The primary function of the respiratory system is to facilitate gas exchange between the body and external environment and to provide oxygen to the body by working with the cardiovascular system. Oxygen diffuses into the body through the lungs and is disseminated throughout the body by the circulatory system to be used for cellular metabolism. Carbon dioxide, the waste product of cellular metabolism, is returned to the lungs by the circulatory system, and the lungs release it to the environment.
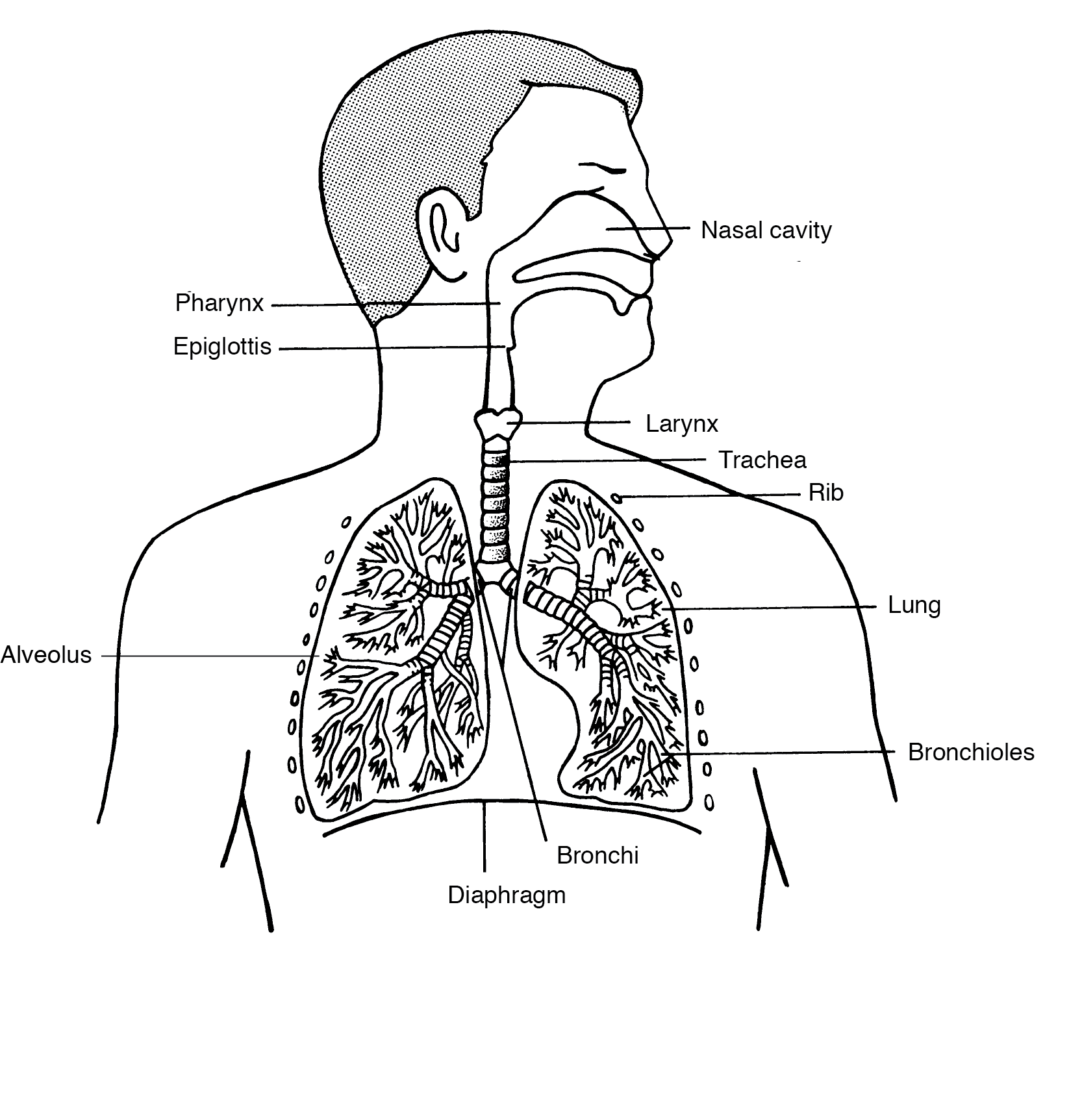
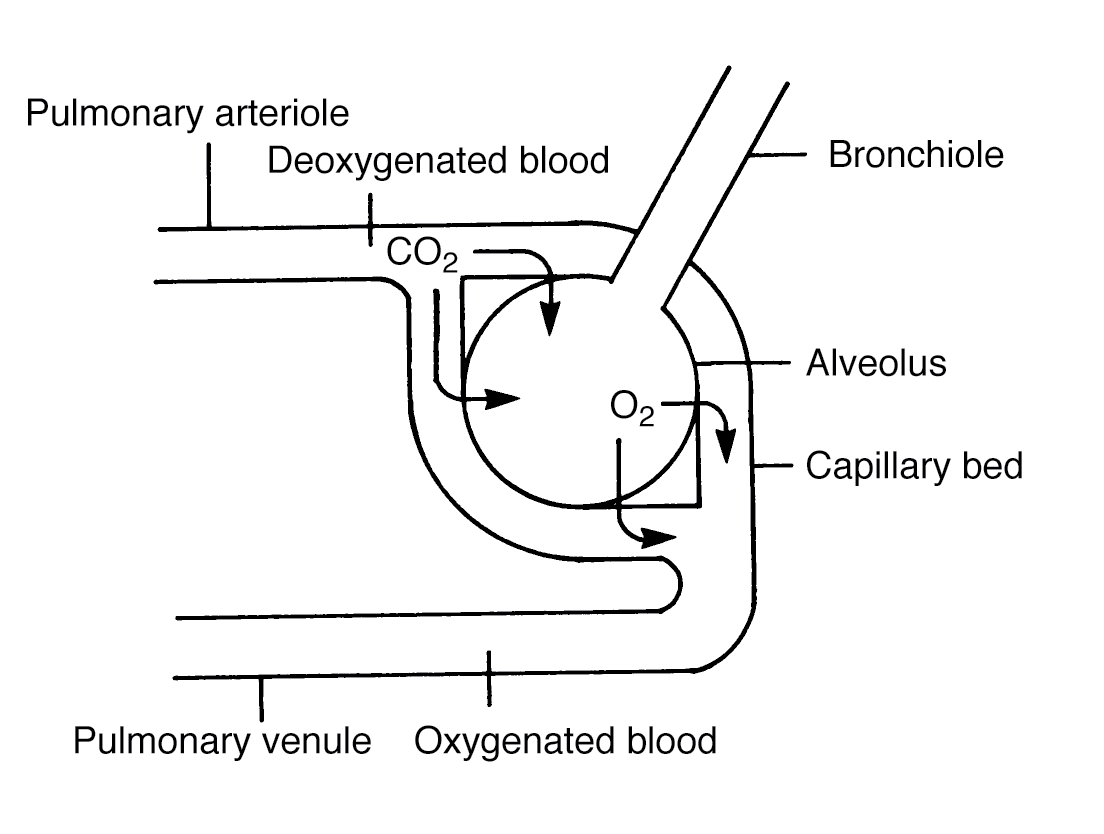
Air first enters the body through the mouth and nasal cavities and passes through the pharynx. A flap of cartilage, the epiglottis, covers the entrance to the pharynx during swallowing, preventing liquids and food from entering the respiratory tract. Traveling past the epiglottis, air then passes through the larynx, also referred to as the voice box, and enters the trachea, or windpipe. The trachea splits into two bronchi (plural of bronchus), which are the main passageways to the left and right lung. As the bronchi move deeper into the lungs, the bronchi split into smaller tubes known as bronchioles, which terminate at the alveoli (plural of alveolus), small sacs only one cell thick. The alveoli are where gas exchange occurs.
This overall pathway of pharynx → larynx → trachea → bronchi → alveoli can be remembered using the mnemonic "please leave the breathing alone."
Cells lining the respiratory tract secrete mucus and other liquids to both keep the lungs moist and trap inhaled pathogens. One such liquid is surfactant, a detergent found bathing the alveoli, which reduces surface tension to prevent lung collapse. Other epithelial cells lining the respiratory tract are covered with short, hairlike cilia, which beat rhythmically to keep mucus and other particles flowing across the interior epithelial surface.
Since the heart is located on the left side of the body, the left lung is slightly smaller than the right lung. The right lung has three segments, or lobes, and the left lung has two lobes. Each lobe is covered by a tough, protective double membrane, each part of which is called a pleura, with pleural fluid between the two pleurae. The lungs are therefore described as residing within the pleural cavity.
Here is how an expert would answer a question on the respiratory system.
| Question | Analysis |
| Which of the following correctly describes the pathway of air into the lungs? | Step 1: This question is asking about the order in which air flows through the parts of the respiratory system. |
| Step 2: Recall the mnemonic for the breathing pathway: please leave the breathing alone. | |
| Step 3: Predict the air travels the path pharynx → larynx → trachea → bronchi → alveoli. | |
| (A) Larynx → pharynx → trachea → bronchi → alveoli | Step 4: The pharynx is before the larynx. Eliminate. |
| (B) Pharynx → larynx → trachea → bronchi → alveoli | Correct. This matches the prediction. |
| (C) Trachea → pharynx → larynx → bronchi → alveoli | The pharynx comes before the trachea. Eliminate. |
| (D) Pharynx → larynx → bronchi → trachea → alveoli | The bronchi come after the trachea. Eliminate. |
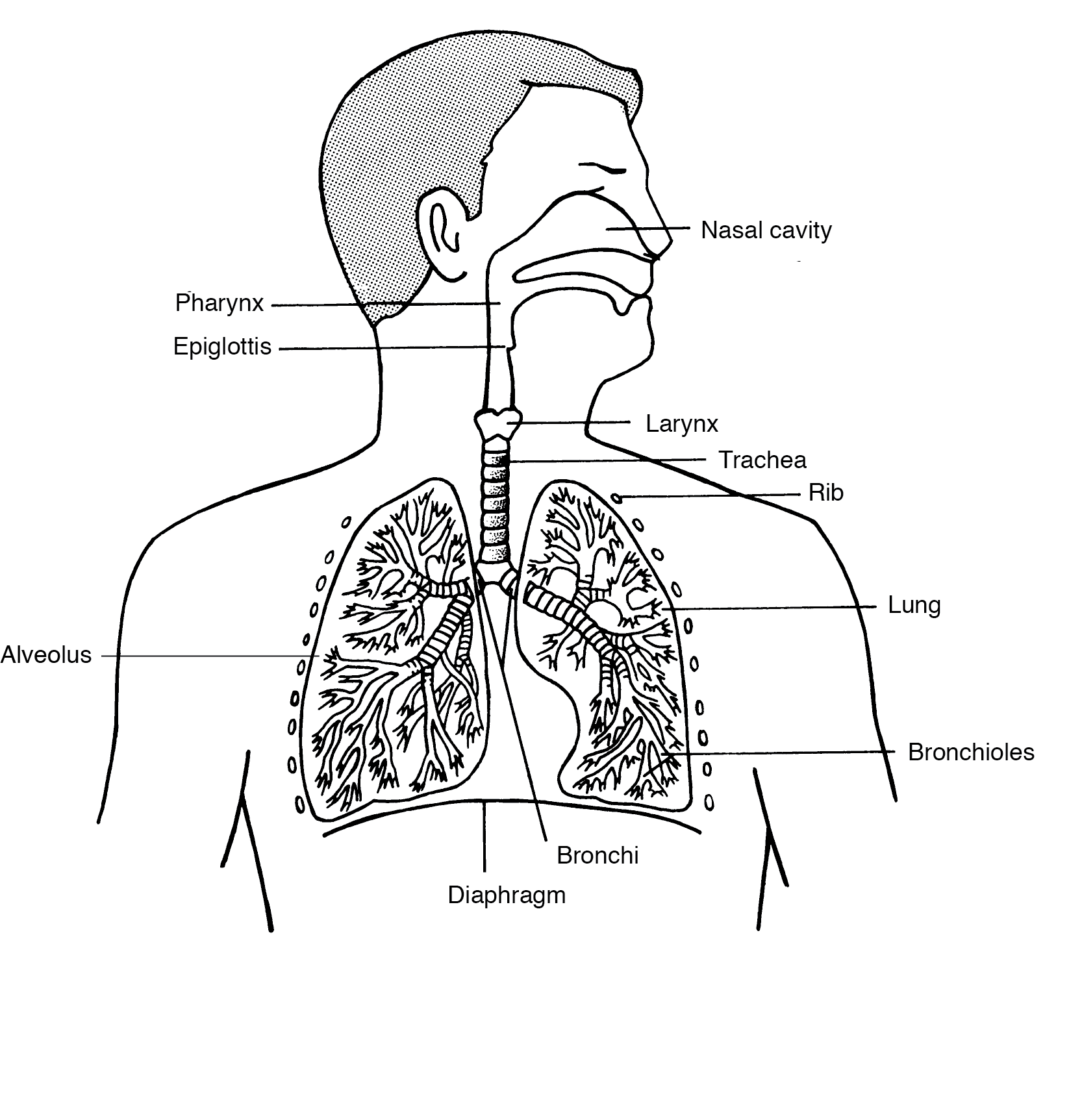
The pulmonary arterioles carry carbon dioxide–rich blood from the right atrium of the heart to the lungs. The blood then enters the capillary beds surrounding the alveoli, where carbon dioxide is exchanged for oxygen. Oxygen-rich blood exits the lungs through the pulmonary venules to be taken back to the left atrium of the heart. From there, the blood flows to the left ventricle, which pumps it into body-wide circulation.
The exchange of carbon dioxide for oxygen at the alveoli relies on simple diffusion. The diffusion rate is directly proportional to the surface area and the concentration gradient and is inversely proportional to the distance between the two gases.
Due to the millions of alveoli in the lung, the surface area for gas exchange is estimated to be between 50 to 75 square meters, or about the size of a tennis court, allowing large amounts of gases to be exchanged quickly. Furthermore, the walls of the alveoli are only one cell thick to minimize distance and maximize diffusion rate.
The diffusion of gases is driven by a concentration gradient. The partial pressure of oxygen is high in the airspace of the lungs and low in the blood, so oxygen will diffuse down its concentration gradient into the blood. The partial pressure of carbon dioxide is higher in the blood than in the airspace in the lungs, so it will diffuse down its concentration gradient out of the blood.
Ventilation rate is controlled by the medulla oblongata, located in the brain stem, which monitors blood pH and carbon dioxide concentration in the blood. Carbon dioxide directly affects pH through the bicarbonate blood-buffering system.

Carbon dioxide (CO2) combines with water (H2O) to form carbonic acid (H2CO3), which can then dissociate into bicarbonate (HCO3–) and protons (H+). When the concentration of carbon dioxide is high, the equilibrium shifts to the right, favoring protons and bicarbonate. An increase in protons decreases the pH of the blood, causing acidosis, and leads to an increase in ventilation rate. When the concentration of carbon dioxide is low, the equilibrium is shifted to the left, favoring carbon dioxide and water, which decreases the concentration of protons and bicarbonate. A decrease in proton concentration increases the pH of the blood, leading to alkalosis, and causes a decrease in ventilation rate.
Now try answering this question about the respiratory system.
Which of the following would NOT be expected to cause a decrease in ventilation rate?
Step 1: This question is asking what will not lead to a decrease in ventilation rate.
Step 2: Recall that the medulla oblongata regulates breathing rate by sensing carbon dioxide levels and pH. Ventilation rate would decrease in response to elevated blood pH caused by low carbon dioxide concentrations in the blood.
Step 3: Predict that ventilation rate would increase, not decrease, in response to high carbon dioxide concentration or decreased blood pH.
Step 4: Choice (D) is correct. The medulla oblongata does not measure oxygen concentration of the blood, so changes in oxygen concentration, (A), would not affect ventilation rate. A decrease in carbon dioxide concentration in the blood, (B), would lead to an increase in blood pH, (C)—both of which would lead to a decrease in ventilation rate.
Humans use negative pressure breathing. During inhalation, the diaphragm contracts and flattens, and the intercostal muscles of the ribs contract and push outward, causing the lungs to expand. As the volume of the lungs increases, the pressure inside the lungs drops. Air then flows from outside the body into the lungs down a pressure gradient. During exhalation, the diaphragm and intercostal muscles simultaneously relax, decreasing the volume of the lungs. This decrease in volume increases the pressure in the lungs, forcing air out.
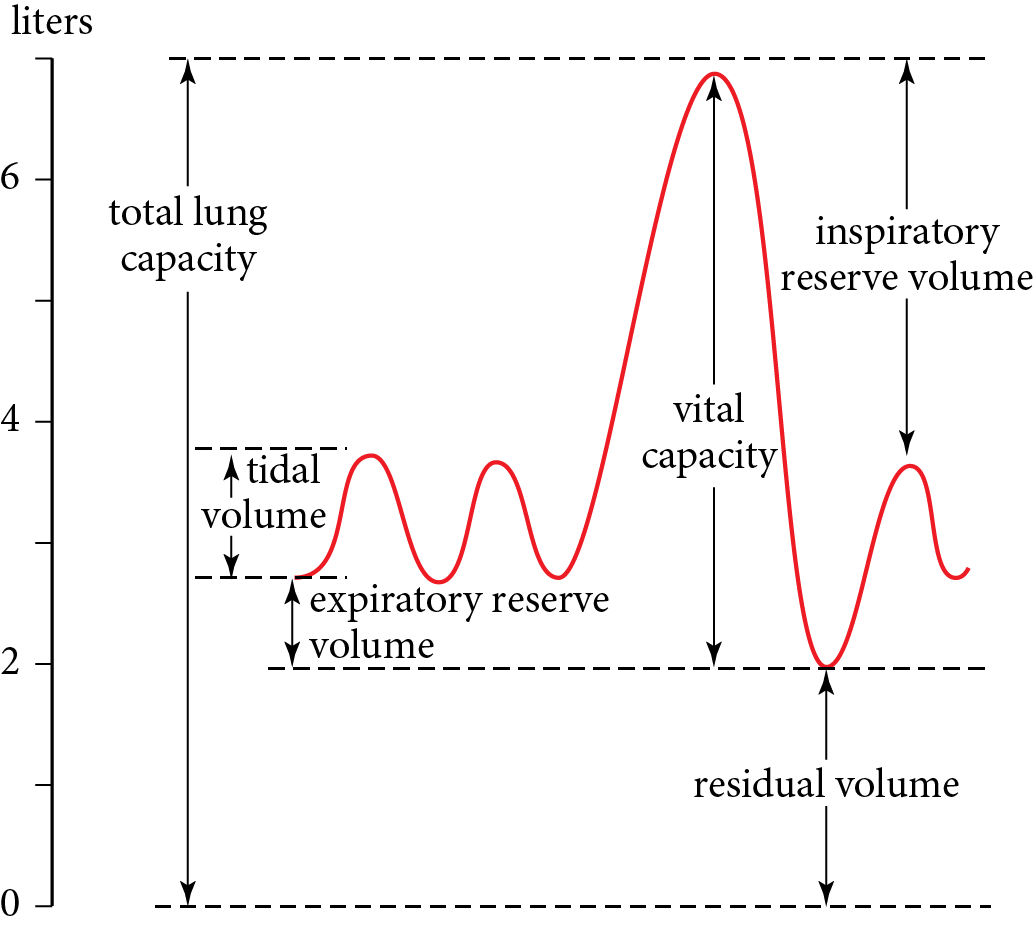
The total lung capacity of an average adult male is approximately 6 liters. This can be further subdivided into the vital capacity and residual volume. Residual volume is the amount of air that always resides within the lungs and functions to prevent lung collapse. Vital capacity is the total volume of air that can be exchanged through inhalation and exhalation and is composed of the tidal volume, inspiratory reserve volume, and expiratory reserve volume. Tidal volume is the amount of air inhaled and exhaled during normal breathing, inspiratory reserve volume is the additional volume of air that can be inhaled following normal inhalation, and expiratory reserve volume is the additional volume of air that can be exhaled following normal exhalation.
Many factors can negatively impact lung function, including genetic disorders, environmental factors, and infection. Genetic diseases arise from mutations in the genome, which can either be spontaneous or inherited from parents. Diseases with a genetic component include the following:
Environmental factors can also affect lung function. Prolonged smoking and chemical exposure can damage the cilia, leading to emphysema (breakdown of the alveoli), inflammation, and allergies.
Many pathogens also infect the lungs. Here are a few examples: