


You made it past the worst bit of pregnancy! I really hope by the time you’re reading this the nausea has gone and you’ve got your energy levels back. There really is nothing worse than those early weeks. Growing tiny humans is hard work, lady, and you rule! This part of your pregnancy is also called the second trimester or the ‘honeymoon’ period because, fingers crossed, you start to feel relatively normal, with some women even feeling at their best!
Never underestimate how much extra rest you still need from now up until you give birth; take advantage of those quiet moments when you could catch a few winks, even if it’s just for 20 minutes. Getting into the habit of power-napping now is a great way to teach your body and mind how to do it when your baby is here. You’ll get told by a million different people about how hard the sleep deprivation is, but one huge tip is to take daytime power- naps where possible. Babies seem to have the habit of waking lots at night for feeds and sleeping for longer periods by day (which, by the way, is totally normal for their development). So grabbing an afternoon nap when you can now will mean you’re a pro when it comes to the early days. Winning!
This stage can sometimes feel as if nothing really happens. You won’t have seen your midwife since your booking appointment, which must feel like a lifetime ago, but you’ll be due to see them for a follow-up check by 18 weeks. At this appointment, your urine will be checked for protein, your blood pressure will be checked and, most excitingly, your midwife will be able to hear your baby’s heartbeat for the first time with a small device called a sonicaid. The heartbeat can range from 110 to 160 beats per minute, but at this stage in pregnancy it will most likely be in the higher end of this range. Your midwife will reassure you what’s normal. It’s not recommended that you buy or use a home Doppler device to listen to your baby’s heartbeat. The Kicks Count charity give the following advice to expectant parents:
It is vital that medical intervention is sought when the baby still has a heartbeat in all incidences of reduced fetal movement. So if you have any concerns about your baby’s movements contact your midwife, do not rely on a home doppler. Assuming the home doppler is being used properly and is not picking up the mother’s heartbeat or the placenta, the presence of a heartbeat does not indicate the baby is well. Any interventions that could save a baby in distress would need to be done when the baby has a heartbeat; leaving it until there is no heartbeat is too late.
You may have heard of all sorts of old wives’ tales about the rate of your baby’s heartbeat. If it sounds like a train, it’s a boy, if it sounds like galloping horses, it’s a girl. Both are incorrect: how can the rate at which your baby’s heart beats tell you its gender? The heart rate is determined by what your baby is doing at that moment. Think about it: if the baby is very active its heart rate speeds up; if it’s slower your baby is probably having a snooze. So don’t use these ‘theories’ apart from maybe as a bit of a fun guessing game between you and your partner. The only reliable way to find out the sex of your baby is by a scan or waiting until he or she arrives!
Probably the most commonly asked question when pregnant is ‘are you going to find out the sex of the baby at the 20-week scan?’ (Followed by ‘when are you due?’ – remember to add a week on to your estimated due date – see here.)
Despite being a slightly irritating question, no matter how well intended, it will be asked by everyone from your friends to your mother-in-law and the person on the checkout at the supermarket. You and your partner need to have a serious chat and decide, well, are you? It is a question that divides couples across the globe. And, of course, there are advantages and disadvantages to each argument: pros and cons that – if you’re not careful – you can end up arguing about until you’re blue (or pink) in the face.
There’s no right or wrong answer – it’s a choice that each couple has to decide on – but ideally think about it before the 20-week scan, unless you want an argument with a sonographer present, which could be awkward . . .
I’ve spoken to lots of women – and men – on this matter and have come up with a list of the most popular pros and cons of finding out. This list won’t necessarily give you the answer – it is such a personal decision, and it has to be right for you – but if you’re undecided it might give you some things for you and your partner to think about.
Remember, once you find out and the sonographer utters those words ‘boy’ or ‘girl’ there’s no going back. However, there is always that very small chance that the scan isn’t accurate, so don’t go crazy and paint the nursery pink just in case she turns out to be a he! Also, some hospitals have a policy not to tell women the gender of their baby – so find out if yours does or not.
PROS
• You can focus your name-deciding on one gender (potentially saving hours of tedious debating).
• You can decorate the nursery in more gender-specific colours rather than sticking to the various shades of white or yellow.
• And the same goes for baby clothes.
• If this is your second baby you can help your older child prepare for a sibling. It also helps you decide whether you need to buy a new set of clothes or can just use hand-me-downs.
• Some couples say they felt closer and bonded to their unborn baby knowing the gender before birth, calling it ‘he’ or ‘she’ rather than ‘it’.
• Friends and family have more direction when deciding on a gift.
• Avoids any element of disappointment if you had your heart set on a boy or a girl.
CONS
• Why spoil one of life’s greatest surprises?
• Some women say it gave them an increased incentive during labour.
• It will not make you love your child any more.
• Does it really matter? As long as it’s healthy.
• Finding out the gender is not 100 per cent accurate.
• Buying neutral-coloured clothes means you can use them for future sons or daughters, thus saving money.
Personal support from a close female friend or relative throughout pregnancy, labour and the post-partum period is a tradition shared by many cultures over thousands of years. In today’s busy world, not everyone has such a support network, and with maternity services being cut constantly, mums-to-be are left wanting more women-centred, nurturing care. This is how doulas came to be.
A doula is experienced and trained to support a mum during pregnancy, labour and beyond, and can fill the gaps in busy maternity services by providing continual support to the woman and her partner throughout the childbearing year. A doula does not replace the midwife and medical staff, but aims to work alongside them in harmony. Neither does she replace the birth partner; instead, she will provide support so that they can focus on loving and encouraging you appropriately. If there will not be a birth partner present then a doula will fill that role too, helping you to gather information about the options available to you for birth and afterwards.
During your labour, your doula will be a constant, calming presence to guide and support you through the birth. Ideally, you will feel unobserved but very well cared for, creating the optimum conditions for a healthy labour.
Every couple and every woman is different, with their own ideas about their ‘perfect birth’. It is a doula’s job to get to know you and your partner, and to support whatever your vision is. This is achieved by:
• Meeting a few times before the birth/getting to know you and your wishes.
• Examining issues from previous labours/settling first-time nerves.
• Talking through the stages of labour and what to expect.
• Discussing techniques to help you cope with the birth itself.
• Helping you to write a birth plan.
• Helping pack your hospital bag, or make a list of what you need for a home birth.
During the birth your doula is an extra pair of hands to help with anything that needs doing – filling the pool, making tea, having a tidy-up, massaging your back, entertaining the kids – you name it, they can do it! They are there to support mother and birth partner with calming words, helpful suggestions to keep you comfortable, and reminders of what a fantastic job you are doing. Your doula will join you at whatever part of the labour you’d like her to – early on or later into it – and will stay with you until your baby is born, you have had a shower and the baby has had a feed. After this they will tuck you up in bed with some tea and toast and leave you to marvel at your baby and all that you have achieved.
Your doula will be available for questions and chats from the time of booking, and will go on call for you (available any time of day or night) from two or three weeks before your due date until your baby is born. For this reason a doula will only take one or two women a month, unless she works in a team of doulas, in which case they may take more bookings. Ask your doula how she works and pick one who suits you best.
And now for the statistics! A recent report showed that women who had the support of a doula during labour had:
• labour duration reduced by 25%
• the odds of forceps reduced by 40%
• 30% reduction in requests for pain relief
• 60% reduction in use of epidural
There are hundreds of doulas listed on www.doula.org.uk – you can have a read of their profiles, meet for an informal cuppa and see who you click with. The doula you feel most at ease with is the doula for you! Doulas’ fees range from between £250 for a mentored doula (see the website for more details on this) up to around £2,000.
I love this quote by John H. Kennell, MD:
If a doula were a drug, it would be unethical not to use it.
The nausea is waning. Hell, you might even be starting to glow! You’ve only gone and made it to your second trimester. This is allegedly the good ‘middle bit’ before you start dealing with piles, gargantuan nipples and uncontrollable wind. (You’ve got that already? Totally normal.) It’s also the bit where your baby starts noticeably growing. Nutrition is the cornerstone of a healthy pregnancy, but chances are you’ve consumed your fair share of junk food over the last few weeks, especially if you’ve been suffering from morning sickness or fatigue. Here then are a few tips to get you back on track.
• Try starting the day with hot water and lemon. It’s a good alternative to caffeine and jumpstarts your digestive juices.
• Focus on the quality, rather than the quantity, of food (unfortunately, the school of thought that said you should be eating for two has closed down).
• Try to make better choices, rather than perfect ones. We all know fresh, unprocessed food is best but if you accidentally inhaled a box of doughnuts for breakfast, don’t beat yourself up.
• Omega-3s are your best friends and great for brain health – yours and your baby’s. Find them in pumpkin seeds, hemp seeds, chia seeds, walnuts, eggs and dark leafy vegetables, as well as low-mercury fish such as sardines, mackerel and wild salmon.
• Drink lots of water. Constipation is the LAST thing you need right now.
• You’re using a lot of iron to make all that extra blood for your baby. Boost your intake with green leafy veg such as spinach or kale, good-quality (preferably organic) lean meat, beans, lentils, cashews and pumpkin seeds. Try a watercress and baby spinach salad with lightly fried halloumi and ripe papaya (vitamin C aids iron absorption).
• Try taking a good probiotic or add a natural source such as kefir (fermented yoghurt) to your diet. Good gut health is all-important.
• Chew your food really well and eat slowly. Heartburn and indigestion are common in pregnancy and often get worse as your growing baby starts putting the squeeze on your internal organs.
• Fill your fridge with healthy, easy-prep foods: avocados, quinoa, yoghurt, fresh berries, nori wraps, energy bombs (see here), eggs, salads, juices, smoothies, sweetcorn and almond butter (delicious with apple slices).
SOURCE OF PROTEIN, IRON, CALCIUM AND VITAMIN C
Mix 4 tbsps of chia seeds with 250ml of almond milk. Add a blob of yoghurt, a tsp of vanilla paste, some desiccated coconut and a sprinkle of cinnamon. Leave in the fridge overnight. In the morning add fresh berries, pomegranate, nuts, goji berries, seeds, nut butter – whatever you have.
CONTAINS FIBRE, IRON, VITAMIN C AND E, CALCIUM, POTASSIUM, MAGNESIUM AND ZINC
Blitz a handful of kale, a handful of spinach, juice of half a lemon, a cup of almond milk, half a pear, half a banana and a tbsp of almond butter.
FULL OF OMEGA-3, CALCIUM, FIBRE, VITAMIN D, B6, B12, FOLATE AND CHOLINE
Blitz 120g defrosted peas with 2 eggs. Fold in 30g rice flour. Stir in 125g chopped red pepper (or mushrooms or ham – whatever you have), 60g crumbled feta, a chopped red chilli, 3 chopped spring onions, small bunch of chopped parsley, salt and pepper. Heat a tbsp of coconut oil in a frying pan and spoon in a large dollop of batter; spread out with a spatula. Heat gently until it browns and firms up, then flip to cook the other side.
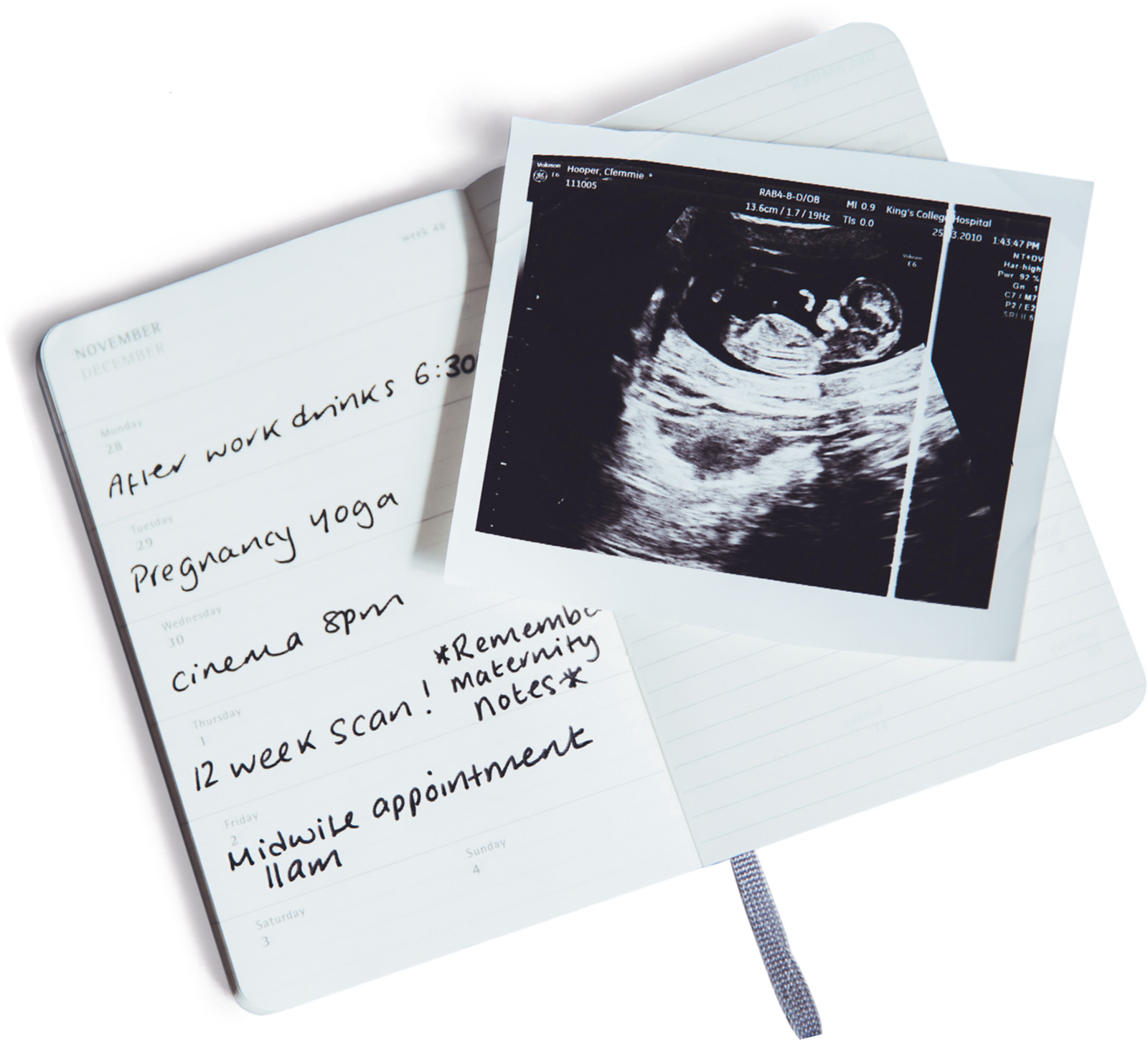
Now that you’re hopefully feeling better, you’re probably eagerly waiting for those first precious feelings of your baby moving in your tummy. During your 12-week scan your baby is often so active in there, the sonographer can find it hard to take the required measurements. During the scan with my twins they looked as if they were taking part in a Zumba class. But isn’t it bizarre that you can’t feel a single movement? It can sometimes make the whole experience very surreal and abstract: is that even my baby and my uterus? Small, gentle kicks are also known as ‘quickening’ and can be so subtle most first-time pregnant women brush them off as hunger pangs or wind passing through their tummy. Everyone feels their baby move at different stages: some as early as 15 weeks and some not until after the 20-week scan. There is no right and wrong here; it’s based on lots of different factors.
• The number of pregnancies you’ve had. Most second- and third-time pregnant women report that they felt their baby move earlier, mainly due to the body knowing and recognising those feelings as baby and not wind.
• Where the placenta is positioned. At your 12-week scan the sonographer will have detected your placenta and said whether it was anterior (at the front of your uterus) or posterior (at the back of your uterus). If you have an anterior placenta the initial kicks may not feel as strong in the early stages as your baby has a big fat squidgy cushion to kick against.
• Your physique. We are all designed differently and come in all shapes and sizes – some of us are blessed with toned washboard stomachs, some are more like me – a little loose and wobbly around that area. Very slim women do seem to be able to feel those first flutters earlier.
• What you’re doing. If you’re busy at work or rushing about you’re not going to feel those subtle movements, which is why lots of women say they first felt them when they were lying still in the bath or in bed at night.
Over the next few weeks it is a good idea to make a note of your baby’s activity pattern. Do they kick more in the morning or evening? Do they have spells when they make a lot of movements? This will help you determine if there is a change in your baby’s regular pattern of movement. You won’t necessarily feel these kicks every day at this stage: it doesn’t mean your baby isn’t moving lots inside because it definitely will be, it’s just that the movements are so small and subtle. As your baby grows and gets stronger the movements will feel stronger; much more like proper kicks rather than flutters or pops. And remember to try not to compare yourself with your pregnant friends – like I said, everyone is different and that includes your baby.

Make sure you attend a class that is suitable for pregnancy.
1 Your baby uses your pelvic floor as a trampoline for a good few months, so you need it to be in top working order. All Pilates exercises focus on pelvic-floor awareness and strength.
2 You’ll also need to be able to release your pelvic floor to allow your baby to exit. Pregnancy Pilates teaches you to fully relax ‘down there’, being mindful of your body and its tensions.
3 Your abdominals stretch as your bump grows, and in most pregnancies they actually split down the middle; this is called diastasis recti. Pilates builds an extra corset of strength to support your back and bump, and to ensure they zip back up once your baby is no longer in your belly.
4 Pilates corrects your posture. Do you slump in your seat? Pilates irons you out to ensure you cope well with the added load of your growing baby.
5 Breath influences and indicates our state of mind and well-being. Pilates encourages you to breathe fully and deeply, which aids relaxation, and is also an effective tool during labour.
6 Pilates is perfect for relieving tension and anxiety. By connecting to your body and achieving balance, you can also release your mind.
7 You can practise Pilates during labour: Pilates squats allow the pelvis to widen to help your baby descend. Regular practice means during labour you’ll be able to enter a familiar physical state and get into a ‘zone’.
8 You’ll tone the bits of your body that don’t have as good an excuse to balloon – your arms, thighs, bum …
9 It’s a safe way to stretch and move your body through all trimesters.
10 Pilates limits the challenges that pregnancy places on your body, and gives you some space to become more in tune with your body.
Pregnancy and yoga are highly compatible because yoga is a tool to explore the depths of our human nature and there is nothing more natural than having a baby. In pregnancy, a woman’s senses are heightened: she can smell more vividly and is more sensitive to taste and to emotional states. This is because she becomes more intuitive. Practising yoga will help tune into those intuitions to positively experience the transformation into motherhood. The breathing techniques, gentle movement exercises, meditation and relaxation methods provide practical tools to support a woman on her journey through pregnancy, labour, post-natal recovery and well into motherhood. Benefits include:
1 Keeps the body supple without strain and helps maintain balance as your centre of gravity changes.
2 Builds strength and stamina while maintaining joint stability.
3 Brings awareness to, and enhances, the tone of the pelvic floor for labour and better post-natal recovery.
4 Relieves common minor ailments during pregnancy, e.g. swollen joints – fat ankles, heartburn, constipation, hip and lower back pain.
5 Prevents stretch marks by increasing the elasticity of the skin.
6 Boosts energy and combats exhaustion.
7 Grounding and centring practice relieves anxiety and calms emotional turbulence, promoting relaxation and restful sleep.
8 Breath awareness and control along with visual techniques help manage contractions during labour.
9 Lots of all-four poses – said to help with optimal fetal positioning.
10 Cultivates core strength safely, to help close abdominal diastasis postnatally.
In the majority of women, the 20-week scan, which is also known as the ‘anomaly scan’, would be the second time they would see their baby, the first scan being around 12 weeks. The anomaly scan is offered in most units between weeks 18 and 20 of pregnancy, although some units may offer it a bit later, up to 23 weeks. This later scan is offered in units where there are extra screening tests available as a part of research for predicting risk of developing high blood pressure or having a small baby in that pregnancy. The anomaly scan is offered to all pregnant women, and there should be written information about it provided by the midwife earlier in pregnancy.
The main purpose of the anomaly scan is to check that the baby is developing normally, rather than checking the gender of the baby. The gender, however, may be disclosed following the scan, upon request, although some hospitals have a policy of not telling parents-to-be. The person carrying out the scan is usually a sonographer who is trained in providing this service to the specific standards that are expected of this scan by the NHS Fetal Anomaly Screening Programme (FASP). It is, however, important that each woman attending the scan has realistic expectations of the process and its outcomes.
During the scan, various parts of the baby’s body are checked to look for any abnormality, ‘defects’ or ‘malformations’. The sonographer looks at the shape and structure of the baby’s head to check for brain or skull defects; the face, to check for a cleft lip and sometimes a cleft palate, which is usually hard to see and often not picked up; the baby’s spine, to make sure that all the bones align, and that the skin covers the spine at the back, which will help indicate whether a condition called spina bifida is present. In addition, a detailed assessment of the baby’s heart is carried out as per the guidance laid out by the Fetal Anomaly Screening Programme. The baby’s abdominal wall (future belly button) is checked to ensure it covers all the internal organs. The baby’s kidneys, bladder, stomach, swallowing and movements are checked. The sonographer will look at the baby’s fingers and toes, but not count them. The baby is then measured, based on the head, tummy (at the level of the waist) and thigh bone to get an estimated weight. This, however, does not reflect the weight of the baby at birth. To ensure that the baby is growing normally, regular visits to the midwife are recommended and an additional scan in late pregnancy is offered if there are any concerns. It is not possible to measure the length of the baby on this scan. The anomaly scan also checks the position of the placenta, and if the placenta is lying low in the womb (uterus), an additional scan is offered late in the pregnancy. The anomaly scan does not usually offer 3D/4D pictures of the baby.
Sometimes, despite best efforts, the scan cannot be completed at the first appointment. Factors limiting the quality of the scan may be the position of the fetus, presence of extra tummy fat, bloating, scar tissue or fibroids, or increased or decreased water around the baby. In such cases, an additional scan is offered around 23 weeks. If there is an ‘anomaly’ detected on the scan, the sonographer will arrange a referral for a specialist fetal medicine scan within three to five working days.
As far as we know, the baby is unaware that the scan is taking place and this scan is not thought to be harmful to the mother or the baby. The anomaly scan is usually a pleasant experience and also serves as a bonding exercise for the expectant mother and the family. Exclamations voiced during scanning such as ‘it’s a baby’ or ‘it’s surreal’ – are not uncommon.
I lay on the bed, pulled my waistband down, tucked some tissue in and the sonographer applied the gel to my tummy – whoever invented the gel- warmer is one of my favourite people in the world! Our sonographer was extremely calm, warm and professional, which helped me to relax. The first thing she said was, ‘There’s baby – with an excellent strong heartbeat,’ which was hugely reassuring. She started the check-up with the brain and was very methodical, explaining exactly what she was looking at, measuring and why, and letting us know that things were fine before moving on.
It’s completely amazing, being taken on a guided tour of this little person you’ve yet to meet, although my mind wandered sometimes – when the image on the screen just looked like a photocopier malfunction to the untrained eye. In those moments, especially when it seemed that all was well, I tried to decide whether or not to find out the sex – we still hadn’t decided – finally picturing the birth and determining that I’d leave it a surprise.
There were also fantastic moments, like when the sonographer pointed out that the baby was yawning or turning to look at us, having a little wriggle and putting its hands up to its head in an uncanny recreation of its big sister’s favourite sleeping position.
I did stress out a little bit when the sonographer said the baby’s legs and feet were too curled up to assess the development and suggested we went for a walk to help it change position, saying she’d check the blood flow of the heart when we got back. She also said she wanted me to have a wee so she could have another look at the placenta after I’d emptied my bladder. Despite convincing myself that all this must mean there was a problem with the heart, legs, feet, placenta, or all of the above, the baby moved and it was absolutely fine. The sonographer also showed me my bladder, birth canal, and the location of the placenta, which is posterior, to the back of the uterus, unlike in my first pregnancy, when it was anterior, to the front, meaning I didn’t feel much kicking. I’ve felt kicks for a few weeks already with this one, so I wasn’t surprised – I even saw my stomach moving when I went to bed that night! She also checked it wasn’t too low. She also spotted, accurately located and measured a small fibroid I’ve had for a while. This fibroid may or may not prevent me from giving birth in the hospital’s birth centre, although they are currently reviewing their policy and there is an appeals system at 36 weeks for women who would like to use this facility but have, for whatever reason, been advised to have a hospital delivery.
Towards the end, I told the sonographer I didn’t want to know the sex and she assured me that even she didn’t know because, as we hadn’t requested it, she wouldn’t look.
Once she’d finished, she asked if I’d be willing for her to check the blood flow to the uterus, which is a new test the hospital is shortly bringing in for women with high blood pressure and suspected pre-eclampsia – not that I have it. I did briefly have high blood pressure towards the end of my first pregnancy, though, so I was more than happy to take part. We got to hear the roar of the blood flow on both sides of the uterus and see it represented on a graph on the screen. I asked if this was anything to do with the placenta noise that midwives pick up on their portable Doppler scanners but it’s different – although apparently it sounds very similar.
By this point, I was having a whale of a time and babbling with relief! The chance to glimpse the secret world your baby inhabits for 40 weeks or so is such a terrific privilege, and I was even pretty fascinated to see my own bladder on TV! I do wish I could have been more relaxed and enjoyed the experience more but I think it’s normal to be nervous. It is a serious check-up that can potentially save lives, so it’s not something to be taken lightly.
Having said that, for those of us who are fortunate enough to leave clutching a batch of pictures at £3 a pop knowing everything is well, the 20-week scan is a pregnancy highlight. I’ve also noticed that a lot of people are waiting till this point to widely announce their pregnancy. I doubt I’ll relax completely, but I now feel I can heave a big sigh of relief, break out the maternity clobber and get on with being properly pregnant.
• My liver had never had such a good detox. It must have given a huge sigh of relief that it didn’t have to filter out any alcohol for almost nine months.
• And that means no hangovers. It’s strangely pleasurable watching your partner suffer the day after your best friend’s wedding while you joyfully skip around the kitchen offering to make bacon sarnies like the perfect wife.
• Seat on the train/tube – once my bump started to show I wore that ‘Baby on Board’ badge with pride.
• Excuse to buy new clothes – finding great maternity clothes on a regular basis is a great way to convince your partner you need new threads.
• (For some people) bigger boobs – it’s like a free boob job on the NHS.
• An excuse to spoil yourself: if you feel like lying around in your bath robe all day, then do it!
• More melatonin in your skin means you hold on to your tan longer – I had the brownest tummy during my pregnancy.
• No periods – literally the best!
• Higher sex drive – my husband didn’t know what had got into me.
• Having the best excuse not to go to stuff you really don’t want to – no one will argue with the ‘my back is killing and I can’t stand in heels for longer than 20 minutes’ reason you don’t want to go to that guy from finance’s leaving drinks.
• Shinier, thicker hair – you don’t necessarily grow thicker hair but you lose less, which means far fewer bad-hair days. And stronger fingernails!
• Better skin – if you’re one of the lucky ones. I hardly got any of those horrible teenage-spot outbreaks throughout my pregnancy and wore much less make-up than usual because my skin didn’t look so tired.
• Not worrying about trying to hold your tummy in. Finally a reason to wear tight-fitting clothing; show that bump off like you mean it! Pregnancy is something to be celebrated, so be proud of your changing shape. It may take some getting used to but once you’ve nailed your pregnancy wardrobe you’ll feel a million times better about yourself (see Zoe: Dress like a mum, here).
• And finally, just feeling a bit special. I know women have been doing this since before history began but it’s an incredible time in your life, even if it’s your second, third or fourth pregnancy. Growing new life is amazing, so remember to embrace this magical time.