TLYMPHOCYTES—white blood cells known as T cells—are the master cells of the immune system. They communicate with almost every other cell in the body. T cells constantly converse among themselves and with the many different kinds of cells they directly influence, including all other immune cells, blood cells, lining cells, and even some friendly microbes.
All organ cells turn to the T cell for help with trauma and infections. T cells chase and kill microbes and attack cancer cells. T cells also morph into a wide range of subtypes that analyze situations, attack problems, and support other cells in a variety of ways. They can rapidly become a large army of fighting cells. T cells are also able to remember for years the particular signals that were successful in defeating a viral invasion.
A primary job for T cells is to evaluate pieces of material that shouldn’t be in the body—microbes, cancer cells, debris, and chemicals. When they find these foreign molecules on the surface of other cells, T cells organize campaigns to eliminate them by directing the activity of traveling blood cells, other immune cells such as B lymphocytes (B cells), lining cells, neurons, supportive brain cells, gut lining cells, skin cells, and many other cells.
A NEW FRONTIER FOR FIGHTING DISEASE
Scientists are largely still learning about T cell communication and the sources by which this communication takes place. Researchers hope that new discoveries will allow the development of a wide range of new medical treatments to stimulate actions against infections and cancers by modifying these natural conversations.
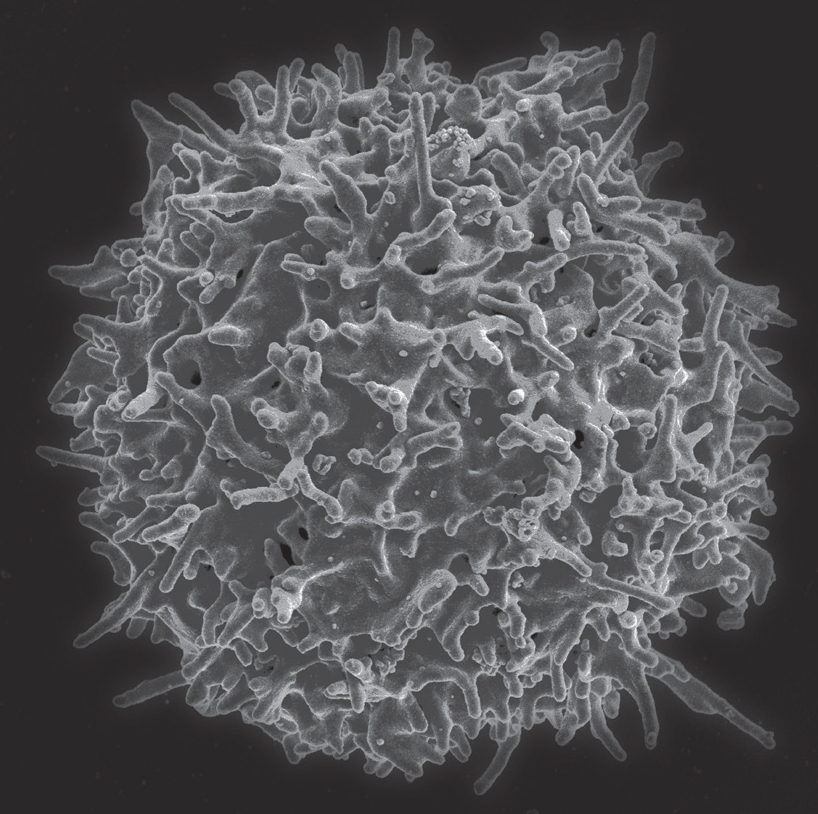
A healthy T lymphocyte. Electron micrograph. (NIAID/Science Source)
Some approaches could involve producing entirely new signals and receptors placed on cells. Treatments could include delivery of signals via microbes that normally talk with each other and with cancer cells. Intercepting signals from T cells will be vital for the treatment of a host of autoimmune diseases. By modifying T cell behavior via new signals, new treatment avenues could open up for diabetes, arthritis, pain, lupus, and multiple sclerosis, among many other diseases.
T cells can now be energized by inserting engineered viruses or other microbes inside them. We call these kinds of T cells superkillers. This genetic engineering technique uses microbes to stimulate new receptors, which unleash a heightened immune response to eradicate cancer and other diseases.
In general, however, it has been found that T cells are naturally better at fighting microbes than cancer. This is because fighting an infection usually involves one intense battle. For cancer, with multiple mutated stem-cell subtypes and various stages of development, a longer, more sequential war must be waged. T cells often become exhausted in such a prolonged battle. Future research could strengthen T cells for a longer-lasting, multifaceted approach to attack various cancer subtypes during multiple stages of the cancer life cycle.
Researchers hope new discoveries into the ways that internal T cell signals alter their own behavior will also lead to medical treatments for food allergies and even cancer. T cells can be very aggressive in producing inflammation and then change entirely to tamp down inflammation activity. This progression from aggressor to helper occurs when a microbe infection is neutralized or after traumatized tissue is rebuilt. The change can halt further damage to tissue that could lead, for example, to scar tissue.
After the battle is over, T cells alter their external signals to modulate the behavior of the entire variety of cells engaged against microbes. This same type of T cell regulatory behavior occurs on a daily basis in the gut, where T cells inhibit immune cells from attacking food particles and friendly microbes.
Understanding how these signals work for these regulatory actions could enable treatments for runaway infections and for alleviating food allergies. On the other hand, finding ways to alter this signal behavior could enable T cells to fight a full battle for a longer period of time as a cancer treatment. In addition, scientists have recently discovered that T cells leave long-lasting offspring at the site of a battle with microbes. These memory T cells stay vigilant in the trouble spot for years. Future treatments based on these memory cell signals could enhance the prevention of infections of all types.

Four T cells fighting a larger cancer cell. Electron micrograph. (Steve Gschmeissner/Science Source)
FROM BIRTH TO GRADUATION
T stands for thymus, which is a small but central gland that contributes to both the lymphatic and endocrine systems. The thymus, little more than two inches long and weighing about a half ounce at its peak, is situated in front of the heart and behind the breastbone. It consists of a left and a right lobe, which in turn consist of smaller sections called lobules, which account for the gland’s bumpy appearance.
Starting life in bone marrow, T cells migrate to the thymus and other lymph tissues. In lymph tissue, dozens of different T cell types can arise. In the thymus, T cells undergo their extensive education with a gradual maturation into fully functioning masters. Only 2 percent graduate. The other 98 percent that do not meet the exact qualifications required by a series of checkpoints are eliminated by their instructors.
After T cells are tested and approved, graduation consists of a change in their status. Mature T cells are released to investigate each cell they meet while traveling in all regions of the body. These T cells can rapidly change themselves into multiple varieties of cells and can trigger various kinds of inflammation. They can transform into fearsome killer cells that fight disease wherever needed in the body.
The Training Process—Meet the Lineup of T Cell Teachers
Thymus teacher cells are a distinct class of lining cells and are different from any other cell in the body. These thymus lining cells organize the structure and functions of the thymus and provide the “training” and pruning of young T cells.
Teacher cells exist in two broad categories, each with many subsets that are just being discovered. One category organizes the outer thymus region into a precise, brainlike, three-dimensional structure of concentric circles. The other exists in an amorphous center region.
It appears that most T cells need training from both types of teacher cells. Some receive training in the outer layers first and are then transferred to the center. Others start in the center and then travel to the edge layers.
The outer thymus cells first attract immature T cell precursor cells that begin to travel through the blood from their birth in the bone marrow. The teacher cells send specific signals with instructions on how to travel to the thymus and enter.
One unusually large teacher cell in the outer region is called a nurse cell. It takes up a student T cell entering the thymus, engulfs it, and forms a cage around it, separating it from the rest of the thymus environment. In this isolated state, the nurse cell tests the immature T cell by bombarding it with a wide variety of signals. In response, the student begins to produce a large number of different receptor types.
Cells that fail at this point are liquidated in the garbage-disposal compartment of the nurse cell. Others are rerouted into a less complex pathway to become regulatory T cells, which focus on specific tasks, rather than a full master T cell that is able to respond to almost any stimuli. Student cells that pass tests in the periphery of the thymus are then sent into the center, where the second set of teacher cells also has several unusual cellular characteristics.
Just as there are a large number of different T cell receptors and an almost infinite number of different antibodies, recently it was found that there are many types of teacher cells in the center of the thymus. These teacher cells use their DNA to maximize training for the T cells. Although most cells use only selected genes to function at particular moments, these special teacher cells in the center of the thymus use all of their genes at once to produce all of their possible proteins.
This deluge of protein molecules from a wide range of teacher cells greatly challenges the T cells to produce more and more receptors. With so many teacher cells testing individual T cells—each type bombarding the student cell with a plethora of proteins—it is clear that T cells undergo rigorous training before they begin their ultimate jobs. But the most important part of the training is that T cells must understand not to attack normal human cells and tissues while they search the body for trouble. When T cells are able to identify the difference between “foreign” molecules and “self” molecules, they avoid causing autoimmune diseases.
Antigens and Affinity
A molecule that could trigger an immune response is called an antigen. When the molecules advertised on the surface of a cell are normal, they are called “self-antigens.” Self-antigens placed in a special groove on the outside surface of cells tell T cells that this cell has no problems and there is no foreign material inside, such as a virus. Self-antigens signify a normal cell.
It is a T cell’s most important function to not harm normal human cells, while actively destroying microbes, cancer, and debris. If T cells don’t get self-antigens right, they attack normal human cells, leading to tissue destruction and autoimmune diseases.
The thymus exam system is, in fact, more subtle than just turning a switch on or off or providing a yes or no answer about self-antigens. For simplicity, the training is often described as a simple dichotomy of the cell knowing whether to respond to foreign molecules with a dangerous attack or not respond at all to self-molecules.
But the process is more complex. To fulfill their multiple functions, T cells must respond to all cells, but in different ways. T cells have to maintain an attraction to all normal human cells to continue communication while not attacking. For example, they must be attracted to neurons enough to engage in back-and-forth conversations about illness but not attracted enough to do damage. Most immune signals that T cells produce are called cytokines, but they also use neurotransmitters to converse with brain cells. When conversing with T cells, neurons use both types of signals as well.
It is not just the ability to recognize self or not-self that is measured by T cell instructors, but even more importantly the ability to measure the intensity of attraction—called affinity—for normal cells that allows graduation. If attraction doesn’t exist at all, T cells can’t communicate well enough with these cells. If attraction is too strong, problems will arise, such as tissue destruction. The amount of attraction has to be just right—not too weak and not too strong.
After graduation, T cells do their job, wandering through blood, lymph, and various types of tissue searching for molecules in the surface grooves of all cells. Unfortunately, after taking a series of exams in the thymus university to test their ability to make these receptors, most T cells fail. Failure to advance is often not just because they cannot produce a large, accurate range of signals and receptors. Many are rejected because they have a poor rating on their ability to avoid harming human cells during attacks.
Recent studies have shown that some of the rejected cells are rerouted into different pathways to produce regulatory T cells instead of the master regulators (as described earlier in the chapter). Future understanding of the signals used for this selection process could allow alterations of T cells to fight a wide range of diseases.
PRODUCING SIGNALS
The T cell builds the largest repertoire of receptors and signals—more than any other cell—for its myriad functions. It is not known how T cells can build so many varied molecules and then adapt them to changing conditions. But it does involve regulating multiple layers of genetic processes to produce unique proteins and then modifying them. Many of these levels of genetic activity occur in all cells, but T cells have the additional ability to edit sections of their own DNA.
As is well known, DNA code produces a particular RNA strand based on that code. A protein is then constructed from this strand of RNA. Other RNAs that are produced from DNA code don’t lead to proteins but instead perform other actions. Some produce factories that manufacture proteins, some carry amino acids to the factories to build proteins, and others are used as signals against microbes and for other purposes. Forming RNA molecules from the DNA code and then manufacturing proteins involve multiple layers of complexity that are not yet fully understood. People used to think that a gene was a single strand of DNA that produces code for one particular RNA and then a protein. In fact, the DNA code that is gathered for the RNA template can be taken from one “gene” and multiple other regions.
Once produced, the RNA template, called messenger RNA, has sections deleted, and the remaining code is sewn together into one usable messenger RNA strand. Once this messenger RNA molecule is produced, it is then further edited in multiple ways without any obvious direction. This single strand of messenger RNA can be cut and pasted in different ways to produce a large number of different proteins. After this editing of the messenger RNA, signals and tags modulate the actions of all the other types of RNAs. Once proteins are produced, they are also tagged and modified in various ways.
Although these editing and modification steps are used by all cells, T cells are one of only two cells that can also self-edit their own strands of DNA to produce totally new types of receptors and signals with entirely new arrangements of DNA code. By editing their own DNA, T cells can produce receptors to respond to newly evolved viruses and microbes, poisons from the environment, and synthesized chemicals that human bodies have never encountered before.
This DNA editing process is complex and tightly orchestrated, with at least ten completely different steps, using a series of large enzymes in sequence. Sections are cut from three regions of their own genes and are sewn together in different ways to make brand-new receptors.
In addition to receptors, T cells produce a wide range of signal molecules that are transmitted to other cells in a variety of ways. Most often, signals are released into the tissue between cells or in blood vessels, where they travel to their target. Signals can also be wrapped in a small sac and launched to their destination. Another tactic is sending signals via tiny protein-based tubes built between cells. T cells can also communicate by direct physical contact between cells with rapid back-and-forth exchanges of molecules.
The only other human cells able to edit their own DNA are B lymphocytes, which use a similar sequence of enzymes to readjust their own DNA in order to produce antibodies. But B cells need T cells to produce the most effective antibodies.
CONVERSATIONS WITH THE BRAIN
While stationary connections between neurons in brain circuits make up the “wired brain” for direct communication to distant locations, traveling T cells can be seen as a “wireless system” that directly communicates with the brain. Neurons and T cells are always talking and working together to keep the body healthy. They both respond to infections, foreign material, trauma, perceptions, and stress.
It is well known that cells in organs talk with their local neurons and traveling immune cells for many reasons. But it has recently been learned that frequent conversations also involve elaborate long-distance communication between immune cells and brain cells. This can occur via secreted signals in the blood or brain fluid or by stimulating local neurons to signal to distant brain circuits.
One example of this signaling phenomenon with local nerves involves T cells that lie in tissue between local neurons. Signals from T cells traveling in the tissue to nearby neurons trigger actions in distant brain circuits that produce an acupuncture effect in an unexpected organ. (This is further discussed later in this chapter and in section two in relation to chronic pain syndromes.)
In the past, conversations between T cells and brain cells were known to be important for infections in the brain, but little research was available to show exactly how these conversations occur. With more advanced lab equipment, scientists now have the ability to pick up distant small molecular signals, which have been found to be vital for global regulation of cognition in normal conditions, as well as mental changes related to stress, depression, and the “sick feeling” during illness. In the future, discovering more of these relevant signals could enable completely new types of psychiatric treatments by intercepting and modifying these communications.
When all is well, T cell signals tell the brain that conditions are safe for normal activity. The T cells do this with a constant pulse of signals to the brain, which enables normal mental processes. The brain responds with its own signals to let the immune system know that everything is okay.
Upon finding microbes, infections, or trauma, T cells change their messages to the brain to signal that the body is sick and the brain must slow it down to rest and conserve energy while fighting the infection. This conversation triggers the “sick feeling” of lethargy and achiness. When the infection has ended, only T cells have the authority to signal that it is okay to restore normal cognitive functions.
Until recently, the brain was considered to be free of immune cells—it was incorrectly called “immune privileged.” With better microscopes, scientists can observe immune cells in the cerebrospinal fluid (CSF) that bathes and protects the entire brain. This fluid was thought to function only as protection for the brain when jostled. But now it is known to be a river of wireless communication, with signals coursing throughout the brain from all regions and all types of cells. Also, it is now known that at most times there are about 500,000 T cells in the CSF along with smaller numbers of other immune cells.
Into the Brain and Through Other Difficult Terrain
T cell conversations with gatekeeper cells determine what is allowed to cross between the sheltered brain fluid and the busy blood vessels. Other immune cells approved for entry into CSF all have particular jobs in relation to T cells. One type of white blood cell picks up molecular samples of microbes, cancer cells, or debris and presents them to T cells for evaluation. B cells are there to make antibodies when needed to fight infections.
If there are no T cells in the CSF to direct these other cells, inflammation is triggered. Other immune cells don’t understand the subtleties of living in the brain as T cells do. So, T cells must actively suppress the actions of all these other cells to keep them from producing dangerous inflammation. Conversations to suppress inflammation occur constantly among T cells and neurons, using both neurotransmitters and cytokine signals.
CSF circulates around the brain, drains along nerves, then joins lymph nodes and blood in the neck. T cells travel through the entire brain fluid, leave the brain, and go to the neck lymph nodes looking for suspicious particles to evaluate. They gain permission from gateway cells over and over as they travel in and out of the CSF and to other parts of the body.
Signals from other cells also help with T cell travel. Local tissue cells and blood vessel cells send supportive and directional signals along the way, both in the brain and throughout the body, to further assist in this difficult journey to the lymph nodes. Using these signals, T cells travel to lymph nodes across a difficult terrain—through dense scaffolding in between cells and often without enough oxygen. T cells also receive permission from capillary cells when they need to leave the blood vessel to get to an infection. Signals even allow them to grab onto the blood vessel lining cells and climb against the flow of blood to get to particular locations.
To pick up invading microbes, cancer cells, and dangerous material, T cells rapidly change their size, shape, and function by altering their internal metabolism, which allows production of powerful armies of killer cells and regulatory cells. Killer cells form potent physical attachments with other cells to rapidly destroy them. They produce regulatory T cells that slow down inflammation after their healing job is done, avoiding damage to tissue. These regulatory cells are similar to the cells inhibiting reactions to food particles, but with other targets and conversations.
T cells also produce memory cells to leave behind. These memory cells stay indefinitely at the inflammation site to monitor the situation. For years, memory T cells screen for any future recurrence and immediately signal for help if there are problems.
T Cells and Microglia—Vital Partners
There is another reason that scientists did not understand immune function in the brain. Until recent technology emerged, conversations between T cells and microglia, the primary immune cells in the central nervous system, could not be detected. Microglia are now known to be vital partners with T cells for all immune activity affecting the brain.
Microglia travel from bone marrow to the brain during fetus development. Once there, microglia and their offspring remain throughout an adult human’s life. Microglia keep up constant conversations with wandering T cells, brain cells, and other immune cells. Chapter eleven presents the complex life of microglia.
Under normal conditions, microglia help to maintain and prune neuron connections. In emergencies, microglia are called to duty as immune cells through signals from T cells. They change their shape and become more aggressive in protecting the brain from infection, cancer cells, or damage from trauma and Alzheimer’s disease.
Activity in microglia’s belligerent state can increase inflammation in some situations and can actually expand the damage caused by Alzheimer’s. Intercepting these natural conversations among T cells, microglia, and other brain cells is now in the vanguard of research into Alzheimer’s and other brain diseases.
T Cells and Acupuncture
Communication between T cells and the brain occurs in other ways. Back-and-forth signals are sent between the brain, lymph tissues, and bone marrow using neurons that extend throughout the body. Two major nerve systems, sympathetic and parasympathetic, perform opposite functions in most internal organs, such as increasing or decreasing heart rate, or making the gut muscles active or inactive. T cells have conversations with neurons in both of these systems while in local regions of the body. Signals between neurons and nearby T cells diffuse through tissue back and forth.
This type of conversation between nerves and T cells appears to be part of the mechanism for the effects of acupuncture. Recently, it was found that an acupuncture point in the arm, not near any blood vessels or nerves, triggered an effect in the brain. Stimulating the acupuncture point with electricity, in fact, activated a T cell at that spot between two nerves. The T cell then sent signals to the nerves that were relayed into the brain, causing effects in distant locations. This type of signaling between nerves and independent traveling cells is discussed in more detail in chapter nine, devoted to neurons, and in chapter fourteen about pain.
A Complex Interplay Between Inflammation and Depression
Other conversations among T cells and the brain reflect a complex interplay between inflammation and depression. When there is no infection, T cells send signals that stimulate normal activity for the brain’s memory center, including the production of new neurons. With depression, T cells signal for inflammation and for less production of memory cells. Then, when treatments help alleviate depression, T cells again send signals to trigger production of new memory cells. Much more needs to be learned about these cellular conversations, which could lead to new treatments for depression. This is discussed further in section two, about the brain.
Stress is another human experience at the interface of brain function and inflammation. T cells are essential for dealing with stress in several ways. Both brain and immune cells pick up perceptions of stress. Brief stress related to learning or the unexpected can be helpful in stimulating positive brain activity. However, chronic stress can trigger damaging inflammation through immune responses.
During brief stress associated with normal learning, T cells help stimulate spatial learning and memory with signals. With chronic stress, T cells direct destructive inflammation responses that can decrease memory and contribute to depression. All of this occurs with back-andforth signals among T cells and a variety of brain cells.
KILL OR DO NO HARM—A COMPLEX PROCESS
We know now that a molecule that could trigger an immune response is called an antigen, and when the molecules advertised on the surface of a cell are normal, they are called self-antigens. Self-antigens that are placed in a special surface groove of a cell’s membrane tell T cells that this cell has no problems and there is no foreign material inside, such as a virus. Self-antigens signify a normal cell.
The T cell’s most important function is to not harm the body while actively destroying microbes, cancer, and debris. If T cells don’t get self-antigens right, they attack normal human cells, which leads to tissue destruction.
Mature T cells scan each cell they meet, looking for specific signs of normalcy and disease. Signs include identification molecules from inside the cell placed on the surface in a special groove, and tags placed by other immune cells to mark internal infections. Identification molecules are placed by each cell to reflect what is occurring inside—normal function, infection with microbe invaders, cancer, or damage.
Two Systems for Evaluation
There are two major systems that T cells use to identify molecules on other cells for evaluation. One system involves special presentation cells that take molecules from abnormal cells and present these particles to T cells. If both the T cell and the presentation cell agree that this is a dangerous particle, the T cell becomes activated and morphs into the fighting variety. For this activation, the presentation cell must not only present the particle but also give a second signal of agreement to the T cell.
The second system occurs with all other cells, except red blood cells, where sample molecules from inside are placed onto their surfaces. T cells evaluate these molecules without the help of presentation cells, but only T cells that are already activated killer cells are able to respond aggressively to these dangerous particles without the additional help of presentation cells.
Daily intake of food presents a special type of foreign material that is evaluated by T cells. In the gut, a constant barrage of food particles that could all potentially be considered foreign could produce deadly immune reactions with every meal. It is necessary for regulatory T cells to be produced strictly for the task of inhibiting such food reactions.
T cells are so expert at this that they can even avoid reactions to synthetic chemicals that have never been seen in nature before. What is difficult about responses to food particles is that these special T cells must be supported by collaborative conversations with gut cells and microbes on a daily basis. Gut lining cells and microbes imbue these T cells with an understanding of necessary nutrients and digestion products, as well as which particular gut microbes are friends.
Vitamins, such as vitamin D3, vitamin A, and folic acid, also serve as important signals in these conversations to remind protective T cells to avoid attacks. The way that gut cells and friendly microbes train T cells on a daily basis is described further in chapter six on gut cells and chapter seventeen about microbes in the gut.
In Hostile Territory
To chase microbes, killer cells must rapidly reproduce and travel throughout the body in hostile territory, often without oxygen and food. T cells are able to use their internal metabolic cycles in totally new ways that are designed for this difficult trip. Molecules that are normally part of ordinary nutrition and energy pathways inside the cell are turned into signals that stimulate the dramatic transformation into a larger, aggressive cell.
The new metabolism that is necessary for aggressive T cells uses alternative methods of obtaining energy from locations inside the cell other than the usual mitochondria. New substituted foods, such as glutamine, are not part of their usual diet. Burning glutamine instead of sugar increases energy production by two hundred times the normal rate for rapid aggressive behavior. However, using this alternative food is very costly to the cell, with extreme demands placed on internal resources; therefore, the new situation cannot last long.
The conversations for this dramatic alteration into a fearsome belligerent cell occur inside, between several cell compartments. One is the location of metabolic pathways in the cell, and another is the nucleus, where genes trigger production of new materials to build the powerful aggressive cell. A similar type of internal signaling also allows cancer cells to have unusually aggressive properties. Understanding these internal T cell signals could allow new treatments based on stimulating T cell strength while decreasing that of cancer cells.
In the midst of battle, as described earlier, killer T cells form a physical attachment, called the immune synapse, with an unfortunate targeted cell. This connection is quite different from a neuron synapse in structure and function, and it only lasts for a brief time. When T cells touch the target cell, almost instantly membranes of both cells form a temporary interlocking connection resembling interlaced fingers. Within minutes, larger scaffolding molecules make a flat, permanent connection, and the interdigitation recedes.
A large, complex molecular machine—usually used during cell division to orchestrate chromosomes being dragged into place—is pushed and pulled by motors into place near the synapse. This machine then produces a large, syringe-like device that launches packets of toxic granules into the poor victim. This complicated process takes only minutes and has dramatic results.
Protecting Healthy Tissue
Another important T cell tactic protects local tissue cells during battles, somewhat similar to protecting against responses to food particles. The original T cell knew how not to kill normal cells, but the army of cloned killer cells needs help with this.
The original T cell doesn’t pass on this subtle knowledge to the rapidly produced army of derivative cells. But when the battle is winding down, T cells produce a new kind of regulatory T cell that watches for danger and instructs killer cells to slow down and avoid attacking normal human cells. These regulatory T cells patrol the action.
Many different signals are used in this protective process to alter the metabolism of the killer cells. If killer cells do attack normal cells, these regulatory T cells actively intervene with signals. This is another area in which future research into signals could enable new ways to treat dangerous infections.