CHAPTER 15
Oral Soft Tissue Lesions and Minor Oral Surgery
Göran Koch and Dorte Haubek
Children and adolescents present a large variety of oral pathologic conditions, such as lesions of the oral mucosa, bone lesions, cysts, and tumors or tumor‐like lesions. Knowledge on pathologic changes of oral tissues is a prerequisite for providing correct diagnosis and adequate treatment. The present chapter deals with the most common pathologic conditions or changes of the oral mucosa in children and adolescents.
Oral surgery in children and adolescents is, with few exceptions, similar to oral surgery in adults. However, there are some specific and common surgical procedures which, due to the special condition of a growing individual, are different to procedures performed in adults. The most common of such surgical procedures will be presented in this chapter. For more extensive knowledge on oral pathology and more detailed information on pediatric oral surgery, the reader is referred to textbooks listed in section “Background literature.”
Oral mucous lesions
Apart from specific skin lesions, a number of common infectious diseases in children are also manifested as oral lesions. For example, bacteria, viruses and fungi may cause infections of the oral mucosa. During the child’s disease and the week after recovery, unnecessary dental treatment should be avoided due to potential risk of contamination.
Bacterial infections
Impetigo contagiosa
This lesion is more common in children than adults. It is caused by streptococci and staphylococci and often affects the perioral area. The infection causes inflammatory vesiculo‐bullous lesions that rupture, leaving secreting or crust‐covered lesions (Figure 15.1). The lesions will cause only a low sensation of pain. As the disease is contagious, it can be spread within the family and between playmates. In the acute stage, dental treatment should be avoided. In most cases, the lesions heal without complication after strict hygiene measures, but intake of antibiotics are often recommended.

Figure 15.1 Impetigo contagiosa in a 7‐year‐old girl.
Scarlet fever
Scarlet fever is a common disease in childhood caused by beta‐hemolytic streptococci. The general symptoms are fever, tonsillitis and lymphadenitis. A papular red skin rash will develop within a few days. Besides swollen tonsils, the most characteristic oral manifestation is the gradual change of the appearance of the tongue from a “strawberry” to a “raspberry” tongue. In the initial stage of the infection the white‐coated tongue shows a scattered pattern of hyperemic fungiform papillae. Later, this coating is lost and the red edematous fungiform papillae dominate the clinical picture.
Viral infections
A number of viruses may cause infections of the oral mucosa in children. In recent years, many vaccination programs have, however, been introduced. One of these is measles, mumps and rubella (MMR) vaccine which is an immunization vaccine against measles, mumps and rubella. In some types of MMR vaccines, the protection against varicella is included (MMRV). In countries with a well‐established vaccination program, many children do not get these diseases anymore. However, brief descriptions of some of these diseases, mainly manifesting in childhood, are given below.
Rubella
Rubella is a virus infection characterized by light red macules on the skin. Occasionally, macules are also found on the soft palate, called Forschheimer’s spots (Figure 15.2).

Figure 15.2 Forschheimer’s spots on the soft palate in a child with rubella.
Measles
Measles is a viral disease. After an incubation time of 10–12 days, the child will have a cough, fever and photophobia. Some days later, light red maculopapular lesions develop all over the skin. The oral manifestations, Koplik’s spots, occur on the buccal mucosa as prodromal grayish‐white macules surrounded by a slightly erythematous zone some days before eruption of the skin lesions (Figure 15.3).

Figure 15.3 Koplik’s spots in the cheek mucosa in a child with measles.
Mumps
Mumps is a viral infection affecting the salivary glands. The general symptoms are fever and pain from the infected glands. In cases where the parotitis is unilateral, difficulties in distinguishing the condition from a swelling of odontogenic origin may arise.
Varicella (chickenpox)
Varicella is a viral disease mostly seen in children. The general symptoms are fever, pharyngitis and vesicular lesions on the skin, beginning on the trunk and then spreading all over the skin (Figure 15.4). The lesions have varying degrees of development. The oral manifestations are whitish vesicles surrounded by a red halo found mostly on the mucosa of the lips, bucca and tongue (Figure 15.5).

Figure 15.4 Vesicular lesions on the skin in a child with varicella (chickenpox).

Figure 15.5 Vesicles on the mucosa of the tongue in a child with varicella.
Herpetic gingivostomatitis
Herpetic gingivostomatitis is caused by herpes simplex virus (HSV) and communicated through personal contact, e.g., transmission via the saliva of the mother. Primary oral infection occurs following the first exposure to the virus. Studies have found antibodies to HSV in 40–90% of individuals in different populations showing that HSV infection affects almost all individuals even if many of them only suffer the infection subclinically. The incidence of primary herpes simplex infection increases from the age of 6 months. It reaches its peak at age 2–5 years. Below 6 months of age, the child is usually protected by maternal antibodies. The primary herpes simplex infection is therefore mainly a disease in children. The incubation period is 3–5 days. The primary infection is often manifested as an acute herpetic gingivostomatitis where the entire gingiva is red, edematous and inflamed. The general symptoms are fever, headache, malaise and pain. After 1–2 days, small vesicles develop on the oral mucosa. Subsequently, they rupture, leaving painful ulcers with a diameter of 1–3 mm (Figure 15.6).

Figure 15.6 (a) Herpes simplex lesions spread over the alveolar mucosa and (b) tongue.
Normally, the primary herpes simplex infection is self‐limiting. The child will recover within a 10‐day period. Treatment is primarily supportive, e.g., painkillers for the pain and fever, fluid to maintain sufficient hydration and, if necessary, topical anesthetic ointments to facilitate eating. In severe cases, hospitalization and/or the use of antiviral agents are necessary.
It has been shown that recurrent herpes simplex infection originates from a reactivation of HSV, which remains dormant in nerve tissue between periods of excitation. Reactivation may be caused by injuries to the mucosa caused by sunlight, citrus fruits or dental treatment, etc. Recurrent herpetic infection will develop at the same location at every excitation, e.g., herpes labialis (Figure 15.7). Topical treatment with ointments containing acyclovir, available on the market, might minimize the symptoms.

Figure 15.7 Herpes labialis.
Verruca vulgaris
Intraoral warts may present as solitary or multiple lesions and are caused by human papillomavirus. They can be associated with skin warts, and precautions to minimize risk of contamination should be considered (Figure 15.8).

Figure 15.8 Wart.
Fungal infections
Fungal infection may cause mucosal pathology in children and adolescents.
Oral candidiasis
Oral candidiasis is caused by the fungus Candida albicans, which is normally found in the oral cavity. The fungus invades the mucosa only when there is a change in the oral environment or a general impairment of the immunologic or hormonal balance. Such changes can be brought about by the administration of antibiotics and immunosuppressive drugs. The clinical manifestations in the oral mucosa can vary. Pseudomembranous candidiasis (thrush) is the most common fungal infection in newborn children and in children with chronic disease. It is characterized by raised, pearly‐white patches (Figure 15.9) that can be rubbed off, leaving an erythematous or bleeding mucosa. The clinical manifestations can vary from acute to chronic forms. In some patients, a hypertrophic variant can be found (Figure 15.10). The treatment is medication with antifungal preparations, such as nystatin, amphotericin B or miconazole. Systemic administration or topical application by mouthrinses, sucking lozenges and gels containing these preparations will be effective in most cases.

Figure 15.9 Candidiasis lesion in cheek mucosa.
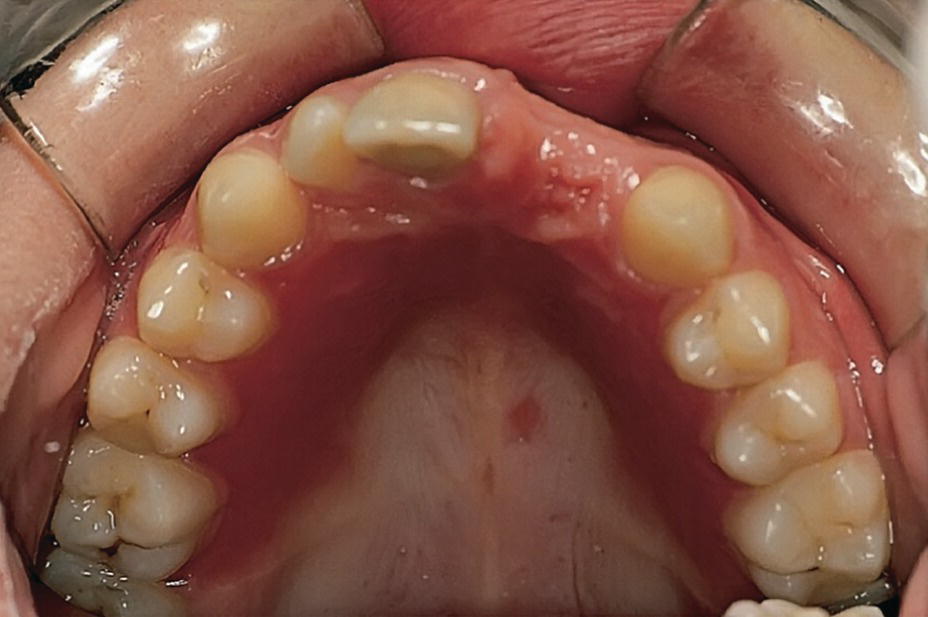
Figure 15.10 Candida albicans infection of the palatal mucosa in child with a partial denture.
Immunologically‐related and other mucous lesions
Aphthous ulcers
Recurrent aphthous ulcerations (RAU) or recurrent aphthous stomatitis (RAS) are the most common oral ulcerations seen in children. Studies indicate a prevalence of about 35% in adolescents. An altered immune defense system has been suggested as the main predisposing factor. This is confirmed by the frequent aphthous ulcers seen in children on immunosuppressive drugs and by the familiar occurrence. As a trigger factor, infection with specific oral streptococci has been suggested.
The lesions are most frequently localized to the non‐masticatory mucosa, e.g., the vestibulum and the tongue. The lesion starts as a small white papule which gradually ulcerates. The ulcers are 0.2–1 cm in diameter with the central part covered with a yellowish–gray coating, and a crateriform base with raised reddened margins. The surrounding tissue shows a light swelling. The ulcers are extremely painful and may be of varying size and number (Figure 15.11). The ulcers heal without scars in 1–2 weeks. The intervals between recurrent episodes may vary from a week to several months.

Figure 15.11 Aphthous ulcer.
Other than reassurance, treatment is often unnecessary, as the lesions usually heal within 10–14 days. However, a variety of treatment modalities has been suggested to be used in the most severe cases. In general, the treatment has followed one or more of the following approaches:
- treatment of the oral microbiota (chlorhexidine, hydrogen peroxide‐producing enzyme solutions)
- increasing the immune system (e.g., intake of Longo‐vital®)
- symptomatic treatment of pain (etching solutions, topical anesthetics).
Erythema multiforme
Erythema multiforme is a dermatologic disease, which may also develop oral lesions or in which the oral lesions are the only symptom of the disease. Erythema is not regarded as a specific disease, but as a general reaction to a series of independent precipitating factors, such as food or drug allergy, infection, radiotherapy or general disease. The onset is very rapid. In 24 hours, a child may develop extensive lesions of the skin and/or mucosa. The skin lesions are asymptomatic erythematous macules or papules, mostly affecting hands and feet. In the generalized vesiculo‐bullous erythema multiforme even the eyes and genitals are involved (Stevens‐Johnson syndrome). Initially, the oral lesion has the character of vesicles or bullae, which rapidly burst, forming ulcers (Figure 15.12a). Compared with viral lesions the ulcers are larger, deeper, and often bleed. Involvement of the lips is most common. After some days, the ulcers will crust and healing takes place within 2 weeks (Figure 15.12b,c).

Figure 15.12 Erythema multiforme: (a) oral lesions showing vesicles and bullae which rapidly burst; (b) lesions after 2–3 days; (c) crust formation (healing) 2 days later.
In cases where the lips are severely affected the patient has great difficulties in eating and drinking. In mild cases, topical anesthetics may be the only treatment. In severe cases, systemic treatment with corticosteroids and antibiotics can be justified.
The diagnosis is based on the overall clinical assessment and examination.
Traumatic lesions
Traumatic irritation of the oral mucosa is occasionally seen in children. The most common situation is cheek, lip or tongue bites occurring accidentally or due to decreased sensation of the oral tissues usually after dental local anesthesia (Figure 15.13). The clinical appearance is considerable swelling and bleeding followed by the development of a large, whitish pseudomembranous mucous lesion. The lesion is self‐limiting and will heal in about a week.

Figure 15.13 Tongue mutilation after local anesthesia.
Self‐mutilation, also called self‐harm or self‐injury, of the mucosa is most commonly seen in children with disabilities, for example, having uncontrolled tongue movements (see Chapter 24). The irritation of the mucosa is caused by the child forcing the tongue out of the mouth and thereby injuring it on the mandibular incisors. Hyperkeratotic wounds may develop. Smoothing of the incisal edges of the incisors or an acrylic splint in the mandible may help to heal the lesion. Other types of self‐harm may also include biting, hitting, or bruising oneself, or picking or pulling the oral mucosal and/or tissues. Self‐mutilation can be episodic or repetitive.
Crohn’s disease
Crohn’s disease is commonly associated with oral lesions. The lesions may also precede symptoms of bowel disease. The most common oral pathologic findings in Crohn’s disease are aphthous ulcers, areas of inflammatory hyperplasia, including mucosal fissuring and indurated “tag‐like” lesions on the retromolar area (Figure 15.14). The lesions tend to run a remitting course.

Figure 15.14 Crohn’s disease, gingival characteristics: (a) incisal region; (b) molar region.
Geographic tongue
Geographic tongue is a benign migratory glossitis occurring in children. Clinical manifestation is pinkish red, irregularly depapillated areas surrounded by a well‐defined, slightly raised whitish border. Affected areas vary from day to day, and the appearance can be described as a continuously changing map (Figure 15.15). Occasionally, other parts of the oral mucosa are affected (stomatitis migrans). A hereditary tendency is seen, but the etiology is unknown. It is normally symptomless, but some children will experience discomfort and burning sensation from the lesions, especially when eating, e.g., spicy food. In severe cases, topical anesthetics are recommended during the acute phase.

Figure 15.15 Geographic tongue is a relatively common condition found in children.
Cysts, tumors, and tumor‐like lesions
Oral cysts are often described as a cavity in the oral tissues containing fluid or gas and frequently lined with epithelium. Some of the most well‐known and frequently occurring cysts are listed in Box 15.1.
Tumor and tumor‐like lesions of the head and neck are recognized even in very young children. Fortunately, most of these lesions are benign and the frequency of malignant neoplasms is very low. However, about 25% of all malignant neoplasms in children develop in the head and neck area. Many of the tumors in the oral region are to be regarded as hamartomas, i.e., a benign, focal malformation that resembles a neoplasm in the tissue of its origin. Due to the disproportionality of the tissues in hamartomas, they can expand to the surrounding tissues. Normally, growth stops when it has reached a certain stage. Hemangioma and lymphangioma are examples of hamartomas. A list of tumors which can be found in the oral structures in children is presented in Box 15.2.
It is important that tumors and tumor‐like lesions in the oral region are properly diagnosed and handled. If a lesion looks suspicious and the diagnosis is uncertain, the child should be referred to a specialist in pathology.
Some oral cysts and tumors manifesting in children and adolescents with considerable frequency will be presented briefly. For more comprehensive information about cysts and tumors, the reader is referred to textbooks on oral pathology.
Bohn’s nodules
Bohn’s nodules (gingival cysts of the newborn) occur with high frequency up to the age of 3 months. The cystic formulations develop from epithelial remnants from the dental lamina and often appear in groups of four to six, situated on the buccal and lingual area of the dental ridge (Figure 15.16). The nodules, which can be misinterpreted as early erupting primary teeth, need no special treatment as they will disintegrate spontaneously.

Figure 15.16 Bohn’s nodules in a newborn baby.
Epstein’s pearls
In the majority of neonate children, small cystic lesions may be seen along the palatal midline and are thought to be trapped epithelium along the palatinal raphe. The Epstein’s pearls usually disappear shortly after birth.
Eruption cysts
Eruption cysts may be defined as dentigerous cysts located in the soft tissues. If there is bleeding in the cyst, it is classified as en eruption hematoma. The cyst can occur in very young children, but is more commonly found in connection with tooth eruption. Usually, there is a small, smooth swelling in the gingival tissues at the site of the erupting tooth. If treatment is indicated, marsupialization is the treatment of choice. The tooth will then erupt rapidly.
Mucous retention cysts (mucocele and ranula)
Mucocele occurs frequently in children, mostly in the lower lip. It is caused by a trauma of the lip, resulting in an obstruction of the excretory duct of one of the numerous glands in the lip. It may lead to formation of an epithelium‐lined mucous retention cyst. The clinical picture is often a smooth, painless, rounded swelling in the lip mucosa. The treatment is removal of the cyst and associated salivary gland (Figure 15.17). Marsupialization may lead to recurrences.
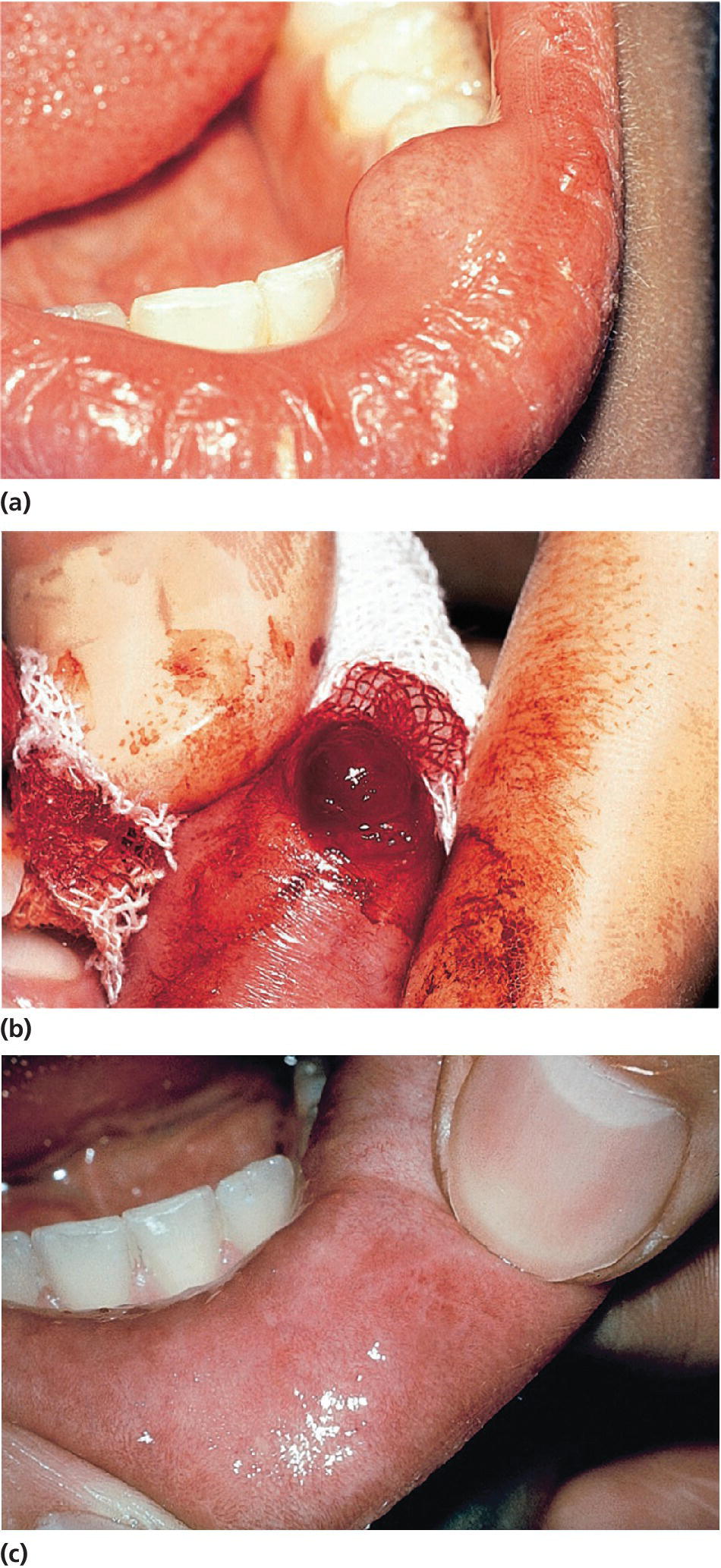
Figure 15.17 (a) Mucous retention cyst in the lower lip. (b) Surgical removal of the cyst. (c) Healing after 1 week.
Ranula is essentially a large mucocele, located as a bluish swelling of the floor of the mouth (Figure 15.18). It arises from the salivary glands in that region. Due to extravasation or retention of mucus from excretory ducts of sublingual glands caused by trauma or infection, the extensive translucent swelling may occur.

Figure 15.18 Ranula located in the floor of the mouth.
Epulides
Epulides are by definition tumor‐like hypertrophic tissue formations located on the gingival mucosa. The etiology is often trauma or irritation in connection with tooth eruption or exfoliation. The size may vary from some millimeters up to several centimeters in diameter. They differ in surface texture, consistence and color, depending on the tissue composition. Pyogenic granuloma, peripheral calcifying granuloma, and peripheral giant cell granuloma (Figures 15.19, 15.20 and 15.21) are all examples of epulides. The treatment is excision, and the final diagnosis is confirmed by histopathologic analysis.

Figure 15.19 Pyogenic granuloma.
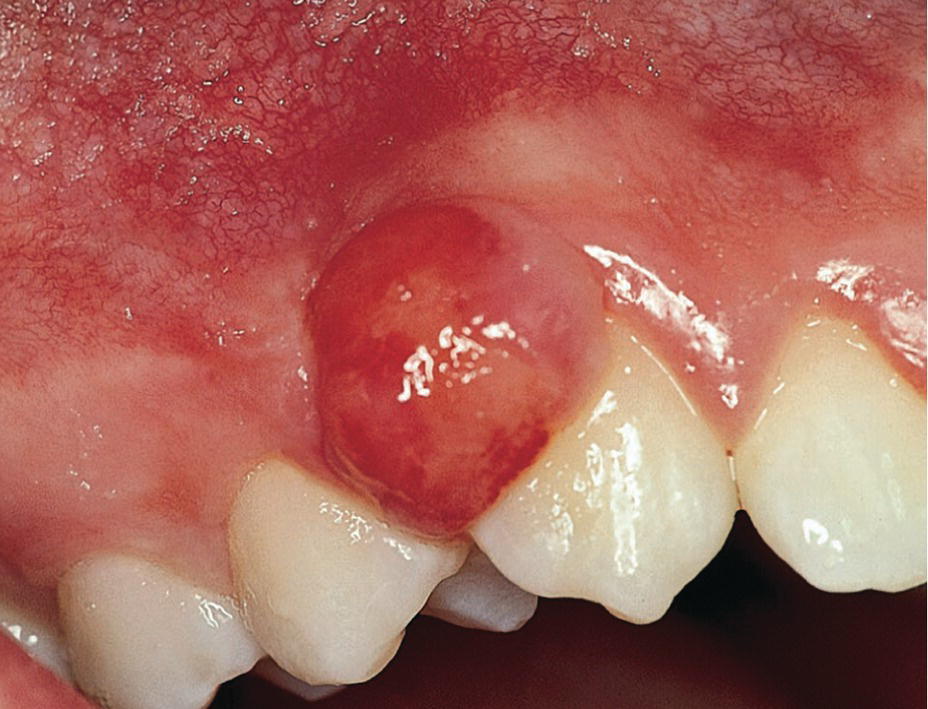
Figure 15.20 Peripheral calcifying granuloma.

Figure 15.21 Peripheral giant cell granuloma.
Hemangioma
Within the group of tumors from soft tissues, hemangioma is a relatively common hamartomatous tumor in children (Box 15.2). Most of the lesions are present at birth. The most common location is the tongue, followed by the lips and buccal mucosa. Clinically, two different forms can be distinguished: the capillary hemangioma and the cavernous hemangioma. The former consists of a proliferation of tiny capillaries, often manifested as red birthmarks on the skin and oral mucosa (Figure 15.22). The cavernous form is frequently situated more deeply and consists of large cavernous blood‐filled vessels. The tumor often causes a compressible swelling of the tissue affected, and the color is frequently more bluish than the capillary hemangioma (Figure 15.23). Treatment of hemangioma is always complicated because of the risk of uncontrolled bleeding. Fortunately, congenital hemangioma in the mucosa most frequently undergoes spontaneous regression.

Figure 15.22 Capillary hemangioma.

Figure 15.23 Cavernous hemangioma in the palate of a newborn. Note also the capillary hemangioma in the cheek.
Pediatric oral surgical procedures
Extraction of teeth
The indications, contraindications and techniques for extraction of teeth in children and adolescents are somewhat different from those in adults. In the primary dentition more radical treatment may, for many reasons, be applied. Generally, necrotic teeth, ankylosed primary teeth without permanent successors, seriously decayed teeth, especially with advanced root resorption, and primary incisors exposed to severe traumatic injuries should be extracted. The forceps used for extraction of primary teeth are specially designed for the anatomical form and size of these teeth. The risk of root fractures during the extraction procedure is somewhat higher for primary molars than for permanent teeth due to the more slender and curved roots. Therefore, careful loosening of the tooth with a straight elevator is recommended before the forceps are applied. It is important to have a firm grip of the jaw in order to control the movement of the forceps more easily and to apply the working branches of the forceps steadily around the crown and neck of the tooth deep in the gingival pocket. The primary molars are extracted by slightly pressing the tooth down in the socket and slowly moving the tooth in a bucco‐lingual direction to enlarge the socket before the tooth is lifted out. Incisors are extracted by a slight rotation of the tooth (Figure 15.24).



Figure 15.24 Extraction of primary teeth: (a, b) molars in upper jaw and (c, d) lower jaw – loosen the tooth carefully with an elevator, place the forceps around the tooth and apply apical pressure and buccal–lingual movements before the tooth is lifted out. (e–g) Incisors are extracted by slight apical pressure and rotary movement.
In some cases, the roots of the primary molar encircle the permanent tooth bud (Figure 15.25). Before extraction, it is therefore wise to cut the tooth into two halves with a diamond or fissure bur (Figure 15.26) to avoid dislodging or avulsing the permanent successor. If a small root tip fractures, the best treatment is to leave it if it is not infected and does not interfere with the eruption of the succeeding tooth. However, if the fragment is infected or non‐vital, it should be removed by using a sharp elevator or a root reamer screwed into the root canal of the fragment.

Figure 15.25 Primary first molar with pulpitis. Roots of the tooth encircle the permanent tooth bud.

Figure 15.26 Primary molar cut into two halves before extraction.
Denudation of impacted or nonerupting teeth
The surgical treatment of impacted teeth is also discussed in Chapter 5. Impacted primary teeth should generally be surgically removed. Permanent teeth with ectopic eruption position will usually be treated by surgical exposure often in combination with orthodontic treatment to guide the impacted tooth into its proper location. Such treatment is often used in cases with ectopic eruption of maxillary canines when risk for resorption of permanent incisors exists (Figure 15.27). If the eruption path for a tooth for some reason is blocked, the hindrance should be removed, and preferably when the tooth root is two‐thirds formed. In cases of early extraction of primary incisors, a delay in the eruption of the permanent incisor can occur. In such cases, a fenestration of the oral mucosa may have to be made (Figure 15.28). Impacted permanent teeth, for example mesiodens, have to be surgically removed if they interfere with eruption of surrounding teeth, cause abnormal positions of erupted teeth, or develop pathologic conditions in the region.

Figure 15.27 (a) Radiographs of upper right canine in palatinal ectopic position with risk for resorption of the permanent incisors. (b) After a palatinal muco‐periostal flap is raised and bone is removed the canine is exposed. (c) Brackets and gold chain are etched to the lingual surface of the canine. (d) The flap is sutured and the free end of the chain is temporarily fastened to a premolar. The contralateral canine was treated at the same session. The patient is now ready for the orthodontic treatment.


Figure 15.28 (a) Delayed eruption of upper central incisor. (b) Denudation of gingival mucosa to enchance eruption.
Soft tissue over erupting teeth or locally extended overgrowth of oral mucosal tissues
A soft tissue flap (operculum) over a normally erupting tooth can sometimes give rise to irritation. It can be treated by irrigation beneath the flap with saline or 0.2% chlorhexidine solution. Removal of the flap is sometimes indicated. This is easily done with electrosurgery or by conventional surgery. In addition, various types of epulis, a local extended growth on the gingiva, can occur along the free gingival margin. Most often, it is hyperplastic tissue that can be curetted or removed with electrosurgery, especially if it is attached to the gingiva by a small stalk.
Cysts
Cysts in the jaws, and especially large follicle cysts emerging from non‐erupted teeth, may displace teeth under development and disturb their eruption (Figure 15.29a–c). In children, it is important not to remove the cysts surgically as a first step procedure since this might damage a number of teeth and tooth germs. Instead, it is recommended in cases with large cysts that the cyst should be shrunk by use of rinsing with saline through an obturator introduced through the cyst wall (Figure 15.29d). In young individuals, the cyst will rapidly decrease and will be substituted by bone and often the dislocated teeth will spontaneously find their normal positions and eruption pathways.
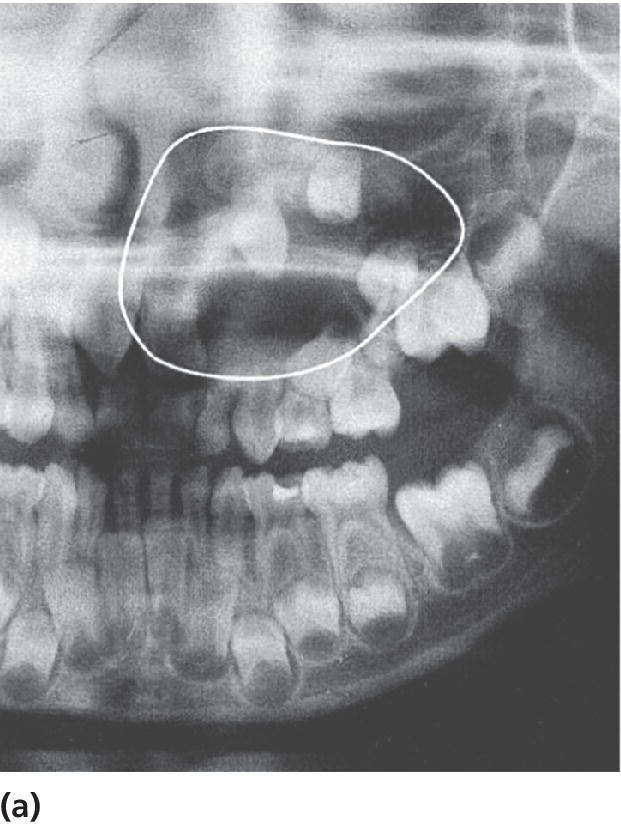
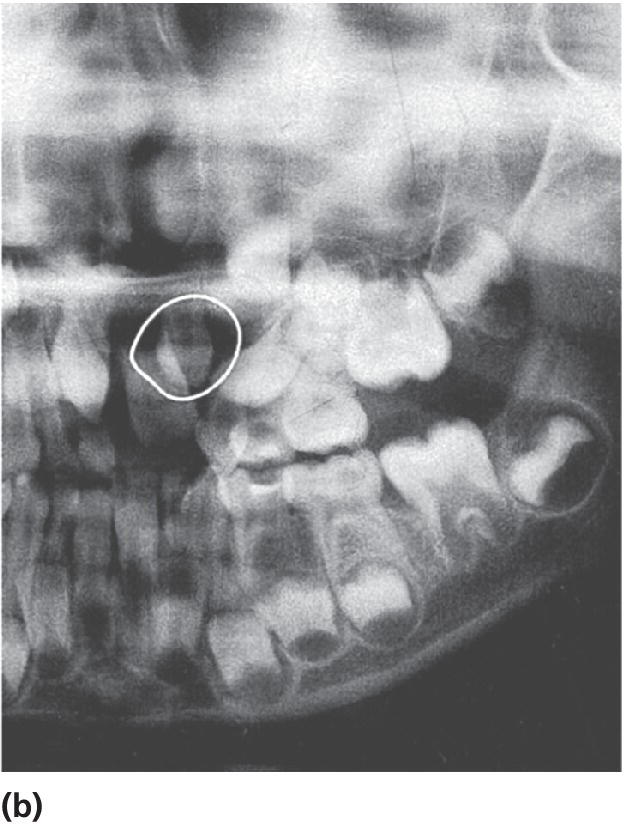
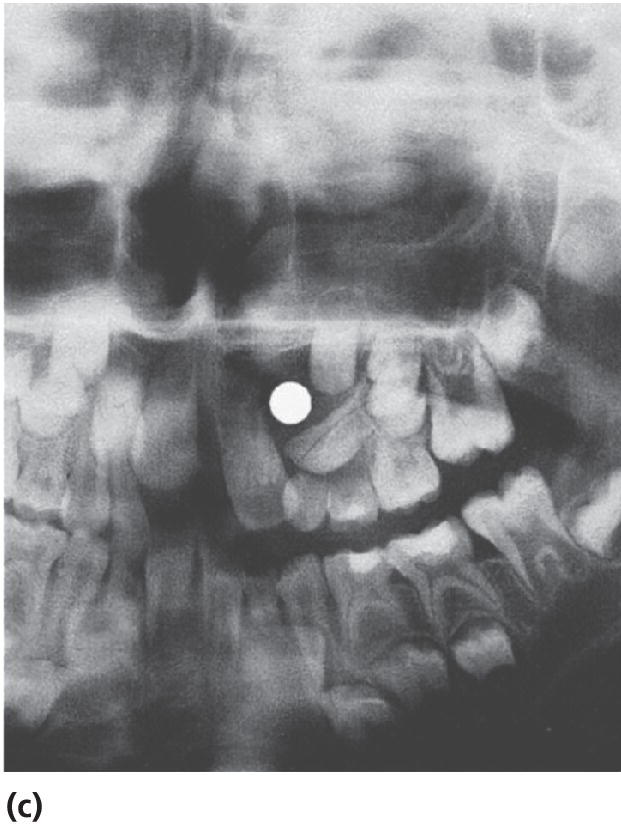

Figure 15.29 (a) Extensive dentigerous (follicular) cyst in left maxilla emerging from a supernumerary tooth and displacing tooth germs and disturbing normal eruption in a 5‐year‐old girl. (b) Radiographic examination after 5 months revealed that the cyst had been reduced considerably and was now available for surgical removal without risk of disturbing the involved teeth. (c) After 4 months and surgical removal of supernumerary teeth and residual cyst tissues. (d) Obturator inserted to facilitate rinsing of the cyst. The obturator was removed after 6 weeks.
Frenuloplasty
Frenulum labii superioris
Occasionally, the frenulum labii superioris has a broad attachment to the upper lip with a thick fibrous string attaching the frenulum to the papilla between the incisors. This strong fibrous part of the frenulum can cause “blanching” of the papilla when forward tension is applied to the upper lip. A bony cleft or fissure can often be found between the central incisors in combination with an extensive diastema. In general, no treatment is necessary as most of these “abnormal” frenula and the diastema will normalize and disappear at the time of the eruption of the permanent incisors and canines. However, if there is no spontaneous closure of the diastema, surgical intervention is recommended. In cases with very fibrous and extensive frenulum labii superioris, causing deep bony defects between permanent central incisors, the surgical treatment may be performed before the eruption of the permanent central incisors (Figure 15.30).
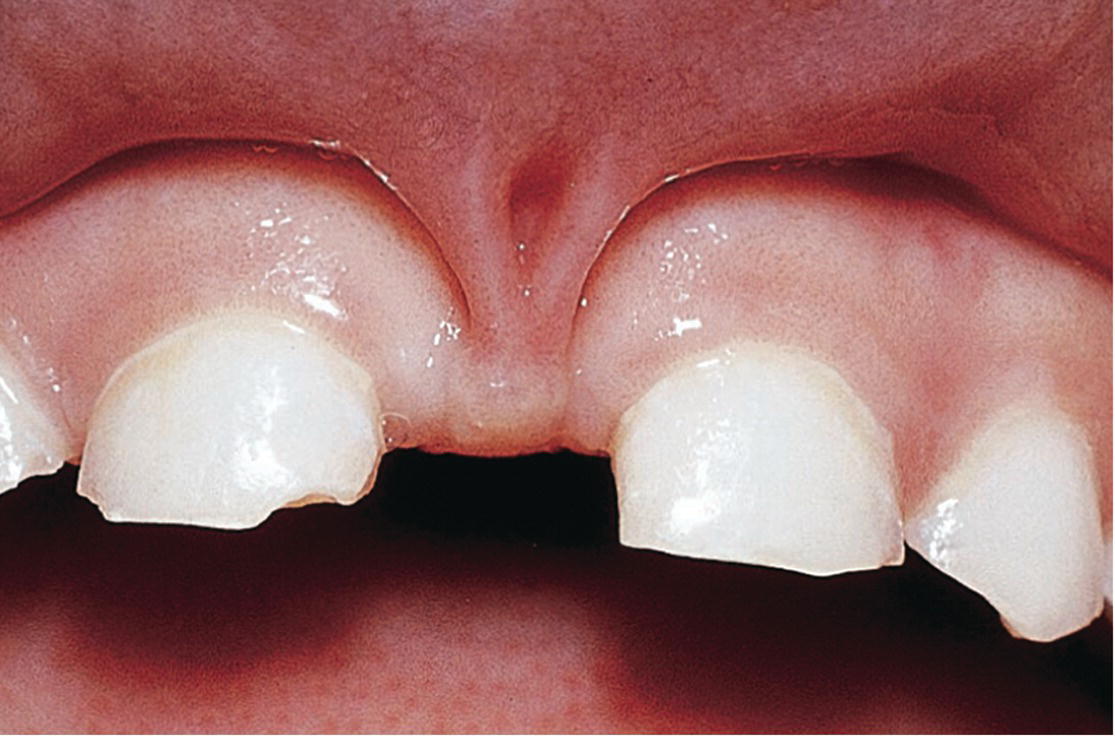
Figure 15.30 Fibrous frenulum causing bony defects in a 5‐year‐old girl.
Frenulum linguae
If a lingual frenulum is frequently traumatized by the mandibular incisors, causes retraction of the lingual gingiva or the mandibular incisors, or interferes with nourishment, speech development, or hygiene procedures it should be cut. It is vital to avoid two structures in this region, being the submandibular duct and the sublingual vein. The dissecting cut is best made lingual to the caruncles, parallel to the undersurface of the tongue, taking care not to go too deep (Figure 15.31).




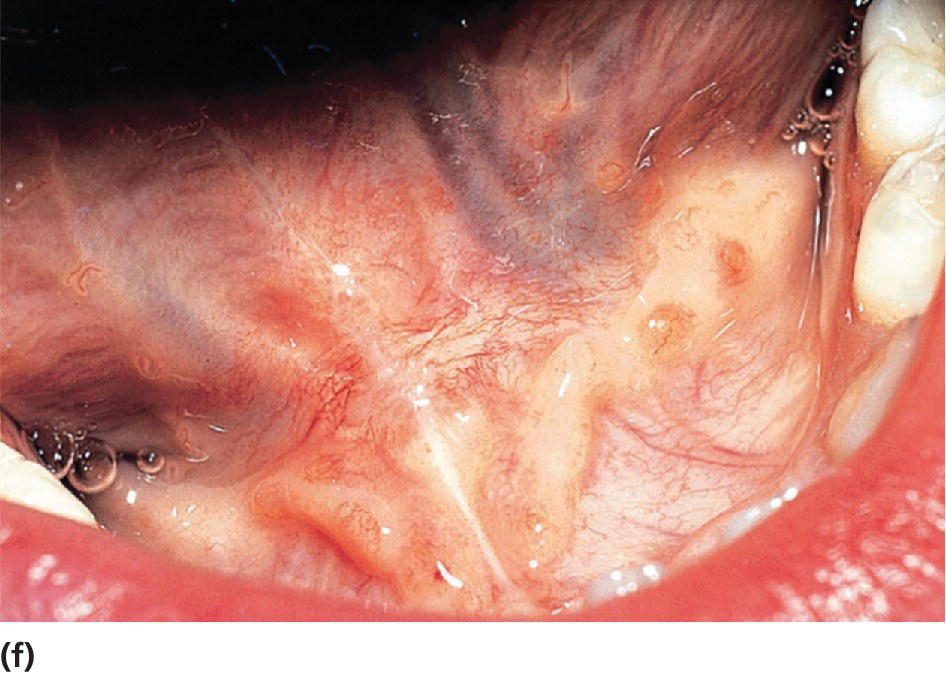
Figure 15.31 Lingual frenuloplasty. (a) Lingual frenulum restricting the movements of the tongue. (b) Local anesthesia. (c) Curved hemostat is placed close to the tongue. (d, e) Frenulum is cut. (f) Healing after 10 days.
Background literature
- Hall RK, eds. Pediatric orofacial medicine and pathology. London: Chapman & Hall, 1994.
- Jones JH, Mason DK, eds. Oral manifestations of systemic disease. London: Baillière Tindall, 1990.
- Kaban LB, Troulis MJ. Pediatric oral and maxillofacial surgery. Elsevier Science USA, 2004.
- Laskaris G. Color atlas of oral diseases in children and adolescents, 3rd edn 2003. Stuttgart‐New York. George Thieme Verlag.
- Pindborg JJ. Atlas of diseases of the oral mucosa. Copenhagen: Munksgaard, 1992.
- Scully C, Welbury R, Flaitz C, de Almeida OP. Color atlas of orofacial health and disease in children and adolescents, 2nd edn 2001. Boca Raton, FL: CRC Press, 2001. ISBN‐1‐84184‐102‐1.