
The Power Vision System (PVS) is based upon training the ocular muscles in order to correct their lack of strength, flexibility, and coordination. These muscles have the responsibility for accurate control of accommodation and “pointing” of the eyes. The starting point for effective intervention with these types of problems is to determine the nature of these muscular defects. (Lateral and front views of the optical muscles are presented in Figure 2.1a and 2.1b.)

Figure 2.1a Lateral view of the ocular muscles.
1. Trochlea
2. Optic nerve
3. Rectus bulbi lateralis muscle (sec.)
4. Obliquus bulbi lateralis muscle
5. Rectus bulbi inferior muscle
6. Rectus bulbi lateralis muscle (sec.)
7. Common tendon ring
8. Rectus bulbi medialis muscle
9. Rectus bulbi superior muscle
10. Levator palpebrae superioris muscle
11. Obliquus bulbi superior muscle

Figure 2.1b Front view of the ocular muscles.
1. Obliquus bulbi superior muscle
2. Rectus bulbi superior muscle
3. Rectus bulbi medialis muscle
4. Rectus bulbi inferior muscle
5. Obliquus bulbi inferior muscle
6. Rectus bulbi lateralis muscle
For other kinds of muscular training, it is necessary to know your own deficiencies (for example, strength, joint mobility, motor coordination, or endurance) to set up specific programs of athletic training. This is similar to requirements of other sports disciplines: you determine the training and discipline that you judge are necessary to accomplish a specific result.
This analogy to sports is very suitable for eye training. For the purpose of decreasing myopia, the crucial point is to optimize the “conditional capabilities” of your eyes—through specific exercises—and to learn the “athletic training” of correct focusing. This will be the basis of your own visual conditioning and capabilities.
Stand in front of a mirror, at about 36 inches distance. The distance you stand from the mirror is the basis of your own focusing capacity. The limit is calculated at the point where you can still see both your pupils clearly. The more myopic you are, the more you must get closer to the mirror in order to see the symmetry and fusion of your eyes.
Position 1
While constantly looking at a selected point (for example, the middle of your eyes or at the tip of your nose), lower your chin, keeping your glance fixed at the chosen central point. Maintain your glance and the pupils at the maximum limit.
Position 2
While constantly looking at a steady point—in the middle of your eyes or the top of your nose—lift your chin up until you reach your limit. In this extreme position, one eye could perform a different convergence from the other, and it might be very hard to maintain convergence in such a position.
Position 3
While looking at a steady point, turn your head to the left until the limit is reached where you can still see with both your eyes without hiding one of your pupils behind your nose.
While looking at a steady point, turn your head to the right until the limit is reached where you can still see both your eyes without hiding one of your eyes with your nose. The same exercise is to be repeated in the other four directions of your visual field.
Position 5
While looking at a steady point, incline your glance down toward your right as far as you can.
Position 6
Looking at a steady point, incline your glance down toward the left as far as you can.
Position 7
While looking at a steady point, incline your glance up toward the right as far as you can.
Position 8
While looking at a steady point, incline your glance up toward the left as far as you can.
It will be hard to maintain the perfect convergence in these extreme positions, so you might have double vision. This phenomenon will become more apparent in certain positions.
These errors in convergence demonstrate a flexibility defect as well as the incapability of maintaining a long fixed glance in such positions. This action demonstrates a strength defect of the agonist muscles (those muscles that are resisted or counteracted by another muscle, the antagonist), and consequently a coordination error.
Weak muscles, with defects in muscular symmetry and improper convergence in one or more directions of the visual fields, lead to inexact accommodation and adjustment, jeopardizing visual functioning. It is very hard, and perhaps impossible, to “point” to an object and make its image fall on the central fovea—the most sensitive retinal portion for accurate focus—in these conditions of muscular imbalance and asymmetry.
The Power Vision System is aimed at improving the “athletic” capabilities of the eyes gradually and specifically with valid and evident improvements. Results will be gradually achieved—restoring the eye’s extrinsic muscles’ symmetry, strengthening them, and increasing their flexibility. All this great work is carried out using the physiologic SAID Principle (Specific Adaptation to the Imposed Demand) through the wise use of lenses with gradations opposite to the corrective one—positive lenses for nearsighted and negative lenses for farsighted people—together with the CRB (Contraction/Relaxation/Blinking) eye movements (explained more fully in Chapter 5).
Striated or “voluntary” muscles work as pairs.
Every muscle is both agonist and antagonist; it depends on which movements are involved (that is, in arm flexion the agonist muscle is the biceps, and the antagonist is the triceps muscle. In arm extension, the agonist is the triceps and the antagonist the biceps.) Due to the stretch reflex called “reciprocal innervation,” when the agonist contracts, the antagonist relaxes. This stretch reflex helps the muscle to lengthen and helps coordination for the best execution. In the eye muscle, the active static stretching exercises help relax the antagonist muscle and develop strength in the agonist.
The best eye stretching exercise is the “rotation from a fixed point” test described previously, because it permits the feedback of perfect coordination. For best results, once some muscular imbalance in coordination is found (when the vision doubles in extreme positions of the visual field), one must continue in those positions searching for ocular fusion, searching to relax the eye muscle in those extreme positions (standing in front of the mirror, rotate the head, searching for the field of double vision, and try to relax, searching for ocular fusion). After some time you eventually will experience clearer vision and improved acuity.
This exercise will ensure the best and fastest results because it greatly improves the muscular performance of the eye muscle (best central fixation and coordination) in those visual fields where it is most needed. The “specificity” of the visual range where the stretching is applied in this exercise is the reason for its efficacy.
The first phase of implementing functional rehabilitation will produce a gradual improvement in your focusing capacity. It includes muscular training, which occurs because the agonist and antagonistic muscles are strengthened.
This phase acts on their properties (strength, flexibility, and coordination) gradually. Working with this muscular group of the six extrinsic eye muscles restores their coordination. It increases the eye’s “central fixation” ability and improves the eye’s dynamic (saccadic) movements. The “plasticity” of the striated muscles has been established by the research carried out in monkeys by A. B. Scott in 1994.
This research was aimed at defining whether the extraocular muscular system of the monkeys had the capacity of adapting (that is, the feature of “plasticity”). The research determined that the monkeys’ extrinsic muscles—being held in the state of lengthening through sutures—lengthen at 18%, 25%, and 33%. Obviously, in the case of PVS, muscular rehabilitation and the restoration of extrinsic eye muscle functioning isn’t achieved by suturing the muscles. It is achieved through the systematic work of ocular stretching at the maximum ranges of the ocular field.
The two fundamental factors of ocular stretching are (1) strength increase and (2) training load increase or a gradual intensity increase.
Since we are working toward a strength increase of the eye’s extrinsic muscles—which are of the striated type—the muscles are subject to the very same rules as any other striated bodily muscle (calf, triceps). The strength of these muscles depends on their capacity of working—shifting a load—over a certain period of time. Similar to strength exercises such as bodybuilding, the muscles carry out dynamic contractions—eccentric and concentric types—in which the trained muscle varies its length to the applied load. An example would be working with a barbell.
When increasing the strength of the eye’s extrinsic muscles, the contractions are of the isometric type, where the resistance is steady and exists even without movement of the visible load. Obviously it is impossible to get a barbell or physical load onto the ocular muscle. In such cases, the resistance is given by the antagonistic muscle, which opposes the movement.
For example, let us review one of your muscular work movements—the one of fixing at a point at the extreme left part of the visual field on a horizontal level. In this movement, the strength of the agonist muscles—musculus rectus on the left side—will increase, and the flexibility of the antagonistic muscles—musculus rectus on the right side—will improve. In the opposite movement—when you fix at the extreme right part of the visual field on a horizontal level—the situation will be different. The strength of the musculi recti, which is agonist in this movement, will increase, and the lengthening capacity of the musculi recti on the left side (antagonistic muscles in this case) will be increased.
Doing these exercises in all sections of the visual field—schematized in eight positions—points to where the imbalance is more evident. Your eyes’ performance is necessarily being gradually improved through this muscular rehabilitation.
The contraction “intensity” factor is the fundamental concept for such rehabilitative work and must be pondered carefully to achieve efficient training stimulus and to generate the required muscular tissue adaptation. A small training stimuli, like very weak contractions, leads to little or no results. However, a well-measured contraction intensity leads to stimulus optimizing, with additional overcompensation. This means muscle adaptation to the stimulus—better muscular performance, and consequently more accurate “pointing.”
You can analyze an overcompensation graph—meant as a performance/functional capacity increase of an organ or system of organs—usually used to highlight improvement of sports performance capacities. Muscular work—in this case, doing the work of fixing at extreme parts of the visual field—leads to an initial drop of the trained muscle’s efficiency. In the case of ocular muscle training, this phase is characterized by a transient and physiological drop in focusing capacity.
After a suitable recovery time, the muscle both overcompensates—becomes used to the training load given by the exercise —and, as a physiological consequence, develops better properties—strength, flexibility, and resistance. As for the extrinsic ocular muscles, the result will be better coordination and “pointing” of the eyes. These muscles are responsible for saccadic movements and central focusing. Proper tone of these muscles is essential for accurate, clear vision.
Intensity Evaluation in Ocular Exercises
How can we calculate load intensity in ocular isometric exercises—fixing the borders of the visual field—if we cannot vary and/or measure it “by sight”? We do this in ordinary strength exercises when we change the weight on a barbell. We can compare it to the forms of isometric strength increases by any striated bodily muscle.
That is the relationship between contraction duration and the range of movement—but in the case of the eyes, the range of the lever can’t be taken into account because the length of the limbs does not exist. The person who has organic visual problems—cataracts, glaucoma, and/or retinal detachment—should not do these exercises.
Optimal Intensity
To achieve intense contraction—efficient stimulus—focusing is maintained at an extreme level as long as possible, until you feel a slight muscular tiredness. However, your contraction intensity should be evaluated by an optometrist who understands the concepts of the Power Vision System. Therefore, the opinion of a physician or a specialist is advisable.
It is very important to adjust the stimulus to your new visual capacities from time to time so as to maintain the stimulus intensity efficiently and to be able to bring about visual system adaptation.
Such training load variation in the ocular stretching exercises can be done by increasing the number and the wideness of ocular rotations as well as the duration of maintaining each position at the extreme point of the visual field (in such cases, the more the speed is decreasing, the more the contraction intensity is increasing).
The relationship of lens to reading distance should be gradually increased in the exercises with lenses (positive for nearsighted/myopic people). Once you are able to read at an arm’s length distance with +1 diopter positive lenses, you should proceed to the +1.50 or +2.0 lens, reading at the distance where you have a slightly blurred vision by trying to focus the text doing CRB movements. In the case of low myopia—when wearing the plus lenses indoors at home or at the office—so as to reduce environmental near-point stress, you should slightly increase the “leisure” lens-induced blur. Slightly myopic or nearly emmetropic people should wear positive lenses at home or at the office. In the case of moderate to high myopia, it is not necessary to wear positive training lenses at home or at the office. It will be enough to wear lenses slightly weaker than the prescribed ones for close work.
If you don’t carry out gradual training load increasing, you will be confined within the limits of the already reached adaptation of your visual system to that kind of stimulus (rotation intensity, the power of training lenses) and, consequently, within the achieved improvements.
Wherever you are, always respect safety rules. If I work in an airport control tower, or if I am a pilot or bus driver where I am required to have perfect sight, I’ll avoid “myopizing” my eyes even for therapeutic reasons. Therefore, I’ll wear full correction lenses for my refractive error.
The same rules apply to personal and collective safety and must be respected. You take complete responsibility for your own actions. Neither the optometrist nor specialist can be blamed for anything under this circumstance.
Active and passive work on oculomotor muscles through active stretching finds its therapeutic validity in the physiological foundation of the relationship of length to muscular tension.
Any imbalance causes lower efficiency in “pointing” movable targets, lower and imprecise focusing capability on central fovea (central fixation), as well as lower saccadic vibration capability (because of slow and “dulled” muscles). The quality of ocular muscles’ work and of all the striated muscles in general depends on harmonious interaction between agonist and antagonistic muscles in a certain movement. Any strength and flexibility imbalance causes a lower capability of working and moving, because of a lower level of active contracting and a higher level of passive resistance created by little-used muscles.
As you can see in Figure 2.2, optimal muscular movement, or its optimal active working (contracting), can be performed when the muscle is in optimal length range. A chronically contracted muscle or, conversely, a too-stretched muscle, can’t perform its function of action/reaction/movement optimally. Analyzing this problem thoroughly, we find that there are two microfilaments that are fundamental components of a muscle: actin and myosin. Muscular contracting comes from these two components sliding one over the other. Stretching happens the opposite way: when the level of superposition between actin and myosin gradually decreases. Opposite to contraction, muscular stretching itself happens in a “passive” way: In the case of ocular muscles, where gravitation can’t act, stretching happens passively, thanks to the agonist muscle.

Figure 2.2 Relationship of muscular length to tension.
When all the range of the movement isn’t completely used (as happens when limited visual ranges are used due to the frame of the glasses), the muscular capability of active contracting becomes lower, as does muscular elasticity itself, affecting fundamental factors for optimal vision like the capability of pointing, central fixation (centralization), and saccadic movements. If ocular stretching is performed symmetrically and within the extreme range of the visual field, it preserves and restores the optimal relationship between length and muscular tension, which is very important for correct, clear, distinct vision.
We can use the SAID Principle here. The eye adapts to the environmentally imposed requests.
As has already been discussed, there is a close relationship between the development of myopia and prolonged close work. In studies carried out on pigeons, researchers discovered a different refractive capacity in different sections of the visual field (Catania, 1964; Millodot & Blough, 1971; Nye, 1973). The pigeons had normal sight when their refractive state was measured when their eye was measured along its own axis, on the frontal level. The more the pupil axis got closer to the lower visual field, the more myopia was increased (Fitzke et al., 1985).
This interesting result shows that the visual system can selectively adapt to its environment, since the bird must both focus on near objects for feeding and at the same time have a correct alignment of the upper parts of its visual field to see birds of prey.
It is important to keep in mind that the variability of such refractive conditions is not steady within a species. The animal’s eye adapted to its visual environment (see Miles & Wallman, 1990).
The eye adapts its focal status to the near visual field. When this happens, a minus lens is prescribed. This lens has a negative effect on the human eye. The minus lens produces an overaccommodative effect. Further, the minus-lens glasses limit normal range of eye movement. Wearing any pair of glasses necessarily limits motion. The eyes hardly ever have room because of the limits imposed by the frame (see Figure 2.3). Such restriction of eye-movement range over time leads to the extrinsic ocular muscles adapting to the range of motion imposed by the frame of the glasses.

Figure 2.3 Limited visual range.
The frame of the glasses hinders and limits the entire eye movement with the consequent decrease of the extraocular muscles’ working range.
As a result there is an in pejus (negative) adaptation by the extrinsic muscles’ elastic capacities. A further consequence is the loss of coordination and quality of saccadic movements. In such a “cage,” the eye’s visual field is imprisoned; this leads to eyestrain and stiffness—with further development of myopia.
These facts were emphasized by Dr. William H. Bates (1881–1920), the father and pioneer of visual rehabilitation. He pointed out that the stiffness and steadiness of the gaze, as well as muscular tension, are the principal causes for defective sight.
Just remember that when a striated muscle is being subjected to a decrease in its normal range of movement, it gradually develops decreased flexibility and coordination. In the case of the extrinsic eye muscles, their flexibility is directly correlated with their coordinating capabilities and is part of their fundamental capability.
The Power Vision System exercises the ocular muscles through ocular rotations—with some variations—at the maximum range of ocular movement.
These motions rehabilitate and prevent the elastic ocular capabilities of the visual field from narrowing. This narrowing occurs because of the habitual wearing of glasses. PVS restores these necessary capabilities of the natural eye—like strength and flexibility—needed for optimal saccadic movement and clear vision.
Active emmetropization is a phenomenon in which the eye adjusts its focal status to its environment. The process is seen in the eye’s tendency to bring its refractive state closer to zero—defined as emmetropic or clear sight. This phenomenon demonstrates the natural eye’s capacity of changing its refractive power toward the applied visual environment. (The word emmetropia means a focal state of exactly zero. Most eyes with 20/20 vision have a focal status of zero to +1.5 diopters [Hayden, 1941]).
The effect of this emmetropization process is clear as it applies to humans. Proper modification of the near environment with a plus lens will help the natural eye emmetropize in a positive direction—thus clearing distance vision.
A slightly nearsighted person who does not wear his minus-lens glasses for some time can notice an adaptation of his focusing capacity in a positive direction. This is a consequence of the active emmetropization stimulus. Not wearing the glasses reduces the hyperopic defocus that is caused by traditional negative optical correction (allowing a certain margin for this emmetropization process to work properly. I grant that gradual emmetropization of refractive error is a slow process. For this reason it is necessary to back up the adaptation of the eye to the lenses through suitable and gradual use of the defocus state).
The phenomenon of active emmetropization has been noticed for some time in experiments with animals. These experiments demonstrate a recovery from nearsighted (nonzero) refractive states. The eye has the ability of compensating for lens-driven retinal defocus.
The first evidence for active emmetropization—the eye’s response to its visual environment—following an induced myopic state was identified in chickens (Wallman & Adams, 1987; Norton, 1990; McBrien & Norton, 1992). The study carried out on the monkeys reported that the primate eye demonstrated a recovery from retinal defocus induced by contact lenses that were experimentally used on these animals (Smith et al., 1994). The studies in monkeys, chickens, and guinea pigs show an adaptation of the visual system—active emmetropization to the visual environment—in response to lens-driven refractive errors.
The effect of applying an external negative lens produced a net negative change in focal status of the eye. The effect of applying an external positive lens produced a net positive change in focal status of the eye. This is because of the eye’s ability to change its length proportional to the applied plus or minus lens, that is, the dynamic and innate emmetropization process. The test demonstrates that the ocular refractive state can be changed suitably by correct application of the correct lens for recovery and prevention.
A mildly myopic person, subjected to certain stimuli—myopic defocus led by positive lenses or undercorrections—will with time decrease his refractive error. If this process is initiated before the minus lens is used, the eye’s focal status can potentially be cleared back to normal (emmetropia). The opposite concept works as well. A hyperopic person, subject to minus-lens hyperopic defocus, can decrease his positive refractive error and get close to an emmetropic state. (I can personally testify to, and prove—apart from clear scientific results—the success of this process in humans, specifically concerning recovery from myopia, since I worked myself out of it over a period of ten years.)
The phenomenon of active emmetropization is an expression of the SAID Principle, meaning that the eye has bidirectional control. This compensating ability acts in response to the use of either positive or negative lenses (myopic or hyperopic defocus).
The theory of accommodation behavior suggests that after
some time retinal position is changed to better
coincide with focal point of the lens-retina system.
—Theodore Grosvenor and David A. Goss,
Clinical Management of Myopia
Current studies carried out on animals suggest that refractive development and, therefore, the refractive state are modulated by the accommodation status and the clarity of focus of retinal image. Defocus of the retinal image with minus lenses causes an acceleration and enlargement of the vitreous chamber. This results in myopia. The plus lenses cause a slowing of the axial elongation of the eye, allowing for the prevention of nearsightedness (Schaeffel et al., 1988; Schaeffel & Howland, 1991; Irving, 1991; Grosvenor & Goss, 1999, p. 54).
The possibility of altering refractive development by inducing retinal defocus (change) was first studied by Hung et al. in 1995, using young monkeys. The study proved that the focal status of Rhesus monkeys was profoundly changed by the forced wearing of a plus or minus lens.
The monkeys wore helmets so the lens could be kept in place. The left eye was used as the control and the right eye had variously a +6, +3, 0, –3, and –6 diopter lens applied. The monkeys were from 21 to 32 days old at the start of the test to confirm the eye’s dynamic response to these applied lenses. The test continued for 72 to 113 days.
At the end of the experiment the refractive change was measured with retinoscopy. The initial focal states of the monkeys were from 2 to 8 diopters. (With respect to the starting focal status, the left eye is almost always very close to the right eye, with a “spread” of about 0.5 diopters.)
The result of this test demonstrated that the right eye followed the applied lens. If the lens was plus, the right eye went more plus (moved in a hyperopic direction). If the applied lens was minus, the focal status moved in a negative direction (that is, moved in a “nearsighted” direction).
This test demonstrated that the natural eye uses its environment or the applied lens to control its long-term focal status. According to the theory of accommodative balance, if the treatment had been stopped at the right moment, the emmetropic state would have been achieved without developing hyperopia. So it is obvious that the refractive state is influenced by the defocus on the retina and that you can voluntarily control your refractive status by modifying your environment, thereby preventing a negative focal status from developing.
PVS provides a system enabling a gradual decrease of refractive errors toward 20/20 vision. It takes its basis from the connection between the development of myopia and near-work, as well as from the eye’s ability to react to induced change in the visual environment. Many studies—carried out in humans and animals—clearly show how the visual system, because of its focusing capacity, changes its focal status as the environment is changed.
There’s a close relationship between the development of myopia and environmentally induced refractive conditions. This is the case when working indoors. The eye can’t adjust to longer focusing distances, so the accommodation system “steers” the eye into nearsightedness.
Such facts are clearly demonstrated in humans. By analyzing this relationship (myopia development by environmentally induced near-point stress/refractive stress), we can confirm different myopic development depending on work and environmentally induced near-point stress (overaccommodation). On the basis of this correlation between the refractive state changes and environmentally induced change, we can see the possibilities for acting on the causes of the problem—the defocused state. Such knowledge allows us not only to prevent myopia from developing but to also act voluntarily to decrease it.
Your refractive state can be consciously manipulated by you. This depends on the kind of refractive error you have (nearsightedness or farsightedness) providing a suitable stimulus. This applied lens is aimed at the visual system’s ability to adapt, consequently helping restore your distance vision to normal.
Such an aim can be achieved through retinal defocus: in the case of nearsightedness, to decrease myopic functional errors using positive lenses or undercorrections; for hyperopic retinal defocus, to decrease hyperopic refractive errors by using a negative lens.
Myopic defocus occurs when the accommodative stimulus exceeds the individual’s amplitude of accommodation by approximately 1 to 2 diopters, producing increased amounts of underaccommodation and consequent retinal image defocus. Beyond this point, the accommodative response becomes progressively smaller and gradually shifts toward the tonic accommodative level (Ong & Ciuffreda, 1997). (See Figures 2.4, 2.5, 2.6.)
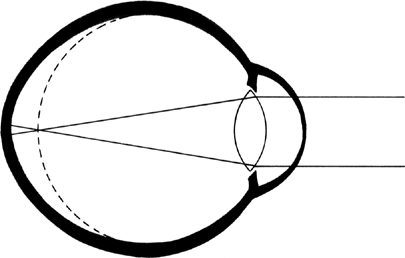
Figure 2.4 Myopic eye.
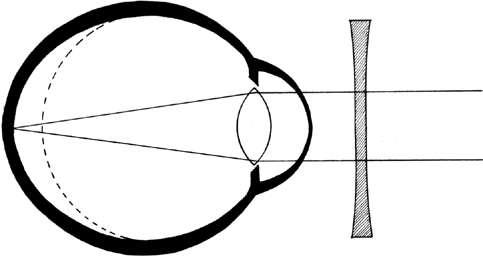
Figure 2.5 Optical correction for myopic eye with a concave lens (–).
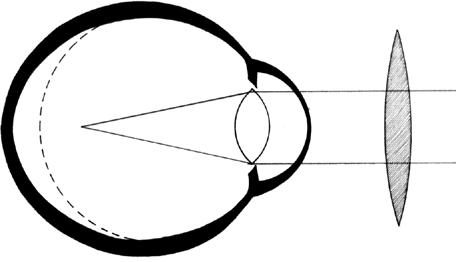
Figure 2.6 Myopic defocus induced by a convex lens (+) on myopic eye.
If the dioptric stimulus is progressively positioned beyond optical infinity (possible only with optical systems), the accommodative response gradually shifts (relative to the response at optical infinity) slightly higher toward the tonic accommodative level (Ong & Ciuffreda, 1997). (See Figures 2.7–2.11.)
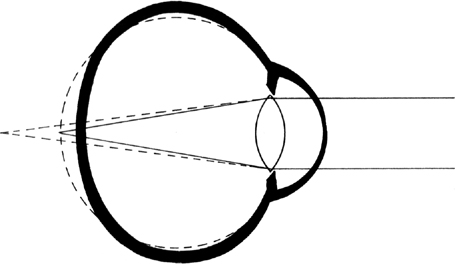
Figure 2.7 Hyperopic eye.

Figure 2.8 Optical correction of the hyperopic eye with a convex lens (+).

Figure 2.9 Hyperopic defocus by concave lens (–) on hyperopic eye.

Figure 2.10 Hyperopic defocus by convex lens (–) on myopic eye.
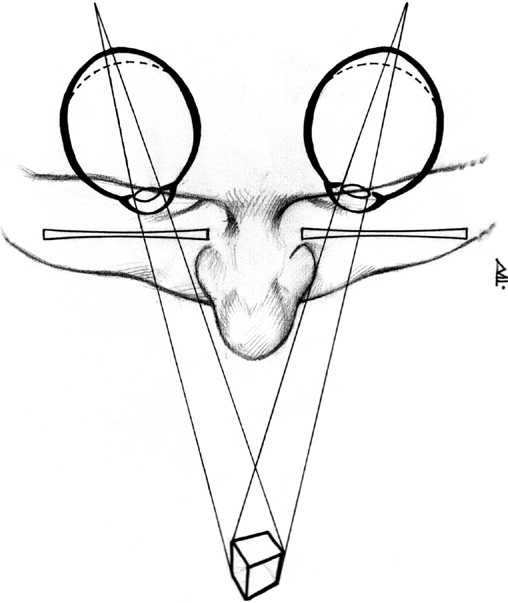
Figure 2.11 Hyperopic defocus induced by the use of negative (concave) lenses—reproduces the effect of near vision on the eyes focal status. In addition, convergence acts as a further myopic impulse.
• Defocus is of the myopic type when using positive lenses or undercorrections. This is because the focal point of ocular imagery is shifted in front of the retina.
• Defocus is of the hyperopic type when, using negative lenses, the focal point of ocular imagery is shifted behind the retina.
Such retinal defocus stimuli are artificially produced in the Power Vision System by using lenses or undercorrections. In this case, both the adaptation and the refractive visual error counterbalancing are found through the suitable state of defocus/fogging.
The retinal defocus state also occurs under normal conditions when we fix on a distant object and then immediately turn our glance to a near object—instantaneously, and before starting the accommodative response, the focus is behind the retina. When the accommodative response is less than the dioptric stimulus (as controlled suitably with lenses), a certain level of hyperopic defocus will remain (Wildsoet, 1998, p. 35).
This stimulation leads to the adaptation of the eye’s refractive capability and consequently its focusing—compensating for the initial refractive error. Such a system of retinal defocus, being prolonged over time, allowed me to decrease my myopia gradually, by 2 diopters in each eye. The complete defocus state, induced by lenses, acts as an overaccommodative balance, thereby providing the rationale for a functional adaptation of the focusing system.
Unsuitable use of defocus, as occurs with current optical “corrections” (hyperopic defocus for nearsighted people through negative lenses, and myopic defocus for farsighted people through positive lenses) tends to worsen visual errors, thus “spoiling” the natural eye’s refractive capabilities. Medina and Fariza (1993) reasoned that the traditional correction of myopia with negative lenses inserts an initial error that causes hyperopic defocus and accelerates nearsightedness progression (that is, worsening). How many pairs of glasses have you changed up to now, increasing the dioptric power of the lenses each time, following this traditional method of correction?
To make this concept completely clear—even to the nonspecialist reader—let me say this: a treadmill carrying a still person (one who was not moving his legs) from one side to the other would hardly ever stimulate the person’s locomotion and walking. Running or walking with increasingly heavier ballast, on the contrary, stimulates one’s physiological abilities to a large degree.
What hinders might strengthen, what helps might destroy, bringing about an undesired adaptation of a physiological system. Such a principle explains the behavior of most physiological systems. A suitable optical stimulus creates the adaptation of the focusing system to the lens as part of the SAID Principle.
The effect of lenses on focal adjustment can be found in many scientific works, such as Smith (1998). Retinal defocus induced by near-work and, if worsened by hyperopic defocus (induced by negative lenses for myopia), will in time lead to axial myopia, that is, eyeball lengthening. (See Smith & Hung, 1995; Raviola & Wiesel, 1985; Wallman, 1993).
The eye’s refractive capacity is influenced by environmental factors—as when the observed object is near. Refractive capacity is affected by emotional factors; our mood can affect our wish to see the observed object. For instance, a severe glance by someone in authority, repeated many times, can cause us to withdraw from the world into a state of comfortable blur, that is, into our “own world.” The eye is a living and vibrant organ, and its refractive status is the sum of all the stimuli that impinge on it.
Your ocular status is characterized by what I define as accommodative balance. Your focal status is the result of all physical and mental stimuli, that is, your environment. These stimuli are imposed on your eyes whether you like it or not. The major stimulus here is overaccommodative stress, induced by near-work. Improvement would be accommodative relaxation, induced by looking at distance, light, and improving the working range of ocular muscles. It is extremely important to understand this concept so as to reduce refractive errors—since you must count on this mechanism to change your refractive state in a positive direction.
Your refractive status is maintained if there is a balance between myopic and hyperopic stimuli (see Figure 2.12). For instance, if myopic stimuli (close work) overcome the hyperopic (distant viewing), this will eventually produce a refractive change toward myopia. Such a phenomenon is nothing else but the reaction and adaptation of a visual system to the applied stimuli—and that is the specific expression of the SAID Principle.

Figure 2.12 Accommodative balance, or the eye in a state of equilibrium.
[left] Visual stimuli at near distance
[right] Visual stimuli at far distance

Figure 2.13 The prevalence of near vision stimuli causes a change of accommodative balance toward myopia.
[left] Visual stimuli at far distance
[right] Visual stimuli at near distance
[right] Stress of the nervous system
Fundamental characteristics required to generate a change in someone’s refractive capacity include:
• Induction of a suitable kind of stimulus (either myopic or hyperopic, depending on the initial functional refractive error)
• Induction of enough intense stimulus or defocus (either too much or too little intense stimuli do not create an adaptation)
• The time of exposure to stimuli (the quantity of time being exposed to defocus must be so great as to induce a transient change of your refractive state)
Such exposure tends to transiently change the accommodative balance with time, causing steadier and steadier changes and becoming a part of one’s normal refractive capabilities. A myopic person, trained with myopic defocus on a regular basis, little by little will get closer to the emmetropic state, intervening over his accommodative balance.
Denying the theory of accommodative balance would mean denying the capacity of all the organs and physiological systems to adapt or modify themselves to various induced stimuli. It would mean denying the physiological principle of Specific Adaptation to the Imposed Demand. The heart gets used to the stimuli that are induced in aerobic training. The skin undergoes adaptation to temperature and light rays. The muscles get used to the induced load. There are countless examples of stimulation that impinge on a living organism.
So—why should the eyes and their refractive state be different? One’s refractive status changes in relation to environmentally induced stimuli. Or this change is willingly caused and led by a specific visual training. By using plus lenses or undercorrections suitably, you can change your visual environment. The result will be a gradual adaptation of your refractive status in a positive direction and a resultant clearing of your distance vision.
It is documented by scientific experimentation and in technical publications that your refractive state is regulated by the diopter power of your visual environment. This includes both the quality and kind of refractive stimuli that impinge on your eyes. Therefore, the eye and its refractive capability to change are influenced by accidental stimuli (like overaccommodative stress induced by near-work) or by willingly and artificially induced stimuli designed to cause either adaptation or compensation for the induced defocus.
The experiments carried out on animals are very significant (Hung et al., 1995; Schaeffel, 1988; Siegwart & Norton, 1993; McFadden & Wallman, 1995). In these studies, lenses were used to induce specific adaptations of animals’ (chickens’ and Guinea pigs’) refractive state. The result was that the eyes adapted themselves toward myopia, using negative lenses that were causing hyperopic defocus and axial elongation of the eyeball. This “adaptation effect” is the unfortunate result of using the improper optical correction.
Let me repeat: Myopia, when corrected with negative lenses, results in myopia worsening. This is because of increasing overaccommodative stress and inducing hyperopic defocus, which in time sets up the stimulus for axial elongation of the eye (see Medina & Fariza, 1993). Conversely, the wise use of positive lenses or undercorrections, generating transient, artificially induced myopia, causes a myopic retinal defocus. This is a stimulus that compensates for the initial error. In this case the eye is “pushed” to compensate for the initial error so as to restore the optimal refractive state (see Smith, 1998).
All this is a direct expression of the SAID Principle: a specific stimuli leads to a specific adaptation. In this case the result worsens the initial refractive error.
Birnbaum and many other clinicians (Birnbaum, 1988, p. 169) state that the use of positive lenses on the threshold of myopia could prevent nearsightedness in the first place. There are quite a few optometrists who have stated this concept over the past century. The reason for using a preventive lens is to modify your visual environment so as to mitigate or completely remove all the near stimuli. Doing so will lead to a reduction of accommodative stress. And, of course, accommodation stress is recognized as the cause of the gradual development of myopia.
Most existing scientific studies on the use of positive lenses for preventing and reducing myopia were conducted using bifocal lenses. The lower part of the lens was positive (to oppose the effects of overaccommodative stress) and the upper part had either no lens (plano) or had a reduced-power negative lens.
Roberts and Banfort (1967) found that the use of bifocal lenses brings about significant reduction in the rate of development of refractive errors. The downward rate developed at –0.31 diopter per year for the test group using a plus lens (bifocal) compared with a rate of –0.41 diopter per year for the control group using the regular minus lens.
The strongest success in preventing negative movement into myopia was conducted by Kenneth Oakley and Francis Young in 1975. In the lower part of the bifocal lenses they used +1.50 diopters, and the upper part of the lens was undercorrected by 0.5 diopters. Oakley and Young determined that the overall average increase of myopic error was –0.02 diopter per year for the bifocal group. The “standard prescription” group continued into myopia at a rate of –0.53 diopter per year. The clear success of this study was attributed to the fact that a sufficiently strong plus lens was used. The “students” were motivated to follow the desired protocol of Francis Young. They were given a strong plus for all close work and a weaker plus for distant viewing.
Many scientific studies confirm the effects of retinal defocus on the refractive state. Each organ adapts to the induced specific stimulation, and the eyes and their refractive capacity are not an exception. The use of gradual myopic defocus (induced by a positive lens or undercorrections) leads toward regressing and gradual compensating for the initial error. The expression “The functioning makes the organ” is very often used in medicine. The expression means, “Each stimulation produces a physiological adaptation.”
Blurred retinal image requires accommodative innervating which is aimed at modifying the dioptric power of a crystalline lens in order to optimize adjustment and thereby achieve clear vision. Retina signals a “focusing error,” and this perception sets up a stimulus to modify the innervating “signal” which controls the crystalline lens. That is when the focusing error is canceled and the modifying stimulus stops.
—Gian Paolo Paliaga, I vizi di refrazione
This stimulus causes focusing adaptation and optimization and is completely opposite to optical correction with corrective lenses. A focusing stimulus, used gradually, generates a natural adaptation of the visual organs and their focusing capacity: it leads to a regression of functional visual errors.
The secret of getting back to 6/6 (20/20, in English units) eyesight—or to decrease your present dioptric prescription—is to use this principle of consistent effort. This means increasing the focusing distance gradually, so that you recognize the necessity of using a stronger plus lens or undercorrections as you see your distance vision improving.
The eye’s focusing power depends on several stimuli, including:
• Psychological or physiological conditions (stress, fear)
• Mental and physical tension
• The visual environment
• Artificially induced refractive conditions caused by contact lenses and glasses
A slightly myopic person who trains with a plus lens or undercorrections while reading a book or the newspaper must always discipline himself to read at the “blur point.” That is, he must push the reading material away from his eyes to the point of “just blurred.” This creates a training load for the focusing system. It is as if we trained the extrinsic ocular and the ciliary muscles using a stronger and stronger applied load.
In this case, the load is part of both your reading distance and the power of training lenses. Once the focusing system gets used to that load—which is the relationship between dioptric power of the eye and the training distance—it is necessary to increase the load in order to clear your vision further. If this is not done, the stimulus will not continue to have the desired training effect.
This phenomenon, which induces a training accommodative stimulus (for better adjustment with the consequent functional refractive error decrease), is called “fogging,” or “blur-driven accommodation”; the eye is voluntarily led to the state of slight fogging so as to be stimulated for focusing. It is very important to measure the training stimulus.
With this kind of system, which leads into a slightly burred state (so the letters of the observed text can be hardly distinguished), the eye’s refractive state can be modified automatically and gradually so as to bring “focus” back on the retina, or at least, as close as possible. It means that a myopic person, whose focal point is in front of the retina, must shift it to nearer the retina, consequently optimizing focusing. For hyperopic people, whose focal point is behind the retina, the principle works well when used in the opposite direction (negative lenses at the shortest possible distance).
The load or the training stimulus imposed on the eye’s focusing capacity must be efficient; that means neither too excessive nor too little. The best training effect is achieved by having minimum fogging, when the letters or the object you are focusing on are slightly out of focus.
Excessive fogging may cause the opposite negative effect, worsening either myopia or hyperopia. The reason might be that in the case of an excessive stimulus, focusing becomes impossible, without even having a try at all.