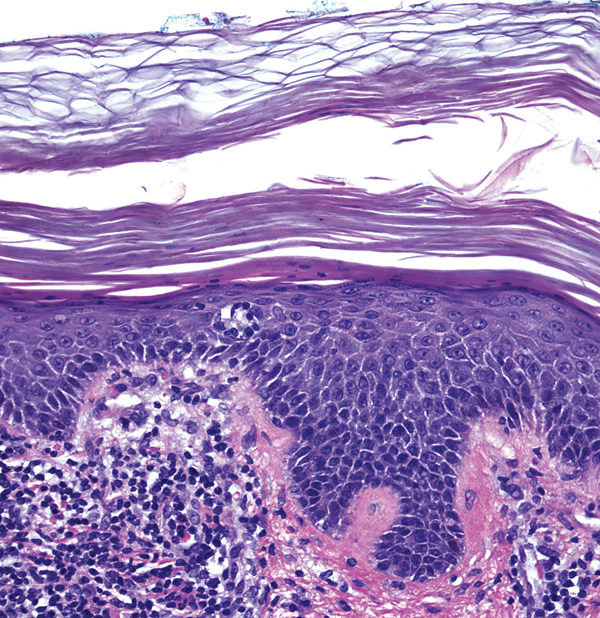
- Lichen simplex chronicus: often a stratum lucidum, minimal intercellular edema, vertical streaking of collagen in papillary dermis (see page 107)
- Psoriasis: dry parakeratosis (parakeratosis generally lacking serum) often with neutrophils, hypogranulosis, neutrophils in stratum spinosum, regular acanthosis, prominent vessels in papillary dermis (see page 100, 109)
- Pityriasis rosea: interrupted foci of parakeratosis, collections of erythrocytes/lymphocytes in the epidermis and papillary dermis
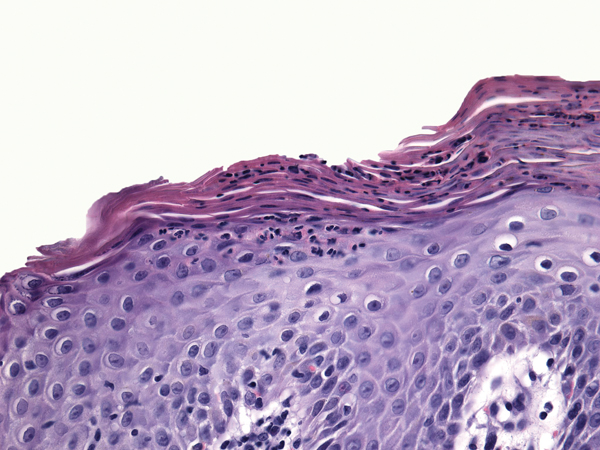
Chronic spongiotic dermatitis
- Papulosquamous (psoriasiform)
- Foci of parakeratosis
- Subtle foci of interkeratinocytic edema
- Irregular acanthosis with preserved granular layer
Perivascular inflammation
Note There is some overlap of chronic spongiotic dermatitis with lichen simplex chronicus, with the latter classically lacking parakeratosis and spongiosis and having dermal fibrosis.
Lichen simplex chronicus
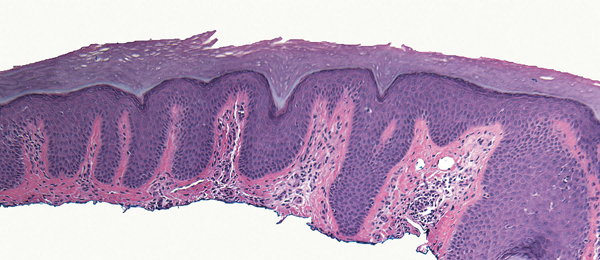
- Papulosquamous (psoriasiform)
- Hyperkeratosis with a stratum lucidum
- Irregular acanthosis with hypergranulosis
- Vertical streaking of collagen into the papillary dermis
Pityriasis rubra pilaris

- Papulosquamous (psoriasiform)
- Hyperkeratosis alternates with dry parakeratosis in a checkerboard pattern
- Follicular plugging
- Irregular acanthosis of epidermis
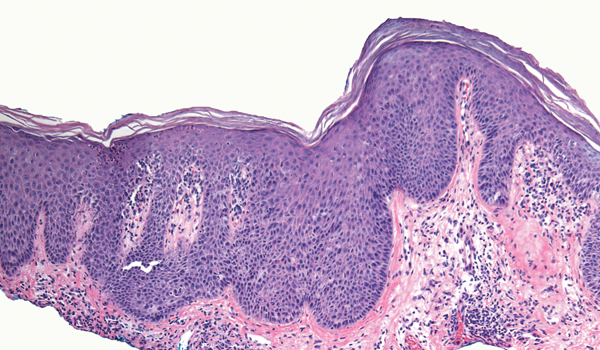
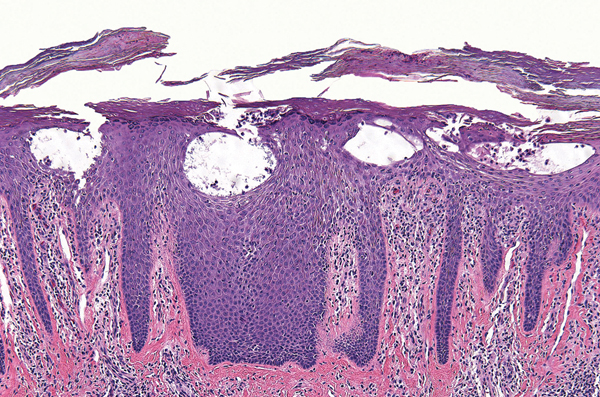
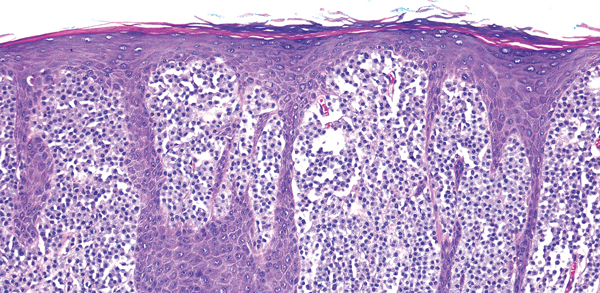
Psoriasis


- Papulosquamous
- Dry parakeratosis with neutrophils
- Regular acanthosis with hypogranulosis
- Prominent papillary dermal blood vessels
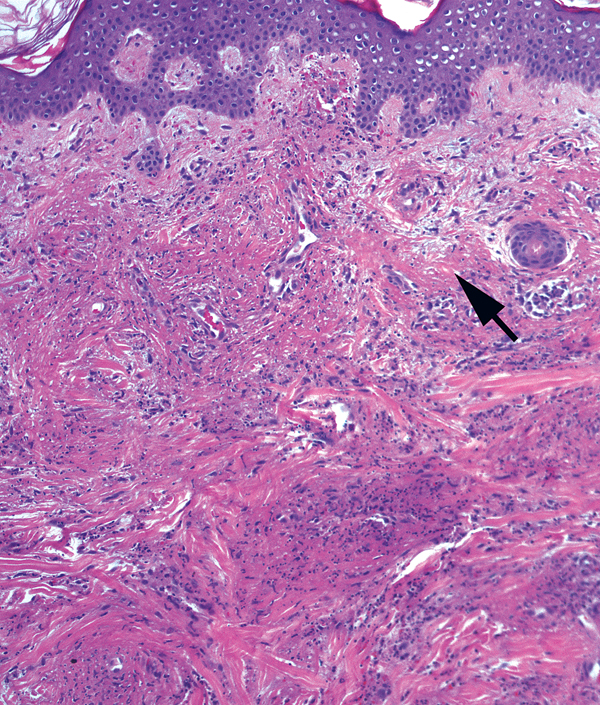
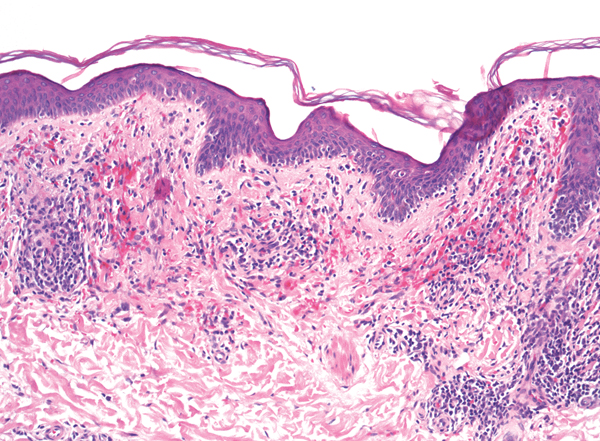
Secondary syphilis
- Papulosquamous (psoriasiform)
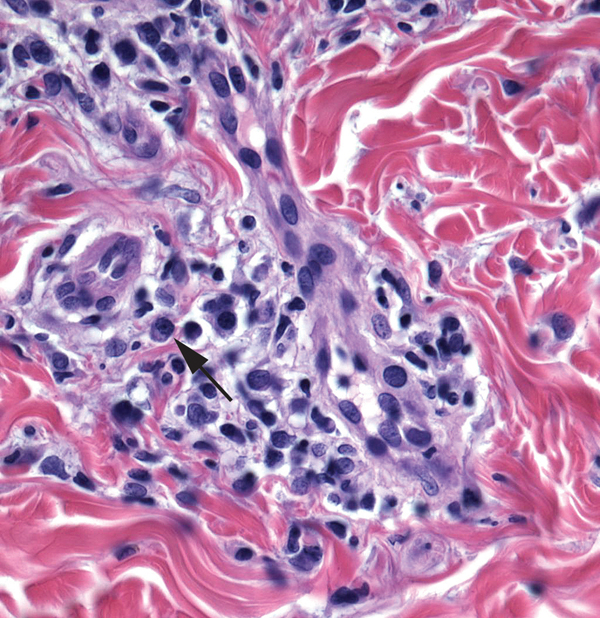
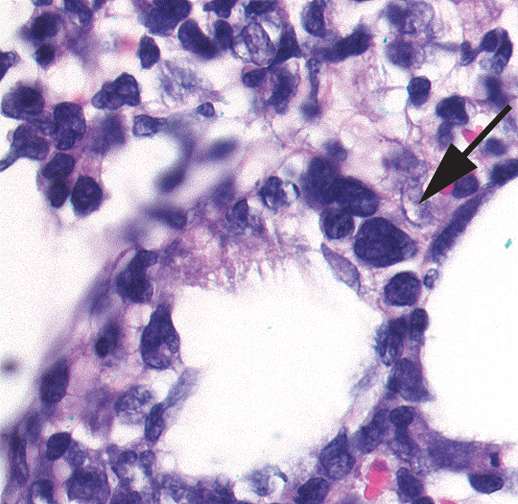
- Looks like pityriasis lichenoides et varioliformis acuta with plasma cells (arrow)
- Parakeratosis, sometimes with neutrophils
- Acanthosis with slender rete
- Lichenoid and deep perivascular lymphoplasmacytic inflammation
- Swollen endothelial cells
Key differences
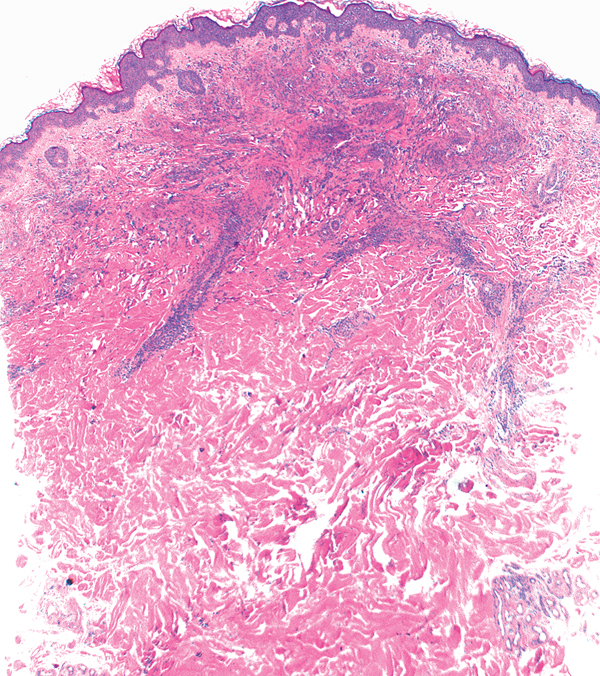
(a)
(b)
(c)
(d)
- Psoriasis: neutrophils in the epidermis, regular acanthosis, prominent papillary dermal blood vessels
- Pityriasis rubra pilaris: checkerboard pattern of hyperkeratosis and parakeratosis, follicular plugging
- Secondary syphilis: acanthosis with slender rete, lichenoid inflammation, swollen endothelial cells, plasma cells may be evident
Chronic spongiotic dermatitis: parakeratosis and foci of spongiosis, irregular acanthosis
Note Some experts reserve the term “psoriasiform” for processes that are difficult/impossible to distinguish from psoriasis.
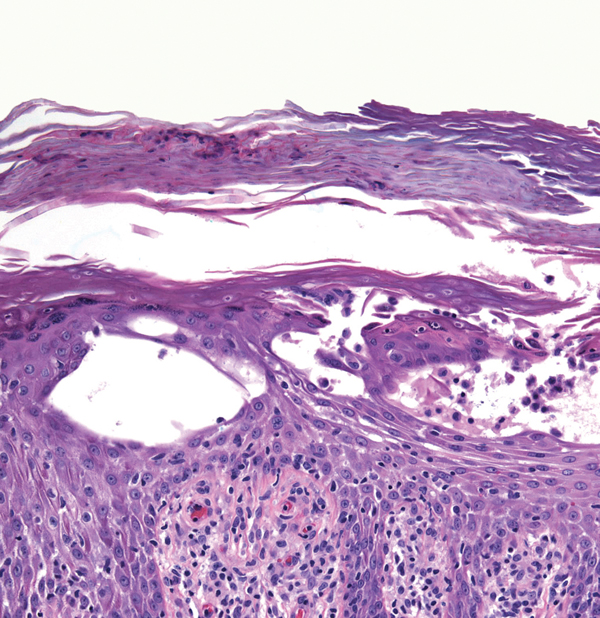
Erythema multiforme

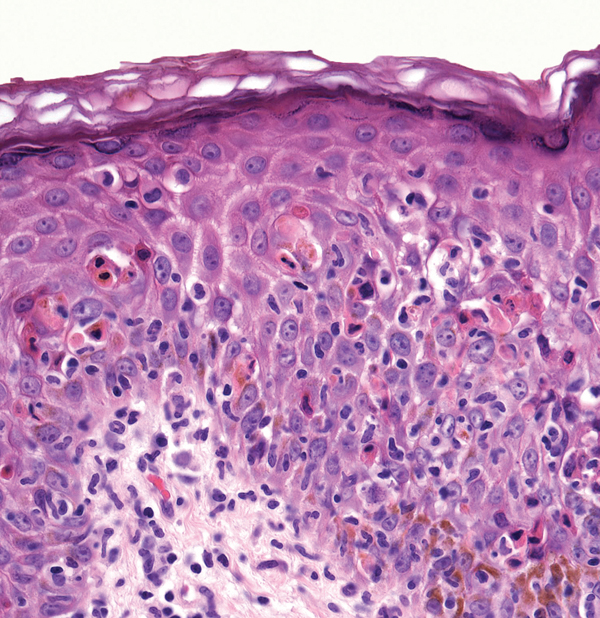
- Interface (vacuolar) change with necrotic keratinocytes in the lower epidermis
- Basket-woven stratum corneum
- Relatively sparse lymphocytic inflammation
Fixed drug reaction
- Interface vacuolar change
- Basket-woven stratum corneum and dermal incontinence of pigment
- Numerous necrotic epidermal cells may be present, mimicking erythema multiforme
- Superficial and deep perivascular infiltrate
- Infiltrate is mixed with eosinophils and neutrophils
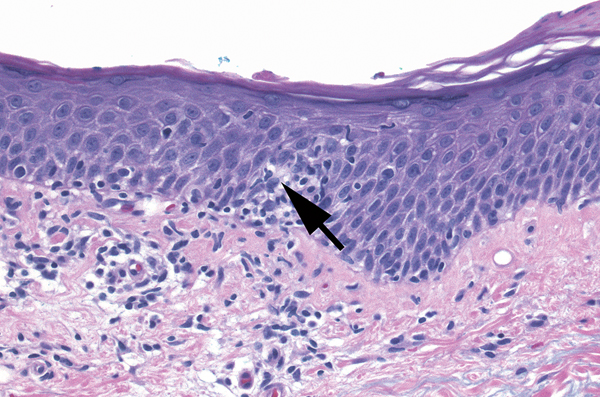
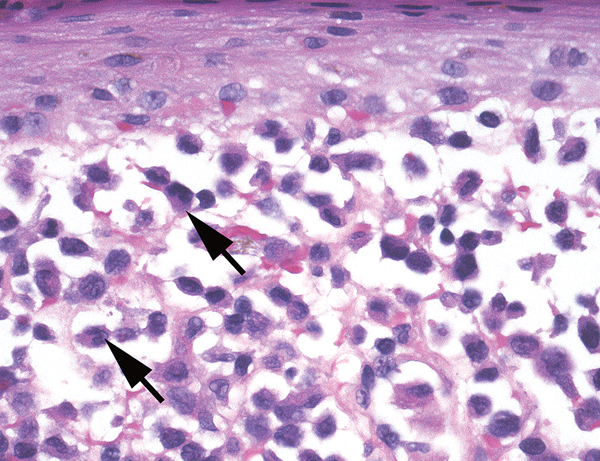
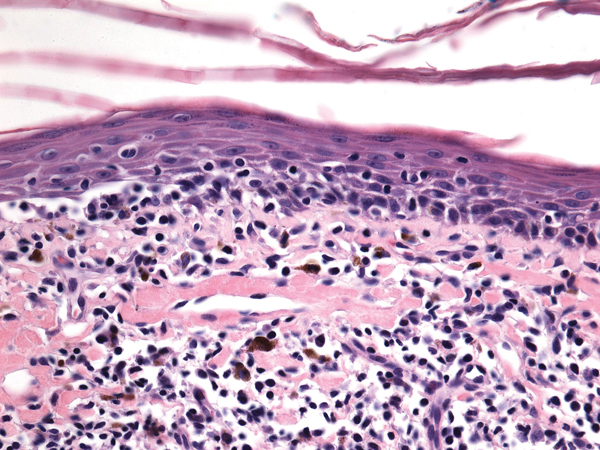
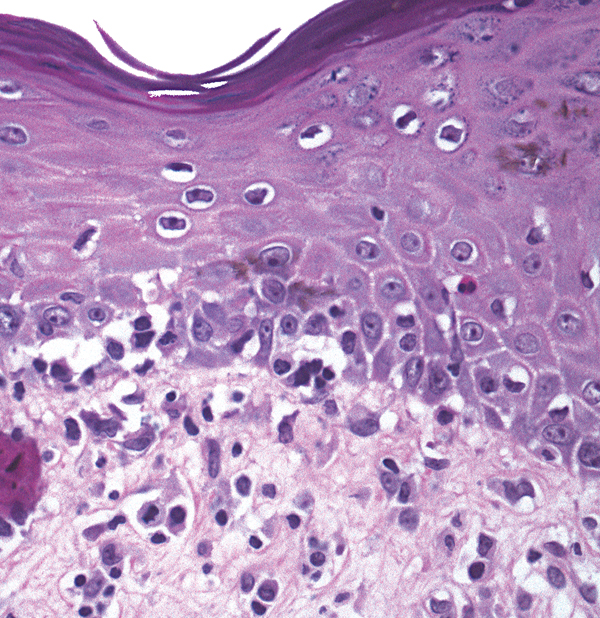
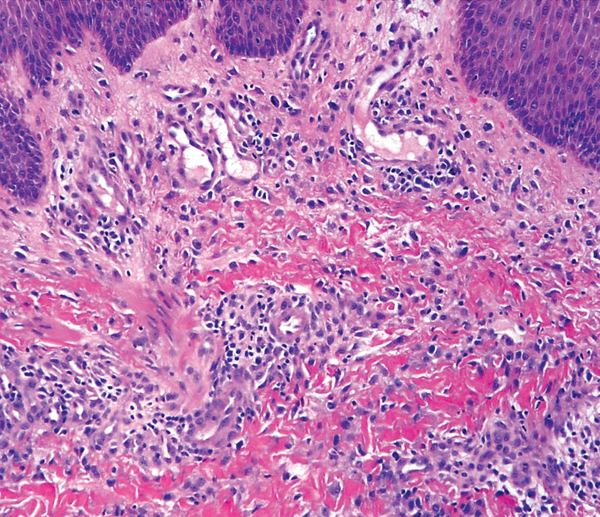
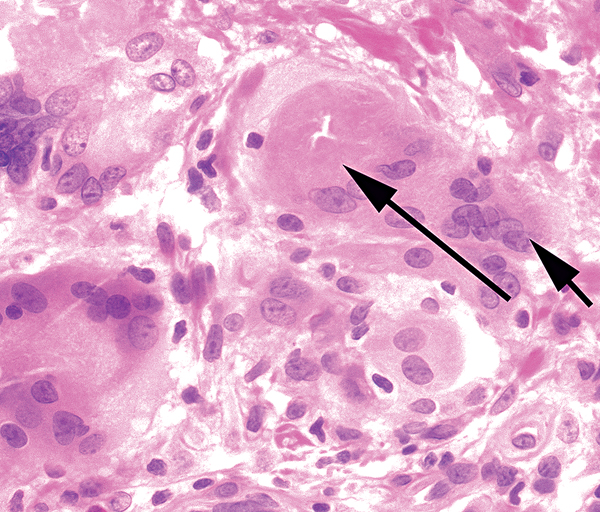
Graft-versus-host disease

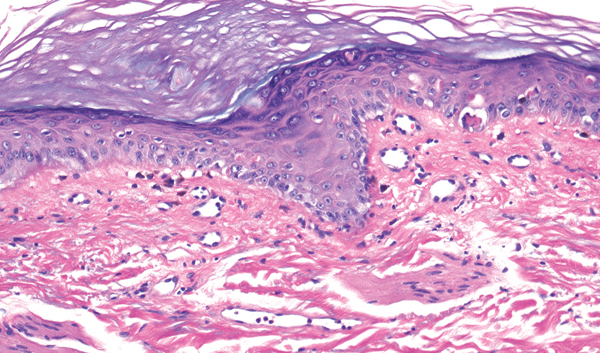

- Vacuolar change at dermoepidermal junction
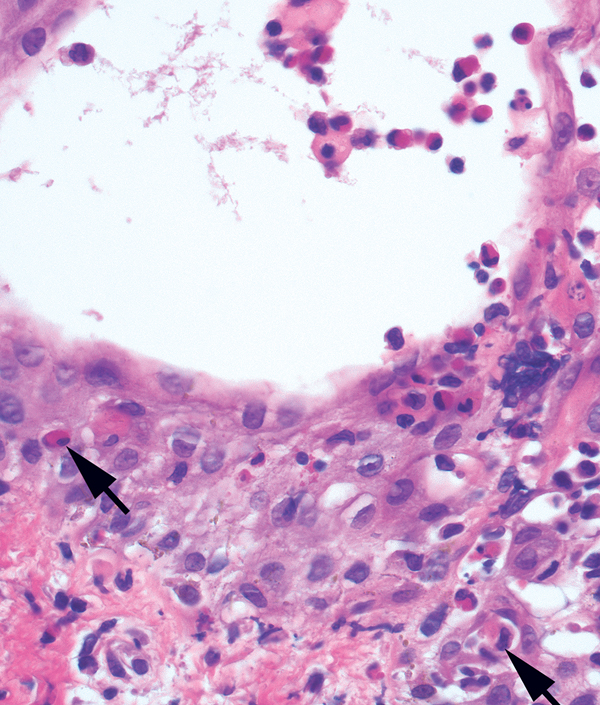
- Necrotic keratinocytes (arrows) in epidermis and follicles with adjacent lymphocytes (satellite cell necrosis)
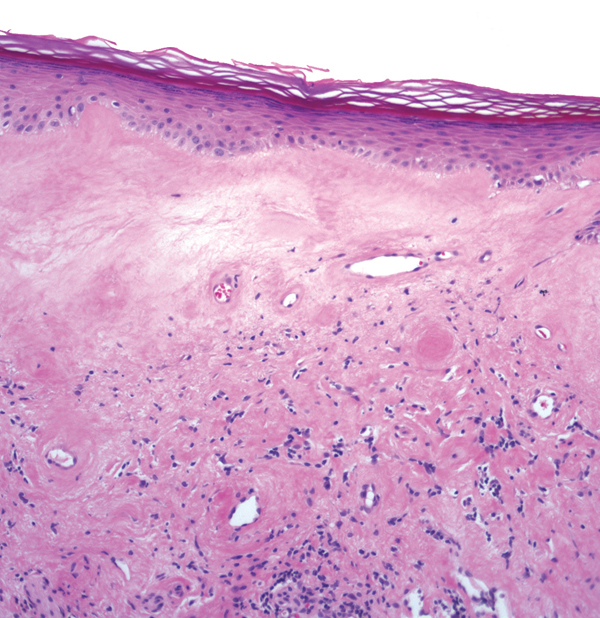
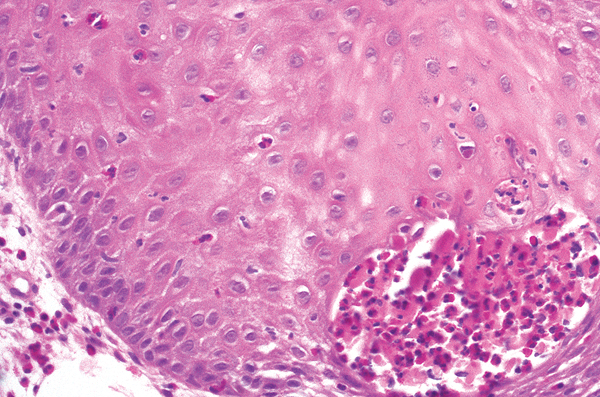
Lichen sclerosus
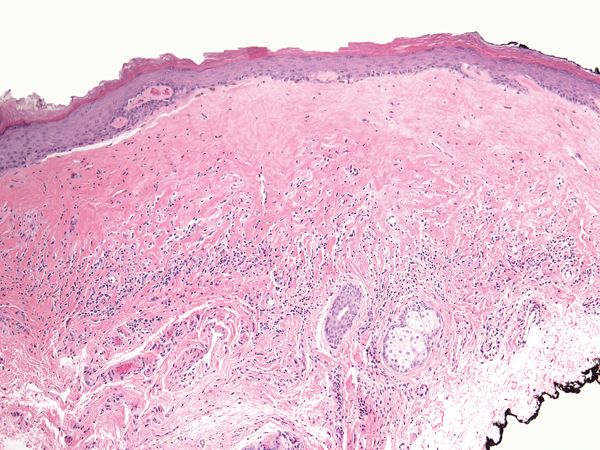
- Hyperkeratosis and lymphocytic infiltrate
- Vacuolar change at dermoepidermal junction
- Pink homogenization of papillary dermis
- Underlying band-like inflammatory infiltrate
Key differences
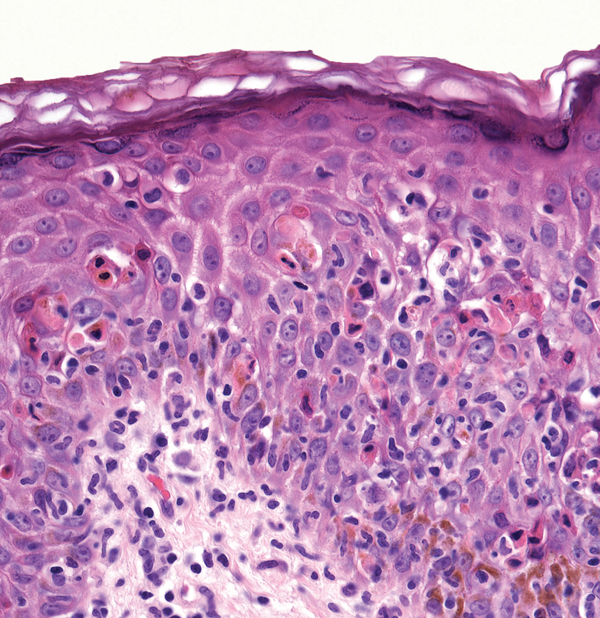
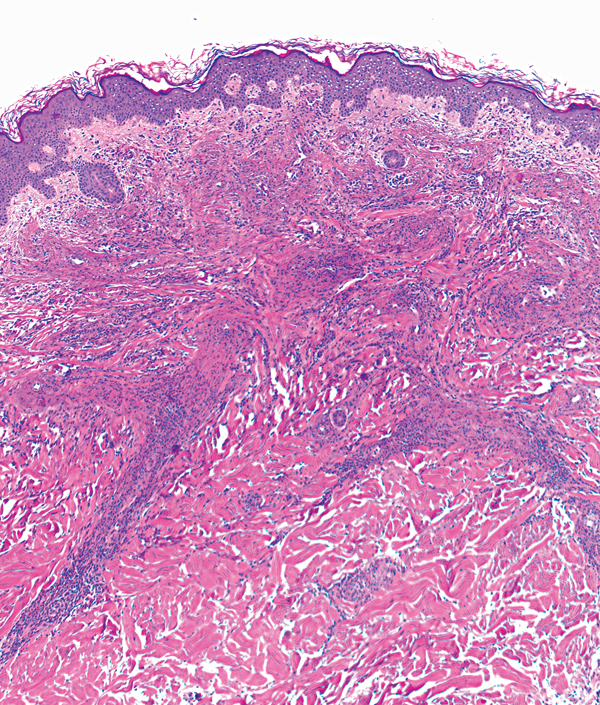
(a)
(b)
(c)
(d)
- Erythema multiforme: basket-woven stratum corneum, many necrotic keratinocytes in lower epidermis, superficial perivascular lymphocytes
- Fixed drug eruption: basket-woven stratum corneum, superficial and deep mixed inflammatory infiltrate, pigment incontinence
- Graft-versus-host disease: necrotic keratinocytes involving hair follicles, relatively sparse inflammation
- Lichen sclerosus: hyperkeratosis, hyalinization of superficial dermis, band of lymphocytes below hyalinized dermis
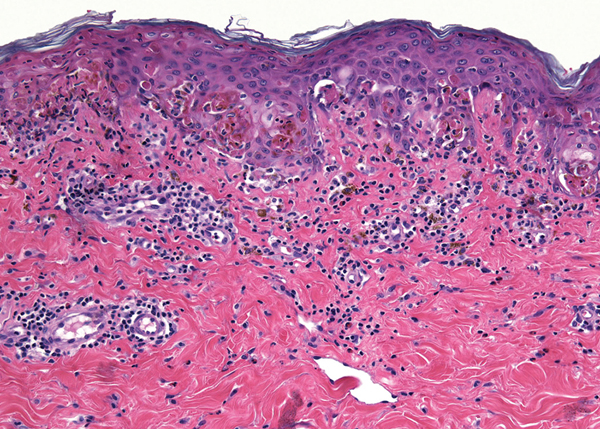
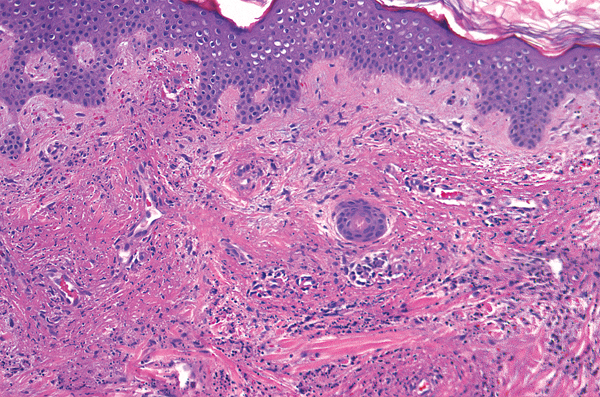
Discoid lupus erythematosus


- Lichenoid infiltrate (note: sometimes discoid lupus shows interface vacuolar change)
- Follicular plugging
- Atrophic epidermis
- Thickened basement membrane
- Pigment incontinence
- Periadnexal and perivascular lymphocytic infiltrate
Halo nevus
- Lichenoid infiltrate
- Nests of melanocytes at junction and/or in dermis (obscured by lymphocytes)
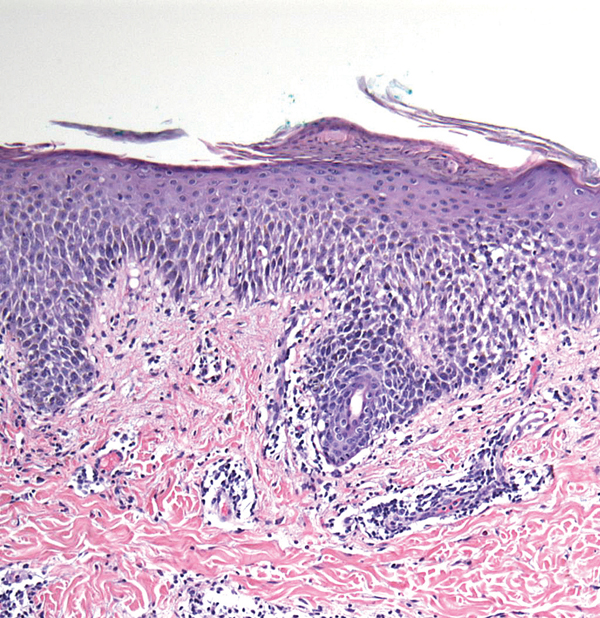
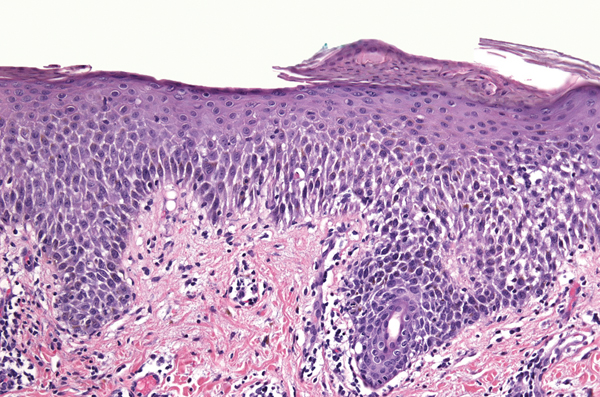
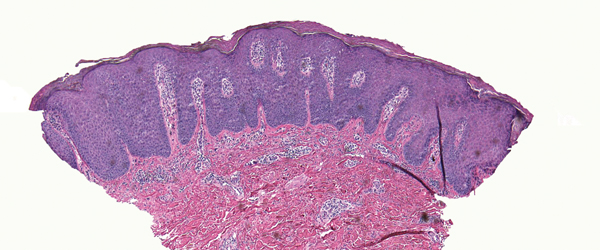
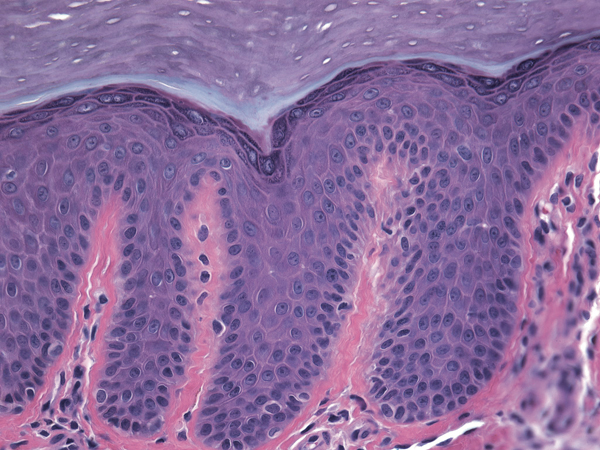
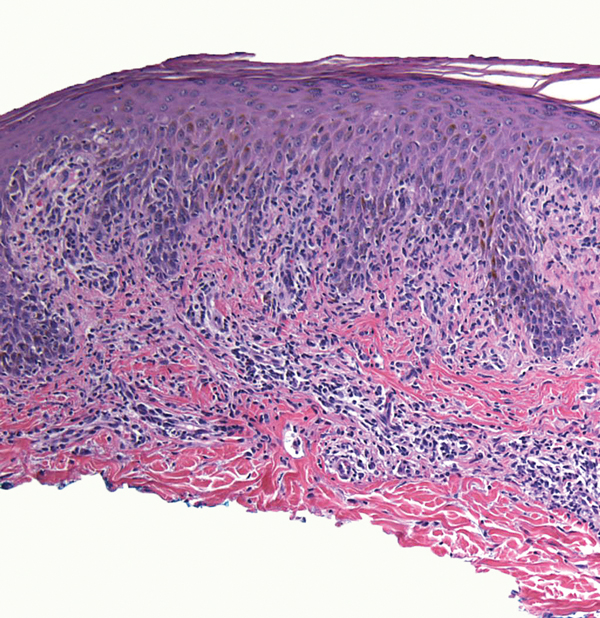
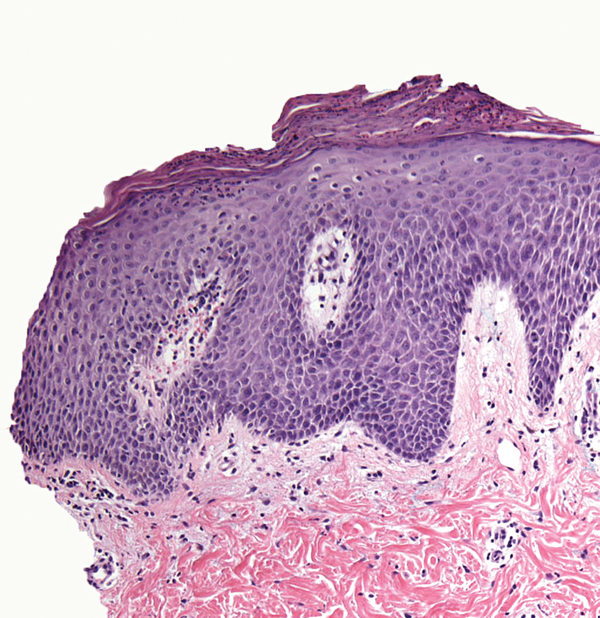
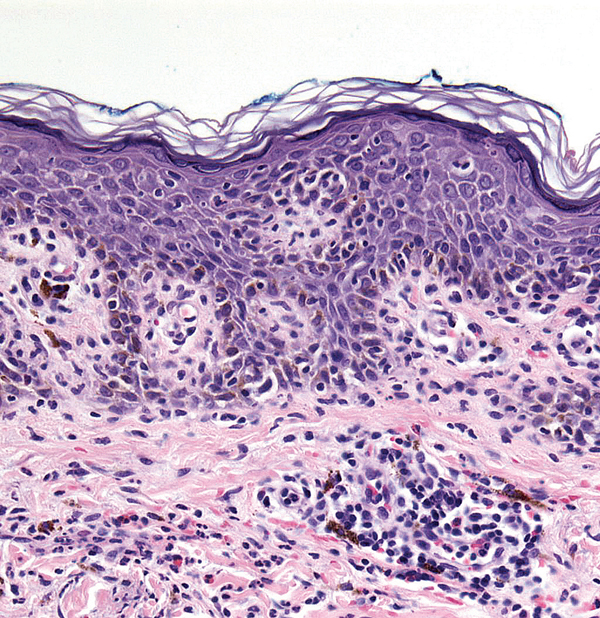
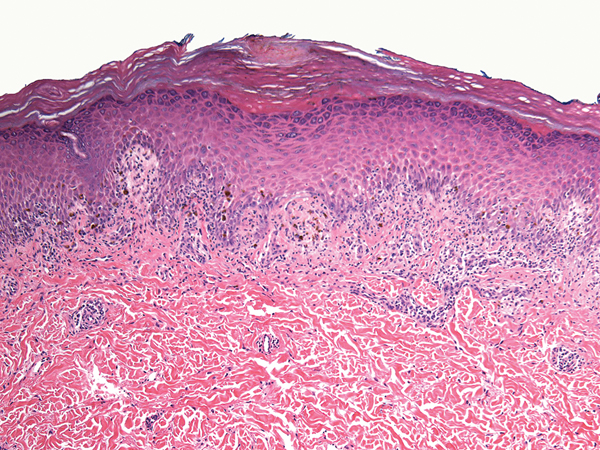
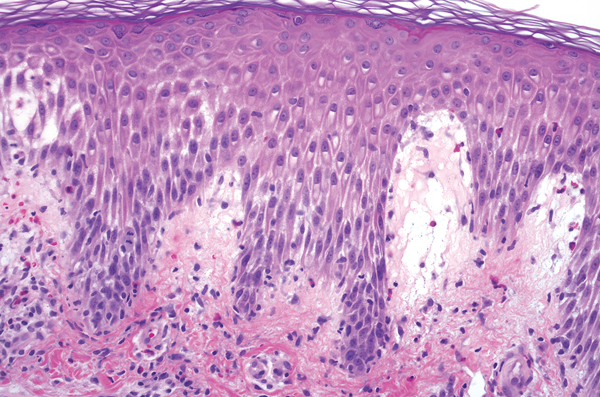
Lichen planus

- Lichenoid infiltrate
- Hyperkeratosis, irregular acanthosis, hypergranulosis
- Saw-toothing of basal layer
- Colloid bodies, civatte bodies
- Pigment incontinence
- Usually no eosinophils
If a mucosal surface, plasma cells may be present
Note Lichenoid drug reactions can look the same but usually show parakeratosis and eosinophils.
Note Benign lichenoid keratosis can look the same (need clinical history).
Lichen striatus
- Patchy lichenoid infiltrate and deep perivascular/periadnexal infiltrate
- Peri-eccrine lymphocytic infiltrate is a clue
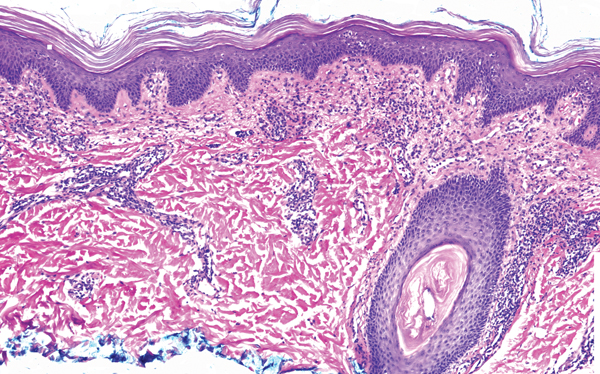
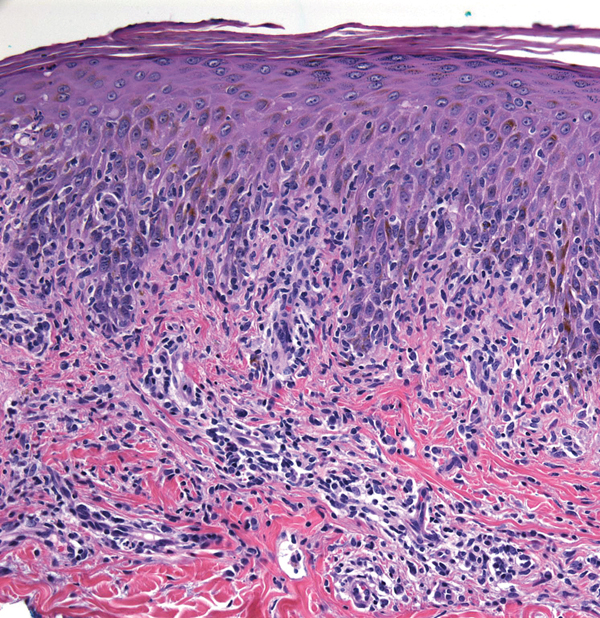
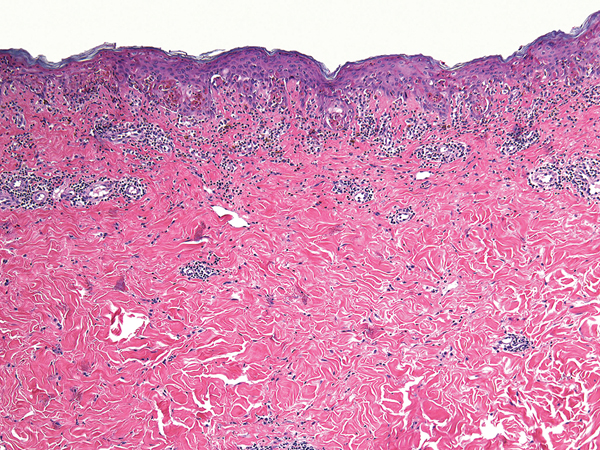
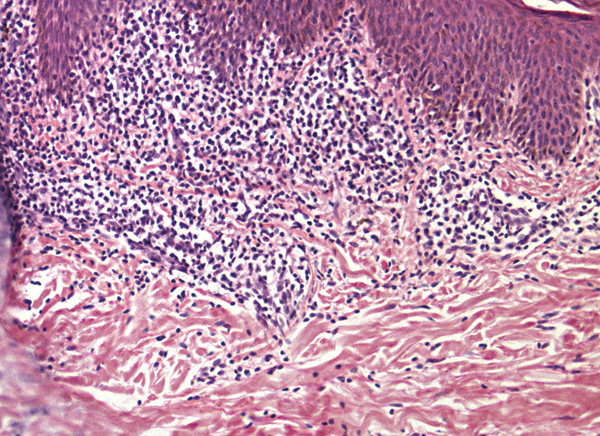
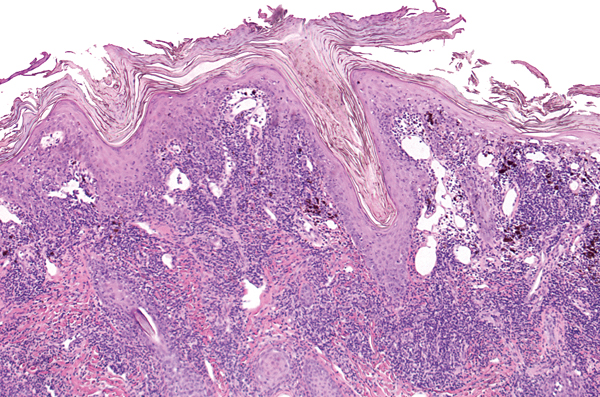
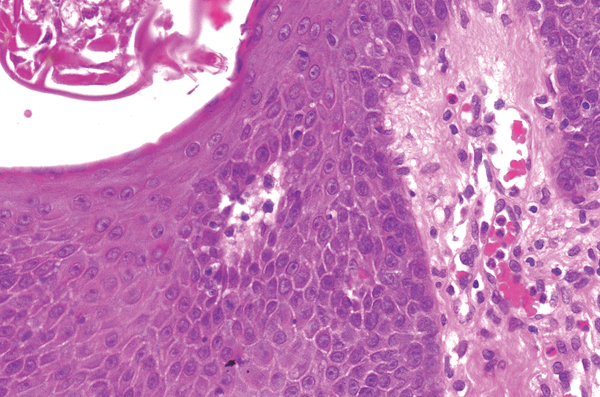
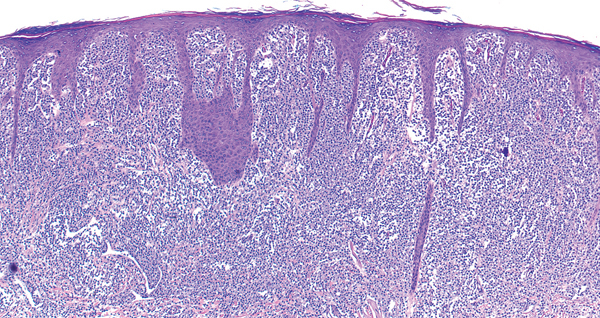
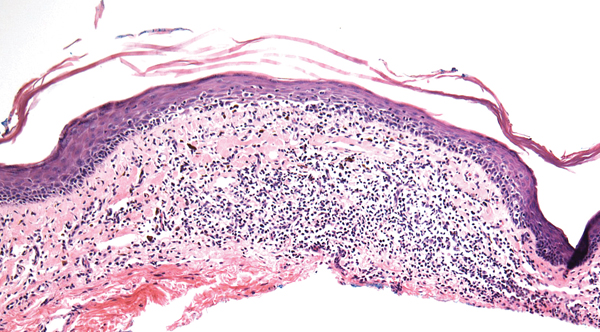
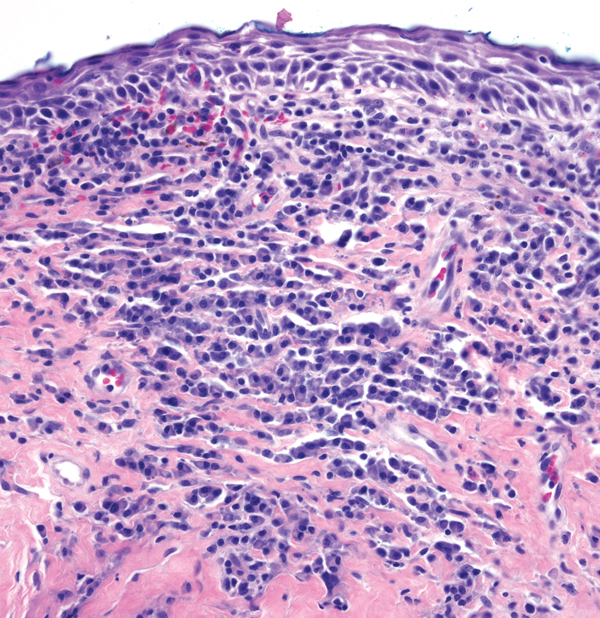
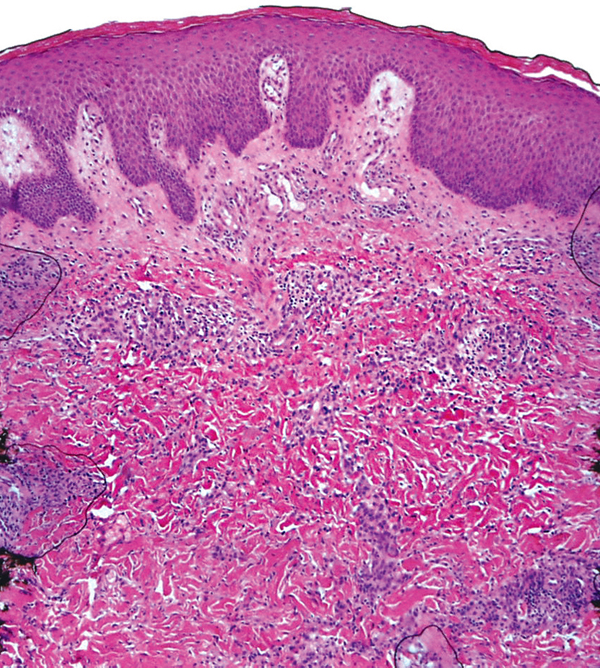
Pityriasis lichenoides et varioliformis acuta

- Lichenoid and deep perivascular lymphocytic infiltrate (wedge-shaped on low power)
- If plasma cells present, consider secondary syphilis
- Parakeratosis
- Erythrocytes in the epidermis and extravasated in the dermis
- Necrosis of the epidermis
Key differences
(a)
(b)
(c)
(d)
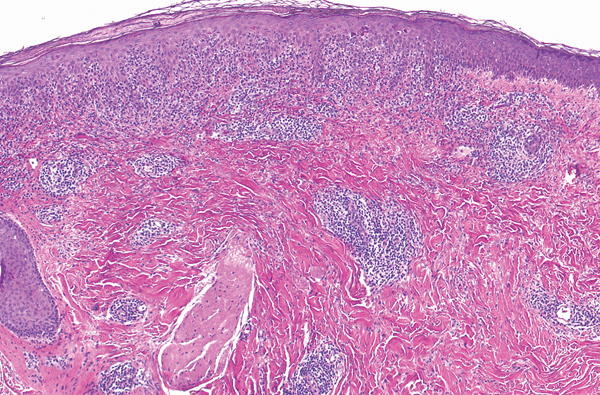
(e)
- Discoid lupus erythematosus: hyperkeratosis, epidermis may be atropic, thickened basement membrane, superficial and deep lymphocytic infiltrate
- Halo nevus: melanocytes present but obscured by lymphocytes
- Lichen planus: hyperkeratosis, hypergranulosis, acanthosis, irregular base of epidermis, heavy band of lymphocytes obscuring the epidermal base
- Lichen striatus: some spongiosis may be present, lymphocytes in the papillary dermis as well as in the deeper dermis around follicles and eccrine glands
- Pityriasis lichenoides et varioliformis acuta: parakeratosis, erythrocytes in epidermis and papillary dermis, lymphocytes peppering the base of the epidermis, superficial and deep lymphocytic infiltrate
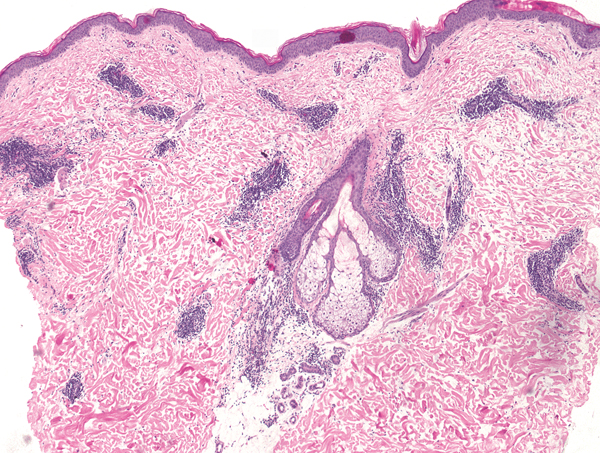
Incontinentia pigmenti
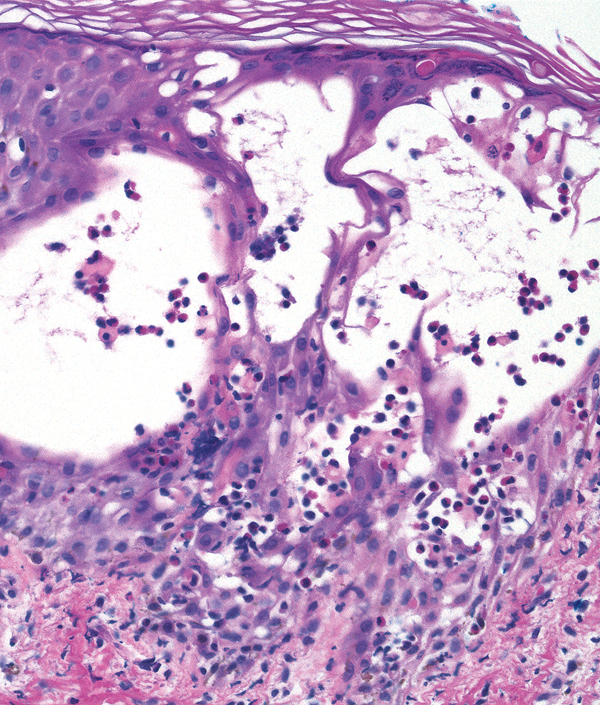
- Epidermal eosinophils
- Dyskeratotic keratinocytes in addition to eosinophils (arrows)
Pemphigus vegetans

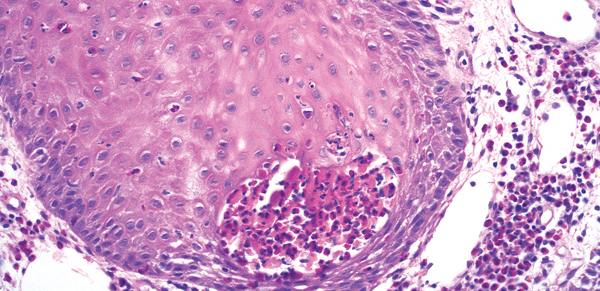
- Eosinophilic abscesses within epidermis
- Acantholysis may be absent to subtle
- Hyperplastic epidermis
Scabies
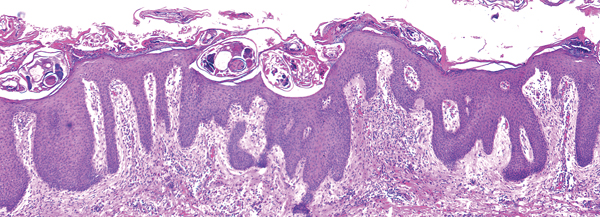
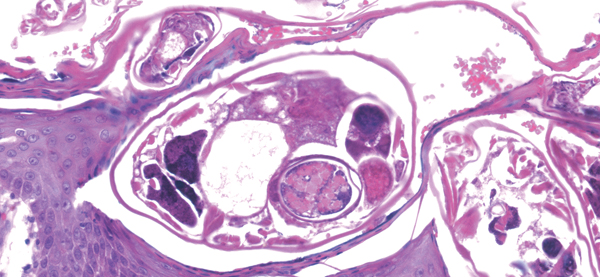
- Epidermal eosinophils
- Mites, scybala, eggs within stratum corneum
Key differences

(a)
(b)
(c)
(d)
(e)
(f)
- Allergic contact dermatitis: orderly vesicles and eosinophils in epidermis (see page 102)
- Arthropod bite reaction: prominent vesicles and eosinophils in epidermis, may see an erosion, wedge-shaped infiltrate (see page 103)
- Bullous pemphigoid: subepidermal cleft and eosinophils at base (see page 249)
- Incontinentia pigmenti: eosinophilic spongiosis with dyskeratotic cells
- Pemphigus vegetans: eosinophilic abscesses within acanthotic epidermis
- Scabies: mites/scybala/eggs in stratum corneum
Gyrate erythema
- Superficial and deep perivascular infiltrate of lymphocytes
Lymphocytes tightly cuffed around vessels
Note Differential includes polymorphous light eruption (classically has dermal edema), Jessner’s lymphocytic infiltrate, and connective tissue disorders.
Leukocytoclastic vasculitis
- Perivascular infiltrate of neutrophils and nuclear debris
- Alteration/necrosis of collagen (arrow)
- Extravasated erythrocytes
- Fibrin around vessels
Pigmented purpuric dermatosis

- Superficial perivascular infiltrate of lymphocytes (sometimes minimal)
- Extravasated erythrocytes (arrows)
- Hemosiderophages
Key differences

(a)
(b)
(c)

(d)
(e)
(f)
- Granuloma annulare: perivascular lymphocytes; interstitial/palisaded histiocytes around mucin (see page 89)
- Gyrate erythema: tightly cuffed superficial and deep perivascular infiltrate of lymphocytes, epidermis is normal
- Leukocytoclastic vasculitis: dermis looks “messy” on low power with perivascular neutrophils and nuclear debris, pink donuts of degenerated collagen, extravasated erythrocytes
- Perniosis: superficial and deep perivascular lymphocytes, perieccrine lymphocytes are a clue
- Pigmented purpuric dermatosis: perivascular (to lichenoid) infiltrate of lymphocytes, extravasated erythrocytes, hemosiderophages
- Pityriasis rosea: mounds of parakeratosis, mild epidermal spongiosis, superficial perivascular infiltrate of lymphocytes. extravasated erythrocytes (see page 104)
Langerhans cell histiocytosis

- Band-like upper dermal infiltrate
- Infiltrate abuts and involves epidermis
- Cells in infiltrate have kidney-shaped or coffee been (clefted) nuclei (arrows)
- Eosinophils may be present
Lichen nitidus
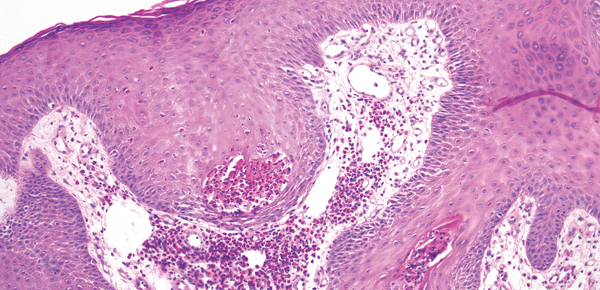
- Lichenoid infiltrate that is the “ball” being held by fingers of epidermis (the “claw”)
- Infiltrate is composed of lymphocytes and histiocytes and occasional giant cells
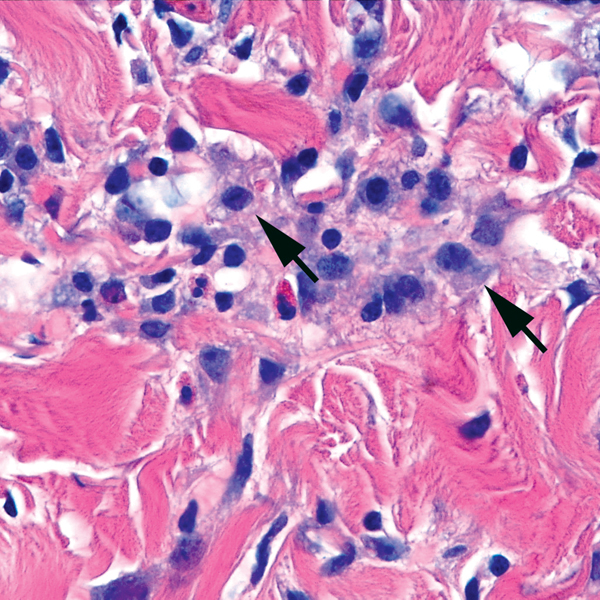
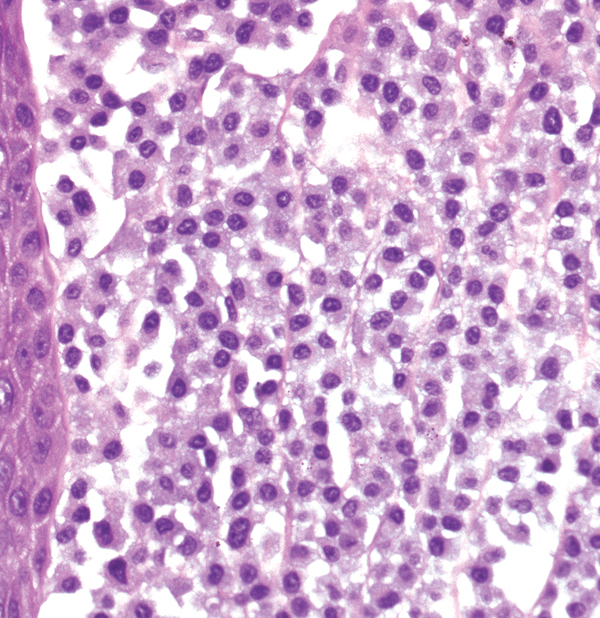
Mastocytosis
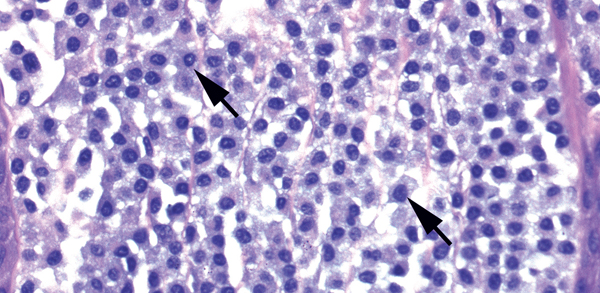
- Band-like upper dermal infiltrate (or sometimes perivascular or nodular)
- A small grenz zone is usually present
- Cells in infiltrate have round nuclei and granular gray-blue cytoplasm (arrows)
- Eosinophils may be present
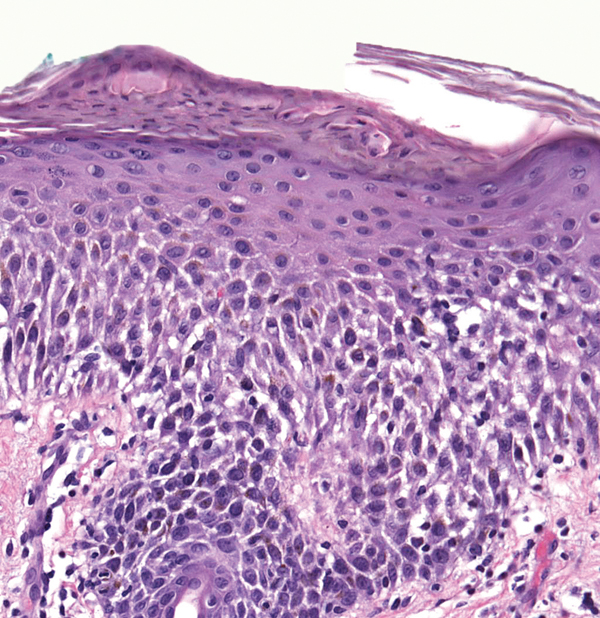
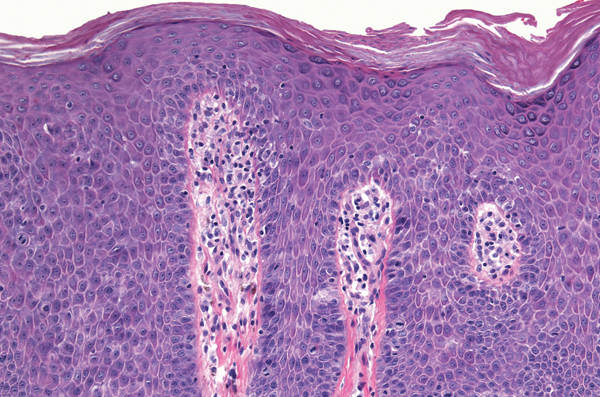
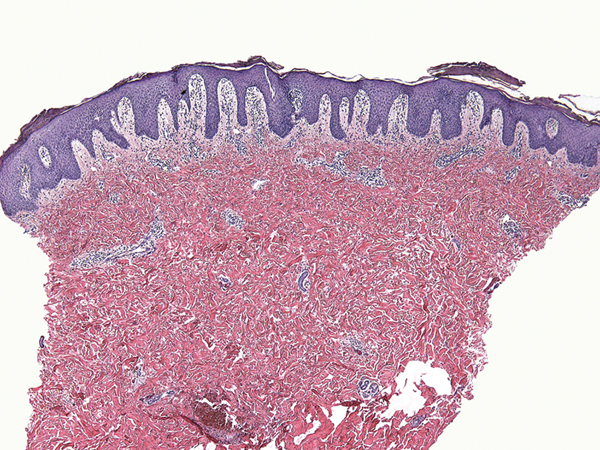
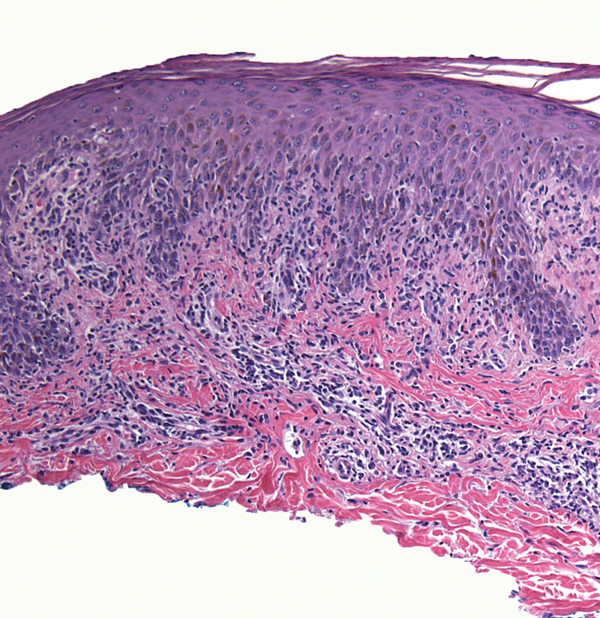
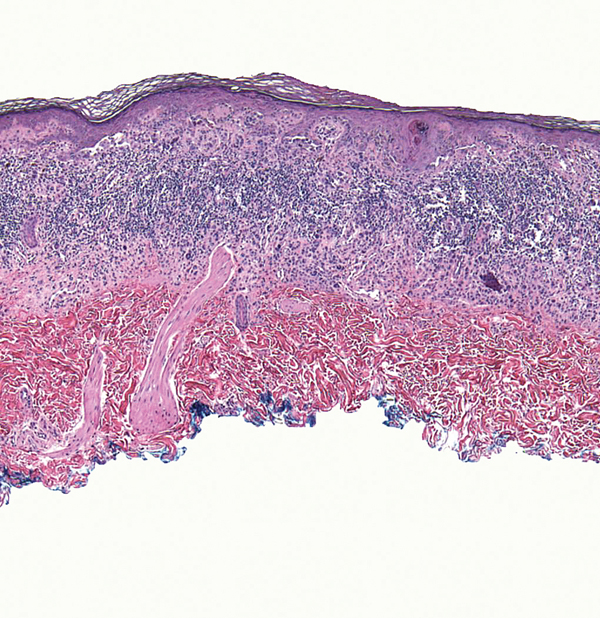
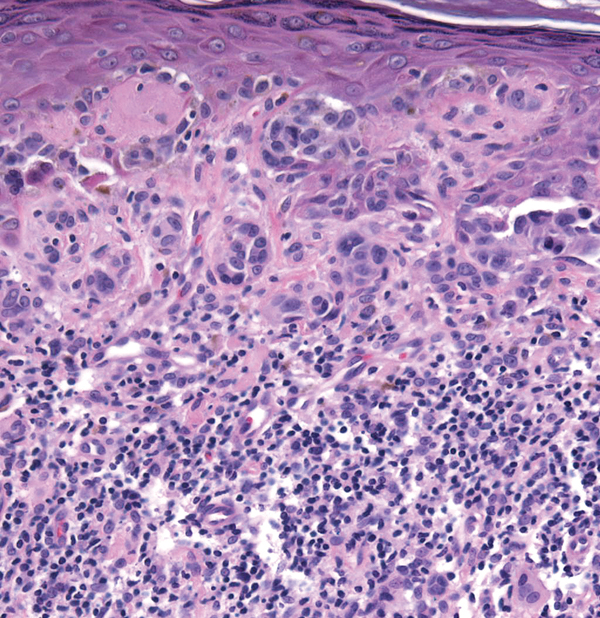
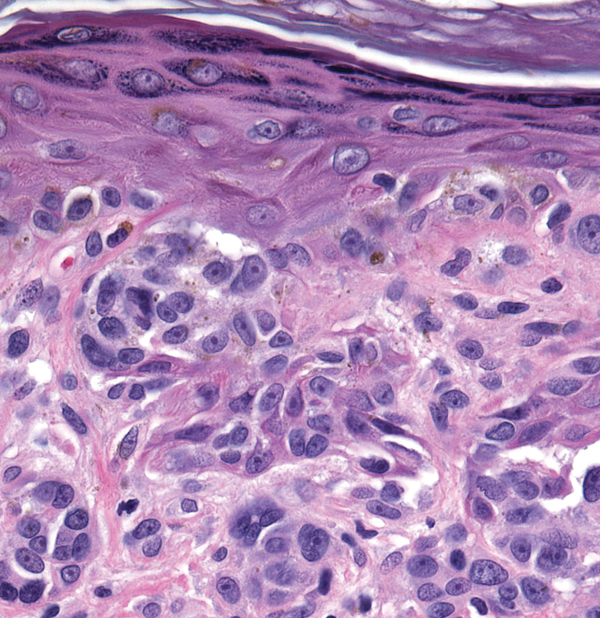
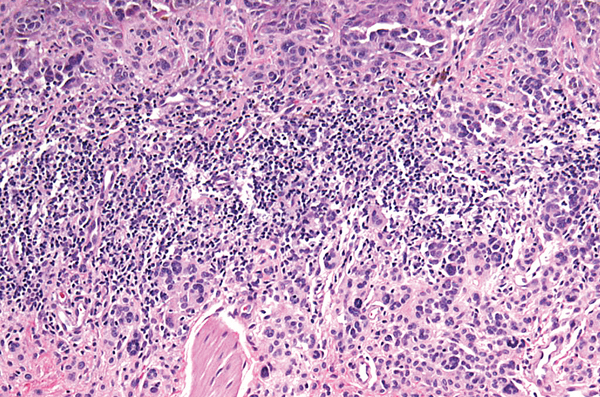
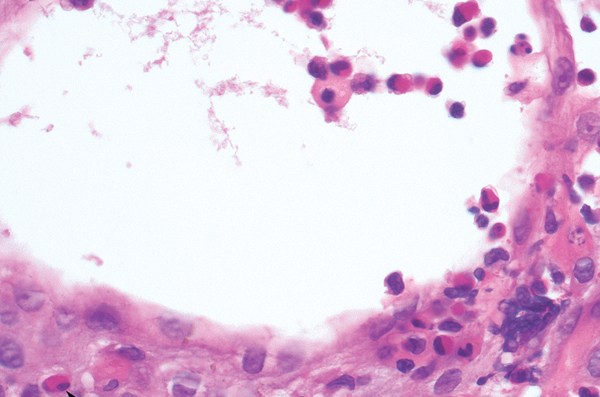
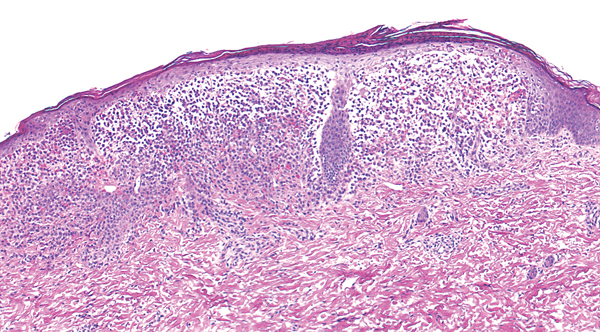
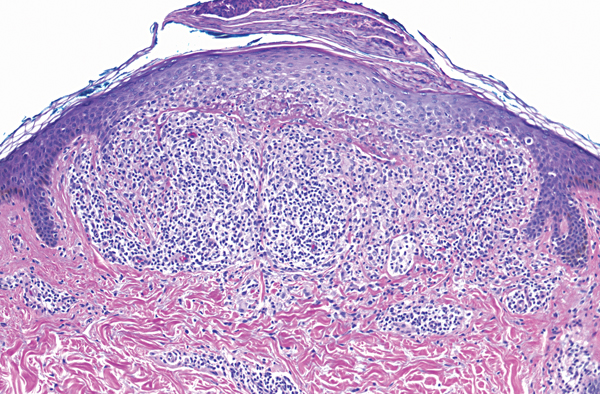
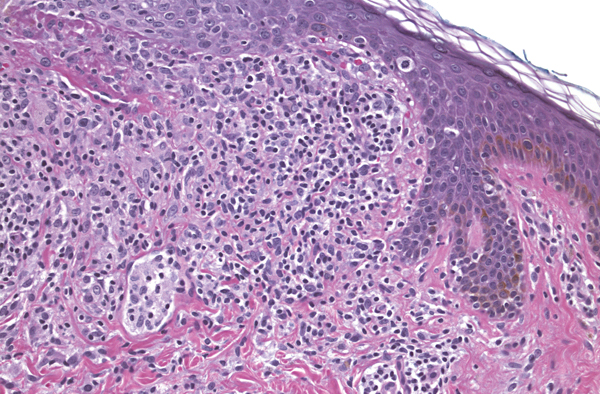
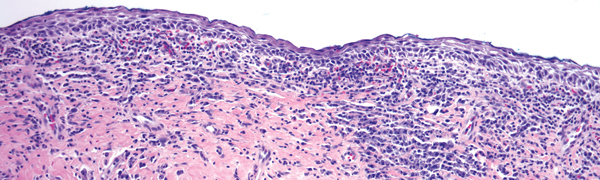
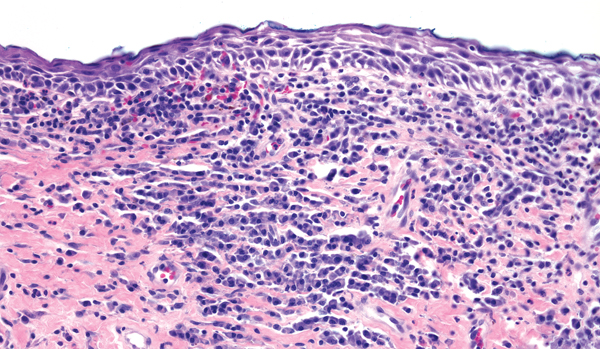
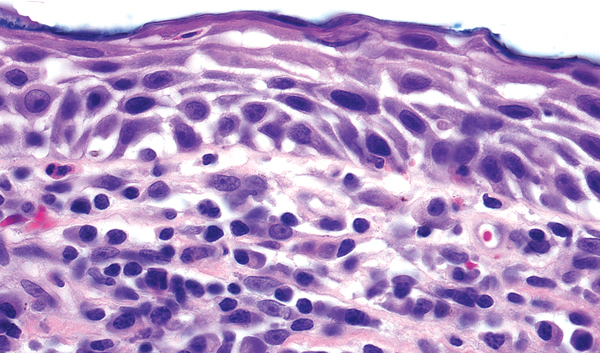
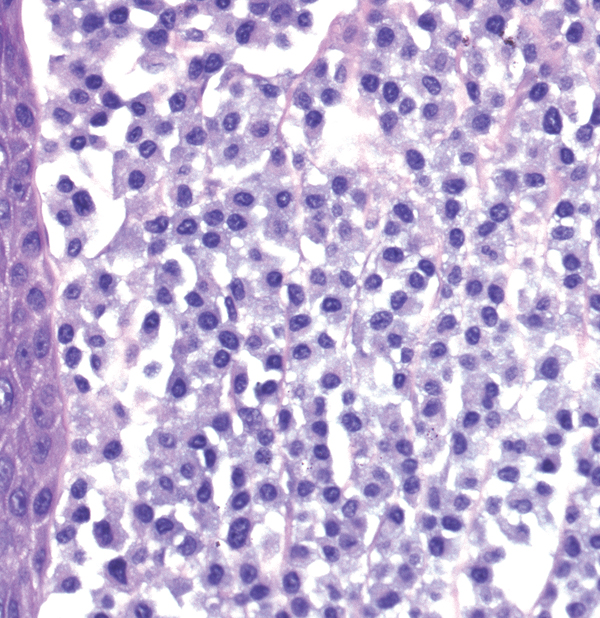
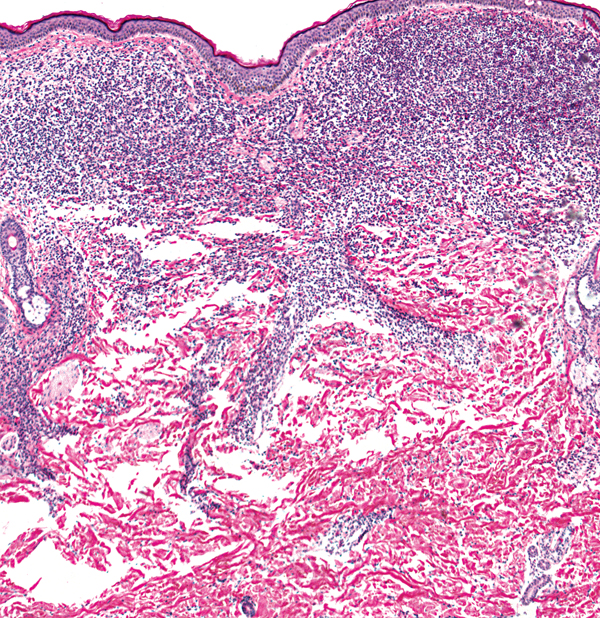
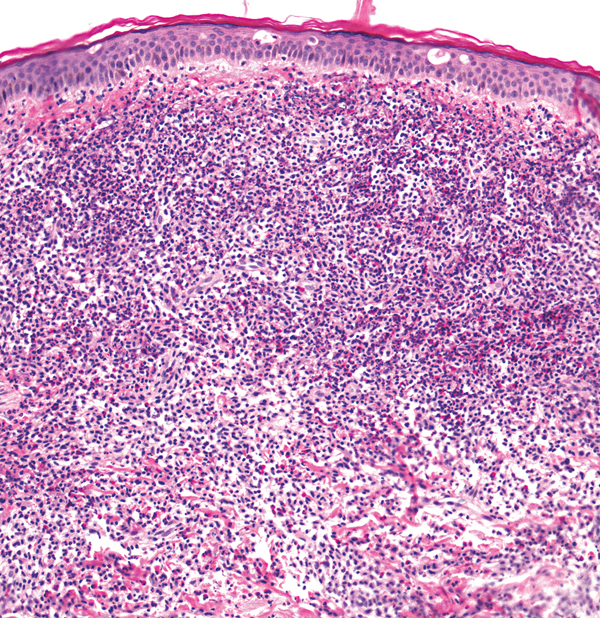
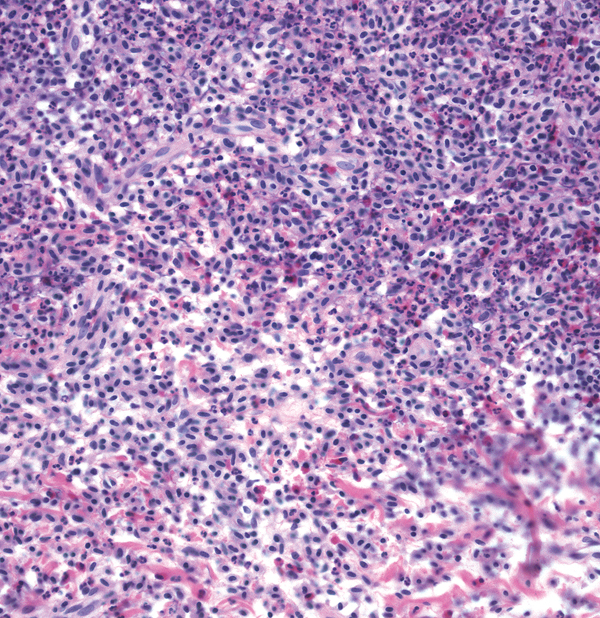
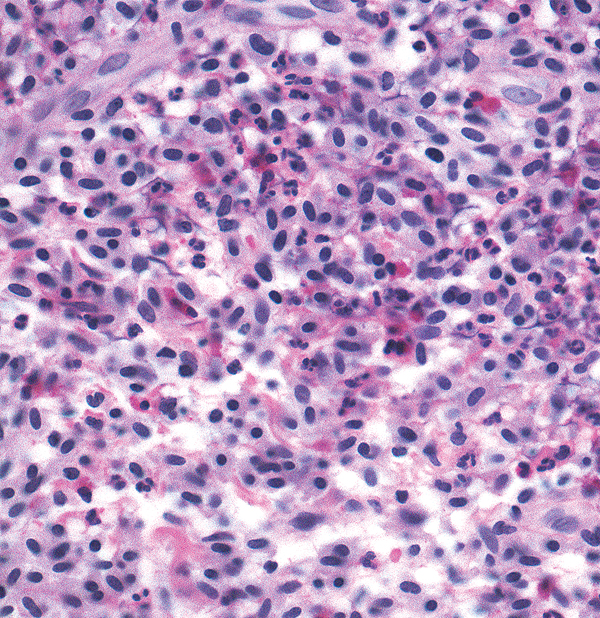
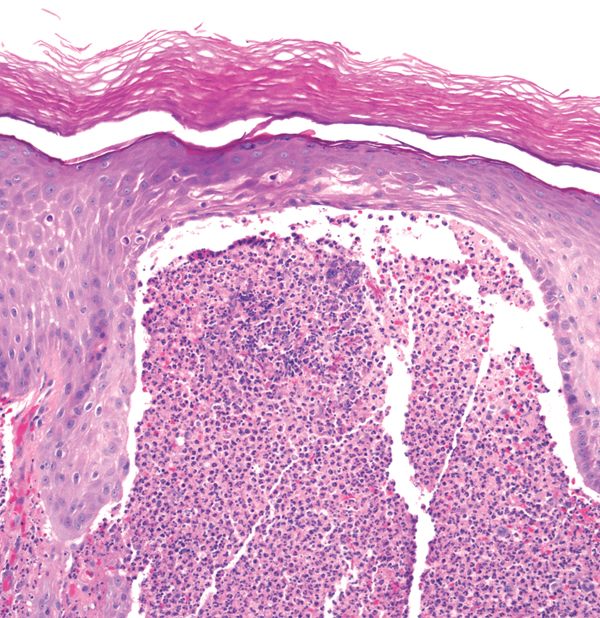
Mycosis fungoides
- Band-like upper dermal infiltrate
- Infiltrate abuts and involves epidermis
- May see Pautrier’s microabscesses
- Hyperchromatic lymphocytes
- Hyalinized papillary dermis
Zoon balanitis (balantis circumscripta plasmacellularis)
- Band-like upper dermal infiltrate
- Atrophic epidermis of diamond-shaped keratinocytes with intercellular edema
- Dermal infiltrate of plasma cells
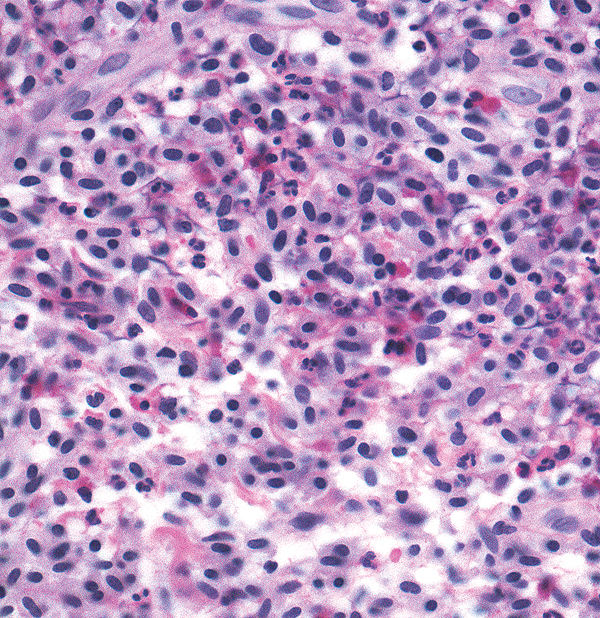
Key differences
(a)
(b)
(c)
(d)
- Langerhans cell histiocytosis: kidney-shaped nuclei
- Mastocytosis: round nuclei and slightly granular cytoplasm
- Mycosis fungoides: cells in infiltrate have atypical nuclei, vacuolar change, fibrosis in dermis, lining up of lymphocytes at dermoepidermal junction
- Zoon balanitis: diamond-shaped keratinocytes with underlying plasma cells
Acne keloidalis


- Blue dense infiltrate
- Lymphoplasmacytic infiltrate surrounds and destroys hair follicles
- Free hair shafts may be seen in the dermis
- Scarring
Granuloma faciale
- Blue dense infiltrate
- Grenz zone
- Infiltrate composed of lymphocytes, histiocytes, eosinophils, neutrophils
- Variable presence of vasculitis
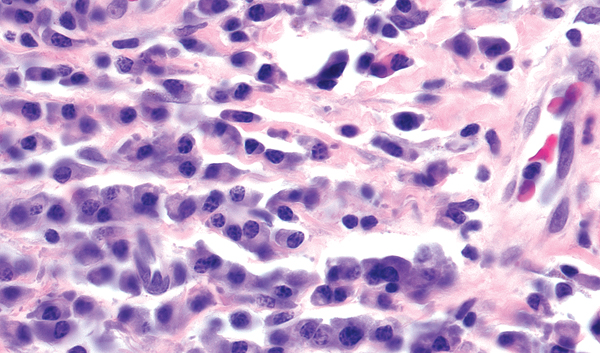
Leukemia (myelogenous)

- Blue dense infiltrate
- Infiltrate is perivascular and infiltrating through collagen
- Cells are atypical with slightly granular cytoplasm (arrows)
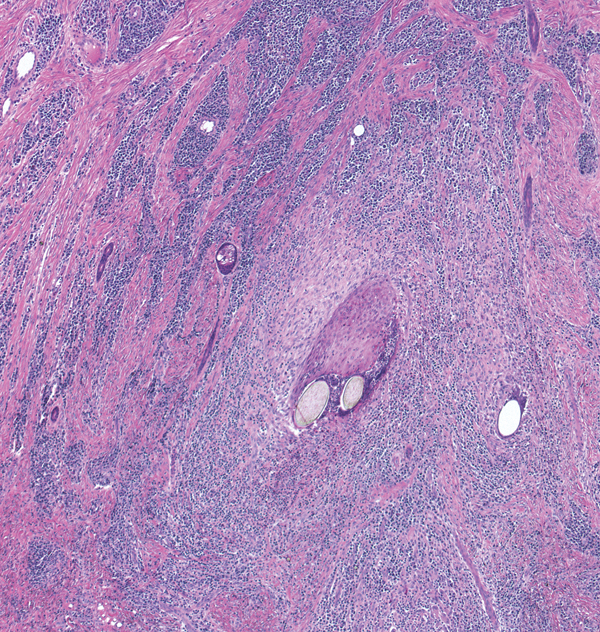
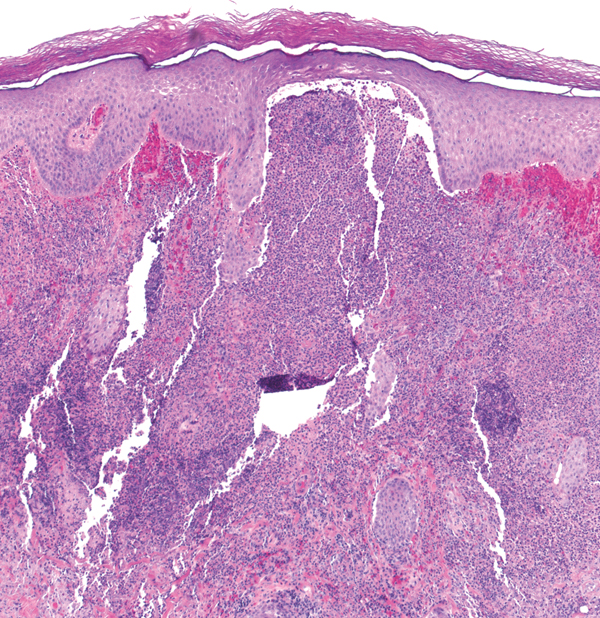
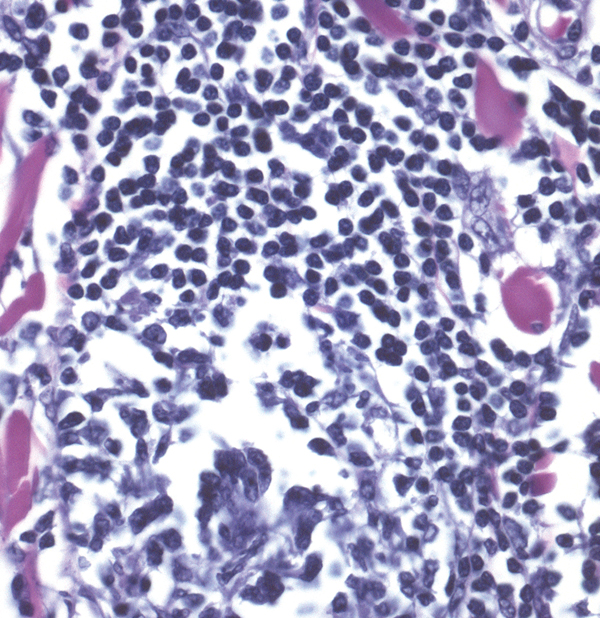
Lymphoma

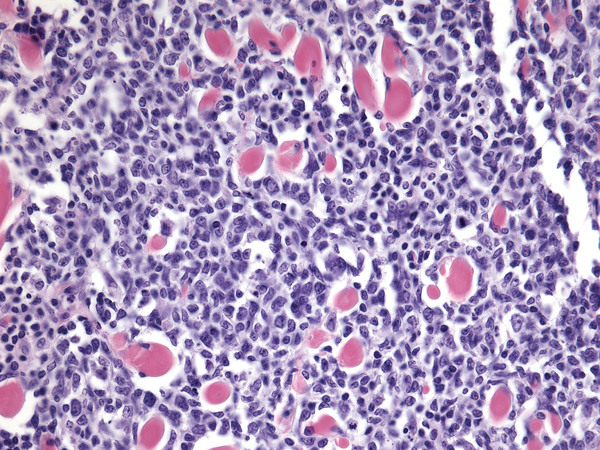
- Blue dense infiltrate
- Infiltrate composed of monomorphous lymphocytes, usually atypical
Often a “bottom-heavy” infiltrate
Note Clinical history and special stains may be critical in making the diagnosis.
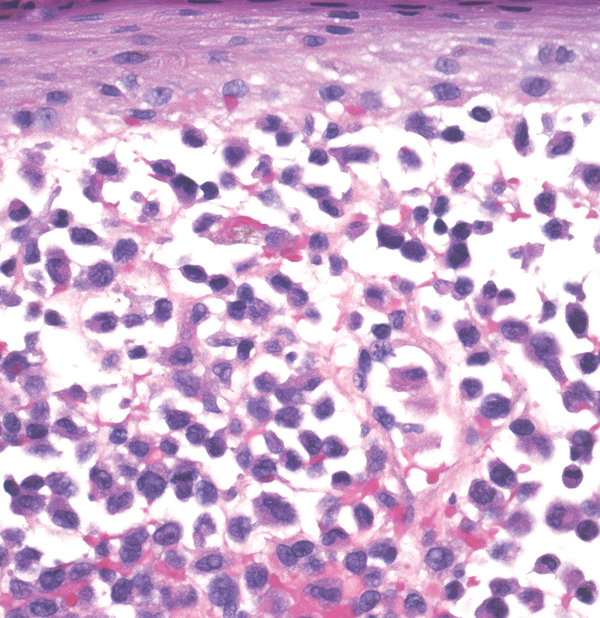
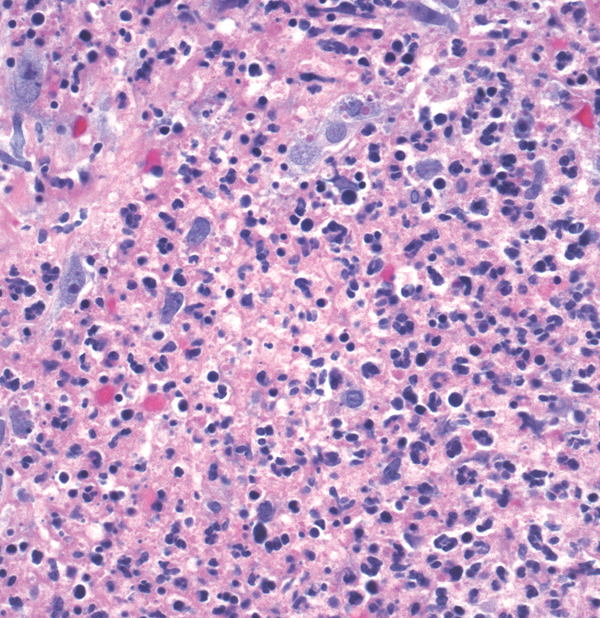
Sweet syndrome
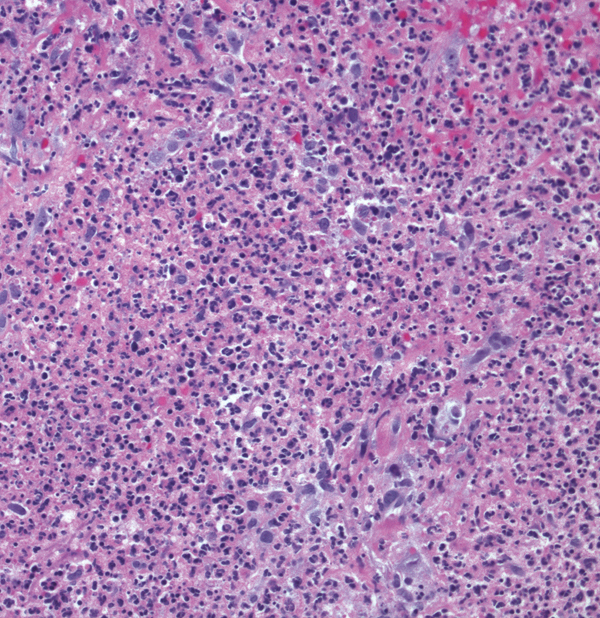
- Blue dense infiltrate
- Papillary dermal edema
- Infiltrate composed of neutrophils
- Generally vasculitis is not prominent
Key differences
(a)
(b)
(c)
(d)
(e)
(f)
(g)
- Acne keloidalis: lymphoplasmacytic infiltrate around/destroying hair follicles with scarring
- Discoid lupus erythematosus: interface changes, superficial and deep perivascular and periadnexal lymphocytic infiltrate, pigment incontinence (see page 117)
- Granuloma faciale: mixed infiltrate with eosinophils under a grenz zone, vasculitis
- Leukemia (myelogenous): atypical cells with granular cytoplasm around vessels and infiltrating dermis
- Lymphoma: monomorphous lymphocytes filling dermis
- Mastocytoma: dense collection of mast cells with “fried egg” appearance (see page 133)
Sweet syndrome: infiltrate of neutrophils
Note Infections may also have a dense infiltrate.
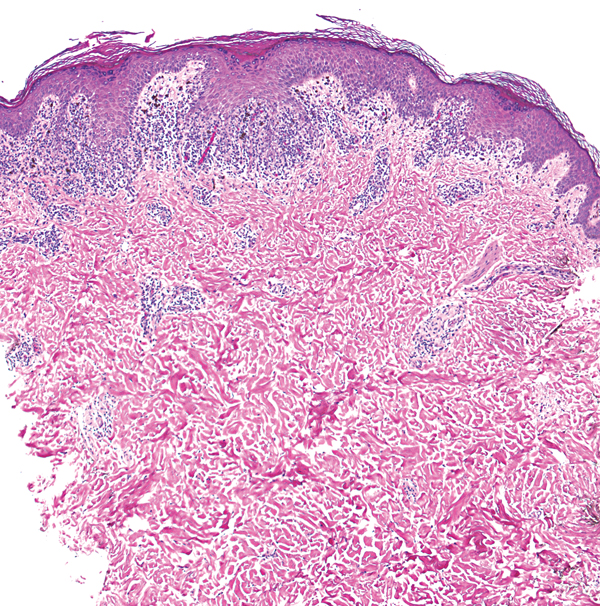
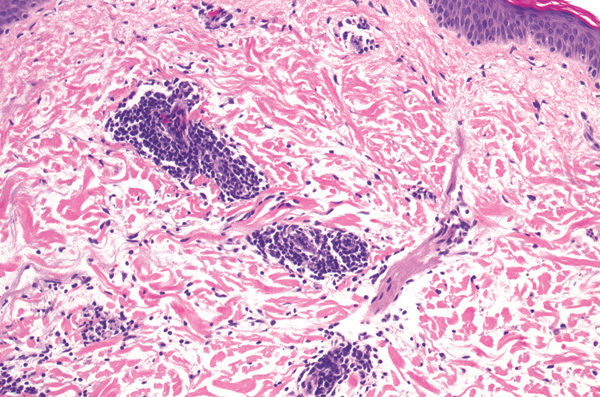
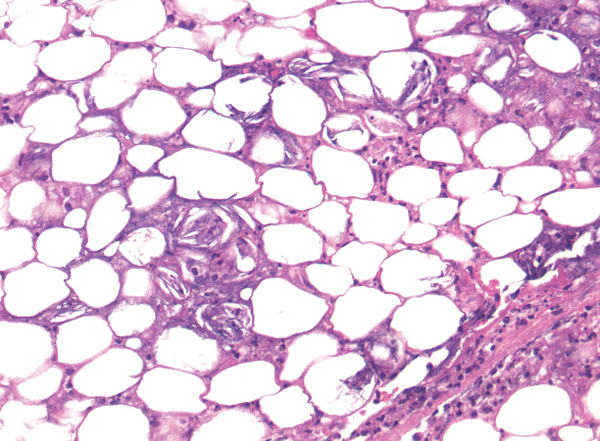
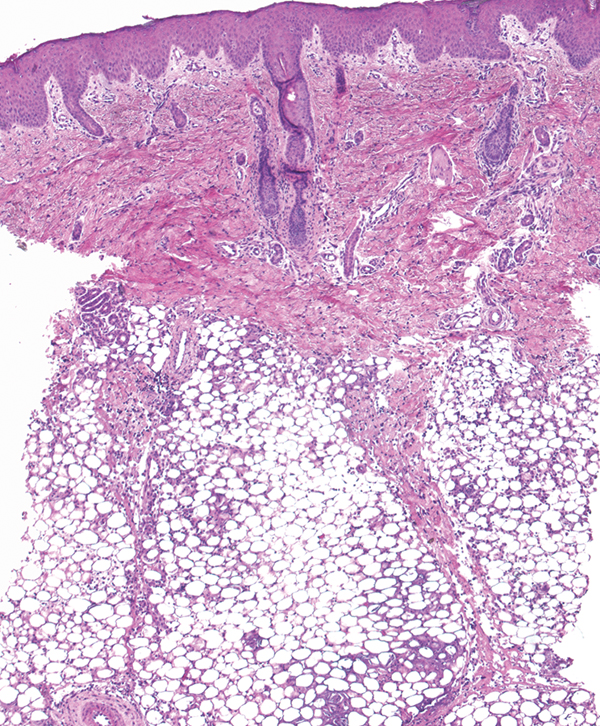
Erythema induratum

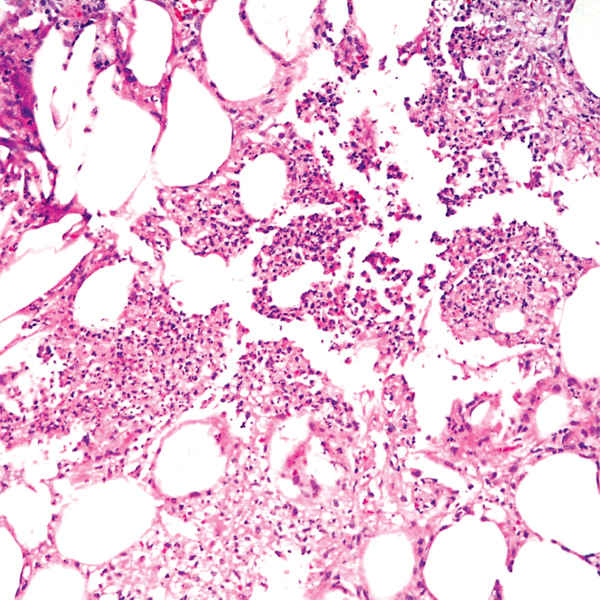
- Subcutaneous inflammation
- Lobular panniculitis with mixed inflammation (histiocytes, lymphocytes, neutrophils)
- Inflammation around vessels (vasculitis) in the septae
- “Panniculitis > vasculitis”; see polyarteritis nodosa on page 147
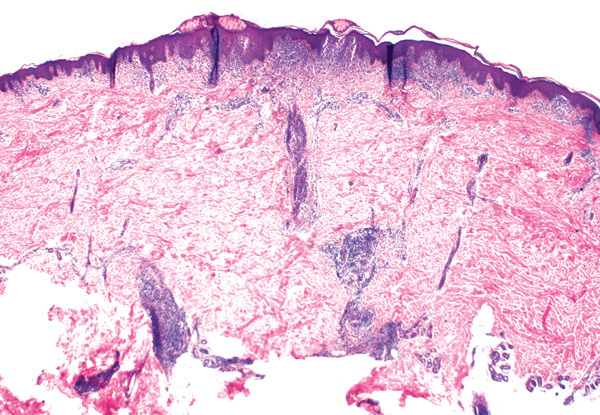
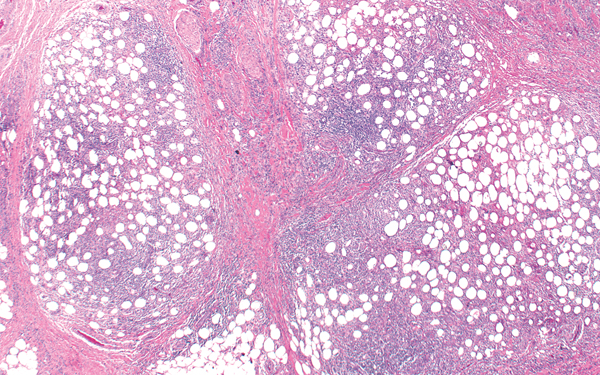
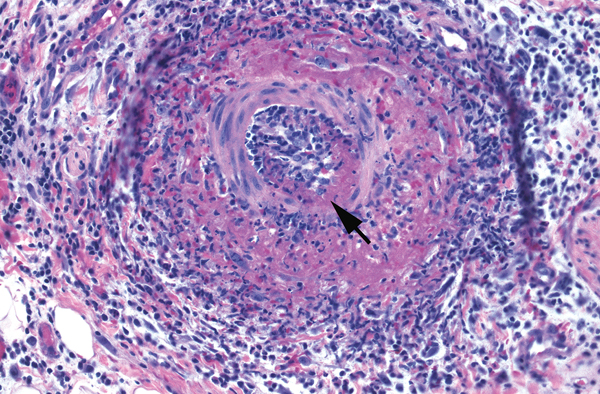
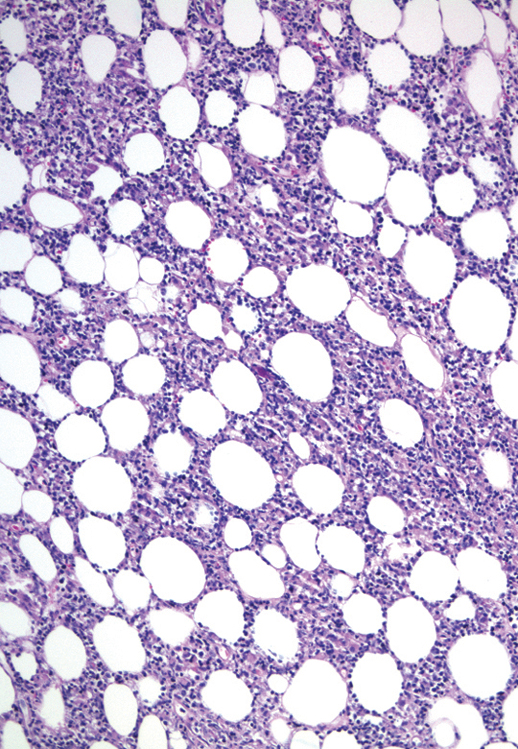
Erythema nodosum
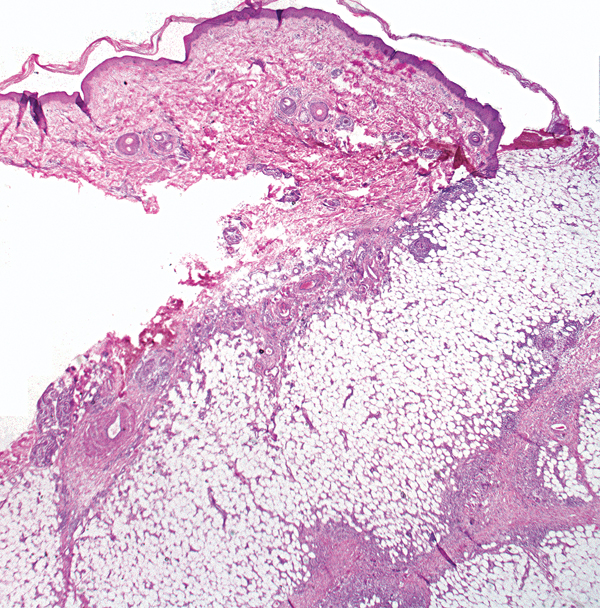
- Subcutaneous inflammation
- Septal panniculitis with thickened septae between lobules of adipocytes
- Septae contain giant cells (short arrow)
- Early lesions may have neutrophils, eosinophils
- Miescher’s radial granuloma may be seen (long arrow)
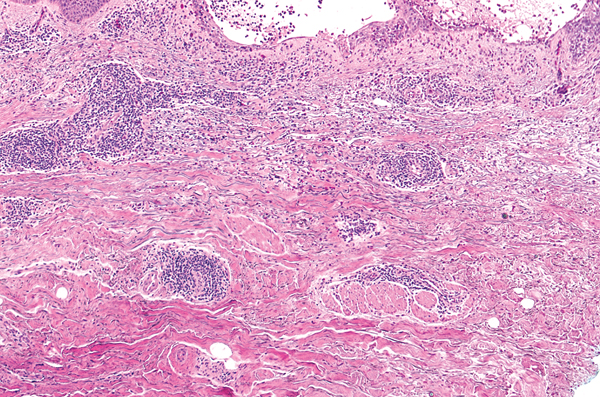
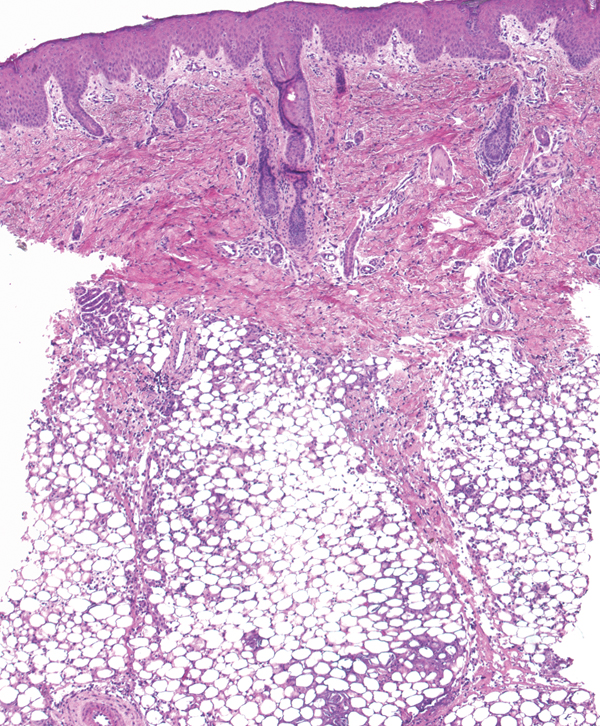
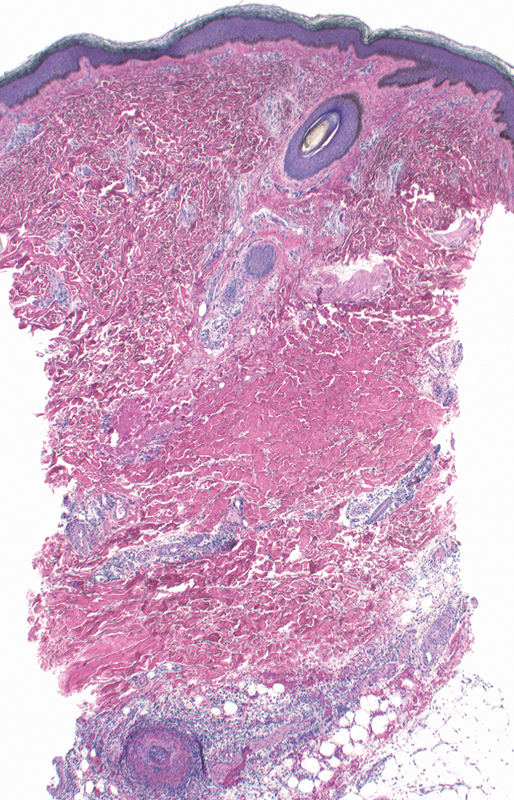
Lupus profundus
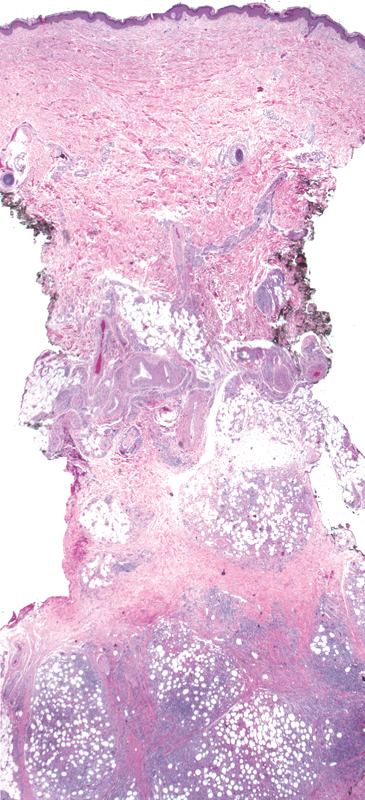
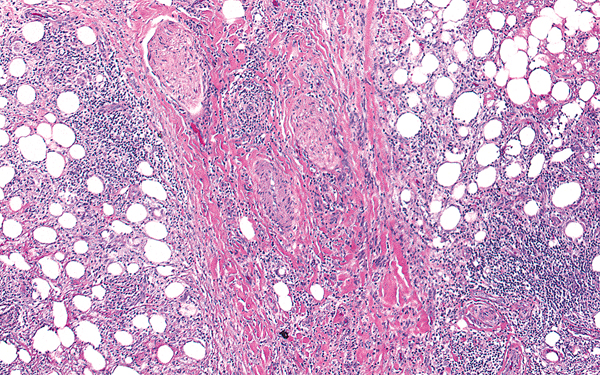
- Subcutaneous inflammation
- Lymphoplasmacytic infiltrate (lobular panniculitis)
- Lymphoid follicles may be present
- Fibrinoid (hyaline) necrosis of fat
- Later stages show hyalinization of fat (hyaline sclerosis)
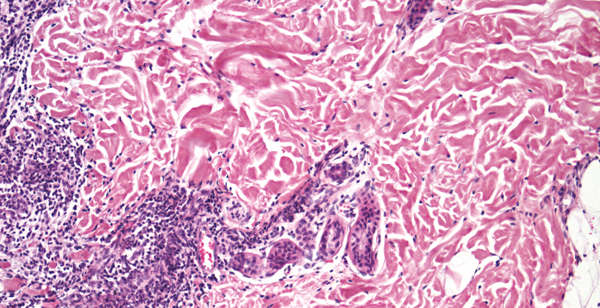
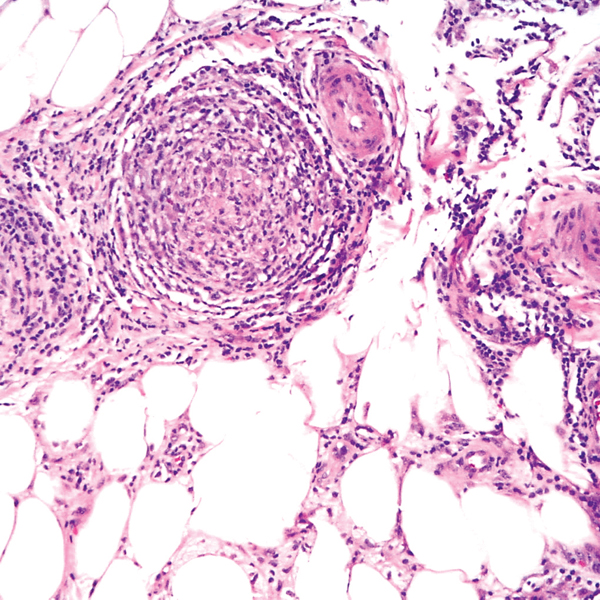
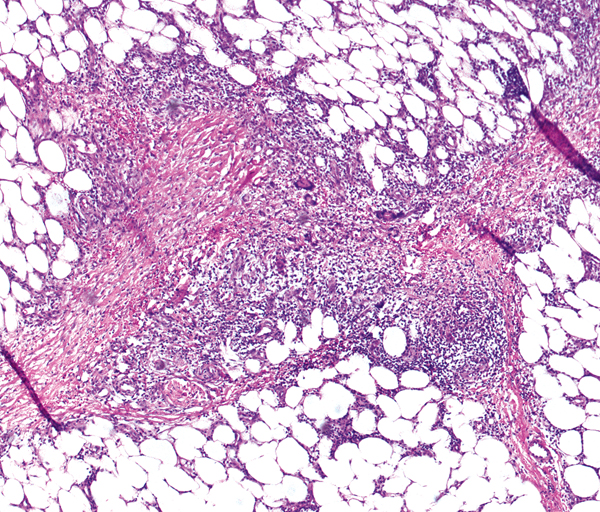
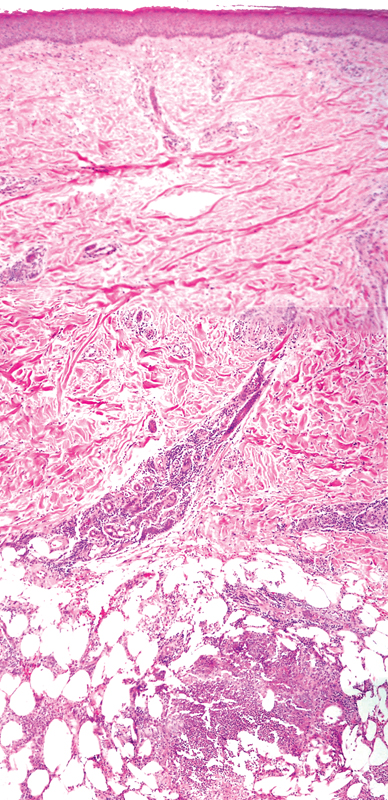
Polyarteritis nodosa
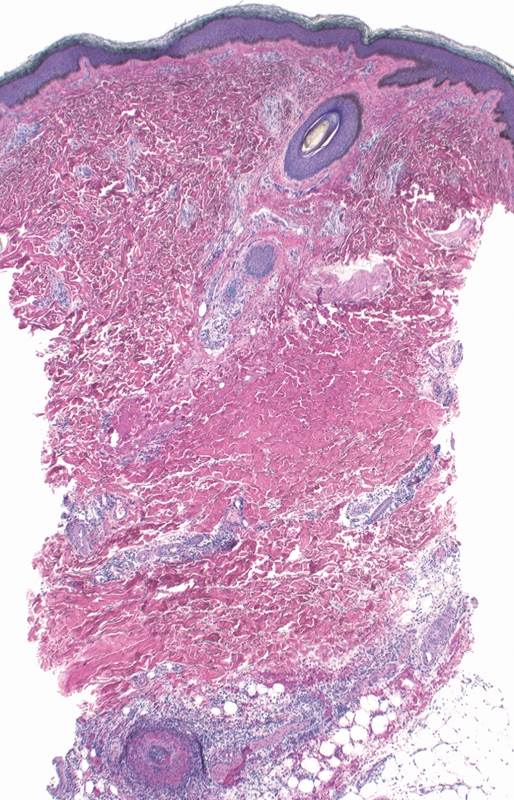
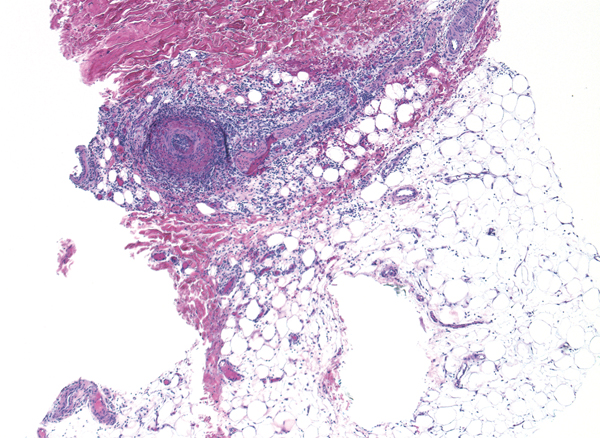
- Subcutaneous inflammation
- Septal panniculitis
- Often at dermal-subcutis junction, a large vessel is involved with inflammation (vasculitis) (arrow)
- “Vasculitis > panniculitis”; see erythema induratum on page 144
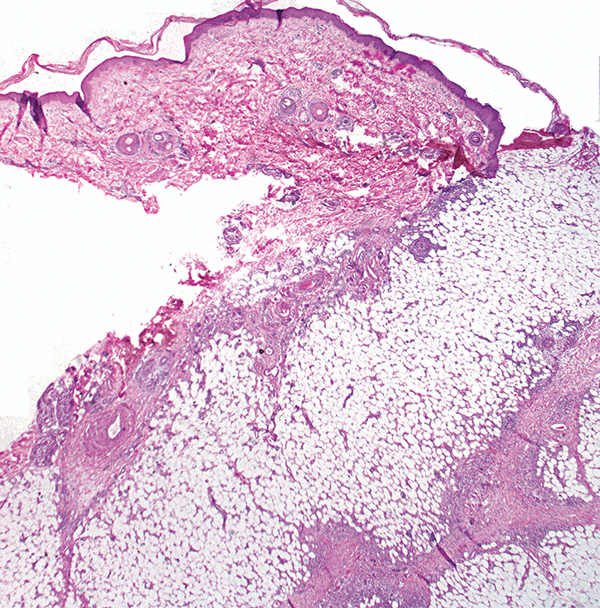
Subcutaneous fat necrosis of the newborn

- Subcutaneous inflammation
- Lobular panniculitis
Inflammation and radial crystalline shapes (arrows) within fat lobules
Note Post-steroid panniculitis can look the same.
Note Sclerema neonatorum also has crystalline shapes but lacks inflammation.
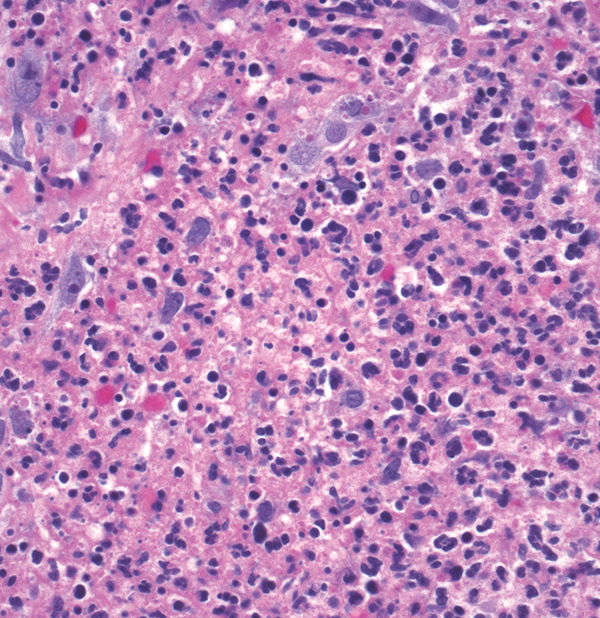
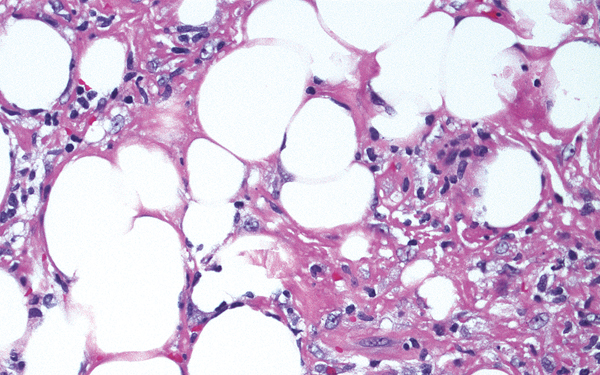
Subcutaneous T-cell lymphoma
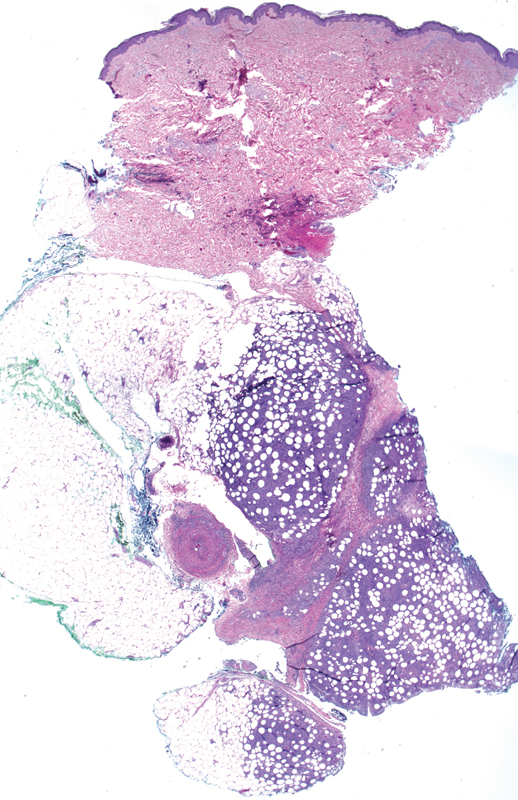
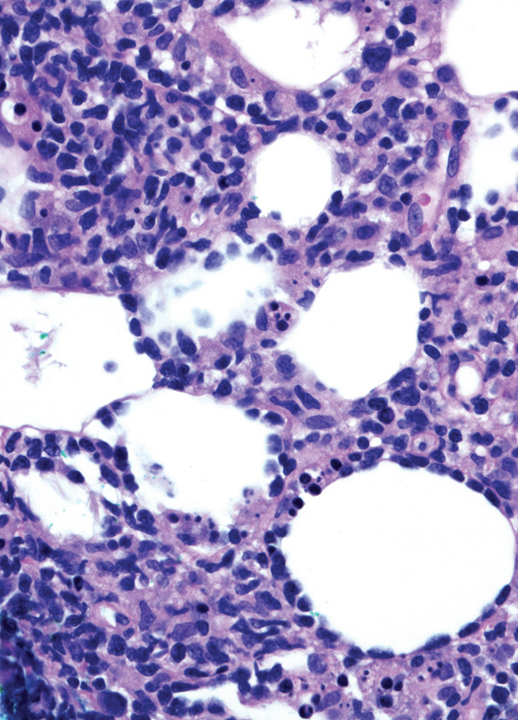
- Subcutaneous inflammation
- Lobular involvement of inflammation
Atypical lymphocytes rim fat cells (arrow)
Source: Photos courtesy of Antonio Subtil, MD.
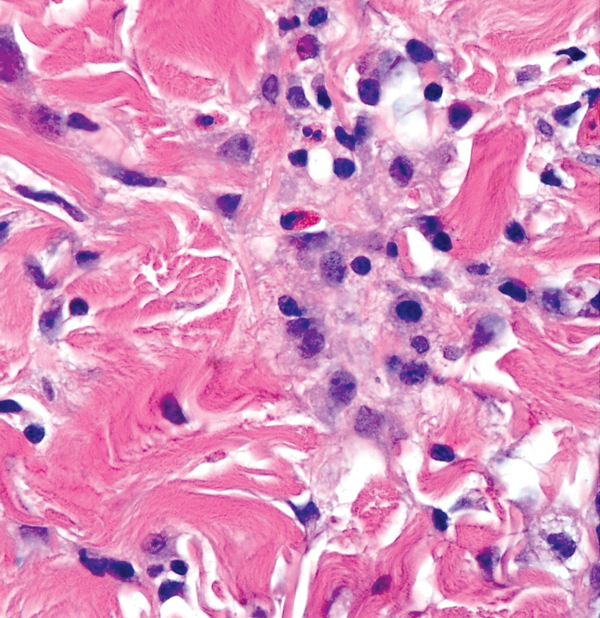
Key differences
(a)
(b)
(c)
- Erythema nodosum: septal thickening with giant cells (sometimes neutrophils and eosinophils)
- Polyarteritis nodosa: vasculitis of a medium-sized vessel, often at dermal-subcutis junction, “vasculitis > panniculitis”
- Erythema induratum: vasculitis and lobular mixed inflammation, “panniculitis > vasculitis”
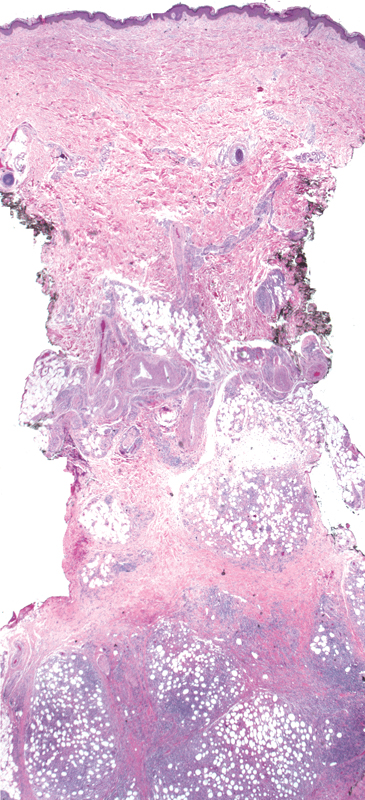
(d)
(e)

(f)
- Lupus profundus: hyaline fat necrosis, lymphoid follicles
- Subcutaneous fat necrosis of the newborn: histiocytes, some containing crystals, and lymphocytes within fat lobules
- Subcutaneous T-cell lymphoma: rimming of adipocytes with atypical lymphocytes